Abstract
Introduction
New treatment options, like endovascular aortic repair, reduced the mortality rate of patients suffering from complications after an acute type A aortic dissection repair. Nevertheless, initial successful treatment of an aortic dissection does not fully eliminate the risk of later adverse aortic events like anastomotic pseudoaneurysm. Pseudoaneurysm of the anastomosis between the ascending and the arch graft could initiate complications like peripheral embolization, dysphagia or compression of mediastinum organs. Re-operation via re-sternotomy bears enormous morbidity and mortality for these patients. There is a high unmet need for percutaneous therapeutic options to treat pseudoaneurysms.
Case Presentation
A 59-year-old-man treated 15 years ago for type A aortic dissection, was hospitalized due to intermittent abdominal pain. A detailed examination revealed 2 pseudoaneurysms: 1 symptomatic at the level of the reimplanted celiac trunk and 1 asymptomatic at the anastomosis between the brachiocephalic trunk and the aortic arch graft. Due to multiple co-morbidities and previous operations, the risk for surgery was considered too high. Both pseudoaneurysm were treated percutaneously, the symptomatic 1 with covered stent and the asymptomatic with Amplatzer™ septal-occluder.
Discussion
We present an alternative percutaneous therapy approach for treatment of pseudoaneurysm using a septal-occluder. A follow-up computed tomography 3 months later showed successfully excluded pseudoaneurysm.
Keywords: pseudoaneurysm, septal occluder, aortic dissection, brachiocephalic trunk
Case Report
With an incidence rate of .00006% per year, acute type A aortic dissection (TAAD) is considered to be a rare disease. 1 Due to improving treatment options for TAAD, mortality has been reduced in the last decade. As such, reinterventions in these patients are becoming more frequent and include recurrence of acute dissections, penetrating atherosclerotic ulcers or pseudoaneurysms. 2
Here we present a 59-year-old-man with multiple known comorbidities such as chronic coronary syndrome, chronic obstructive pulmonary disease and chronic kidney disease, who was hospitalized due to a late-onset complication of 2 pseudoaneurysm after a long and complex treatment of a TAAD. The patient suffered a TAAD in 2005, followed by supracoronary graft replacement with aortic valve resuspension. 3 years later an aneurysm of the right common iliac artery was treated with an aorto-biiliac polytetrafluoroethylene (PTFE) graft. In 2012, the patient was hospitalized due to an increasing dilatation of the aortic-arch and thoracic-abdominal aortic aneurysm, which was treated with a mechanical composite graft (Medtronic ATS™ 23 mm) and a Frozen-Elephant-Trunk (Vascutek Terumo Gelweave™ 26 × 8 mm Anteflo) to replace the primary ascending graft and the dilated aortic-arch. The left common carotid artery and the brachiocephalic trunk (BCT) were reimplanted directly in the aortic-arch graft, whereas the left subclavian artery was reimplanted with a dacron-bypass (Vascutek Terumo Gelsoft™ Plus 10 mm) from the aortic graft. The thoraco-abdominal aortic aneurysm was treated by open and endovascular means: visceral debranching via laparotomy was followed by thoracic endovascular aortic repair with 3 stent-grafts (Medtronic Valiant™ Thoracic distal 26/22 mm, medial 32/28 mm, proximal 34/34 mm). Over the next 7 years, the patient underwent numerous re-interventions to treat endoleaks in the aorta.
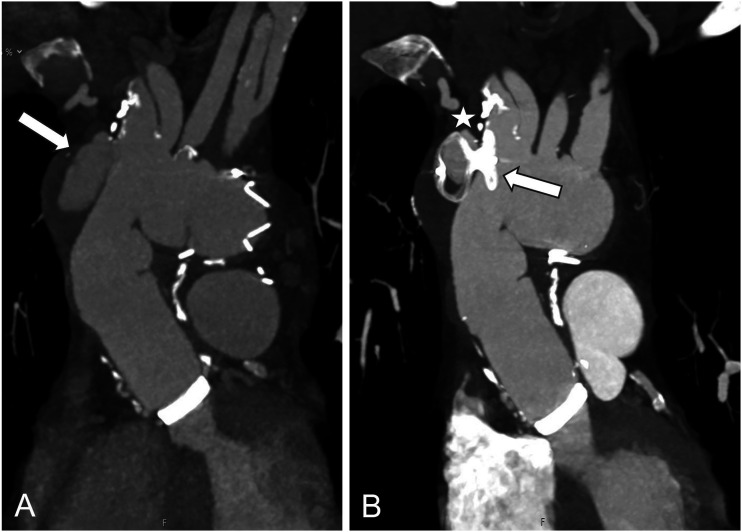
In December 2020 the patient presented with abdominal pain and emergency computed tomography angiography (CTA) revealed an 11 cm large symptomatic pseudoaneurysm at the anastomosis to the celiac trunk and a 5 cm asymptomatic pseudoaneurysm between the brachiocephalic trunk and the aortic arch graft with an anastomotic defect of 7 × 7 mm (Figure 1A). In view of the symptomatic large aneurysm, treatment during the same hospitalization was planned. Considering the multiple comorbidities, open surgery and general anesthesia was considered to be high-risk and therefore, a two-stage percutaneous intervention was preferred (EuroScore II = 18%).
Figure 1.
Computed tomography angiography (CTA) images of the thoracic aorta with pseudoaneurysm of the brachiocephalic trunk before (A) and after (B) repair with a septal occluder; minimal endoleak (B *).
In an urgent procedure, the pseudoaneurysm at the level of the celiac trunk was excluded by inserting a covered stent (Gore® Viabahn® 10x50 mm) in the hepatic artery. In addition, the splenic-artery was occluded with a vascular plug (Amplatzer™ Vascular Plug II 10 mm) to counteract a retrograde flow, which can lead to type 2 endoleak.
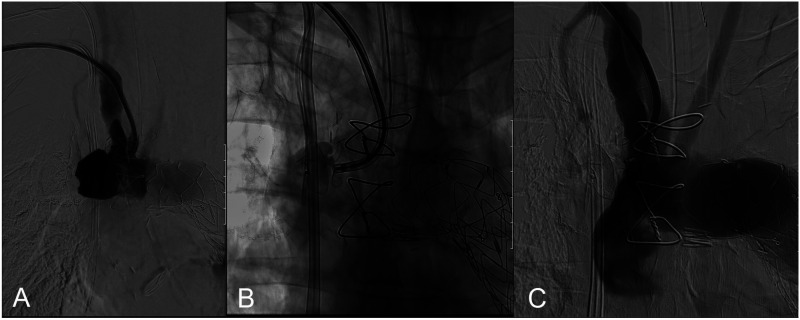
Two weeks later the asymptomatic pseudoaneurysm between the brachiocephalic trunk and the aortic arch graft (Figure 2A) was treated to prevent rupture. 3 A 55 cm 7 French Flexor® Ansel guiding sheath was introduced over the brachial artery under therapeutic anticoagulation with heparin and was inserted to the aortic-arch but the aneurysm could not be reached. We switched to a 71 cm 8.5 French Oscor® Destino steerable sheath, which was managed to place over the entrance of the aneurysm, so that the selected septal-occluder (Amplatzer™ Septal Occluder 12 mm) could be introduced into the anastomotic defect. Under fluoroscopic guidance, 1 part of the occluder was positioned in the vessel lumen and the other part in the aneurysm (Figure 2B), similar to occlusion of a septal defect. Final angiography showed a minimal residual perfusion of the pseudoaneurysm with the occluder fully unfolded and in good and stable position (Figure 2C).
Figure 2.
Angiography with contrast agent of the pseudoaneurysm of the brachiocephalic trunk (A); placement of a septal occluder into the pseudoaneurysm (B); final angiography of the repaired pseudoaneurysm (C).
Postprocedural, the patient developed a minor CT proven stroke with dysarthria and weakness of the right arm despite continued oral anticoagulation due to the mechanical aortic valve. The neurological symptoms improved substantially and the patient was sent to a neurological rehabilitation. The CTA follow-up at 3 months demonstrated stable pseudoaneurysm diameter with persistent minimal perfusion and small endoleak at the level of the aortic-arch (Figure 1B) and completely excluded infradiaphragmal pseudoaneurysm. In a telephonic consultation 5 months after treatment, the patient reports stable cardiac conditions, with complete neurological recovery. The patient was on anticoagulation with coumarin because of the mechanical aortic valve.
Few cases described the use of septal-occluder in treatment of pseudoaneurysms, but none of them reports the follow-up data. 4 In conclusion, we report a patient with pseudoaneurysm at the level of the proximal aortic-arch, who underwent a successful off-label endovascular repair with a septal-occluder. In high-risk patients, endovascular repair under local anesthesia could be a valid option to protect these patients from serious consequences. For this reason, novel and alternative treatment options are of great importance and newsworthy, since no consistent treatment guidelines are applicable. The risk of periprocedural neurological events, however, requires consideration.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent: Informed consent has been obtained from the patient for publication of the case report and accompanying images.
ORCID iD
Julia Vogel https://orcid.org/0000-0003-0503-7198
References
- 1.Reutersberg B, Salvermoser M, Trenner M, et al. hospital incidence and in-hospital mortality of surgically and interventionally treated aortic dissections: Secondary data analysis of the Nationwide German Diagnosis-Related Group Statistics from 2006 to 2014. J Am Heart Assoc. 2019;8(8):e011402. doi: 10.1161/JAHA.118.011402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rylski B, Beyersdorf F, Desai ND, et al. Distal aortic reintervention after surgery for acute DeBakey type I or II aortic dissection: Open versus endovascular repair. Eur J Cardio Thorac Surg. 2015;48(2):258-263. doi: 10.1093/ejcts/ezu488. [DOI] [PubMed] [Google Scholar]
- 3.Robaldo A, Apostolou D, Peano E, Novali C. Giant saccular aneurysm of the innominate artery. Interact Cardiovasc Thorac Surg. 2020;30(2):321-323. doi: 10.1093/icvts/ivz244. [DOI] [PubMed] [Google Scholar]
- 4.Quevedo HC, Santiago-Trinidad R, Castellanos J, Atianzar K, Anwar A, Abi Rafeh N. Systematic review of interventions to repair ascending aortic pseudoaneurysms. Ochsner J. 2014;14(4):576-585. [PMC free article] [PubMed] [Google Scholar]