Abstract
Background:
Partial-thickness rotator cuff tears (PTRCTs) often progress to full-thickness rotator cuff tears (FTRCTs). Thus, it is important to analyze the risk factors for tear progression to determine the proper timing of repair.
Purpose:
To identify the risk factors associated with progression of PTRCT.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Included were 89 patients diagnosed with PTRCT on magnetic resonance imaging (MRI) scans who underwent nonoperative treatment at the authors’ institution between August 2012 and August 2019. Patient characteristics, shoulder stiffness (compared with the contralateral shoulder); work level (classified as high [heavy manual labor], medium [manual labor with less activity], and low [sedentary activity]); and radiological factors including initial tear size, acromion type (flat, curved, hooked, or heel-shaped), and initial tear involvement (as a percentage of the rotator cuff tendon footprint length) were analyzed to assess their association with tear progression, defined as >20% increase in tear involvement.
Results:
The mean MRI follow-up period was 22.3 ± 17.2 months (median, 16.1 months; range, 6.4-89.5 months), and tear progression was observed in 12 patients (13.5%). In these 12 patients, tear involvement increased by 60% of the rotator cuff footprint, while mediolateral (ML) and anteroposterior (AP) tear sizes progressed by 1.1 and 1.8 mm, respectively. Univariate regression analysis showed that shoulder stiffness (P = .031), work level (P = .001), initial tear involvement (P < .001), ML and AP tear sizes (P < .001 and P = .005, respectively), and acromion type (P = .003) were significantly associated with tear progression. Multivariate regression analysis showed that initial tear involvement (odds ratio [OR], 1.053; 95% CI, 1.006-1.102; P = .026) and high work level (OR, 15.831; 95% CI, 1.150-217.856; P = .039) were independent risk factors for tear progression. The cutoff value for initial tear involvement was 47.5% (sensitivity, 81.8%; specificity, 85.7%).
Conclusion:
Tear progression was observed in 14% of patients with PTRCT in this study. To predict tear progression, evaluating the tear involvement during initial MRI is essential. The risk of tear progression increased with initial tear involvement >47.5% and a heavy work level.
Keywords: partial thickness, symptomatic rotator cuff tear, tear progression, risk factor, initial tear involvement, work level
Partial-thickness rotator cuff tear (PTRCT) is as common as full-thickness rotator cuff tear (FTRCT) 29 and is often associated with more pain than FTRCT, leading to functional limitations. 6,16,30 However, compared with FTRCT, the footprint of the supraspinatus muscle is partially preserved in PTRCT; thus, the retraction of the torn tendon is relatively less severe. Moreover, several previous studies have reported satisfactory outcomes with nonoperative treatment. 17,21,27 On the other hand, there is an increased likelihood of progression to FTRCT in high-grade PTRCT, and the torn rotator cuff tendon does not spontaneously heal. 16,27
Clinicians may consider the risk of tear progression as an important factor while choosing between nonoperative and operative treatment for patients with PTRCT. Compared with FTRCT, PTRCT is known to have a relatively low risk of tear progression. However, only a limited number of studies have analyzed the tear progression rate, which yielded various progression rates varying from 15% to 80%. 15,17,29,34 Thus, there is no clear consensus on progression rate of PTRCT. In addition, while a number of studies have analyzed the risk factors of tear progression in FTRCT, there is a lack of studies involving PTRCT. Therefore, this study aimed to identify the risk factors associated with tear progression of PTRCT.
Methods
This was a retrospective study to identify risk factors of tear progression in PTRCT. Informed consent was obtained from all patients at the time of follow-up MRI, and final approval was obtained from our institutional review board. Eligible patients were those diagnosed with PTRCT of the supraspinatus tendon using magnetic resonance imaging (MRI) between August 2012 and August 2019.
Initial nonoperative treatment included physical therapy, medications (nonsteroidal anti-inflammatory drugs), and standard rehabilitation. When symptoms did not improve after the initial treatment, steroids were injected once into the patients by a single senior author (S.H.K.). If symptoms such as pain and limited range of motion (ROM) persisted, then patients were advised to refrain from lifting heavy objects over the shoulder or playing sports activities. If the symptoms did not improve and the PTRCT depth was >50% after at least 3 months of nonoperative treatment, surgical treatment was recommended. However, patients who refused surgical treatment continued to receive nonoperative treatment. All patients diagnosed with PTRCT, except those who underwent surgical treatment, were recommended for follow-up MRI at 6 months after nonoperative treatment to assess tear progression.
Included in this study were patients with symptomatic PTRCT of the supraspinatus confirmed via MRI scans and who agreed to undergo follow-up MRI. We excluded patients who (1) underwent surgical treatment within the follow-up period, (2) previously underwent shoulder surgery on the ipsilateral side, (3) had arthritis of the glenohumeral joint (eg, osteoarthritis or postinfectious sequelae), and (4) had a full-thickness subscapularis tendon tear graded as Lafosse type ≥2. 2
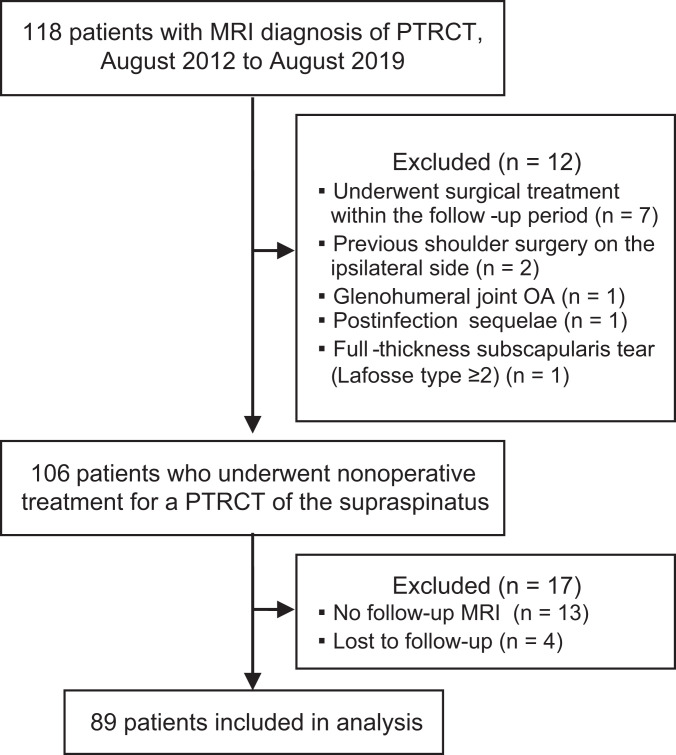
During the study period, 118 patients underwent nonoperative treatment after being diagnosed with a PTRCT. Of these patients, 29 did not meet the inclusion criteria, leaving a total of 89 patients enrolled in the study. Figure 1 provides a summary of the patient enrollment process.
Figure 1.
Flow diagram of patient enrollment. MRI, magnetic resonance imaging; OA, osteoarthritis; PTRCT, partial-thickness rotator cuff tear.
Patient Characteristics and Clinical Evaluation
At the first outpatient visit, characteristics of patients including age, sex, affected side (right or left), body mass index (BMI), symptom duration, comorbidities (eg, diabetes mellitus [DM] and hypercholesterolemia), history of trauma before symptom onset, smoking and alcohol status, and patient’s physical work level were collected. Symptom duration was defined as the time from the onset of pain to the first outpatient visit. Patients with DM were classified into 3 groups according to their serum glycosylated hemoglobin (HbA1c) levels 3 : patients with controlled DM with HbA1c <7.0%, patients with uncontrolled DM with HbA1c ≥7.0%, and patients without DM. Although no study has shown an association between hypercholesterolemia and RCT progression, hypercholesterolemia is known to affect the development of RCT 28 and its integrity after repair. 8 Therefore, hypercholesterolemia was assessed.
Smoking status was classified into nonsmokers, current smokers, and former smokers. 14 Alcohol status was classified into 3 groups according to the frequency of drinking: nondrinkers (less than once a month), light drinkers (more than once a month but less than twice a week), and heavy drinkers (more than twice a week). 9 Physical work level was divided into high (heavy manual labor), medium (manual labor with less activity), and low (sedentary work activity). 4 Clinical assessment included pain level and stiffness. Pain level at the first outpatient visit was compared with that during follow-up MRI and was classified as “improved,” “no change,” and “aggravated.” 33 Stiffness was defined as 40°, 20°, and 5 spine-level differences in forward flexion, external rotation at the side, and internal rotation to the posterior, respectively, compared with the passive ROM of the opposite shoulder. 13 Internal rotation to the posterior was measured according to the vertebral level reached with the tip of the thumb. 13
Radiologic and MRI Evaluations
All radiologic parameters were measured independently by 2 orthopaedic surgeons in a blinded setting (M.S.K. and Y.D.J.). Interobserver reliability was calculated, and to evaluate intraobserver reliability, one of the observers (M.S.K.) repeated all measurements within 3 months of the original evaluation. Radiographs (true anteroposterior [AP] view and outlet view) were taken at the first outpatient visit to measure critical shoulder angle (CSA), 22 lateral acromial angle (LAA), 2 acromial slope (AS), 1 and acromiohumeral interval (AHI) 24 using the original method. The type of acromion was classified according to its shape: flat, curved, hooked, or heel. 23,25
All shoulder MRI scans were obtained with the patients in the supine position using a Philips Achieva 1.5-T scanner with a dedicated shoulder coil. Included in the MRI protocol were axial, oblique coronal, and sagittal turbo (fast) spin-echo T2-weighted imaging (repetition time/echo time [TR/TE], 1850-3800/80 ms, 3000-3800/80 ms, and 1697-3900/80 ms, respectively; slice thickness, 3.5 mm; slice gap, 0.35 mm; field of view [FOV], 15 cm; matrix, 448 × 224; echo train length [ETL], 14); oblique coronal turbo (fast) spin-echo T1-weighted imaging (TR/TE, 500/20 ms; slice thickness, 3.5 mm; slice gap, 0.35 mm; FOV, 15 cm; matrix, 448 × 224; ETL, 3); and oblique coronal turbo (fast) spin-echo proton-density DRIVE-weighted imaging with fat saturation (TR/TE, 1733/20 ms; slice thickness, 3.5 mm; slice gap, 0.35 mm; FOV, 15 cm; matrix, 224 × 224; ETL, 4).
PTRCT was diagnosed using T2-weighted coronal MRI. A PTRCT was defined as a condition in which a high-intensity signal was observed in the footprint area of the RCT with partial continuity. Mediolateral (ML) and AP tear sizes were measured on T2-weighted images, while the length of the rotator cuff tendon footprint was used to calculate the ML tear involvement percentage 17 (Figure 2). Progression of PTRCT was defined when the ML tear involvement increased by >20% on follow-up MRI scan compared with the initial MRI scan. An increase or decrease ≤20% in tear involvement was considered as no change, and a decrease >20% was defined as improvement. 17 Articular- and bursal-side PTRCTs were defined as focal defects or discontinuities in the rotator cuff tendon in the articular and bursal sides, respectively. 10 Accompanied subscapularis tendon tears were analyzed for Lafosse type 1 partial-thickness tears. 18 Fatty infiltration of the rotator cuff muscles was evaluated in the Y-shaped view, which is the outermost area of the T1-weighted oblique sagittal view, using the Goutallier classification modified by Fuchs et al. 5
Figure 2.
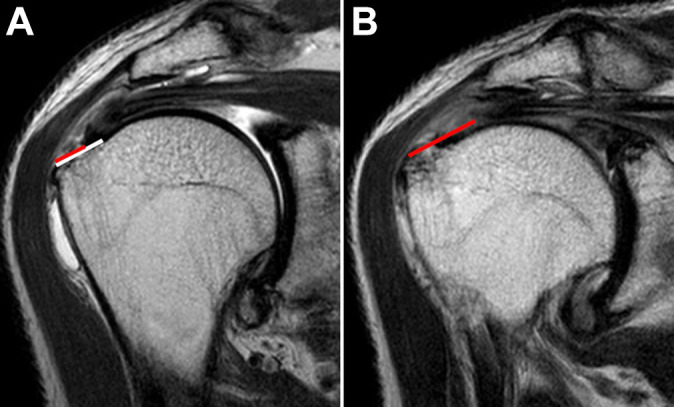
Coronal and sagittal T2-weighted magnetic resonance imaging (MRI) scans from a 54-year-old man with a high work level. (A) A bursal-side partial-thickness rotator cuff tear was observed on the initial visit; tear involvement was calculated as the percentage of the mediolateral tear size (red line) to the length of the rotator cuff tendon footprint (white line). The initial tear involvement of the supraspinatus muscle was 60.8%. (B) On follow-up MRI scan 13 months later, a larger rotator cuff tear was observed (red line), indicating tear progression.
Statistical Analyses
The Mann-Whitney U test, Wilcoxon signed rank test, and chi-square or Fisher exact test were used to compare descriptive variables and radiologic parameters between groups. Any significant predictive values in the univariate analysis were included in the multivariate logistic regression analysis to identify independent risk factors for PTRCT progression. To calculate the optimal cutoff value for predicting tear progression, we used receiver operating characteristic (ROC) curves; the value with the highest sensitivity and specificity was set as the cutoff value. Significance was set at P = .05, with associated 95% CIs. The SPSS software package (Version 21.0; IBM Corp) was used for all statistical analyses.
The inter- and intraobserver reliability of the radiologic parameters were determined using the intraclass correlation coefficient (ICC) with a 2-way random-effects model and the Cohen kappa (κ). The ICC values were interpreted as poor (<0.01), slight (0.01 to 0.2), fair (>0.2 to 0.4), moderate (>0.4 to 0.6), good (>0.6 to 0.8), or excellent (>0.8 to 1.0). 19 The κ values were interpreted as poor (≤0.2), fair (>0.20 to 0.40), moderate (>0.40 to 0.60), good (>0.60 to 0.80), excellent (>0.80 to <1.0), or perfect (1.0). 19
An a priori analysis performed using G*Power (Version 3.1.9.7) indicated that the required sample size was 11 patients in each group; thus, the sample size in this study was sufficient to have a power >0.80.
Results
The characteristics and radiologic parameters of the 89 enrolled patients are summarized in Table 1. Pain was improved in 52 patients (58.4%), unchanged in 33 patients (37.1%), and aggravated in 4 patients (4.5%) at the time of the follow-up MRI compared with the initial outpatient visit. The mean MRI follow-up duration was 22.3 ± 17.2 months (median, 16.1 months; range, 6.4-89.5 months).
Table 1.
Overall Patient Characteristics and Radiologic Parameters (N = 89 Patients) a
| Variable | Value |
|---|---|
| Age, y | 55.9 ± 9.6 |
| Sex, male/female | 26/63 |
| Side, right/left | 66/23 |
| Symptom duration, mo | 25.7 ± 33.5 |
| BMI | 23.7 ± 3.0 |
| Comorbidities | |
| DM, controlled/uncontrolled | 6/3 |
| Hypercholesterolemia | 8 |
| Smoking status, none/current/former | 75/10/4 |
| Alcohol use, none/light/heavy | 72/14/3 |
| Trauma history | 17 |
| Stiffness | 21 |
| Work level, low/medium/high | 28/48/13 |
| Time to follow-up MRI, mo | 22.3 ± 17.2 |
| Articular/bursal tear | 60/29 |
| Subscapularis tear, intact/partial | 70/19 |
| Acromion type, flat/curved/hooked/heel | 12/66/8/3 |
| Radiologic parameters | |
| CSA, deg | 33.5 ± 3.5 |
| LAA, deg | 75.1 ± 11.5 |
| AS, deg | 28.0 ± 8.9 |
| AHI, mm | 8.9 ± 1.5 |
a Data are reported as No. or mean ± SD unless. AHI, acromiohumeral interval; AS, acromial slope; BMI, body mass index; CSA, critical shoulder angle; DM, diabetes mellitus; LAA, lateral acromial angle; MRI, magnetic resonance imaging.
The tear involvement on follow-up MRI scans was 38.4% ± 48.5% (range, 3.0%-281.0%) of the length of the rotator cuff tendon footprint, which was significantly higher than that on initial MRI scans (28.2% ± 28.1% [range, 3.0%-99.0%]; P < .001). The footprint length, which was measured on the initial and follow-up MRI scans, was not significantly different (P = .862). A >20% progression of tear involvement was observed in 12 patients (13.5%). On the other hand, a ≤20% increase or decrease was observed in 73 patients (82.0%). Tear involvement was improved by >20% in 4 patients (4.5%), including 3 patients and 1 patient with tears on the articular and bursal sides, respectively. The ML tear size was 4.6 ± 5.0 mm on the follow-up MRI scans, which was significantly different from the size of 3.9 ± 4.4 mm noted on the initial MRI scans (P = .017). The AP tear sizes were 5.1 ± 4.1 and 5.5 ± 4.8 mm on the initial MRI and follow-up MRI scans, respectively; there was no significant difference in AP tear size (P = .413). For fatty infiltration, there were no significant differences in the supraspinatus, subscapularis, and teres minor muscles between the initial and follow-up MRI scans. However, fatty infiltration of the infraspinatus muscle was 0.9 ± 0.3 on the follow-up MRI scans, which was significantly different from 0.8 ± 0.4 on the initial MRI scans (P = .02) (Table 2).
Table 2.
Overall Results, Natural History of PTRCT a
| Overall | Initial MRI | Follow-up MRI | P |
|---|---|---|---|
| Tear involvement, % | 28.2 ± 28.1 | 38.4 ± 48.5 | .001 |
| ML tear size, mm | 3.9 ± 4.4 | 4.6 ± 5.0 | .017 |
| AP tear size, mm | 5.1 ± 4.1 | 5.5 ± 4.8 | .413 |
| Fatty infiltration b | |||
| Subscapularis | 0.9 ± 0.5 | 0.9 ± 0.5 | .320 |
| Supraspinatus | 0.9 ± 0.4 | 0.9 ± 0.4 | .369 |
| Infraspinatus | 0.8 ± 0.4 | 0.9 ± 0.3 | .020 |
| Teres minor | 0.9 ± 0.4 | 0.9 ± 0.3 | .181 |
a Data are reported as mean ± SD. Boldface P values indicate a statistically significant difference between groups (P < .05). AP, anteroposterior; ML, mediolateral; MRI, magnetic resonance imaging; PTRCT, partial-thickness rotator cuff tear.
b Goutallier classification, modified by Fuchs et al. 5
The interobserver ICCs were excellent: 0.96 for initial tear involvement, 0.95 for the initial ML tear size, 0.91 for the initial AP tear size, 0.90 for CSA, 0.96 for LAA, 0.92 for AS, and 0.87 for AHI. The κ values for fatty infiltration in the rotator cuff muscle between the independent observers were also good: 0.73 for the subscapularis, 0.70 for the supraspinatus, 0.74 for the infraspinatus, and 0.71 for the teres minor. The intraobserver ICCs were excellent: 0.96 for initial tear involvement, 0.97 for the initial ML tear size, 0.87 for the initial AP tear size, 0.90 for CSA, 0.96 for LAA, 0.97 for AS, and 0.86 for AHI. The intraobserver κ values for fatty infiltration were also good to excellent: 0.82 for the subscapularis, 0.79 for the supraspinatus, 0.74 for the infraspinatus, and 0.82 for the teres minor.
Risk Factors for Tear Progression
Univariate analysis showed that physical work level (P = .001) and stiffness (P = .031) were associated with PTRCT progression (Table 3). Among radiologic factors, initial tear involvement (P < .001), ML (P < .001) and AP (P = .005) tear sizes, and acromion type (P = .003) were associated with tear progression (Table 4).
Table 3.
Comparison of Patient Factors According to Tear Progression at Follow-up a
| Univariate Analysis | Tear Progression, n = 12 | No Tear Progression, n = 77 | P |
|---|---|---|---|
| Age, y | 55.7 ± 9.7 | 56.8 ± 8.6 | .709 |
| Sex, male/female | 3/9 | 23/54 | .730 |
| Side, right/left | 7/5 | 59/18 | .178 |
| Symptom duration, mo | 25.3 ± 35.1 | 25.8 ± 33.5 | .965 |
| BMI | 25.9 ± 2.2 | 23.4 ± 2.9 | .081 |
| Comorbidities | |||
| DM, controlled/uncontrolled | 1/1 | 5/2 | .323 |
| Hypercholesterolemia | 0 | 8 | >.999 |
| Smoking status, none/current/former | 2/9/1 | 8/66/3 | .387 |
| Alcohol use, none/light/heavy | 9/3/0 | 63/11/3 | .616 |
| Trauma history | 3 | 14 | .624 |
| Stiffness, n (%) | 6 (50) | 15 (19) | .031 |
| Work level, low/medium/high, n (%) | 5 (42)/1 (8)/6 (50) | 23 (30)/47 (61)/7 (9) | .001 |
| Time to follow-up MRI, mo | 20.3 ± 11.4 | 22.6 ± 17.8 | .670 |
| Shoulder pain status | .906 | ||
| Improved | 1 | 4 | |
| Similar | 4 | 29 | |
| Aggravated | 7 | 41 |
a Data are reported as No. or mean ± SD unless otherwise indicated. Boldface P values indicate a statistically significant difference between groups (P < .05). BMI, body mass index; DM, diabetes mellitus; MRI, magnetic resonance imaging.
Table 4.
Comparison of Radiologic Factors According to Tear Progression a
| Univariate Analysis | Progression, n = 12 | Not, n = 77 | P |
|---|---|---|---|
| Initial tear involvement, % | 67.2 ± 28.3 | 22.5 ± 23.2 | <.001 |
| Initial tear size, mm | |||
| ML | 9.8 ± 6.8 | 3.0 ± 3.1 | <.001 |
| AP | 9.1 ± 5.2 | 4.2 ± 3.4 | .005 |
| Follow-up tear involvement, % | 126.0 ± 70.0 | 24.5 ± 23.5 | <.001 |
| Follow-up tear size, mm | |||
| ML | 10.9 ± 5.9 | 3.7 ± 4.0 | <.001 |
| AP | 10.9 ± 3.9 | 4.2 ± 3.4 | <.001 |
| Radiologic parameters | |||
| CSA, deg | 35.1 ± 3.6 | 33.3 ± 3.5 | .107 |
| LAA, deg | 79.4 ± 11.2 | 74.4 ± 11.5 | .166 |
| AS, deg | 33.2 ± 10.1 | 27.2 ± 8.5 | .070 |
| AHI, mm | 9.1 ± 2.2 | 8.9 ± 1.4 | .563 |
| Acromion type, n (%) | .003 | ||
| Flat | 5 (41.7) | 7 (9.1) | |
| Curved | 4 (33.3) | 62 (80.5) | |
| Hooked | 1 (8.3) | 7 (9.1) | |
| Heel | 2 (16.7) | 1 (1.3) | |
| Articular/bursal tear | 11/1 | 49/28 | .094 |
| Subscapularis tear, intact/partial | 11/1 | 59/18 | .237 |
| Initial fatty infiltration b | |||
| Subscapularis | 0.9 ± 0.8 | 0.9 ± 0.4 | .946 |
| Supraspinatus | 0.8 ± 0.6 | 0.9 ± 0.3 | .779 |
| Infraspinatus | 0.8 ± 0.5 | 0.8 ± 0.4 | .483 |
| Teres minor | 0.9 ± 0.3 | 0.7 ± 0.5 | .171 |
| Follow-up fatty infiltration b | |||
| Subscapularis | 1.0 ± 0.7 | 0.9 ± 0.4 | .665 |
| Supraspinatus | 0.8 ± 0.6 | 0.9 ± 0.4 | .665 |
| Infraspinatus | 0.9 ± 0.3 | 0.9 ± 0.4 | .976 |
| Teres minor | 0.9 ± 0.3 | 0.8 ± 0.5 | .267 |
a Data are reported as No. or mean ± SD unless otherwise indicated. Boldface P values indicate a statistically significant difference between groups (P < .05). AHI, acromiohumeral interval; AP, anteroposterior; AS, acromial slope; CSA, critical shoulder angle; LAA, lateral acromial angle; ML, mediolateral.
b Goutallier classification, modified by Fuchs et al. 5
In multivariate logistic regression analysis, initial tear involvement (odds ratio [OR], 1.053; 95% CI, 1.006-1.102; P = .026) and high physical work level (OR, 15.831; 95% CI, 1.150-217.856; P = .039) were significant independent predictors of tear progression (Figure 2 and Table 5).
Table 5.
Independent Risk Factors for PTRCT Progression a
| Multivariate Analysis | OR (95% CI) | P |
|---|---|---|
| Stiffness | 0.610 (0.101-3.676) | .590 |
| Work level (reference: low) b | ||
| Medium | — | .996 |
| High | 15.831 (1.150-217.856) | .039 |
| Initial tear involvement | 1.053 (1.006-1.102) | .026 |
| Initial AP tear size | 1.015 (0.754-1.367) | .920 |
| Acromion type (reference: flat) b | ||
| Curved | — | .996 |
| Hooked | — | .997 |
| Heel | 20.054 (0.611-658.537) | .092 |
a Boldface P values indicate statistical significance (P < .05). AP, anteroposterior; OR, odds ratio; PTRCT, partial-thickness rotator cuff tear. Dashes indicate not applicable.
b Revealed by multinomial logistic regression.
The ROC curve was used to evaluate the optimal cutoff value for initial tear involvement, while the area under the curve was 0.883. The cutoff value for initial tear involvement with the highest sensitivity and specificity was 47.5% (sensitivity, 81.8%; specificity, 85.7%).
We performed a post hoc power analysis using the value of initial tear involvement, which showed significant association with tear progression. The effect size was 1.870 (95% CI, 1.197-2.534), and at an alpha of .05, the power of this study was 0.961.
Discussion
In the current study, tear progression was observed in 13.5% of patients with PTRCT after a mean follow-up period of 22.3 ± 17.2 months (median, 16.1 months; range, 6.4-89.5 months). Overall, in all patients with PTRCT involved in this study, the initial tear involvement progressed by approximately 10%. In patients with tear progression, the initial tear involvement, ML tear size, and AP tear size increased by approximately 60%, 1.1 mm, and 1.8 mm, respectively. Independent risk factors that could predict the progression of PTRCT were the initial tear involvement and high work level.
PTRCT is observed in 5% to 30% of patients with shoulder pain and is a common disease with an incidence similar to that of FTRCT. 17,29 However, there are a limited number of studies on the natural history of PTRCT, especially on disease progression. In 1994, Yamanaka and Matsumoto 34 reported that tears progressed in 80% of patients with PTRCT over a mean follow-up period of 1.1 years. Keener et al 12 analyzed tear progression of PTRCT via ultrasonography over a mean follow-up period of 2.8 years and observed tear progression in 44% of patients. However, Yamanaka and Matsumoto only analyzed patients with articular-side PTRCT. Moreover, both studies reported by Keener et al and Yamanaka and Matsumoto only analyzed a small sample size of 36 and 54 patients, respectively. In contrast, Kong et al 17 observed tear progression in 16% of patients with high-grade PTRCT during a mean follow-up period of 1 year, reporting a relatively lower progression rate compared with previous studies. Furthermore, in a study by Maman et al, 21 tear size progressed by >5 mm in only 2 (8%) of 26 patients with PTRCT over a mean follow-up period of 20 months, suggesting a low tear progression rate despite the small sample size. Tear progression was observed in approximately 14% of the patients, which was similar to that reported by Kong et al and was lower than that reported in other previous studies. 12,34 During the follow-up period, the ML tear size progressed significantly; however, the mean difference was 0.7 mm, which may not have clinical significance.
Kim et al 15 followed up patients with PTRCT for approximately 2 years and observed that fatty infiltration in the supraspinatus did not change in 90% of the patients and that degeneration was aggravated in only 10% of patients. However, in that study, fatty infiltration in the supraspinatus muscle was classified only into the following: improved, no changes, and aggravated. Thus, the severity of fatty infiltration could not be properly assessed. In another study by Keener et al, 12 the fatty infiltration of the supraspinatus and infraspinatus muscles was more aggravated in patients with tear progression than in those without tear progression. Moreover, patients with FTRCT or PTRCT were included in their study; thus, changes in fatty infiltration of rotator cuff muscles according to tear progression in PTRCT were not reported. We observed that after a mean follow-up period of 22.3 ± 17.2 months (median, 16.1 months; range, 6.4-89.5 months), only the fatty degeneration of the infraspinatus muscle worsened; however, the mean difference was 0.1, which may not have clinical significance. There were no differences in fatty filtration between the initial and follow-up MRI scans in both patient groups with and without tear progression. This finding may be attributed to the patient group, as only patients with PTRCT were analyzed.
A torn rotator cuff is known to not spontaneously heal over time in patients with FTRCT. 11,15,31 However, in the natural history of PTRCT, tear size may decrease in 4% to 25% of patients, although this rate is not high. 15,17,20 Such a decrease in tear size may be related to the formation of scar or fibrotic tissues in the tear defects 7,26 or healing of the torn rotator cuff. 17 However, the detailed mechanisms are unknown. Additionally, factors that may reduce tear size have not been reported. Consistent with the findings of previous studies, we observed that tear size was significantly reduced in a small proportion of patients with PTRCT (approximately 5%). However, since the tear size was decreased in a small number of patients, factors that affect tear size reduction could not be analyzed; this must be investigated in further studies.
Lo et al 20 reported that tear progression was observed in 55% of patients with PTRCT with a tear thickness >50%, suggesting that this may predict tear progression. Furthermore, the dominant side and trauma history were also independent risk factors for PTRCT progression. Although, Yamamoto et al 32 did not evaluate patients with PTRCT, they reported that the dominant arm was a risk factor for RCT, which was similar to what was reported by Lo et al. Kong et al 17 had reported that the initial tendinosis grade was the only factor that was significantly associated with tear progression in patients with high-grade PTRCT. However, no other studies have reported risk factors associated with the progression of PTRCT. Although we did not analyze the dominant side and tendinosis, analysis of descriptive and radiologic variables showed that the initial tear involvement and a high work level were independent risk factors for PTRCT progression. Additionally, we calculated the cutoff value of the initial tear involvement with the highest sensitivity and specificity using the ROC curve, and the optimal cutoff value was 47.5%. The findings of Lo et al suggest that the increased use of the dominant side may increase the probability of tear progression. In our study, a high work level indicated heavy manual labor with abundant physical activity. Therefore, these findings suggest that repetitive physical work may increase the likelihood of tear progression.
Limitations
This study has some limitations. First, as this study was retrospective in design, there might be an inherent bias in determining which patients had follow-up MRI. Second, since the average follow-up period (approximately 22 months) was not long enough, long-term data were insufficient. In addition, there was a wide range of follow-up MRI, which may confound observations of tear progression. Third, as tear size was reduced only in a small number of patients, factors related to PTRCT improvement could not be analyzed thoroughly. Finally, previous studies reported no differences in functional scores between patients with and without tear progression. 15,17 In our study, functional scores according to tear progression, other than changes in pain, were not compared. Despite these limitations, our study is significant in the field because it is the first to identify the risk factors of PTRCT and to analyze the predictive cutoff value for the initial tear involvement.
Conclusion
Tear progression was observed in 14% of patients with PTRCT over a 2-year follow-up period. To predict tear progression, it is important to evaluate the tear involvement during the initial MRI. Moreover, the risk of tear progression increases with tear involvement >47.5% and a heavy physical work level.
Footnotes
Final revision submitted February 26, 2022; accepted March 31, 2022.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Ulsan University Hospital (UUH IRB File No. 2021-080-024).
References
- 1. Balke M, Schmidt C, Dedy N, et al. Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. 2013;84(2):178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Banas MP, Miller RJ, Totterman S. Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. 1995;4(6):454–461. [DOI] [PubMed] [Google Scholar]
- 3. Cho NS, Moon SC, Jeon JW, Rhee YG. The influence of diabetes mellitus on clinical and structural outcomes after arthroscopic rotator cuff repair. Am J Sports Med. 2015;43(4):991–997. [DOI] [PubMed] [Google Scholar]
- 4. Chung SW, Park JS, Kim SH, Shin SH, Oh JH. Quality of life after arthroscopic rotator cuff repair: evaluation using SF-36 and an analysis of affecting clinical factors. Am J Sports Med. 2012;40(3):631–639. [DOI] [PubMed] [Google Scholar]
- 5. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605. [DOI] [PubMed] [Google Scholar]
- 6. Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman’s classic. J Shoulder Elbow Surg. 2000;9(2):163–168. [PubMed] [Google Scholar]
- 7. Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85(1):3–11. [DOI] [PubMed] [Google Scholar]
- 8. Garcia GH, Liu JN, Wong A, et al. Hyperlipidemia increases the risk of retear after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2017;26(12):2086–2090. [DOI] [PubMed] [Google Scholar]
- 9. Jang HD, Hong JY, Han K, et al. Relationship between bone mineral density and alcohol intake: a nationwide health survey analysis of postmenopausal women. PLoS One. 2017;12(6):e0180132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jung JY, Jee WH, Chun HJ, Ahn MI, Kim YS. Magnetic resonance arthrography including ABER view in diagnosing partial-thickness tears of the rotator cuff: accuracy, and inter- and intra-observer agreements. Acta Radiol. 2010;51(2):194–201. [DOI] [PubMed] [Google Scholar]
- 11. Jung W, Lee S, Hoon Kim S. The natural course of and risk factors for tear progression in conservatively treated full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2020;29(6):1168–1176. [DOI] [PubMed] [Google Scholar]
- 12. Keener JD, Galatz LM, Teefey SA, et al. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015;97(2):89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim SH, Kim YH, Lee HR, Choi YE. Short-term effects of high-intensity laser therapy on frozen shoulder: a prospective randomized control study. Man Ther. 2015;20(6):751–757. [DOI] [PubMed] [Google Scholar]
- 14. Kim SJ, Lee SK, Kim SH, et al. Effect of cigarette smoking on the clinical outcomes of ACL reconstruction. J Bone Joint Surg Am. 2014;96(12):1007–1013. [DOI] [PubMed] [Google Scholar]
- 15. Kim YS, Kim SE, Bae SH, et al. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2073–2080. [DOI] [PubMed] [Google Scholar]
- 16. Kim YS, Lee HJ, Kim JH, Noh DY. When should we repair partial-thickness rotator cuff tears? Outcome comparison between immediate surgical repair versus delayed repair after 6-month period of nonsurgical treatment. Am J Sports Med. 2018;46(5):1091–1096. [DOI] [PubMed] [Google Scholar]
- 17. Kong BY, Cho M, Lee HR, Choi YE, Kim SH. Structural evolution of nonoperatively treated high-grade partial-thickness tears of the supraspinatus tendon. Am J Sports Med. 2018;46(1):79–86. [DOI] [PubMed] [Google Scholar]
- 18. Lafosse L, Reiland Y, Baier GP, Toussaint B, Jost B. Anterior and posterior instability of the long head of the biceps tendon in rotator cuff tears: a new classification based on arthroscopic observations. Arthroscopy. 2007;23(1):73–80. [DOI] [PubMed] [Google Scholar]
- 19. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 20. Lo IK, Denkers MR, More KD, et al. Partial-thickness rotator cuff tears: clinical and imaging outcomes and prognostic factors of successful nonoperative treatment. Open Access J Sports Med. 2018;9:191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91(8):1898–1906. [DOI] [PubMed] [Google Scholar]
- 22. Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J. 2013;95-B(7):935–941. [DOI] [PubMed] [Google Scholar]
- 23. Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5(1):1–11. [DOI] [PubMed] [Google Scholar]
- 24. Nove-Josserand L, Edwards TB, O’Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res. 2005;433:90–96. [DOI] [PubMed] [Google Scholar]
- 25. Oh JH, Kim JY, Lee HK, Choi JA. Classification and clinical significance of acromial spur in rotator cuff tear: heel-type spur and rotator cuff tear. Clin Orthop Relat Res. 2010;468(6):1542–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rhee SM, Youn SM, Ko YW, et al. Retracted rotator cuff repairs heal with disorganised fibrogenesis without affecting biomechanical properties: a comparative animal model study. Arthroscopy. 2021;37(12):3423–3431. [DOI] [PubMed] [Google Scholar]
- 27. Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39(4):710–714. [DOI] [PubMed] [Google Scholar]
- 28. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. [DOI] [PubMed] [Google Scholar]
- 29. Tsuchiya S, Davison EM, Rashid MS, et al. Determining the rate of full-thickness progression in partial-thickness rotator cuff tears: a systematic review. J Shoulder Elbow Surg. 2021;30(2):449–455. [DOI] [PubMed] [Google Scholar]
- 30. Wolff AB, Sethi P, Sutton KM, et al. Partial-thickness rotator cuff tears. J Am Acad Orthop Surg. 2006;14(13):715–725. [DOI] [PubMed] [Google Scholar]
- 31. Yamaguchi K, Tetro AM, Blam O, et al. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. [DOI] [PubMed] [Google Scholar]
- 32. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. [DOI] [PubMed] [Google Scholar]
- 33. Yamamoto N, Mineta M, Kawakami J, Sano H, Itoi E. Risk factors for tear progression in symptomatic rotator cuff tears: a prospective study of 174 shoulders. Am J Sports Med. 2017;45(11):2524–2531. [DOI] [PubMed] [Google Scholar]
- 34. Yamanaka K, Matsumoto T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin Orthop Relat Res. 1994;304:68–73. [PubMed] [Google Scholar]