Abstract
Background
Acinetobacter baumannii infections cause high morbidity and mortality in intensive care unit (ICU) patients. However, there are limited data on the changes of long-term epidemiology of imipenem resistance in A. baumannii bacteremia among pediatric ICU (PICU) patients.
Methods
A retrospective review was performed on patients with A. baumannii bacteremia in PICU of a tertiary teaching hospital from 2000 to 2016. Antimicrobial susceptibility tests, multilocus sequence typing (MLST), and polymerase chain reaction for antimicrobial resistance genes were performed for available isolates.
Results
A. baumannii bacteremia occurred in 27 patients; imipenem-sensitive A. baumannii (ISAB, n = 10, 37%) and imipenem-resistant A. baumannii (IRAB, n = 17, 63%). There was a clear shift in the antibiogram of A. baumannii during the study period. From 2000 to 2003, all isolates were ISAB (n = 6). From 2005 to 2008, both IRAB (n = 5) and ISAB (n = 4) were isolated. However, from 2009, all isolates were IRAB (n = 12). Ten isolates were available for additional test and confirmed as IRAB. MLST analysis showed that among 10 isolates, sequence type 138 was predominant (n = 7). All 10 isolates were positive for OXA-23-like and OXA-51-like carbapenemase. Of 27 bacteremia patients, 11 were male (41%), the median age at bacteremia onset was 5.2 years (range, 0–18.6 years). In 33% (9/27) of patients, A. baumannii was isolated from tracheal aspirate prior to development of bacteremia (median, 8 days; range, 5–124 days). The overall case-fatality rate was 63% (17/27) within 28 days. There was no statistical difference in the case fatality rate between ISAB and IRAB groups (50% vs. 71%; P = 0.422).
Conclusion
IRAB bacteremia causes serious threat in patients in PICU. Proactive infection control measures and antimicrobial stewardship are crucial for managing IRAB infection in PICU.
Keywords: Pediatric Intensive Care Units, Acinetobacter baumannii, Bacteremia
Graphical Abstract
INTRODUCTION
Improved medical care and invasive procedures for high-risk pediatric intensive care unit (PICU) patients have led to a longer duration of survival and prolonged hospitalization. However, prolonged hospitalization results in a higher probability of healthcare-associated infection. Common bacterial pathogens in pediatric healthcare-associated infection are Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, coagulase negative staphylococci, Escherichia coli, and Acinetobacter spp.1,2,3
Acinetobacter baumannii is an aerobic, Gram-negative bacterium associated with high morbidity and mortality in clinical settings. A. baumannii infection may lead to high health-care costs and prolonged hospitalization. The most common clinical manifestations are ventilator-associated pneumonia and bacteremia.4 Furthermore, the imipenem resistance rate of A. baumannii species is increasing worldwide.5,6
However, there are limited data on long-term epidemiology of A. baumannii bacteremia among PICU patients.7,8,9 In this study, we analyzed the epidemiology of bacteremia caused by A. baumannii infection in PICU patients and molecular analysis of isolated bacteria.
METHODS
Collection of patient’s information
A retrospective chart review was performed on pediatric patients < 19 years old who developed bacteremia caused by A. baumannii from January 2000 to December 2016 in the PICU at Samsung Medical Center, Seoul, South Korea. Matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) biotyper was not used during the study period. Clinical information and microbiological data were collected from all patients.
Bacterial isolates and species identification
A. baumannii were detected among patients with bloodstream infections in the PICU from January 2000 to December 2016. Only the first isolate from each patient was included in this study. Initially, isolates that were identified as Acinetobacter species by the VITEK 2 system (bioMérieux, Marcy l'Etoile, France) from clinical care were included. All of A. baumannii were differentiated to imipenem-sensitive A. baumannii (ISAB) and imipenem-resistant A. baumannii (IRAB).
From January 2010 to December 2016, A. baumannii were collected and species-level identification using partial rpoB gene sequences were performed,10,11 and were tested for antimicrobial susceptibility.
Antimicrobial susceptibility testing
Antimicrobial susceptibility was confirmed for available isolates using the broth microdilution method following the Clinical and Laboratory Standards Institute (CLSI) guidelines.12 The minimum inhibitory concentrations (MICs) of 12 antimicrobial agents, including imipenem, meropenem, cefotaxime, cefepime, ceftazidime, amikacin, ciprofloxacin, tetracycline, piperacillin-tazobactam, colistin, polymyxin B, and tigecycline were determined. Susceptibility was defined according to CLSI breakpoints,12 using Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 as controls. All tests were performed in duplicate, and each test included three biological replicates per strain.
Multilocus sequence typing (MLST) and antimicrobial resistance genes
MLST was performed for A. baumannii isolates as previously described.13 All MLST data were submitted to the A. baumannii MLST database and Oxford scheme was applied.14,15 Clonal complexes were determined using the eBURST program.16 For all of the IRAB isolates, resistance genes, including blaIMP, blaVIM, blaGIM, blaSIM, blaKPC, blaNDM-1, blaOXA-48, blaOXA-23-like, blaOXA-24-like, blaOXA-51-like, and blaOXA-58-like were detected by polymerase chain reaction, as described previously.17
Statistical analysis
Fisher’s exact test was used to analyze categorical variables. A P value of < 0.05 was considered statistically significant. Overall survival rates were estimated using the Kaplan-Meier method, and differences in survival curves were compared using the log-rank test by GraphPad Prism version 9.3.1 (GraphPad Software, San Diego, CA, USA).
Ethics statement
The Institutional Review Board (IRB) at Samsung Medical Center, Seoul, South Korea, reviewed and approved this study (approval number: 2020-05-020-002). Informed consent was exempted by IRB.
RESULTS
Patient characteristics and epidemiology
Bacteremia episodes occurred in 27 patients; ISAB (n = 10) and IRAB (n = 17). Male patients were 41% (11/27), and the median age at the onset of bacteremia was 5.2 years (range, 0–18.6 years). Among the underlying conditions in patients with A. baumannii bacteremia, hematology-oncology disease was the most common underlying condition (14/27, 52%) followed by neurological diseases (4/27, 15%) (Table 1).
Table 1. Characteristics of patients with underlying diseases.
| Parameters | All (N = 27) | ISAB (n = 10) | IRAB (n = 17) | |
|---|---|---|---|---|
| Median age, yr | 5.2 | 1.9 (range, 0.6–16) | 5.4 (0–18.6) | |
| Male | 11 | 5 | 6 | |
| Median ICU stay prior to bacteremia, day | 5 | 5 (range, 0–51) | 4 (0–48) | |
| Underlying disease | ||||
| Hematology and oncology | 14 | 2 | 12 | |
| HCT | 8 | 0 | 8 | |
| Cardiologya | 3 | 2 | 1 | |
| Pulmonology | 2 | 1 | 1 | |
| Neurology | 4 | 3 | 1 | |
| Othersb | 3 | 2 | 1 | |
| No underlying disease | 1 | 1 | 0 | |
ISAB = imipenem-sensitive A. baumannii, IRAB = imipenem-resistant A. baumannii, ICU = intensive care unit, HCT = hematopoietic cell transplantaion.
aThere was one neonate under 28 days with congenital heart disease was included.
bPrimary immunodeficiency, renal disease, vascular malformation.
In 33% (9/27, ISAB = 3/10, IRAB = 6/17) of patients, A. baumannii was isolated from tracheal aspirate prior to the development of bacteremia with a median duration of 8 days (range, 5–124).
Epidemiological changes in imipenem susceptibility and antimicrobial resistance pattern
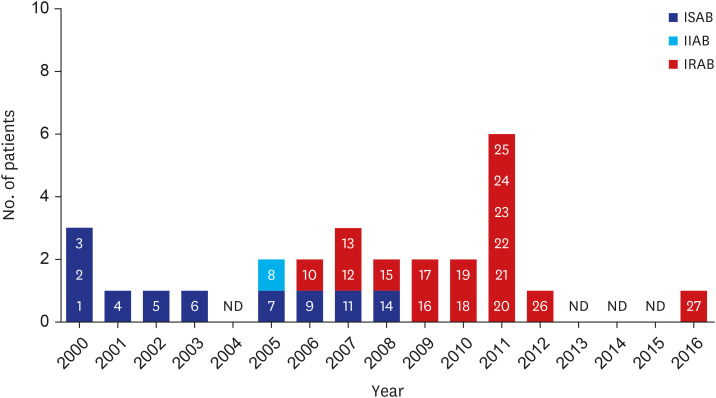
There was a clear shift in the antibiogram of A. baumannii during the study period. From 2000 to 2003, all A. baumannii isolates were ISAB (n = 6). From 2005 to 2008, both IRAB (n = 5) and ISAB (n = 4) were isolated. However, from 2009, all A. baumannii isolates were IRAB (n = 12) (Fig. 1).
Fig. 1. Epidemiology of A. baumannii bacteremia in pediatric intensive care unit from 2000 to 2016.
Numbers shown in each bar refer to the isolate number.
ISAB = imipenem-sensitive A. baumannii, IIAB = imipenem-intermediate-resistant A. baumannii, IRAB = imipenem-resistant A. baumannii, ND = not detected.
In 2011, an outbreak of IRAB occurred causing six patients with IRAB bacteremia (patient number 20–25).
Among 27 A. baumannii bacteremia episodes, 10 isolates were available. All 10 isolates were resistant to imipenem and meropenem. They were also all resistant to amikacin and ciprofloxacin. Five isolates were sensitive to tetracycline, and three were sensitive to tigecycline. All of the isolates were sensitive to colistin with MIC ≤ 2 mg/L and polymyxin B with MIC ≤ 1 mg/L by microdilution methods (Table 2).
Table 2. Antimicrobial susceptibility profiles of A. baumannii isolates.
| Isolate | MIC, mg/L (antimicrobial susceptibility category) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IMI | MRP | CTX | CFP | CAZ | AMK | CIP | TET | P/T | CL | PB | TIG | |
| Ab10-18 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 16 (R) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
| Ab10-19 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | 64 (R) | > 64 (R) | > 64 (R) | > 256/4 (R) | 2 (S) | 1 (S) | 8 (R) |
| Ab11-20 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 4 (S) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
| Ab11-21 | > 64 (R) | > 64 (R) | > 128 (R) | 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 8 (I) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
| Ab11-22 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | 64 (R) | 4 (S) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
| Ab11-23 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | 64 (R) | 4 (S) | > 256/4 (R) | 1 (S) | 1 (S) | 2 (S) |
| Ab11-24 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 16 (R) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
| Ab11-25 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | 64 (R) | 4 (S) | > 256/4 (R) | 1 (S) | 1 (S) | 2 (S) |
| Ab12-26 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 64 (R) | > 128 (R) | 64 (R) | 8 (I) | > 256/4 (R) | 2 (S) | 1 (S) | 2 (S) |
| Ab16-27 | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | > 64 (R) | > 128 (R) | > 64 (R) | 4 (S) | > 256/4 (R) | 1 (S) | 1 (S) | 4 (I) |
MIC = minimum inhibitory concentration, IMI = imipenem, MRP = meropenem, CTX = cefotaxime, CFP = cefepime, CAZ = ceftazidime, AMK = amikacin, CIP = ciprofloxacin, TET = tetracycline, P/T = piperacillin-tazobactam, CL = colistin, PB = polymyxin B, TIG = tigecycline, R = resistant, I = intermediate-resistant, S = susceptible, Ab#-# = A. baumannii isolated year-patient number.
MLST and antimicrobial resistance genes
Among the 10 isolates tested for molecular analysis, nine were isolated from 2010 to 2012 (Table 3). During that period, seven of them were sequence type (ST) 138 and two isolates from patients who were transferred from outside hospitals, were ST75 and ST92.
Table 3. Genotypes of A. baumannii and identification of OXA-type carbapenemase genes.
| Isolate No. | Year | CC | ST | OXA-23-like | OXA-24-like | OXA-51-like | OXA-58-like |
|---|---|---|---|---|---|---|---|
| Ab10-18 | 2010 | CC92 | ST138 | + | - | + | - |
| Ab10-19a | 2010 | CC92 | ST75 | + | - | + | - |
| Ab11-20 | 2011 | CC92 | ST138 | + | - | + | - |
| Ab11-21 | 2011 | CC92 | ST138 | + | - | + | - |
| Ab11-22 | 2011 | CC92 | ST138 | + | - | + | - |
| Ab11-23 | 2011 | CC92 | ST138 | + | - | + | - |
| Ab11-24 | 2011 | CC92 | ST138 | + | - | + | - |
| Ab11-25c | 2011 | CC92 | ST92 | + | - | + | - |
| Ab12-26 | 2012 | CC92 | ST138 | + | - | + | - |
| Ab16-27c | 2016 | CC92 | ST191 | + | - | + | - |
All of the A. baumannii isolates were negative to blaIMP, blaVIM, blaNDM, blaGIM, blaSIM, and blaSPM.
CC = clonal complex, ST = sequence type, Ab#-# = A. baumannii isolated year-patient number.
aThese patients were transferred from outside hospital.
Following the 2011 outbreak, there were no A. baumannii bacteremia cases from 2013 to 2015. An IRAB isolate with ST191 was identified in 2016 in a patient transferred from outside hospital and this was not progressed to additional outbreak in the PICU.
Among the resistance genes tested (blaIMP, blaVIM, blaGIM, blaSIM, blaKPC, blaNDM-1, blaOXA-48, blaOXA-23-like, blaOXA-24-like, blaOXA-51-like, and blaOXA-58-like), carbapenemase Ambler class A and B genes were not detected. All ten isolates were positive to class D genes (OXA-23 like and OXA-51 like) and negative to OXA-24-like and OXA-54-like genes (Table 3).
Treatment outcome
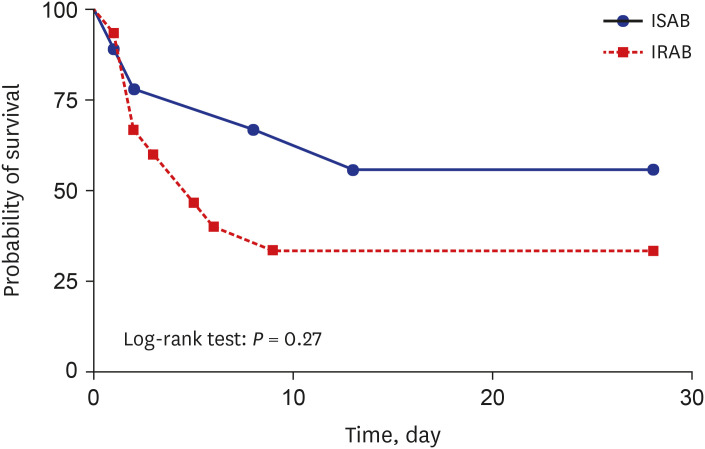
Overall, among the 27 patients (ISAB: n = 10, IRAB: n = 17), the case-fatality rate within 28 days from bacteremia was 63% (17/27). There was no statistical difference in the fatality rate between the ISAB and IRAB groups (5/10, 50% vs. 12/17, 71%; P = 0.422). In Kaplan-Meier survival curve, no significant difference between the two groups was observed (Fig. 2). However, the case fatality rate of hematology-oncology patients was higher than that of rest of other patients (86% vs. 38%, P = 0.011).
Fig. 2. Survival curve of ISAB and IRAB group.
ISAB = imipenem-sensitive A. baumannii, IRAB = imipenem-resistant A. baumannii.
The median interval from A. baumannii bacteremia onset to death was two days (range, 0–13) in ISAB and it was also two days in IRAB (range, 0–9) group. When IRAB group was examined further in detail, 35% (6/17) of patients with IRAB bacteremia died within 2 days before the culture and susceptibility test results became available and 67% (4/6) of patients had previous positive culture for IRAB from the tracheal aspirate before bacteremia developed.
A total of 78% (21/27) of all the patients were treated with susceptible antibiotics within 2 days from bacteremia onset, 62% (13/21) of patients died. In ISAB group, six patients (6/10) were treated with carbapenem and 33% (2/6) died. Whereas four patients (4/10) were treated without carbapenem and 75% (3/4) died (P = 0.519). In IRAB group, seven patients (7/17, 41%) were treated with colistin and 71% (5/7) died. Ten patients (10/17, 59%) in IRAB group did not receive colistin and 70% (7/10) died (P = 0.949).
Infection control
With an alert on IRAB outbreak in 2011, environmental culture including the hands of medical workers, computers and telephones of the nursing station, sink, and all of 15 bed rails was performed in 2011–2012. Reeducation of contact precaution and hand hygiene were performed to PICU medical workers. IRAB isolation frequency was dramatically decreased after infection control intervention. Antibiotic stewardship was strengthened.
DISCUSSION
This was a study on the long-term epidemiology of A. baumannii bacteremia and antibiotic resistance in PICU for 17 consecutive years of pre-MALDI-TOF period. We observed a dramatic shift in antibiotic susceptibility from all ISAB before 2004 to all IRAB in 2009 that was followed by an outbreak with high mortality due to ST138 IRAB. This outbreak peaked in 2011 and was controlled after an extensive infection control intervention.
Resistance to the carbapenem is a global issue. In the United States, the rate of A. baumannii resistance to imipenem and meropenem in 2008 was reported as 48% and 57.4% respectively.18 In Korea, the rate of A. baumannii resistance to carbapenem among adult patients was 85% in 2015.19 Imipenem resistance among pediatric patients is also increasing.9,20 In other study of Korean PICU and neonatal intensive care unit (ICU) of Taiwan, the rapid emergence of IRAB was also observed.9,21 Cases of colistin-resistant AB were reported among patients who were treated with colistin to treat carbapenem-resistant A. baumannii (CRAB) infection.22
We observed that all isolates were positive for OXA-23 like and clonal complex 92. OXA-23 like β-lactamase is a main carbapemase of A. baumannii.23,24 Clonal complex 92 is a widely distributed clone and major cause of A. baumannii outbreaks worldwide.25 It is also a major clone in Korean CRAB.26 The distribution of sequence type and resistant gene change according to year of isolation with ST191 predominance was observed among isolated A. baumannii in Korean tertiary hospitals.23,27
In this study, 35% (6/17) of patients with IRAB bacteremia died within 2 days before the culture and susceptibility test results became available. Among the six patients, 67% (4/6) had previous positive culture for IRAB from the tracheal aspirate before bacteremia onset. Active surveillance for preceding tracheal colonization or pneumonia and proactive antibiotic treatment strategy may allow the early initiation of appropriate antibiotic treatment in high risk rapidly deteriorating patients.28
In the ICU, the early identification and prevention of an outbreak are important. The infection control team consisting of healthcare personnel expertise is important.29 In a study of Korean adults in ICU, active surveillance and cohorting of patients for the CRAB infected or colonized patients reduced CRAB infection.30 In this study, infection control efforts in PICU were sustained to prevent additional outbreak. As a result, there was not a single case of A. baumannii bacteremia (both ISAB and IRAB) for three years (2013–2015). When we have there was one IRAB bacteremia patient transferred from an outside hospital in 2016, this was not progressed to outbreak due to strict infection control measures (Fig. 1). Multifaceted infection control approaches including timely feedback, regular education and revisiting of control measures among infection control team, pediatric infectious disease experts, critical care physicians, and nursing staffs are essential.
This study has some limitations. Although the study period was relatively long (17 years), this was a retrospective study, and not all bacterial isolates were tested. Therefore, MLST or bacterial resistance analysis could not be performed on isolates from the early period. In addition, the source of the outbreak was not clear.
In conclusion, this was a long-term epidemiology study that evaluated IRAB bacteremia in PICU patients. Antimicrobial stewardship programs and multifaceted infection control approaches are essential to reduce outbreak caused by a resistant pathogen such as IRAB in high-risk PICU patients.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim D, Cho J, Choi SH.
- Data curation: Kim D, Lee H, Choi JS, Croney CM, Park KS, Park HJ.
- Formal analysis: Kim D, Lee H.
- Investigation: Kim JY, Kim YJ.
- Methodology: Son S, Choi SH, Huh HJ, Lee NY, Kim YJ.
- Validation: Ko KS.
- Writing - original draft: Kim D, Lee H.
- Writing - review & editing: Kim D, Lee H, Kim YJ.
References
- 1.Lakshmi KS, Jayashree M, Singhi S, Ray P. Study of nosocomial primary bloodstream infections in a pediatric intensive care unit. J Trop Pediatr. 2007;53(2):87–92. doi: 10.1093/tropej/fml073. [DOI] [PubMed] [Google Scholar]
- 2.Le NK, Hf W, Vu PD, Khu DT, Le HT, Hoang BT, et al. High prevalence of hospital-acquired infections caused by Gram-negative carbapenem resistant strains in Vietnamese pediatric ICUs: a multi-centre point prevalence survey. Medicine (Baltimore) 2016;95(27):e4099. doi: 10.1097/MD.0000000000004099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lake JG, Weiner LM, Milstone AM, Saiman L, Magill SS, See I. Pathogen distribution and antimicrobial resistance among pediatric healthcare-associated infections reported to the National Healthcare Safety Network, 2011-2014. Infect Control Hosp Epidemiol. 2018;39(1):1–11. doi: 10.1017/ice.2017.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vila J, Bonomo RA. 46th Interscience Conference on Antimicrobial Agents and Chemotherapy. Future Microbiol. 2007;2(1):9–12. doi: 10.2217/17460913.2.1.9. [DOI] [PubMed] [Google Scholar]
- 5.Endo S, Yano H, Hirakata Y, Arai K, Kanamori H, Ogawa M, et al. Molecular epidemiology of carbapenem-non-susceptible Acinetobacter baumannii in Japan. J Antimicrob Chemother. 2012;67(7):1623–1626. doi: 10.1093/jac/dks094. [DOI] [PubMed] [Google Scholar]
- 6.Evans BA, Amyes SG. OXA β-lactamases. Clin Microbiol Rev. 2014;27(2):241–263. doi: 10.1128/CMR.00117-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee HY, Hsu SY, Hsu JF, Chen CL, Wang YH, Chiu CH. Risk factors and molecular epidemiology of Acinetobacter baumannii bacteremia in neonates. J Microbiol Immunol Infect. 2018;51(3):367–376. doi: 10.1016/j.jmii.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Sultan AM, Seliem WA. Identifying risk factors for healthcare-associated infections caused by carbapenem-resistant Acinetobacter baumannii in a neonatal intensive care unit. Sultan Qaboos Univ Med J. 2018;18(1):e75–e80. doi: 10.18295/squmj.2018.18.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hong KB, Oh HS, Song JS, Lim JH, Kang DK, Son IS, et al. Investigation and control of an outbreak of imipenem-resistant Acinetobacter baumannii infection in a pediatric intensive care unit. Pediatr Infect Dis J. 2012;31(7):685–690. doi: 10.1097/INF.0b013e318256f3e6. [DOI] [PubMed] [Google Scholar]
- 10.Ko KS, Kuwahara T, Haehwa L, Yoon YJ, Kim BJ, Lee KH, et al. RNA polymerase beta-subunit gene (rpoB) sequence analysis for the identification of Bacteroides spp. Clin Microbiol Infect. 2007;13(1):48–54. doi: 10.1111/j.1469-0691.2006.01553.x. [DOI] [PubMed] [Google Scholar]
- 11.La Scola B, Gundi VA, Khamis A, Raoult D. Sequencing of the rpoB gene and flanking spacers for molecular identification of Acinetobacter species. J Clin Microbiol. 2006;44(3):827–832. doi: 10.1128/JCM.44.3.827-832.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clinical and Laboratory Standards Institute (CLSI) CLSI Supplement M100S. Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. Wayne, PA, USA: CLSI; 2016. [Google Scholar]
- 13.Park YK, Choi JY, Jung SI, Park KH, Lee H, Jung DS, et al. Two distinct clones of carbapenem-resistant Acinetobacter baumannii isolates from Korean hospitals. Diagn Microbiol Infect Dis. 2009;64(4):389–395. doi: 10.1016/j.diagmicrobio.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Public databases for molecular typing and microbial genome diversity. [Updated 2022]. [Accessed September 5, 2021]. https://pubmlst.org/bigsdb?db=pubmlst_abaumannii_seqdef&page=profiles .
- 15.Bartual SG, Seifert H, Hippler C, Luzon MA, Wisplinghoff H, Rodríguez-Valera F. Development of a multilocus sequence typing scheme for characterization of clinical isolates of Acinetobacter baumannii . J Clin Microbiol. 2005;43(9):4382–4390. doi: 10.1128/JCM.43.9.4382-4390.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feil EJ, Smith JM, Enright MC, Spratt BG. Estimating recombinational parameters in Streptococcus pneumoniae from multilocus sequence typing data. Genetics. 2000;154(4):1439–1450. doi: 10.1093/genetics/154.4.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park YK, Jung SI, Park KH, Kim DH, Choi JY, Kim SH, et al. Changes in antimicrobial susceptibility and major clones of Acinetobacter calcoaceticus-baumannii complex isolates from a single hospital in Korea over 7 years. J Med Microbiol. 2012;61(Pt 1):71–79. doi: 10.1099/jmm.0.033852-0. [DOI] [PubMed] [Google Scholar]
- 18.Rhomberg PR, Jones RN. Summary trends for the Meropenem Yearly Susceptibility Test Information Collection Program: a 10-year experience in the United States (1999-2008) Diagn Microbiol Infect Dis. 2009;65(4):414–426. doi: 10.1016/j.diagmicrobio.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 19.Kim D, Ahn JY, Lee CH, Jang SJ, Lee H, Yong D, et al. Increasing resistance to extended-spectrum cephalosporins, fluoroquinolone, and carbapenem in Gram-negative bacilli and the emergence of carbapenem non-susceptibility in Klebsiella pneumoniae: analysis of Korean Antimicrobial Resistance Monitoring System (KARMS) data from 2013 to 2015. Ann Lab Med. 2017;37(3):231–239. doi: 10.3343/alm.2017.37.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu A, Zheng B, Xu YC, Huang ZG, Zhong NS, Zhuo C. National epidemiology of carbapenem-resistant and extensively drug-resistant Gram-negative bacteria isolated from blood samples in China in 2013. Clin Microbiol Infect. 2016;22(Suppl 1):S1–S8. doi: 10.1016/j.cmi.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 21.Thatrimontrichai A, Apisarnthanarak A, Chanvitan P, Janjindamai W, Dissaneevate S, Maneenil G. Risk factors and outcomes of carbapenem-resistant Acinetobacter baumannii bacteremia in neonatal intensive care unit: a case-case-control study. Pediatr Infect Dis J. 2013;32(2):140–145. doi: 10.1097/INF.0b013e318270b108. [DOI] [PubMed] [Google Scholar]
- 22.Garcia Casallas JC, Robayo-Amortegui H, Corredor-Rozo Z, Carrasco-Márquez AM, Escobar-Perez J. Bacteremia by colistin-resistant Acinetobacter baumannii isolate: a case report. J Med Case Reports. 2019;13(1):141. doi: 10.1186/s13256-019-2062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeon H, Kim S, Kim MH, Kim SY, Nam D, Park SC, et al. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii isolates from a Korean hospital that carry blaOXA-23 . Infect Genet Evol. 2018;58:232–236. doi: 10.1016/j.meegid.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Smith CA, Antunes NT, Stewart NK, Toth M, Kumarasiri M, Chang M, et al. Structural basis for carbapenemase activity of the OXA-23 β-lactamase from Acinetobacter baumannii . Chem Biol. 2013;20(9):1107–1115. doi: 10.1016/j.chembiol.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karah N, Sundsfjord A, Towner K, Samuelsen Ø. Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii . Drug Resist Updat. 2012;15(4):237–247. doi: 10.1016/j.drup.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 26.Kim DH, Jung SI, Kwon KT, Ko KS. Occurrence of diverse AbGRI1-type genomic islands in Acinetobacter baumannii global clone 2 isolates from South Korea. Antimicrob Agents Chemother. 2017;61(2):e01972-16. doi: 10.1128/AAC.01972-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim MH, Jeong H, Sim YM, Lee S, Yong D, Ryu CM, et al. Using comparative genomics to understand molecular features of carbapenem-resistant Acinetobacter baumannii from South Korea causing invasive infections and their clinical implications. PLoS One. 2020;15(2):e0229416. doi: 10.1371/journal.pone.0229416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lampati L, Maggioni E, Langer M, Malacarne P, Mozzo R, Pesenti A, et al. Can routine surveillance samples from tracheal aspirate predict bacterial flora in cases of ventilator-associated pneumonia? Minerva Anestesiol. 2009;75(10):555–562. [PubMed] [Google Scholar]
- 29.Karageorgopoulos DE, Falagas ME. Current control and treatment of multidrug-resistant Acinetobacter baumannii infections. Lancet Infect Dis. 2008;8(12):751–762. doi: 10.1016/S1473-3099(08)70279-2. [DOI] [PubMed] [Google Scholar]
- 30.An JH, Kim YH, Moon JE, Jeong JH, Kim SH, Kang SJ, et al. Active surveillance for carbapenem-resistant Acinetobacter baumannii in a medical intensive care unit: can it predict and reduce subsequent infections and the use of colistin? Am J Infect Control. 2017;45(6):667–672. doi: 10.1016/j.ajic.2017.01.016. [DOI] [PubMed] [Google Scholar]