Abstract
Introduction
Plasmodium knowlesi malaria is a zoonotic mosquito-borne disease with complex epidemiology. According to the WHO, the prevention and control of vector-borne diseases require community participation to increase coherence between malaria interventions and sustainable public health programmes. We describe a participatory research (PR) design for a study aimed at exploring the key anthropological drivers of and barriers to zoonotic malaria preventive behaviour among communities exposed to P. knowlesi infection in Malaysia. Participatory approaches can facilitate policymakers in designing future zoonotic malaria control programmes by investigating community perspectives and concerns about zoonotic malaria in a local context.
Methods and analysis
The PR will be conducted over a period of 12 months, from March 2022 to March 2023, among adults (>18 years old) who are permanent residents in a rural village exposed to P. knowlesi malaria in Sabah, Malaysia. We will select patients who were diagnosed with P. knowlesi infection from January to December 2021 for focus group discussions (FGDs), as they can provide perspectives on the disease from the point of view of those previously diagnosed with infection. In-depth interviews (IDIs) with people of importance in the community, such as village heads, will also be conducted. Both FGDs and IDIs will be conducted from March 2022 until June 2022. Concurrently, a photovoice with adults over 18 years old who reside in the community will be conducted. The target sample sizes for FGDs, IDIs and photovoice are 6–8, 12 and 10–15 participants, respectively. We will use a study framework as a theoretical lens to guide the exploration of the beliefs, social contexts, barriers and drivers surrounding zoonotic malaria preventive behaviour.
Ethics and dissemination
This study has been approved by the Medical Research and Ethics Committee Ministry of Health Malaysia (NMRR ID-21-01980-JEH) and the Research and Innovation Secretariat, Faculty of Medicine, Universiti Kebangsaan Malaysia (FF-2021-462). All participants will provide consent prior to participation. The results will be reported in international peer-reviewed journals and presented at conferences and on other platforms.
Keywords: QUALITATIVE RESEARCH, INFECTIOUS DISEASES, Epidemiology, SOCIAL MEDICINE, Tropical medicine, Public health
Strengths and limitations of this study
The study will use a participatory approach to explore the challenges facing communities practising preventive behaviour against zoonotic malaria in their local settings.
The participatory approach protocol is geared toward conducting a research process with adults >18 years old in communities exposed to Plasmodium knowlesi malaria in Sabah, Malaysia to explore their perspectives on malaria and facilitate policymakers in designing future zoonotic malaria control programmes.
The participatory research method will use a theoretical framework that has been generated from expert consensus.
Qualitative studies are difficult to replicate in different settings and the results may not be relevant to other communities and larger populations.
The study is time-consuming and continuous engagement is needed with all community members in order to build trust with researchers.
Introduction
In 2020, the WHO included Plasmodium knowlesi malaria in its World Malaria Report for the first time.1 Since the first report of P. knowlesi cases in Kapit, Sarawak, Malaysia in 2004, the parasite has been reported infecting people in other countries throughout the South-East Asia region.2 3 The increasing incidence of P. knowlesi malaria among humans is a possible public health threat in the future.3 The highest number of P. knowlesi cases in humans occur in Sabah and Sarawak states, Malaysian Borneo.4 Despite positive progress towards achieving elimination of human malaria in Malaysia, the increasing incidence of P. knowlesi requires the application of interim strategies to reduce its transmission.3 The threat of zoonotic malaria infection has increased dramatically, and thus it is critical to revisit current malaria control strategies and design interventions specific to zoonotic malaria.3
In Sabah state, cases of P. knowlesi malaria infection increased from 100 cases per year in the year 2000 to 1325 cases in 2014.4 In 2018, there were 4131 reported P. knowlesi cases throughout Malaysia, with the highest incidence rate of 0.13 cases per 1000 population.4 Malaysia reported its last indigenous human malaria cases in 2017, with only 85 cases.4 P. knowlesi malaria cases were commonly diagnosed in adult men and persons who performed forest-related work.5 While majority of cases were uncomplicated, fatalities were reported in patients as young as 31 years old.6 Furthermore, the detection of asymptomatic cases of P. knowlesi malaria in human populations, including in children and within families, suggests potential target populations for interventions.3 7
Malaria generally affects poor communities with low levels of education and limited access to health services.1 Individuals who may come into contact with macaques and Anopheles mosquitoes are at risk of P. knowlesi malaria.2–10 Ecological changes due to deforestation and other anthropogenic activities increase the risk of zoonotic malaria.8 Zoonotic spillovers expose communities living in rural and semirural areas to P. knowlesi malaria infection due to the destruction of the natural hosts’ habitat. Macaque monkeys move farther from logging activities and favour human settlements.9 In addition, Anopheles mosquito vectors from the Leucospyrus group prefer to breed in muddy ground pools, swamp water and water pockets.10 Vectors may also breed in sites like bamboo stumps, tins and other artificial containers.10 The potential impact of this zoonotic spillover into vulnerable communities requires interim strategies and multisectoral approaches for its prevention and control.7 11
In 1961, Malaysia launched its Malaria Eradication Program.12 Various vector control measures were introduced including indoor residual spraying and the distribution of insecticide-treated bednets (ITNs).12 The provision of free malaria tools has reduced human malaria cases by sevenfold over 30 years.4 Zoonotic malaria, however, may not be controlled to the same degree as human-restricted malaria due to the different factors that control its transmission.5 Exacerbating this problem, persuading the local populations to adopt different control measures for what they perceive as the same problem is difficult. In Indonesia, for example, zoonotic malaria-specific preventive measures such as protective clothing and bednets were perceived as ‘uncomfortable’ by community members.13 Among the indigenous tribal people of Peninsular Malaysia, there is a belief that malaria has a supernatural origin, causing the community to perceive zoonotic malaria differently.14 Further research that explores the social context and human-related factors that contribute to disease transmission is warranted.5
Malaria control strategy: social context and human behaviour
Based on the United Nations Development Programme (UNDP)/World Bank/WHO Special Programme for Research and Training in Tropical Diseases, understanding the behaviour of members of a community and its social contexts can inform preventive measures.15 Quantitative surveys often fail to account for the underlying causes of human behaviour that lead to exposure to health risks.15 16 Furthermore, social contexts such as lifestyle, sociocultural belief, economic factors, and behavioural factors can influence malaria exposure and the usage of preventive measures.3 15–17 Social gatherings and other activities that are performed before bedtime can increase the risk of mosquito bites.18–20 Furthermore, ITNs are not effective when communities do not use them throughout the night.19 P. knowlesi vectors are typically exophagic, exophilic and bite early during the night-time, thus indoor-based interventions are unlikely to provide sufficient protection.10 Recently, mosquitoes of the Umbrosus group were found to bite early (from 11:00 in the afternoon), thus increasing the risk to communities performing daytime activities.20 In addition, cultural and economic activities also affect the acceptance and usage of malaria preventive measures.5 Farming communities and agricultural sector workers in oil palm farm and rubber estates were non-compliant with preventive measures due to various factors such as inconvenience and low perceive threat.5 13 These populations are at high risk of exposure to P. knowlesi malaria and thus complementary antimalarial strategies are required.3 7 21 For example, the One Health initiatives enforce ecological regulations that limit deforestation.21 P. knowlesi malaria control measures should integrate transdisciplinary approaches through identification of the risks of vector–human contact during outdoor activities.5 7 21
Numerous previous studies have been conducted on local beliefs concerning malaria in different regions of the world.14 22–24 In Indonesia, belief in a supernatural cause of malaria influences individuals to consume certain foods and to use pendants and jampi (magic). They apply these measures rather than implementing evidence-based antimalarial measures or seeking treatment at healthcare centres.13 Individuals seek treatment with traditional practitioners because of cost, and claim that these are more effective and reliable.13 25
Studies from Malaysia, Africa, Indonesia, India and the Philippines suggest that cultural and religious beliefs influence understandings of the causation of malaria.15 23–25 These beliefs impact on adherence to bednet usage and influence attitudes towards health-seeking behaviour. Understanding how communities perceive malaria and preventive measures such as bednet compliance can inform future P. knowlesi malaria control programmes.3 Along with understanding community behaviour, existing traditional knowledge should also be assessed prior to the design and implementation of P. knowlesi malaria control strategies.3 For a programme to be sustainable, the community should be involved in its planning, implementation and evaluation.11 15 Rather than focusing on the individual, community empowerment helps to increase the sustainability of interventions.11 As one of the pillars of a multisectoral approach to vector-borne disease control, community participation is a powerful component that is cost-effective and practical and facilitates behavioural changes that focus on enhanced vector control measures.11
The failures of ‘one-size-fits-all’ strategies for malaria control have prompted a re-evaluation of the importance of communities’ local priorities and needs.11 15 For example, participatory research (PR) approaches can be used to explore the influence of social context on the surrounding environment as well as community behaviours that increase exposure to zoonotic malaria. It is crucial to investigate and explore opportunities for improving malaria disease control. This will assist acceptance in local communities.
PR, also known as ‘community-based PR (CBPR)’ or ‘community research’, is a collaborative and iterative research design involving input from researchers and participants.26 It focuses on research processes that involve local people.27 28 The term is used interchangeably, thus throughout this protocol manuscript, the term CBPR will be used. Israel et al described CBPR as a constructivist and critical theoretical perspective that argues with positivist ideology.28 Through CBPR, the findings can facilitate improvements in health-related interventions and generate evidence-based practices.27 28 CBPR incorporates community perspectives and emphasises the direct engagement of local priorities.27 CBPR differs from participatory action research by shifting the emphasis from action to collaborative research activities.27 28
CBPR aims to produce knowledge through collaboration between researchers and research participants.27 28 CBPR embeds the practice of knowledge democracy by using multiple ways of exploring community knowledge through expressions such as local narratives and songs.27 This can lead to new insights regarding health research, and can act as a tool for exploring social activity in relation to social action and health equity.27 Greater sensitivity to communities involving listening to their voices can generate trust and build partnerships and relationships between researchers and participants.27 In CBPR studies, both quantitative and qualitative methods can be used.27 The advantage of CBPR is that researchers can conduct systematic inquiries with study participants. Often these are marginalised or disenfranchised communities, who are immediately affected by the ongoing issues.27 28
Characteristics of the community-based participatory approach
Discrete differences exist between CBPR and other research methodologies.27 CBPR democratises participant knowledge by instilling the belief that people exert a positive influence on their circumstances.27 CBPR reduces the gap between theory, research and practical recommendations.27 28 There are guidelines such as those described by Israel et al28; however, each research is unique in that it is dependent on local issues.27 For example, CBPR studies emphasise a ‘bottom-up’ approach by incorporating local knowledge in future planning and programme implementation.27 The co-learning process between researchers and participants facilitates reciprocal transfer of knowledge, skills and capacity.27 In contrast, other research designs often aim to generate knowledge from research without incorporating local priorities and perspectives. This oversight may result in inappropriate recommendations.27 28 CBPR also places an emphasis on the empowerment of community members as co-researchers, by allowing the sharing of information, decision-making and partnerships.27 CBPR is an alternative approach for empowering, engaging, and creating cohesive and sustainable vector control programmes addressing local issues.29 In the Philippines, through the Participatory Visual Method using photovoice methodology, researchers gained access to the live and social context of the communities through images captured by the participants.29 The images act as a powerful tool to inform policymakers on communities’ belief and preventive measures against malaria, through the eye of community members.29 Below we describe the methods that will be used and the analyses that will be conducted in this study.
Study perspective and health behaviour model
From a constructivist perspective, the meaning and experience of phenomena are socially constructed, for example, by social norms, beliefs and environment, rather than inherent within individuals.30 This paradigm emphasises the generation of understanding an issue ‘from the bottom-up’ approach.30 In CBPR studies, community involved in the research through their participation in addressing the research inquiry, through discussion of the data and interpretation of the findings. This process is valued and underpinned by the concept of critical consciousness31 and feminist theory.32 Through this ideology, the Brazilian educator, Paulo Freire, proposed the concept of education through collective dialogue with the oppressed and poor people.31 In feminist theory, participants are able to participate in the decision-making process through the power that arises from the voice of people who live within the issues.32
This study seeks to incorporate an understanding of sociocultural contexts and their structural conditions on malaria preventative behaviour among individuals and communities exposed to P. knowlesi malaria. Previous studies have shown that individuals and communities have their own native and sociocultural beliefs toward the disease and that influenced malaria preventive behaviour.13–15 In addition, there are also drivers of and barriers to malaria preventative behaviour in the communities.15 18 19 Participants in the study can provide local perspectives on their beliefs and preventive measures, and offer opinions for future improvement of methods and tools to deliver preventative messages.
Study framework
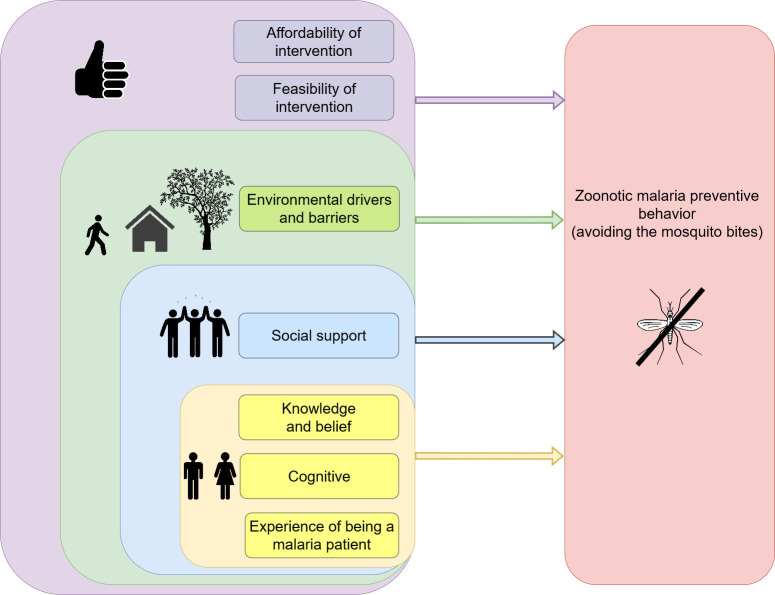
The study framework will integrate the ideation model,33 the explanatory model34 and Murdock et al’s illness causal model.35 This framework will act as a theoretical lens for knowledge processing in this study. Theory can convey a clear signpost of the study and provide guidance on how and what method will help to answer the research questions.30
The ideation model is a predictive model of behaviour change involving both individuals and communities.33 36 It is a socioecological approach involving the integration of communication and multiple behaviour theories.33 36 The model acts as a conceptual tool that can identify common psychosocial variables that may influence malaria-related behaviour.37–39 This framework identifies a set of psychosocial variables grouped into three domains: cognitive, social support and emotion.33 For example, cognitive variables or factors include the attitude towards the recommended preventive behaviour, perceived risk and self-efficacy to avoid malaria infection, while emotion could describe the feelings of fear towards malaria infection. Social support variables or factors embrace the community support and peer pressure to practice or avoid the recommended preventive behaviour.37–39
The explanatory model is a tool for medical and public health professionals to investigate cultural variations in illness experiences, diagnosis and treatment.34 The model aids in developing rapid assessments through direct communication with patients, family members and relatives.16 34 The data produced can facilitate the translation of interventions that consider the local perceptions of illness, circumstances that result in a risk pattern and community structures that might support the intervention.16 34
Murdock et al’s illness causal model conceptualised the local perception of causation of disease.35 According to this theory, it is important to distinguish between beliefs about natural and supernatural causes of illness, which are diverse worldwide, as they influence how disease treatment and behaviour are perceived.35 40
Study aim
This study aims to explore the key anthropological drivers of and barriers to zoonotic malaria preventative behaviour among communities exposed to P. knowlesi malaria infection. This study will be conducted among adults (age >18 years old), including those with a history of P. knowlesi malaria infection and those who live in areas with a high incidence of the infection.
The study will address the primary research question: ‘According to adults (age >18 years old), including those with a history of this infection and who live in an area exposed to P. knowlesi malaria infection, how and why do their beliefs towards the disease, and social, cultural and environmental challenges influence zoonotic malaria preventive behaviour?’ In view of the fact that current vector control measures do not protect against Anopheles mosquito bites, we defined preventive behaviour as ‘avoidance of mosquito bites’. We will then translate the views of the communities into information for policymakers, thus addressing the second research question: ‘How can the views and concerns of these communities regarding zoonotic malaria infection inform future P. knowlesi malaria control programme?’
Methods and analysis
Study setting
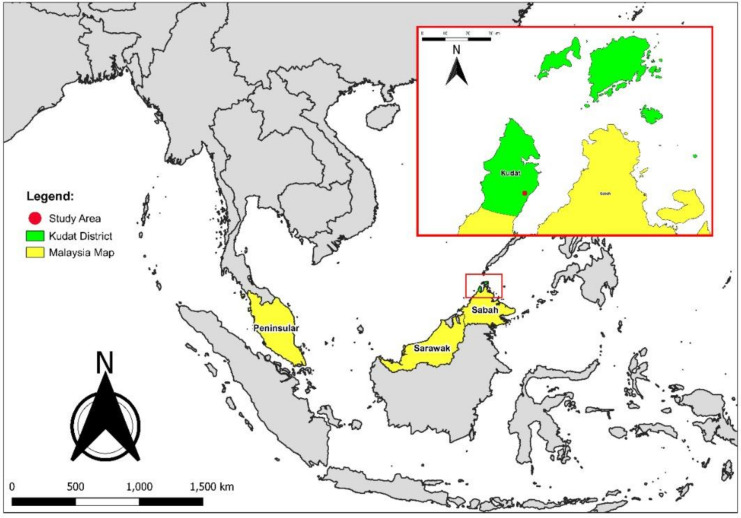
This study will be conducted in the highly P. knowlesi endemic state of Sabah, Malaysia.41 Sabah covers 73 904 km2, with an estimated population of 3.90 million in 2019.42 Geographically, Sabah is composed of a mix of mountainous regions, coastlines and tropical rainforests. In Sabah, Anopheles leucosphyrus group mosquitoes are the major vector for P. knowlesi malaria infection.43 A study by Cooper et al reported five districts in Sabah with a high incidence of P. knowlesi malaria: Ranau, Keningau, Tenom, Tambunan and Kota Marudu, which are located along the Crocker range.44 The present study will be conducted in the northern region of Sabah in Kudat region, the location of several recent studies on zoonotic malaria8 9 43 45 (figure 1). The incidence in Kudat district is estimated at 0.90–1.36 per 1000 population.44 The location was selected after obtaining a list of districts with village names from the Sabah State Health Department, within areas with high incidences of P. knowlesi in 2020.
Figure 1.
The study area.
Study participants
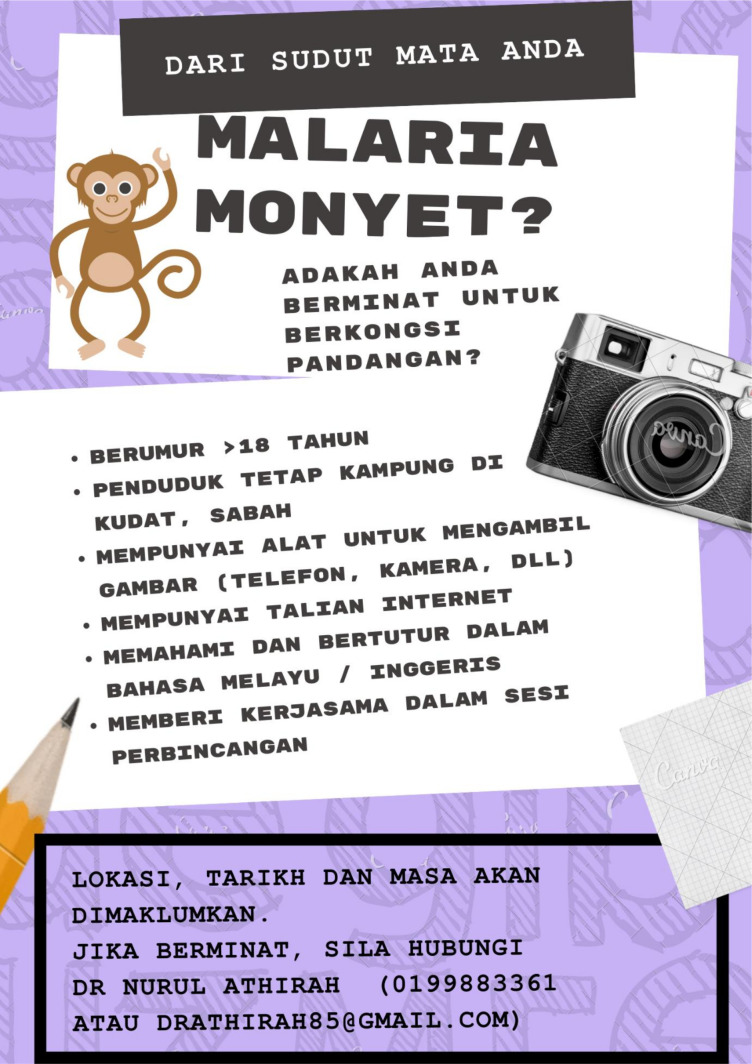
The study participants will be adult men and women (above 18 years old) who can provide informed consent prior to the focus group discussions (FGDs), in-depth interviews (IDIs) and photovoice. The study will include participants who are permanent residents of the village, are mobile, without known cognitive or mental health issues, and are able to answer questions in Malay or English language. Due to restrictions imposed by the current COVID-19 pandemic, participants with access to electronic communication tools will be preferred.46 47 We anticipate the recruitment of participants with access to electronic communication tools will cause bias in the study results. However, in view of the improved COVID-19 situation in Malaysia and the ability to conduct fieldwork with strict Standard Operating Procedures (SOPs), this bias may be minimised by conducting the study at the study sites and via face-to-face interviews. The sampling method for the FGDs will be purposive sampling among individuals who were previously diagnosed with P. knowlesi malaria infection between January 2021 and December 2021. Community leaders will be selected for IDIs. Subsequently, a snowballing technique will be used to recruit other information-rich individuals. For the photovoice, a recruitment pamphlet will be distributed in the village, and we will use purposive sampling to recruit the participants. Excluded from the study will be non-residents, people with known cognitive or mental health issues, and those who are unable to attend interviews or FGDs after two invites. All these methods will be conducted concurrently for 12 months from March 2022 to March 2023.
Sample size
For FGDs, 6–8 participants will be enrolled,48 while the sample size for IDIs may be up to 12 participants.49 Data will be collected until data saturation is reached, defined as when there is no new information collected from subsequent participants.48 49 Earlier studies using photovoice reported enrolling between 4 and 122 participants.50 We aim to recruit 10–15 participants.
Categorisation of participation
The gradation of participation in this study is informed by Arnstein’s ‘ladder of citizen participation’ categorisation.51 This ladder distinguishes three main participation categories: citizen power, tokenism and non-participation; and eight levels: manipulation, therapy, informing, consultation, placation, partnership, delegated power and client control.51 We will use tokenism in our study. During the FGDs, IDIs and photovoice, we will ensure that communication between researchers and participants allows them the opportunity to influence the discussion and analysis. However, those with power (eg, policymakers) will have power over decisions.51 For example, to ensure meaningful ‘tokenism’ between researchers and participants in photovoice, we will provide an introduction and training workshop prior to commencing the method. The workshop will ensure a safe working environment, and agreements will be reached between the researchers and participants upon the methodology.52 53 During the photovoice progress, we will regularly discuss the conditions for cooperation with the participants. The research questions will be shared with participants.53 We will communicate in a clear manner in the Malay language and tailor communication to the literacy and coping level of the participants. The participants will receive a ‘token’ for participating in the study. Participants will have the right to withdraw from the study at any point.
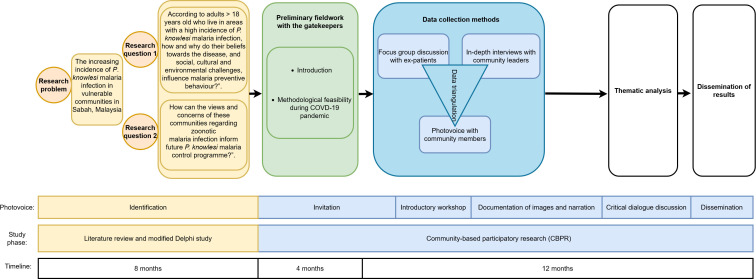
Study design
The study is a multimethod design using the CBPR methodology.27 This study will be conducted over a 12-month period. Rapport will be established with individuals so that topics can be freely discussed.27 The study will use FGD, IDI and the photovoice method, which offers the advantage of triangulating the data. Semistructured interview guides have been prepared and approved by the research supervisory and ethical committees. The views of all participants, who will be recruited in different methods, will be compared and interpreted to achieve data triangulation. The photovoice will raise their perspectives and concerns using an iterative and collaborative process.50 54 The researchers’ role will be to introduce the research aims and questions to the participants. In view of study using the CBPR methodology, the creation of discussion will be conducted through dialogues with participants (co-researchers).27 The dissemination of study findings with policymakers will either be conducted through exhibition (eg, at local townhall) or different platforms (eg, coloured book, peer-reviewed manuscript, conference presentations)53–55 (figure 2). However, due to the COVID-19 pandemic, research methods may be modified to accommodate social distancing requirements and other SOPs.
Figure 2.
The study flow chart.
Study phases
Phase 1: preparation
The first phase of the study is to conduct a systematic literature review to understand: (1) the behaviour or activities that expose humans to P. knowlesi malaria infection, and (2) how data on behaviour were collected in previous studies.5 The literature searched was from standard scientific databases. The article abstracts were screened and assessed by three researchers, and any disagreement on the quality of the studies was resolved by consensus of the coauthors.5 The Joanna Briggs Institute critical appraisal checklist was used to rate the quality of the studies. A grey literature search was also performed from the WHO website. It was found that the majority of the included studies were done quantitatively, limiting a deep understanding of human behaviour.5 Several factors such as socioeconomic status, beliefs, perceived threats, motivation and coping issues can influence communities’ malaria preventive behaviour.5 Future studies must consider using qualitative study designs in order to generate rich information and address how human behaviour can influence the exposure to zoonotic malaria.5 Furthermore, the importance of community perspective on P. knowlesi malaria control is critical to strategise specific P. knowlesi malaria control guidelines.5 7
The next step was to develop a research framework that would function as the theoretical lens for this study. The theoretical lens is the study’s assumptions that will guide the study methodology.30 Using the modified Delphi study, new themes were generated through the consensus of experts.56 The experts were selected based on the inclusion criteria as per the protocol.56 Twelve experts were selected based on (1) having more than 5 years of experience working or practising in any research institutions, having an administrative post in any organisation and conducting malaria research, (2) individuals who have published more than one study on malaria in peer-reviewed journals and (3) consented. This framework focused on factors that possibly influence malaria preventative behaviour in communities exposed to P. knowlesi malaria infection through the collective agreement among the expert panels56 (figure 3).
Figure 3.
The study framework.
The third stage will be selection of participants. A pamphlet using the Malay language was distributed in the village to recruit participants for photovoice (figure 4). The distribution was done after the meeting with the community leaders. Only those individuals who show interest and match our eligibility criteria will be recruited. The purposive and convenience sampling method will be used to avoid participants’ dropouts. The photovoice participants will attend a workshop introducing the study, discussing ethical considerations, distributing tasks and outlining responsibilities. Participation will continue throughout the study duration.55
Figure 4.
The photovoice recruitment pamphlet in the Malay language.
Phase 2: implementation of the study
The implementation of the study is as follows: FGDs and IDIs will be conducted with participants to answer the specific research questions. Participants will participate in discussions and undergo interviews using the interview guides. Data will be collected and analysed by the research team. The research team consists of epidemiologists, public health specialists, medical anthropologists, infectious disease experts and a postgraduate student. FGDs, IDIs and photovoice will be recorded, transcribed verbatim by the research team, and analysed using thematic analysis by Braun and Clarke approach.57
The FGDs and IDIs will be performed in a place familiar to the participants.58 The FGDs will start with a general question about what participants perceive about P. knowlesi malaria infection, explore their beliefs concerning illness causation, and how and why these beliefs influence their malaria preventive behaviour. Prompts will also be used to gather information and to generate richer data. The FGDs will be conducted for approximately 90 min, preferably without breaks.58 The session will continue until a clear pattern emerges and subsequent interviews do not produce new information.57 IDIs will be conducted individually using an interview guide. Potential key informants, such as people of influence in the community, such as the head of village and faith leaders,59 will be contacted by a formal letter, individually. A meeting has been arranged with this gatekeeper to build rapport and to request permission to conduct the study at the site.60
Interviews will be conducted using face-to-face sessions; however, electronic communication may be warranted depending on the COVID-19 situation. The duration of the interview will be approximately 60–90 min.57 58 The session will be written in fieldnotes and recorded, audio and verbally. As a means to maintain data trustworthiness, member-checking and external coding will be used to validate the data interpretation and coding.61
In photovoice, participants will take photographs (eg, using camera or smartphones), discuss them through the FGDs and select the photos that best reflect the community for future dissemination of study findings.62 63 Photovoice research team will work as closely as possible with the local structures and institutions to facilitate meaningful long-term participation.62 The goals, strategies, and limitations for social change will be clearly and realistically defined and communicated to avoid raising the expectations of participants.54 63 The photovoice participants will have specific rules, such as the requirement of consent before taking pictures of adults and avoiding pictures of children. A WhatsApp group will be created by the researchers through which the participants will be encouraged to share the photos. The photographs taken by the participants, which will be shared with policymakers, have value in that they provide the opportunity for virtual display when words are difficult to express their views.54 62 Previous research described participants shared around 9–182 photographs and suggests that participants take an average of 40–50 photos each.62 We will recommend 10 photos per participant. The photographs can be taken anywhere, such as the home, street, or other aspects of the participant’s environment, target actions, places, and situations.55 62 63 We will use the SHOWeD algorithm to reveal the participants' reflections of their photos.63 The narrative caption of the photos will reveal meaningful experiences that can improve awareness of relevant issues.63
Phase 3: dissemination
Due to the ongoing COVID-19 epidemic and resulting restrictions, we will look for opportunities to present the research findings on appropriate platforms. Thus, dissemination will not only be at the local townhall with the participants, but also through online research presentations, various scientific presentations and a book.55 The book will include coloured photos and narratives from participants that illustrate their perspectives on local beliefs, and the drivers and barriers to malaria preventive behaviour. All the photovoice participants will be given an opportunity to review the initial draft. Hardcopies will be disseminated to policymakers (for example, the Sabah State Health Department and Ministry of Health Malaysia).
Supervisory committee
The supervisory committee will monitor the study process, from initiation to the end of the study. They will provide advice on the content of the study and its appropriateness with respect to the study aims. Monthly meetings are planned and members of the supervisory committee will be asked for further input, if needed. Researchers and stakeholders will be a part of this supervisory committee.
Patient and public involvement
Participants were not directly involved in the study design. The FGD and IDI participants will only act as research participants. Meanwhile, the photovoice participants will conduct the photography session, give inputs in analysis and participate in the exhibition. The researchers will conduct the final reporting and dissemination plan of this research.
Data analysis
Data will be collected by the researcher and research assistants (RAs), who are proficient in the local language. The RAs will be trained by the research team and will be the observers, note-takers and translators. The RAs will assist in transcribing the data from the local language into English. We will use the qualitative software program ATLAS.ti V.9 (ATLAS.ti Scientific Software Development), to assist with data handling, storing and creating networks images, quotations, codes and themes, in a systematic way.
Thematic analysis
Thematic analysis by Braun and Clarke will be used to generate codes and themes from the data.57 Data familiarisation will be through re-reading the verbatim and re-viewing the photographs.57 Familiarisation is a time-consuming process which includes the phase of immersion, where researchers engage deeply with the data to find a richer meaning and generate patterns from the data.57 In addition, this phase includes critical engagement and note-taking of thoughts related to the data.57 Then, initial codes will be generated systematically across the whole data set.57 Themes will be identified within codes, and these themes will be named and defined.57 Prior to the write-up, a review of the themes will be conducted.57
Rigour and data trustworthiness
Rigour is defined as the demonstration of integrity and competence within a study.64 Data trustworthiness will be gained through feedback from participants (credibility, dependability), checks by participants and the research team (confirmability), and a thorough description of data collection and analysis (transferability).61 Member-checking will be performed after all sessions of the chosen methods are completed.61 For example, after an IDI session is completed, a summary will be given to participants to confirm or comment on the researcher’s understanding throughout the session, and to maintain data accuracy. It will provide the opportunity to modify errors or wrong interpretations.61 External coding will increase the validity of the data.61 The coding process will be individually applied to the IDIs, FGDs and photovoice data. The data will be triangulated to answer the research questions, as well as by generating new themes.57
Reflexivity of the researcher
Reflexivity and subjectivity are important characteristics of qualitative studies using thematic analyses.57 The CBPR method encourages a self-reflective, engaged and self-critical role among researchers.27 The primary investigator (PI) in this study has 10 years of experience of working as a primary care medical practitioner in a rural district in Sabah, Malaysia. The PI will be the ‘facilitator’ or ‘moderator’ to guide the discussion between participants.30
Study outcome
Community participation in research is critical for developing information, education, and communication tools to produce and promote public health programmes.27 The views and reflections of the community in the study are relevant for culturally sensitive and effective future P. knowlesi malaria intervention programmes. Furthermore, it could result in a more sustainable malaria intervention.11 The outcome of this study will be used to inform the development of community-friendly and appropriate intervention tools. This approach is viewed as an essential component of ethical good practice in research.27 It brings the communities’ perspective and voices a way forward, through engagement in research and health equity and increasing the chances of success of an intervention.11 27 Intervention can be in the form of education, reflection and discussion.27
Study status
The preliminary study was conducted from 30 December 2021 to 28 February 2022. As part of the participatory approach, the gatekeepers (the healthcare workers and community leaders in the study sites) were met to introduce the study and discuss the methodological feasibility and appropriateness of conducting the study during the COVID-19 pandemic. In view of COVID-19 prevention, only fully vaccinated community members will be allowed to participate in the study and all participants need to adhere to COVID-19 SOPs such as wearing masks and social distancing. The results of this preliminary study will be disseminated in future peer-reviewed manuscript.
Ethics and dissemination
This study has been approved by the Medical Research and Ethics Committee, Ministry of Health Malaysia (NMRR ID-21-01980-JEH), and the Research and Innovation Secretariat, Faculty of Medicine, Universiti Kebangsaan Malaysia (FF-2021-462). All the participants will provide consent prior to participation. Participants are allowed to withdraw at any point during the study. The results will be disseminated in various academic (eg, conferences, journals) and non-academic (eg, town hall meetings) platforms.
Discussion
Efforts have been made to assess how CBPR can be an effective research methodology for P. knowlesi malaria intervention. CBPR has possible important implications for the sustainability and appropriateness of P. knowlesi malaria interventions. Many previous programmes have failed because of a lack of genuine community participation.11 CBPR provides insights from local people to improve the quality of research, ensure validity and improve public health intervention.27 The recognition of community perspectives on the aetiology of illness, drivers of and barriers to preventive measures can provide a fresh perspective on research issues, and helps to facilitate intervention tailored to local conditions.27 The engagement of communities has improved communication tools for the promotion of effective and sustainable interventions, enhanced their relevance and feasibility, and improved data utilisation by all stakeholders.11 27 The use of CBPR in health research promises far-reaching changes in short-term and long-term outcomes.27 We hope to provide empirical evidence to help develop future zoonotic malaria control programmes. Community engagement and feedback in our research will increase the reliability and validity of the study through local knowledge and theory based on experiences. Changing the relationship between researchers and those who participate in research involves a transformation of power and views of the issues that should promote a more flexible and reflexive process among researchers.27 Participants will be empowered when their views and voices are heard.54 Future studies and collaborations that combine CBPR methodology and emphasise on community participation will reinforce additional knowledge and appropriate behaviour changes.27
Study limitations
It is possible that we may encounter a lack of trust among community members with the study, due to the limitation of time and space to engage with the whole community members due to the current COVID-19 pandemic. We will attempt to minimise this by establishing trust through early communication and engagement with the head of the villages. Community members may be sceptical about participating in the study in case their opinions are considered invalid, thus a poor response rate in certain phases of this study may be encountered. A qualitative study is not a generalisable design but has the potential to develop an in-depth understanding of the community from a small number of participants.30 Due to differences in overall philosophy, assumptions, beliefs, decision-making and values, conflicts can arise between study members and different organisations.
Supplementary Material
Acknowledgments
The writing of this protocol was made possible by input from various experts. For their positive and constructive critiques, we would like to thank Professor Douglas Storey and Dr April Monroe from the John Hopkins Center for Communication Studies; Dr Gill Black from the Sustainable Livelihoods Foundation (SLF); Dr Jeffrey Hii from the Malaria Consortium, Mahidol University, Thailand; Professor Kalsom Kayat from Universiti Utara Malaysia; Professor Lenore Manderson from the School of Public Health, University of the Witwatersrand and the Monkeybar project. We are truly grateful to both Dr Janet Cox-Singh from the University of St Andrews and Dr Cyrus Daneshvar from Plymouth Hospitals NHS for their sharing of expert advice and experiences during their early years conducting malaria studies in Sarawak, Malaysia.
Footnotes
Contributors: NAN was the principal investigator responsible for the design of the study and drafting the manuscript. MRH was the coordinating investigator. RC, MSJ, RH, KA and MRH contributed equally to the content of the study protocol with important intellectual revisions. All authors read and approved the final protocol manuscript.
Funding: This study received funding from Universiti Kebangsaan Malaysia (grant FF-2021-462).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.World Health Organization . World malaria report: 20 years of global progress and challenges. Geneva: World Health Organization, 2020. ISBN: 978-92-4-001579-1. https://www.who.int/publications/i/item/9789240015791 [Google Scholar]
- 2.Ahmed MA, Cox-Singh J. Plasmodium knowlesi - an emerging pathogen. ISBT Sci Ser 2015;10:134–40. 10.1111/voxs.12115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naserrudin NA, Hod R, Jeffree MS, et al. The Emerging Threat of Plasmodium knowlesi Malaria Infection: A Concept Paper on the Vulnerable Factors in Human. Int J Environ Res Public Health 2022;19:4419. 10.3390/ijerph19074419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chin AZ, Maluda MCM, Jelip J, et al. Malaria elimination in Malaysia and the rising threat of Plasmodium knowlesi. J Physiol Anthropol 2020;39:1–9. 10.1186/s40101-020-00247-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naserrudin NA, Hod R, Jeffree MS, et al. The Role of Human Behavior in Plasmodium knowlesi Malaria Infection: A Systematic Review. Int J Environ Res Public Health 2022;19:3675. 10.3390/ijerph19063675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajahram GS, Cooper DJ, William T, et al. Deaths from Plasmodium knowlesi malaria: case series and systematic review. Clin Infect Dis 2019;69:1703–11. 10.1093/cid/ciz011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naserrudin NA, Monroe A, Culleton R, et al. Reimagining zoonotic malaria control in communities exposed to Plasmodium knowlesi infection. J Physiol Anthropol 2022;41:14. 10.1186/s40101-022-00288-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fornace KM, Brock PM, Abidin TR, et al. Environmental risk factors and exposure to the zoonotic malaria parasite Plasmodium knowlesi across Northern Sabah, Malaysia: a population-based cross-sectional survey. Lancet Planet Health 2019;3:e179–86. 10.1016/S2542-5196(19)30045-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stark DJ, Fornace KM, Brock PM, et al. Long-Tailed macaque response to deforestation in a Plasmodium knowlesi-Endemic area. Ecohealth 2019;16:638–46. 10.1007/s10393-019-01403-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vythilingam I, Chua TH, Liew JWK, et al. The vectors of Plasmodium knowlesi and other simian malarias Southeast Asia: challenges in malaria elimination. Adv Parasitol 2021;113:131–89. 10.1016/bs.apar.2021.08.005 [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO) . Multisectoral approach to the prevention and control of vector-borne diseases: a conceptual framework, 2020. World Health Organization. Available: https://apps.who.int/iris/handle/10665/331861 [Accessed 30 Oct 2021].
- 12.Mak JW, Jegathesan M, Lim PK. Epidemiology and control of malaria in Malaysia. Southeast Asian J Trop Med Public Health 1992;23:572–7. [PubMed] [Google Scholar]
- 13.Ekawati LL, Johnson KC, Jacobson JO, et al. Defining malaria risks among forest workers in Aceh, Indonesia: a formative assessment. Malar J 2020;19:441. 10.1186/s12936-020-03511-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munajat MB, Rahim MAFA, Wahid W, et al. Perceptions and prevention practices on malaria among the Indigenous Orang Asli community in Kelantan, Peninsular Malaysia. Malar J 2021;20:202. 10.1186/s12936-021-03741-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heggenhougen HK, Hackethal V, Vivek P. The behavioural and social aspects of malaria and its control : an introduction and annotated biliography. UNDP/World Health Organization Special Programme for Research and Training in Tropical Diseases, 2003. Available: https://apps.who.int/iris/handle/10665/42504 [Accessed 1 Nov 2021].
- 16.Manderson L, Cartwright E, Hardon AE. The Routledge Handbook of medical anthropology. Milton Park, Abingdon, UK: Routledge, 2016. [Google Scholar]
- 17.Finda MF, Moshi IR, Monroe A, et al. Linking human behaviours and malaria vector biting risk in south-eastern Tanzania. PLoS One 2019;14:1–23. 10.1371/journal.pone.0217414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monroe A, Olapeju B, Moore S, et al. Improving malaria control by understanding human behaviour. Bull World Health Organ 2021;99:837–9. 10.2471/BLT.20.285369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monroe A, Asamoah O, Lam Y, et al. Outdoor-sleeping and other night-time activities in northern Ghana: implications for residual transmission and malaria prevention. Malar J 2015;14:35. 10.1186/s12936-015-0543-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Ang JX, Yaman K, Kadir KA, et al. New vectors that are early feeders for Plasmodium knowlesi and other simian malaria parasites in Sarawak, Malaysian Borneo. Sci Rep 2021;11:7739. 10.1038/s41598-021-86107-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott J. Proposed Integrated Control of Zoonotic Plasmodium knowlesi in Southeast Asia Using Themes of One Health. Trop Med Infect Dis 2020;5:175. 10.3390/tropicalmed5040175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamat VR. "I thought it was only ordinary fever!" cultural knowledge and the micropolitics of therapy seeking for childhood febrile illness in Tanzania. Soc Sci Med 2006;62:2945–59. 10.1016/j.socscimed.2005.11.042 [DOI] [PubMed] [Google Scholar]
- 23.Taek MM, Banilodu L, Neonbasu G, et al. Ethnomedicine of Tetun ethnic people in West Timor Indonesia; philosophy and practice in the treatment of malaria. Integr Med Res 2019;8:139–44. 10.1016/j.imr.2019.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Espino F, Manderson L, Acuin C, et al. Perceptions of malaria in a low endemic area in the Philippines: transmission and prevention of disease. Acta Trop 1997;63:221–39. 10.1016/s0001-706x(96)00623-7 [DOI] [PubMed] [Google Scholar]
- 25.Sundararajan R, Kalkonde Y, Gokhale C, et al. Barriers to malaria control among marginalized tribal communities: a qualitative study. PLoS One 2013;8:e81966. 10.1371/journal.pone.0081966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cornwall A, Jewkes R, Rachel J. What is participatory research? Soc Sci Med 1995;41:1667–74. 10.1016/0277-9536(95)00127-s [DOI] [PubMed] [Google Scholar]
- 27.Wallerstein N, Duran B, Oetzel JG. Community-based participatory research for health : advancing social and health equity. San Francisco, CA: Jossey-Bass, a Wiley Brand, 2018. [Google Scholar]
- 28.Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173–202. 10.1146/annurev.publhealth.19.1.173 [DOI] [PubMed] [Google Scholar]
- 29.Iskander D. Re-imaging malaria in the Philippines: how photovoice can help to re-imagine malaria. Malar J 2015;14:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Creswell JW, Plano-Clark VL. Designing and conducting mixed methds research. 3rd ed. Thousand Oaks, CA: SAGE, 2018. [Google Scholar]
- 31.Freire P. Education for critical consciousness. In: Continuum. 1. New York Seabury, 1973. https://www.scirp.org/reference/ReferencesPapers.aspx?ReferenceID=1055706 [Google Scholar]
- 32.Edith SD. Everyday world as problematic a feminist sociology, 1987. Boston northeastern university press. Available: https://www.scirp.org/reference/ReferencesPapers.aspx?ReferenceID=1010569 [Accessed 15 Dec 2021].
- 33.Health Communication Capacity Collaborative (HC3) . Ideation - An HC3 Research Primer. Balt. HC3 John Hopkins Cent. Commun. Program, 2014. Available: https://healthcommcapacity.org/hc3resources/ideation-hc3-research-primer/ [Accessed 1 Sep 2021].
- 34.Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Soc Sci Med 1978;12:85–93. 10.1016/0160-7987(78)90014-5 [DOI] [PubMed] [Google Scholar]
- 35.Murdock GP, Wilson SF, Frederick V. World distribution of theories of illness. Ethnology 1978;17:449–70. [Google Scholar]
- 36.Kincaid DL. Social networks, ideation, and contraceptive behavior in Bangladesh: a longitudinal analysis. Soc Sci Med 2000;50:215–31. 10.1016/S0277-9536(99)00276-2 [DOI] [PubMed] [Google Scholar]
- 37.Storey JD, Babalola SO, Ricotta EE, et al. Associations between ideational variables and bed net use in Madagascar, Mali, and Nigeria. BMC Public Health 2018;18:484. 10.1186/s12889-018-5372-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Do M, Babalola S, Awantang G, et al. Associations between malaria-related ideational factors and care-seeking behavior for fever among children under five in Mali, Nigeria, and Madagascar. PLoS One 2018;13:e0191079. 10.1371/journal.pone.0191079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olapeju B, Adams C, Wilson S, et al. Malaria care-seeking and treatment ideation among gold miners in Guyana. Malar J 2022;21:29. 10.1186/s12936-022-04045-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kahissay MH, Fenta TG, Boon H. Beliefs and perception of ill-health causation: a socio-cultural qualitative study in rural North-Eastern Ethiopia. BMC Public Health 2017;17:124. 10.1186/s12889-017-4052-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abeyasinghe R. Outcomes from the evidence review group on Plasmodium knowlesi, 2017. Available: https://www.who.int/malaria/mpac/mpac-mar2017-plasmodium-knowlesi-presentation.pdf [Accessed 30 Sep 2021].
- 42.Department of Statistics Malaysia . Department of statistics Malaysia press release: current population estimates, Malaysia, 2018-2019, 2019. Available: https://www.dosm.gov.my [Accessed 15 Sep 2021].
- 43.Chua TH, Manin BO, Vythilingam I, et al. Effect of different habitat types on abundance and biting times of Anopheles balabacensis Baisas (Diptera: Culicidae) in Kudat district of Sabah, Malaysia. Parasit Vectors 2019;12:364. 10.1186/s13071-019-3627-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooper DJ, Rajahram GS, William T. Plasmodium knowlesi Malaria in Sabah, Malaysia, 2015 – 2017 : ongoing increase in incidence despite near- elimination of the human-only Plasmodium species 2020;70:2015–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown R, Chua TH, Fornace K, et al. Human exposure to zoonotic malaria vectors in village, farm and forest habitats in Sabah, Malaysian Borneo. PLoS Negl Trop Dis 2020;14:1–18. 10.1371/journal.pntd.0008617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malka M. Photovoice as a creative coping tool with the COVID-19 crisis in practical training seminar for social work students. Qual Soc Work 2021;20:544–52. 10.1177/1473325020973309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dodds S, Hess AC. Adapting research methodology during COVID-19: lessons for transformative service research. J Serv Manag 2020;32:203–17. [Google Scholar]
- 48.Guest G, Namey E, McKenna K. How many focus groups are enough? building an evidence base for Nonprobability sample sizes. Field Methods 2016;29:3–22. [Google Scholar]
- 49.Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS One 2020;15:1–17. 10.1371/journal.pone.0232076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hergenrather KC, Rhodes SD, Cowan CA, et al. Photovoice as community-based participatory research: a qualitative review. Am J Health Behav 2009;33:686–98. 10.5993/ajhb.33.6.6 [DOI] [PubMed] [Google Scholar]
- 51.Arnstein SR. A ladder of citizen participation. J Am Plan Assoc 1969;35:216–24. [Google Scholar]
- 52.Wang C, Burris MA. Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav 1997;24:369–87. 10.1177/109019819702400309 [DOI] [PubMed] [Google Scholar]
- 53.Catalani C, Minkler M. Photovoice: a review of the literature in health and public health. Health Educ Behav 2010;37:424–51. 10.1177/1090198109342084 [DOI] [PubMed] [Google Scholar]
- 54.Budig K, Diez J, Conde P, et al. Photovoice and empowerment: evaluating the transformative potential of a participatory action research project. BMC Public Health 2018;18:1–9. 10.1186/s12889-018-5335-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Black GF, Davies A, Iskander D, et al. Reflections on the ethics of participatory visual methods to engage communities in global health research. Glob Bioeth 2018;29:22–38. 10.1080/11287462.2017.1415722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naserrudin NA, Hod R, Jeffree MS, et al. Expert Consensus on a Proposed Study Framework to Explore Factors Influencing Plasmodium knowlesi Malaria Preventive Behavior: A Modified Delphi Method Protocol. Int J Environ Res Public Health 2022;19:4141. 4141. 10.3390/ijerph19074141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Braun V, Clarke V. Thematic analysis: a practical guide, 2021. Available: https://books.google.com.my/books?id=mToqEAAAQBAJ&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false [Accessed 10 Sep 2021].
- 58.Khan M, Manderson L. Focus groups in tropical diseases research. Health Policy Plan 1992;7:56–66. [Google Scholar]
- 59.Marshall MN. The key informant technique. Fam Pract 1996;13:92–7. 10.1093/fampra/13.1.92 [DOI] [PubMed] [Google Scholar]
- 60.McAreavey R. Das C. a delicate balancing act: negotiating with gatekeepers for ethical research when researching minority communities. Int J Qual methods 2013;12:113–31. [Google Scholar]
- 61.Lincoln YS, Guba EG. Naturalistic inquiry. Newbury park, CA: SAGE, 1985. [Google Scholar]
- 62.Nykiforuk CIJ, Vallianatos H, Nieuwendyk LM. Photovoice as a method for revealing community perceptions of the built and social environment. Int J Qual Methods 2011;10:103. 10.1177/160940691101000201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Latz A O. Photovoice research in education and beyond: a practical guide from theory and exhibition. New York, NY: Routledge, 2017. [Google Scholar]
- 64.Fereday J, Muir-Cochrane E, Adelaide N. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80–92. 10.1177/160940690600500107 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.