Abstract
Background
Little is known about healthcare-seeking behaviour and barriers to care for cardiovascular disease (CVD) in sub-Saharan Africa.
Methods
Emergency department patients in Tanzania with acute CVD were prospectively enrolled. Questionnaires were administered at enrollment and 30 d later.
Results
Of 241 patients, 186 (77.2%) had visited another facility for the same illness episode (median symptom duration prior to presentation was 7 d) and 82 (34.0%) reported that they were initially unaware of the potential seriousness of their symptoms. Of the 208 (86.3%) patients completing follow-up, 16 (7.7%) had died, 38 (18.3%) had visited another facility for persistent symptoms, 99 (47.6%) felt they understood their diagnosis, 87 (41.8%) felt they understood their treatment and 11 (7.8%) could identify any of their medications. Predictors of 30 d survival with symptom improvement included medication compliance (p<0.001), understanding the diagnosis (p=0.007), understanding the treatment (p<0.001) and greater CVD knowledge (p=0.008).
Conclusions
Patients with CVD in Tanzania usually visit multiple facilities for the same illness episode, typically after prolonged delays. Only a minority understand their diagnosis and treatment, and such understanding is correlated with survival with symptom improvement. Patient-centred interventions are needed to improve the quality of cardiovascular care in Tanzania.
Keywords: barriers to care, cardiovascular disease, healthcare-seeking behaviour, sub-Saharan Africa
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality worldwide.1 In sub-Saharan Africa (SSA), infectious diseases such as HIV and malaria remain important causes of death,1 but recently the region has experienced rapid growth in CVD risk factors such as hypertension, diabetes and obesity.2 As countries across SSA proceed through the epidemiological transition, CVD is projected to become increasingly common.3 In 2013, CVD was already responsible for nearly 1 million deaths across SSA.4
Despite the growing burden of CVD in SSA, much remains to be learned about healthcare-seeking behaviour and barriers to care for patients with CVD across the region. Some have speculated that CVD may be underdiagnosed and inadequately treated in SSA due to healthcare system factors and patient care-seeking behaviour.5 In Tanzania, for example, many healthcare facilities lack the basic equipment needed to diagnose CVDs and many providers report that they are uncomfortable treating CVDs.6,7 Against this backdrop, increasing numbers of patients with CVDs must navigate healthcare systems that may be ill-equipped to care for them. To date, however, there has been little study of the ways in which patients with CVD navigate the healthcare system in SSA and the barriers they encounter while doing so.
Beyond understanding patterns of healthcare seeking and barriers to care, there is a need to identify predictors of patient outcomes for CVDs in SSA. Although outcomes data in SSA are limited, the existing evidence suggests that patients with CVDs have poor prognoses.8 Recent studies from Uganda and Zambia, for example, found that the in-hospital mortality rate among patients admitted for heart failure was approximately 20%,9,10 four times higher than the in-hospital mortality rate for patients with heart failure in the USA.11 Given this tremendous discrepancy, there is an urgent need to identify predictors of mortality and morbidity for CVDs in SSA in order to develop interventions to improve outcomes. In particular, to our knowledge, currently no data exist from SSA describing the relationship between patient-centred factors such as disease understanding or medication compliance and CVD outcomes.
In order to address these gaps in the literature, the purpose of this study was to observe patterns of healthcare-seeking behaviour among adults with acute CVD in northern Tanzania, to describe barriers to care from the patient perspective and to identify predictors of survival with symptom improvement among such patients. To do so, we conducted a prospective observational study in an emergency department (ED) in the Kilimanjaro Region of Tanzania.
Materials and methods
Setting
This study was conducted at Kilimanjaro Christian Medical Centre (KCMC), a tertiary care centre located in the Kilimanjaro Region of northern Tanzania. In 2014, the community prevalence of hypertension was 28% and the community prevalence of diabetes was 6%.12,13 The physicians in the KCMC ED include attending physicians with and without residency training in emergency medicine, residents, interns and clinical officers.
Participant selection
All adult patients (≥18 y of age) presenting to the KCMC ED were screened by trained research assistants. All patients with acute chest pain or shortness of breath were eligible for enrolment, but only patients who subsequently received any acute CVD-related diagnosis from the ED physician were included in the analysis. Thus only CVD events associated with acute chest pain or shortness of breath were captured by these recruitment methods. Adjudication of whether not a patient’s ED diagnosis was CVD related is described below. Exclusion criteria were self-reported fever, traumatic chest pain and inability to provide informed consent due to altered mental status. Screening was conducted during one clinical shift per day (morning, evening or night) from 20 August 2018 through 4 January 2019. The number of days spent screening during each clinical shift was assigned proportionally to total patient volume during each shift.
Study procedures
Patients were administered a questionnaire regarding sociodemographic information, medical history and prior care seeking for the present illness. This questionnaire was adapted from the WHO Stepwise Approach to Surveillance (STEPS) survey for non-communicable disease, which includes questions about cardiovascular comorbidities and lifestyle behaviours such as diet, exercise and tobacco use.14 If patients reported that they did not present to the hospital immediately, they were asked in an open-ended fashion to explain the reasons for their delay. A single blood pressure measurement was obtained in a seated position using the calibrated Beurer BM40 automatic blood pressure monitor (Beurer, Ulm, Germany). Patient weight and height were measured and recorded by a member of the study team and patient diagnoses and prescriptions were recorded directly from each patient’s ED chart.
Thirty days after enrolment, enrolled patients were contacted via telephone and a follow-up questionnaire was administered. If participants were unavailable or deceased, the questionnaire was administered to a relative. The follow-up questionnaire included questions regarding vital status, symptom progression, medication compliance and additional healthcare utilization. Participants were asked to report any routine follow-up appointments as well as unscheduled visits to healthcare facilities for persistent symptoms from the same illness episode. Participants were asked, in an open-ended fashion, to identify any barriers they encountered during or after their ED visit. Finally, patients were asked to identify their medications and their ED diagnosis and whether they felt they understood their diagnosis and treatment. All survey instruments were administered in Swahili. Although English versions of the survey instruments were available, these were not used as we did not encounter any patients who were not fluent in Swahili.
Study definitions
Each patient’s primary diagnosis was defined as the first diagnosis listed by the ED physician. An adjudication committee of emergency physicians from Tanzania and the USA reviewed the physician-recorded primary diagnoses and determined whether or not they were related to CVD. CVD-related diagnoses were defined as acute coronary syndrome, ischemic heart disease, heart failure, angina, rheumatic heart disease, arrhythmia, pericarditis, pulmonary embolism and symptomatic hypertension (defined as hypertensive emergency, hypertensive urgency or severe hypertension). Examples of diagnoses not considered to be CVD-related included peptic ulcer disease, pneumonia and asthma exacerbation. Disagreements among members of the adjudication committee were resolved by consensus. The study team and adjudication committee did not have access to the results of individual patient diagnostic testing, such as echocardiograms or electrocardiograms, thus determination of CVD cases was made solely from the physician-documented diagnoses. The adjudication committee then compared the diagnoses and prescriptions reported by the patients to those recorded by the ED physician in the medical record. Patients were classified as successfully identifying their diagnosis if the patient-reported diagnosis matched the physician-recorded diagnosis or if, in the view of the committee, the patient was able to adequately describe his/her diagnosis without identifying it by name. For example, a patient diagnosed with heart failure who described the diagnosis as his/her heart not pumping well was classified as correctly identifying the diagnosis. However, a patient diagnosed with heart failure who could not name his/her diagnosis or who identified a different disease process, such as pneumonia, was classified as being unable to identify the diagnosis. Similarly, patients were classified as being able to correctly identify their medications if they could name the medications prescribed by the ED physician by any generic or brand name. Hypertension was defined as a self-reported history of hypertension or a measured blood pressure ≥140/90 mmHg. Diabetes, hyperlipidaemia, HIV infection, alcohol use and smoking status were defined by patient self-reports. Sedentary lifestyle was defined as a self-report of <150 min of moderately vigorous physical activity per week, as per WHO guidelines.15
Cardiovascular disease knowledge
A knowledge, attitudes and practices (KAP) survey regarding CVD was administered to all participants at the time of enrolment. The KAP survey was developed locally and has been published previously.16 An individual CVD knowledge score was generated for each participant by giving 1 point for each correct answer to the knowledge-related questions in the survey, with a maximum score 10.
Statistical analysis
All analyses were performed in RStudio (Boston, MA, USA). Body mass index (BMI) was calculated by dividing the measured weight in kilograms by the square of the measured height in metres. Any patient with a BMI ≥25 kg/m2 was considered to be overweight and those with a BMI <25 kg/m2 were considered to have a normal weight. Continuous variables are presented as medians (IQRs) and categorical variables are presented as proportions. The 5 y risk of cardiovascular event was calculated for each patient using the Harvard National Health and Nutrition Examination Survey (NHANES) risk score, which is based on age, systolic blood pressure, sex, current smoking, diabetes and BMI.17,18 The NHANES risk score has been well validated internationally, including in SSA.18 Associations between patient-reported symptom improvement at 30 d and various patient characteristics were assessed using Welch’s t-test for continuous variables and Pearson’s χ2 for categorical variables. Multivariable logistic regression was performed to identify predictors of survival with symptom improvement at 30 d. ORs and 95% CIs were calculated from two-way contingency tables. A statistical significance threshold of 0.05 was used in all analyses.
Ethical approval
This study received ethics approval from the Duke Health Institutional Review Board, the Kilimanjaro Christian Medical Centre Research Ethics Committee and the Tanzania National Institutes for Medical Research Ethics Coordinating Committee. All participants provided written informed consent prior to enrolment.
Results
During the study period, a total of 3909 adult ED patients were screened, of whom 349 (8.9%) had chest pain or shortness of breath. Of these patients, 339 (97.1%) consented to enrolment in the study. Of enrolled patients, 241 (71.1%) had a diagnosis of CVD and were included in the analysis. Figure 1 summarizes the flow of patients from screening through study follow-up.
Figure 1.
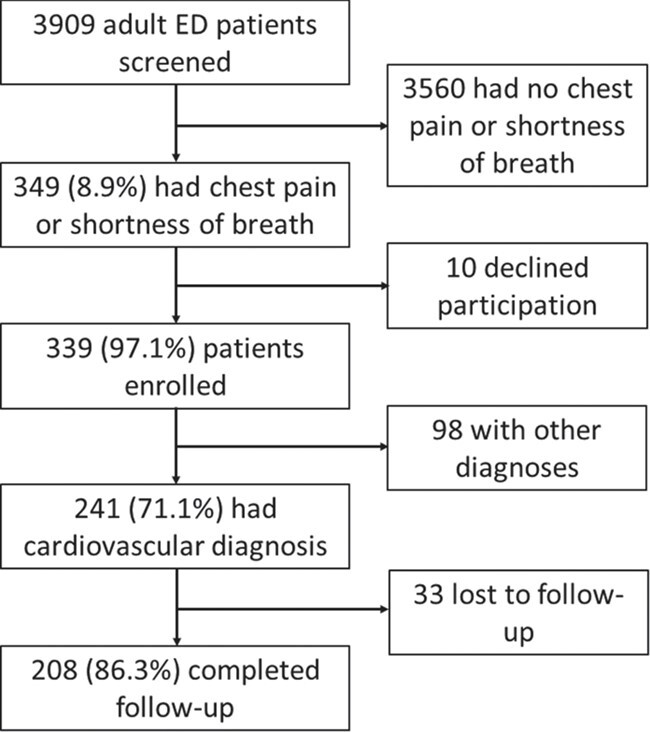
Patient flow diagram.
Table 1 summarizes the sociodemographic and health characteristics of patients included in this analysis. The median age was 62 y (IQR 48–72) and 147 patients (61.0%) were female. The majority of participants (193 patients [80.1%]) had hypertension and half (122 patients [50.6%]) were overweight. Few (14 patients [5.8%]) reported ongoing tobacco use. Overall, 173 (71.8%) had a >10% 5 y risk of a cardiovascular event. The most common ED diagnoses among participants were symptomatic hypertension and heart failure, ascribed to 110 (45.6%) and 105 (43.6%) patients, respectively.
Table 1.
Characteristics of adults with CVD presenting to the ED, northern Tanzania, 2018 (N=241)
| Patient characteristics | Median (IQR) | |
|---|---|---|
| Age (y) | 62 (48–72) | |
| Vegetable consumption per week (d) | 3 (2–6) | |
| Fruit consumption per week (d) | 3 (2–6) | |
| CVD knowledge score | 6 (2–8) | |
| Female sex, n (%) | 147 (61.0) | |
| Education, n (%) | ||
| None | 19 (7.9) | |
| Primary | 152 (63.1) | |
| Secondary | 39 (16.2) | |
| Post-secondary | 31 (12.9) | |
| Hypertension, n (%) | 193 (80.1) | |
| Diabetes, n (%) | 33 (13.7) | |
| Hyperlipidaemia, n (%) | 34 (14.1) | |
| Ongoing tobacco use, n (%) | 14 (5.8) | |
| Ongoing alcohol use, n (%) | 64 (39.0) | |
| Overweight, n (%) | 122 (50.6) | |
| Sedentary lifestyle, n (%) | 92 (38.2) | |
| HIV infected, n (%) | 2 (0.8) | |
| 5 y risk of cardiovascular event, n (%) | ||
| <10% | 68 (28.2) | |
| ≥10% | 173 (71.8) | |
| Primary ED diagnosis, n (%) | ||
| Symptomatic hypertension | 110 (45.6) | |
| Heart failure | 105 (43.6) | |
| Angina | 11 (4.6) | |
| Acute coronary syndrome | 6 (2.5) | |
| Rheumatic heart disease | 5 (2.1) | |
| Other | 4 (1.7) | |
Table 2 presents the healthcare-seeking behaviour reported by participants prior to and following their ED visit. The majority of participants (186 [77.2%]) reported that they had sought care elsewhere for the same illness episode prior to presentation at the KCMC. The median duration of symptoms prior to presentation at the KCMC was 7 d (IQR 3–28). A total of 208 (86.3%) participants completed a 30 d telephone follow-up. Of these, 24 (11.5%) reported that their symptoms had resolved and 16 (7.7%) had died. Most patients who completed follow-up (156 [75.0%]) reported taking their medications as prescribed. Of the 73 patients who were given a follow-up appointment within 30 d of their ED visit, 44 (60.3%) reported that they attended their appointment. Of all patients completing the telephone follow-up, 38 (18.3%) reported that they visited another healthcare facility for the same illness episode following their ED visit.
Table 2.
Patterns of healthcare seeking for adults with CVD presenting to the ED, northern Tanzania, 2018
| All patients (N=241) | Patients, n (%) |
|---|---|
| Prior facilities visited for this illness episode | |
| Another hospital | 129 (53.5) |
| Health centre | 48 (19.9) |
| Self-treatment at home | 28 (11.6) |
| Dispensary | 18 (7.5) |
| Pharmacy | 6 (2.5) |
| Traditional healer | 1 (0.4) |
| None | 55 (22.8) |
| Travel time to the hospital (min), median (IQR) | 60 (30–120) |
| Symptom duration before presentation (d), median (IQR) | 7 (3–28) |
| Participants completing telephone follow-up (N=208) | |
| Symptom status at 30 d | |
| Resolved | 24 (11.5) |
| Improved | 128 (61.5) |
| Worsened or unchanged | 40 (19.2) |
| Death | 16 (7.7) |
| Reports taking medication as prescribed | 156 (75.0) |
| Given follow-up appointment within 1 mo | 73 (35.1) |
| Attended follow-up appointment (N=73) | 44 (60.3) |
| Had unscheduled visit to another facility for persistent symptoms within 30 d following ED visit | 38 (18.3) |
| Feels they understand their diagnosis | 99 (47.6) |
| Patient-reported diagnosis consistent with physician-documented diagnosis | 45 (21.6) |
| Feels they understand their treatment and necessary lifestyle modifications | 87 (41.8) |
| Received a prescription from the ED (N=141) | |
| Able to identify any medication prescribed from the ED | 11 (7.8) |
| Able to identify all medications prescribed from the ED | 2 (1.4) |
Of the 208 participants completing follow-up, fewer than half reported that they understood their diagnosis (99 patients [47.6%]) or the necessary treatment and lifestyle modifications needed for their disease (87 patients [41.8%]). When compared with the physician-documented diagnoses in the medical record, only 45 (21.6%) patients were able to identify or describe their diagnosis accurately. Of the 141 patients who received a prescription from the ED, only 11 (7.8%) were able to identify any medication prescribed by their ED physician and only 2 (1.4%) were able to identify all of the medications prescribed.
Table 3 presents associations between various patient characteristics and symptom improvement 30 d after ED presentation. Among patients completing the follow-up, symptom improvement or resolution was not associated with age, sex or overall cardiovascular risk. However, symptom improvement was associated with medication compliance (OR 4.68, p<0.001), patient understanding of their diagnosis (OR 2.39, p=0.007), patient understanding of their treatment (OR 5.40, p<0.001) and better knowledge of CVD (p=0.008). Patients with an ED diagnosis of heart failure were significantly less likely to report symptom improvement at 30 d (OR 0.35, p<0.001). On multivariable logistic regression, understanding treatment (OR 3.72 [95% CI 1.63 to 9.17], p=0.003), medication compliance (OR 3.46 [95% CI 1.60 to 7.57], p=0.002) and not having a diagnosis of heart failure (OR 0.36 [95% CI 0.17 to 0.76], p=0.008) were predictive of survival with symptom improvement at 30 d.
Table 3.
Predictors of self-reported improvement in symptoms among patients with CVD 30 d following an ED visit, northern Tanzania, 2018
| Patients with symptom improvement or resolution (N=152), n (%) | Patients who died or had no symptom improvement (N=56), n (%) | OR (95% CI) | p-Valuea | |
|---|---|---|---|---|
| Male | 56 (36.8) | 27 (48.2) | 0.63 (0.34 to 1.17) | NS |
| ≥10% 5 y risk of cardiovascular event | 109 (71.7) | 40 (71.4) | 1.02 (0.50 to 1.99) | NS |
| ED diagnosis of heart failure | 53 (34.9) | 34 (60.7) | 0.35 (0.18 to 0.65) | <0.001* |
| Compliant with medications | 127 (83.6) | 29 (51.8) | 4.68 (2.38 to 9.33) | <0.001* |
| Patient feels they understand their diagnosis | 81 (53.3) | 18 (32.1) | 2.39 (1.26 to 4.65) | 0.007* |
| Patient feels they understand the necessary treatment | 78 (51.3) | 9 (16.1) | 5.40 (2.57 to 12.57) | <0.001* |
| Patients with symptom improvement or resolution (N=152), mean (SD) | Patients who died or had no symptom improvement (N=56), mean (SD) | p-Valueb | ||
| Age (y) | 58.5 (18.0) | 60.1 (18.1) | NS | |
| CVD knowledge score | 5.5 (3.1) | 4.1 (3.3) | 0.008* |
NS: not significant.
p<0.05.
Univariate analyses of categorical predictor variables were assessed via Pearson’s χ2 test.
Univariate analyses of continuous predictor variables were assessed via Welch’s t-test.
Table 4 summarizes the barriers to care identified by participants. The most common pre-hospital barrier resulting in delayed presentation was a lack of awareness of the seriousness of their symptoms, which was cited by 82 patients (34.0%). The most common in-hospital barrier to care identified by living participants completing the follow-up was long wait times (65 patients [33.9%]). The most common post-hospital barrier to care mentioned by participants was intolerable medication side effects (43 patients [22.4%]). Figure 2 summarizes barriers to care and associated health outcomes.
Table 4.
Barriers to care identified by patients with CVD presenting to the ED, northern Tanzania, 2018
| All enrolled patients (N=241) | Patients, n (%) | |
|---|---|---|
| Pre-hospital barriers to prompt presentation | ||
| Did not think symptoms were serious | 82 (34.0) | |
| Concerns about cost of care | 24 (10.0) | |
| Responsibilities at home or work | 21 (9.7) | |
| Trouble finding or affording transportation | 22 (9.1) | |
| Other | 28 (11.6) | |
| Living patients completing telephone follow-up (N=192) | ||
| In-hospital barriers to care | ||
| Long wait times | 65 (33.9) | |
| Uncaring, rude or lazy staff | 23 (12.0) | |
| Insufficient treatment or counselling | 15 (7.8) | |
| Cost of testing and treatment | 12 (6.3) | |
| Other | 6 (3.1) | |
| Post-hospital barriers to care | ||
| Intolerable medication side effects | 43 (22.4) | |
| Cost of follow-up care | 13 (6.8) | |
| Finding/affording transportation for follow-up appointments | 12 (6.3) | |
| Other | 29 (15.1) | |
Figure 2.

Barriers to cardiovascular care and associated health outcomes in northern Tanzania, 2018.
Discussion
This study is among the first to explore healthcare-seeking behaviour, barriers to care and predictors of symptom improvement among patients with CVD in SSA. We found that in northern Tanzania, the majority of patients with acute CVD visit multiple facilities for the same illness episode and prolonged delays prior to hospital presentation are common. Moreover, we found that most patients do not understand their diagnosis or their treatment and that such understanding is predictive of symptom improvement. Finally, we found that the most frequently encountered patient-perceived barriers were lack of patient awareness of the seriousness of their symptoms, long in-hospital wait times and medication side effects. Together, these findings highlight the urgent need for patient-centred interventions at the patient, hospital and healthcare system levels to improve the quality of care for CVDs in Tanzania.
More than three-quarters of participants had visited another healthcare facility for the same illness episode prior to presentation to the ED and nearly one in five visited another facility within a month following their ED visit for the same symptoms. This observation suggests that patients with acute CVD struggle to efficiently navigate the healthcare system in northern Tanzania and rarely receive sufficiently beneficial treatment at their first healthcare encounter. This finding underscores a need to improve quality of CVD care at first-line facilities and to streamline referral processes for patients requiring advanced CVD care. Given existing data demonstrating that many healthcare facilities in Tanzania lack both the equipment and expertise to manage CVDs,6,7 making improvements in first-line care and the referral system would likely require both educational and infrastructural interventions. In 2016, the Tanzanian Ministry of Health released a strategic plan to combat CVD, which included an emphasis on health system strengthening;19 the findings presented here highlight the importance of this mission. To our knowledge, there has been little prior study of healthcare seeking for CVD in SSA, but additional research is needed to determine if patients with acute CVD in other settings in SSA exhibit similar patterns of care seeking. In a study of patients with severe febrile illness in Tanzania, visiting multiple facilities for the same febrile illness was found to be common and associated with increased odds of mortality.20 If a similar association exists for CVD, then streamlining the referral system may have the potential to reduce mortality due to both communicable and non-communicable diseases in Tanzania.
Only a minority of patients in this study felt that they understood their diagnosis or treatment, and fewer than a quarter of patients could accurately identify their diagnosis or medications. To our knowledge, this is the first assessment of patient understanding of their own CVD in SSA, and the results are concerning. Although ensuring patient comprehension of their disease is challenging even in high-income settings, the proportion of patients able to identify their diagnosis in our study was particularly low. In a recent study in the UK, for example, more than half of patients with heart failure were able to describe their disease as involving damaged heart muscle.21 Thus, in Tanzania, efforts are needed to improve provider–patient communication in order to increase patient comprehension of both their disease and treatment. Numerous strategies have been developed in countries outside of SSA to improve patient understanding of CVDs,22,23 and additional research is needed to adapt such strategies to the Tanzanian context.
Thirty days after their ED visit, only 11% of patients had symptom resolution, although the majority reported symptom improvement. The 30 d mortality rate among participants in this study (7.7%) was high, approximately 100-fold higher than the 0.08% 30 d community mortality rate for adults in Kilimanjaro.24 This high level of mortality warrants urgent attention from public health officials and researchers alike to improve the quality of CVD care in Tanzania. Most of the important predictors of 30 d survival with symptom improvement evaluated in this study were related to patient comprehension, including understanding the diagnosis, understanding the treatment, general CVD knowledge and medication compliance. Interestingly, well-established predictors of cardiovascular outcomes like age and overall cardiovascular risk were less important than these patient-centred factors in our study. The fact that patient comprehension and knowledge were significantly associated with symptom improvement emphasizes the importance of patient education and provider–patient communication in Tanzania, and further study is needed to determine whether these patient-centred factors are associated with long-term outcomes.
In settings outside SSA, there has been extensive study of the effect of patient knowledge and understanding on CVD outcomes, and the results have been mixed: although increased health literacy and comprehension of one’s diagnosis has often been linked with increased uptake of positive health behaviours, such knowledge and comprehension has rarely been found to improve clinical outcomes.23,25 The correlation between greater patient understanding and improved CVD outcomes observed in our study suggests that factors related to patient self-efficacy may be relatively more important in countries like Tanzania with a less developed healthcare infrastructure. Additional study is needed across SSA to determine whether the associations observed here exist in other low-income settings. Patients diagnosed with heart failure were significantly less likely to report survival with symptom improvement at 30 d, thus particular attention is needed to improve care for these patients.
The most common patient-identified barriers to care in our study were lack of recognition of symptom seriousness, long in-hospital wait times and medication side effects. Patients cited unawareness of the seriousness of their symptoms as the primary reason for the delayed hospital presentation. This is consistent with prior community-based research from northern Tanzania that found very few patients recognized cardiovascular causes of chest pain and shortness of breath,26,27 and underscores the need for community education regarding symptoms of cardiovascular disease and appropriate care seeking for such symptoms. Beyond symptom knowledge, a complex set of factors likely contributes to delayed care seeking in this population, and additional theory-based research is needed to identify other modifiable determinants of pre-hospital delays among patients with acute CVD in Tanzania.28 The fact that medication side effects were the most commonly cited post-hospital barrier to care suggests that there is a need for pre-emptive counselling regarding potential side effects at the time of prescription or dispensation and special attention to side effects during follow-up care. Such efforts would presumably improve medication compliance, which was associated with greater odds of survival with symptom improvement in our study.
To our knowledge, few studies have examined barriers to cardiovascular care in SSA from the patient’s perspective. A qualitative study of patients with heart failure in Kenya found that the cost of care and lack of information about their disease were primary patient-perceived barriers.29 Although patients in our study did not identify a lack of information about their disease when asked to identify barriers in an open-ended fashion, the fact that only a minority of them understood their diagnosis or treatment indicates that this was a barrier to care in our patient population as well. Further research is needed across SSA to describe and minimize barriers to cardiovascular care. Additional studies utilizing qualitative methods are particularly needed to further illuminate patient perspectives on healthcare seeking and barriers to care for CVD in SSA.
This study had several limitations. First, the 30 d follow-up was conducted via telephone, which presumably resulted in underrepresentation of lower income patients and those who had died. This likely produced an underestimation of the 30 d mortality rate. Second, we depended on patient self-reports to measure patient behaviours such as compliance with medications and follow-up. As patients’ responses to these questions may have been affected by social desirability bias, we may have overestimated the proportion of patients who were adherent with their medications and who attended scheduled follow-up appointments. We also relied on patient self-reports when assessing for cardiovascular risk factors such as diabetes and hyperlipidaemia. As large majorities of those with comorbidities such as diabetes in SSA are unaware of their disease,30 this likely resulted in an underestimation of the overall cardiovascular risk profile of our patient population. Furthermore, this study only included patients presenting with chest pain or shortness of breath; as not all cardiovascular events present with these symptoms, the findings presented here may not be representative of the full spectrum of CVD in Tanzania. Finally, we required a physician-documented clinical diagnosis of CVD for study inclusion, but the accuracy of these clinical diagnoses could not be assessed without access to results of diagnostic testing. Misdiagnoses of CVD could have led to inappropriate exclusion of patients with CVD or inclusion of those without CVD.
Conclusions
Patients with acute CVD in northern Tanzania often visit multiple healthcare facilities after prolonged delays. Only a minority of these patients leave the hospital with an understanding of their diagnosis and treatment, but those that have such an understanding are more likely to survive with symptom improvement. Barriers to cardiovascular care include inadequate patient education, long in-hospital wait times and poorly managed medication side effects. Patient-centred interventions are needed to improve the quality of acute cardiovascular care in Tanzania.
Authors’ contributions:
JTH, NMT and JAB conceived the study. GLK recruited participants and administered questionnaires. JTH, FMS and GT supervised the study. JTH and ZL performed the data analysis. JTH and ZL drafted the manuscript. FMS, GLK, NMT, GT and JAB critically revised the manuscript for intellectual content. All authors read and approved of the final manuscript. JTH and JAB are guarantors of the paper.
Acknowledgements:
None.
Funding:
This study received support from the US National Institutes of Health Fogarty International Center (grant D43TW009337).
Competing interests:
None declared.
Ethical approval:
This study was conducted in accordance with the ethical standards of the Helsinki Declaration. This study received ethical approval from the Duke Health Institutional Review Board, the Kilimanjaro Christian Medical Centre Research Ethics Committee and the Tanzania National Institutes for Medical Research Ethics Coordinating Committee. All participants provided informed consent prior to enrolment.
Abstract
- 1. Naghavi M. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tibazarwa K, Ntyintyane L, Sliwa K, et al. A time bomb of cardiovascular risk factors in South Africa: results from the Heart of Soweto Study “Heart Awareness Days”. Int J Cardiol. 2009;132(2):233–9. [DOI] [PubMed] [Google Scholar]
- 3. Onen CL. Epidemiology of ischaemic heart disease in sub-Saharan Africa. Cardiovasc J Afr. 2013;24(2):34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mensah GA, Roth GA, Sampson UK, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26(2 Suppl 1):S6–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nkoke C, Luchuo EB. Coronary heart disease in sub-Saharan Africa: still rare, misdiagnosed or underdiagnosed? Cardiovasc Diagn Ther. 2016;6(1):64–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Masanja H, Smithson P, Ipuge Y. Tanzania Service Availability and Readiness Assessment (SARA) 2012. Dar es Salaam: Ifakara Health Institute, Tanzania Ministry of Health and Social Welfare; 2013.
- 7. Leung C, Aris E, Mhalu A, et al. Preparedness of HIV care and treatment clinics for the management of concomitant non-communicable diseases: a cross-sectional survey. BMC Public Health. 2016;16:1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nyaga UF, Bigna JJ, Agbor VN, et al. Data on the epidemiology of heart failure in sub-Saharan Africa. Data Brief 2018;17:1218–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kingery JR, Yango M, Wajanga B, et al. Heart failure, post-hospital mortality and renal function in Tanzania: a prospective cohort study. Int J Cardiol. 2017;243:311–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okello S, Rogers O, Byamugisha A, et al. Characteristics of acute heart failure hospitalizations in a general medical ward in southwestern Uganda. Int J Cardiol. 2014;176(3):1233–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akintoye E, Briasoulis A, Egbe A, et al. National trends in admission and in-hospital mortality of patients with heart failure in the United States (2001–2014). J Am Heart Assoc. 2017;6(12):e006955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Galson SW, Staton CA, Karia F, et al. Epidemiology of hypertension in northern Tanzania: a community-based mixed-methods study. BMJ Open. 2017;7(11):e018829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stanifer JW, Cleland CR, Makuka GJ, et al. Prevalence, risk factors, and complications of diabetes in the Kilimanjaro region: a population-based study from Tanzania. PLoS One. 2016;11(10):e0164428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . WHO STEPS Instrument. The WHO STEPwise approach to noncommunicable disease risk factor surveillance (STEPS). Geneva: World Health Organization; 2003. [Google Scholar]
- 15. World Health Organization . Global recommendations on physical activity for health. https://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng.pdf(accessed 12 July 2019]. [PubMed]
- 16. Hertz JT, Sakita FM, Manavalan P, et al. Knowledge, attitudes, and preventative practices regarding ischemic heart disease among emergency department patients in northern Tanzania. Public Health. 2019;175:60–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gaziano TA, Young CR, Fitzmaurice G, et al. Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I follow-up study cohort. Lancet. 2008;371(9616):923–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gaziano TA, Abrahams-Gessel S, Alam S, et al. Comparison of nonblood-based and blood-based total CV risk scores in global populations. Glob Heart 2016;11(1):37–46.e2. [DOI] [PubMed] [Google Scholar]
- 19. Ministry of Health , Community Development, Gender, Elderly and Children. Strategic and action plan for the prevention and control of non communicable diseases in Tanzania 2016–2020. Dar es Salaam: Tanzania Ministry of Health, Community Development, Gender, Elderly and Children; 2016.
- 20. Snavely ME, Maze MJ, Muiruri C, et al. Sociocultural and health system factors associated with mortality among febrile inpatients in Tanzania: a prospective social biopsy cohort study. BMJ Glob Health. 2018;3(1):e000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Banerjee P, Gill L, Muir V, et al. Do heart failure patients understand their diagnosis or want to know their prognosis? Heart failure from a patient's perspective. Clin Med. (Lond). 2010;10(4):339–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oates DJ, Paasche-Orlow MK. Health literacy: communication strategies to improve patient comprehension of cardiovascular health. Circulation. 2009;119(7):1049–51. [DOI] [PubMed] [Google Scholar]
- 23. Safeer RS, Cooke CE, Keenan J. The impact of health literacy on cardiovascular disease. Vasc Health Risk Manag 2006;2(4):457–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. National Bureau of Statistics . United Republic of Tanzania mortality and health. Dar es Salaam: National Bureau of Statistics; 2015. [Google Scholar]
- 25. Aaby A, Friis K, Christensen Bet al. Health literacy is associated with health behaviour and self-reported health: a large population-based study in individuals with cardiovascular disease. Eur J Prev Cardiol. 2017;24(17):1880–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hertz JT, Madut DB, Tesha RA, et al. Perceptions of chest pain and healthcare seeking behavior for chest pain in northern Tanzania: a community-based survey. PLoS One. 2019;14(2):e0212139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hertz JT, Madut DB, Tesha RA, et al. Knowledge of myocardial infarction symptoms and perceptions of self-risk in Tanzania. Am Heart J. 2019;210:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cornally N, McCarthy G. Help-seeking behaviour: a concept analysis. Int J Nurs Pract. 2011;17(3):280–8. [DOI] [PubMed] [Google Scholar]
- 29. Kimani KN, Murray SA, Grant L. Multidimensional needs of patients living and dying with heart failure in Kenya: a serial interview study. BMC Palliat Care. 2018;17(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Manne-Goehler J, Atun R, Stokes A, et al. Diabetes diagnosis and care in sub-Saharan Africa: pooled analysis of individual data from 12 countries. Lancet Diabetes Endocrinol 2016;4(11):903–12. [DOI] [PubMed] [Google Scholar]


