Abstract
Background
A community-based approach has been identified as one key strategy to improve the health of Indonesians. In 2015, the government initiated the ‘Smart Use of Medications Movement’ (GeMa CerMat) to promote responsible self-medication. This study aims to explore pharmacist/pharmacy staff trainers’ views on strategies to implement GeMa CerMat community training.
Methods
Four focus group discussions were conducted with 38 pharmacist/pharmacy staff trainers in Ngawi, Indonesia and a thematic analysis was used to obtain the key strategies.
Results
The identified key strategies were building community readiness via well-designed training (considering participant characteristics, training methods, and materials and resources); policy, regulation and organizational support; access to training in a cultural context; communication media to promote training and the inclusion of active-learning tools.
Conclusions
These identified multilevel strategies require collaboration among national bodies and the involvement of trusted community members (‘change agents’). A new strategy using ‘active learning tools’ was necessary to build critical thinking and understanding of the use of medications in everyday life. Future research should focus on process, impact and outcome evaluation involving GeMa CerMat training implementation and sustainability in Indonesia.
Keywords: education, Indonesia, pharmacist, self-medication
Introduction
Indonesia is the world’s largest island nation with a population of >200 million.1 With an increasing ageing population and prevalence of non-communicable diseases, in conjunction with the high prevalence of infectious diseases, health challenges in Indonesia are daunting.2 It is a priority of the Indonesian government to improve the quality of life among Indonesians through a ‘Healthy Indonesia’ programme, including promoting a healthy living paradigm, strengthening health services/facilities and implementing Jaminan Kesehatan Nasional (JKN), which provides basic healthcare coverage to the entire population.3 Primary care facilities, mainly primary health centres (PHCs, puskesmas), are the front-line providers to implement these programmes. However, the wide dispersion of islands making up Indonesia creates problems with supply, mix and distribution of primary health facilities and workforce.2,3 Thus community empowerment could be seen as one key strategy to improve the health of Indonesians.2
In 2015, the Indonesian government initiated a community empowerment programme, the ‘Smart Use of Medications Movement’ (Gerakan Masyarakat Cerdas Menggunakan Obat [GeMa CerMat]), which aimed to promote responsible self-medication among Indonesians;4 this was followed by an overarching programme, the ‘Healthy Lifestyle Movement’ (Gerakan Masyarakat Hidup Sehat [GerMas]) to include self-care.5 Self-medication is defined as ‘the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms’.6 Due to the overstretched health system in Indonesia,2 self-medication plays a pivotal role as the first action taken by Indonesians in managing their healthcare, especially for minor ailments. Minor ailments can be defined as usually self-limiting medical conditions that can be reasonably self-diagnosed and self-managed with over-the-counter (OTC) products; this might include headache, coughs, colds and constipation.7 Based on a survey in 2014, 61% of the Indonesian population practises self-medication.8
While responsible self-medication can move people toward greater independence to treat their minor ailments, potential risks of self-medication have been reported, such as incorrect self-diagnosis, drug interactions, infrequent but severe adverse reactions, incorrect choice of therapy and risk of drug dependence and abuse.9,10 Community pharmacists are well established in Indonesia and have traditionally assisted the community with the management of minor ailments and, when appropriate, referred them to other health practitioners; however, many medicines are also available from drugstores, informal outlets and street peddlers.2 Hence the GeMa CerMat initiative is expected to improve self-medication literacy, thus empowering Indonesians in the safe use of OTC medicines.
As part of the GeMa CerMat initiative, community training on basic medication information was developed.4 Pharmacists, with their educational background in medications and as suppliers of OTC medicines, are appropriate healthcare practitioners for providing community training. In 2016, selected pharmacists/pharmacy staff were invited for a GeMa CerMat trainers’ briefing in four cities/districts: Nganjuk, Blitar, Ngawi and Sumenep.11 Little is known, however, regarding pharmacist/pharmacy staff trainers’ experiences (barriers/facilitators) while performing the community training in their practice settings. This study aims to explore trainers’ views on strategies to implement GeMa CerMat community training to promote responsible self-medication in Indonesia.
Methods
The study was approved by the ethics committee of the Faculty of Medicine, Islamic University of Indonesia (No. 08/Ka.Kom.Et/70/KE/IX/2016).
Setting, design and sample
The study site was Ngawi, a district (kabupaten) in the western part of East Java province, Indonesia. Based on statistical data from 2012,12 Ngawi covers an area of 1296 km2 with a population of 911 911 people and is divided into 17 subdistricts (kecamatan) consisting of 217 villages (desa). Health facilities in Ngawi include 2 hospitals, 24 PHCs and 51 community pharmacies; a PHC is a technical unit of the Region Health Office that provides primary healthcare at a subdistrict level. In 2016, 46 pharmacist/pharmacy staff in Ngawi were invited to attend a GeMa CerMat trainers’ briefing. A module was provided to guide trainers to facilitate interactive learning on basic medication information provided on the label/package/leaflet (i.e. drug name, indication, administration, adverse effects and storage).11
This study was to follow up pharmacists/pharmacy staff involved in the prior trainers’ briefing in Ngawi to explore their views on strategies to implement community training to promote responsible self-medication in Indonesia. Focus group discussions (FGDs) were chosen since this allowed the trainers, who had similar backgrounds or experiences, to discuss a specific topic of interest.13 Thus FGDs are a good way to provide insights into a range of views/opinions of people involved in the change process, especially where the aim is to improve a targeted service. These were guided by the Consolidated Criteria for Reporting Qualitative Research (COREQ) requirements.14
Data collection
Invitation letters were sent by the head of the Pharmacy Division of the Ngawi Health Office to a total of 46 pharmacist/pharmacy staff who had participated in the prior GeMa CerMat trainers’ briefing to attend a meeting that was scheduled in May 2017. The meeting was conducted in the Ngawi Health Office. The researcher initially introduced the research and asked for the trainers’ participation. Those willing to participate were asked to complete a short demographic questionnaire and to provide written informed consent. They were then invited to join one of four FGDs.
Each FGD was facilitated by one of the researchers, who were a master/doctor in pharmacy as well as an academic. All FGDs were conducted in Bahasa Indonesia and were aided by a semi-structured FGD guide. The guide was developed in conjunction with all researchers and was field tested. The guide explored two areas: training experiences (barriers/facilitators) and proposed strategies to implement the community training. Probing questions were asked when necessary to expand on the participants’ responses. The FGDs lasted 45–60 min and were audio recorded.
Data analysis
Audio-recorded data from the FGDs were transcribed verbatim by the facilitators. Transcripts were reviewed using inductive thematic analysis to identify salient themes;15 all transcripts were coded manually by cutting and pasting between documents. The analysis was performed by YW and the emerging themes were validated by discussion with the other research team members (AP, ES) to reach a consensus. The data analysis first involved a process of familiarization; significant statements related to proposed strategies to implement community training from the data were then identified and coded. The codes were categorized into a broader conceptual level (i.e. into themes). The process of theme generation was reviewed and refined by going back and forth between the themes, the codes and the transcripts until the final themes were identified. Finally, examples of responses were selected to illustrate each theme. The final themes and quotes were discussed with the trainers during a follow-up seminar in October 2017 as a means of member-checking, thus ensuring the credibility of the data.16 Data analysis was conducted in Bahasa Indonesia and the illustrative verbatim quotes and theme labels were translated into English.
Results
Of 46 pharmacists/pharmacy staff who participated in the prior trainers’ briefing and were thus invited to participate in this study, a total of 40 consented and attended a meeting held in the Ngawi Health Office in May 2017. Two subsequently withdrew due to emergency work tasks, leaving 38 who were allocated to join four FGDs (their characteristics are summarized in Table 1).
Table 1.
Characteristics of the pharmacist/pharmacy staff trainers involved in the FGDs
| Characteristics | FGD 1 (n=10) | FGD 2 (n=9) | FGD 3 (n=10) | FGD 4 (n=9) |
|---|---|---|---|---|
| Age range (years) | 30–48 | 29–39 | 30–51 | 25–41 |
| Gender | 3 males, 7 females | 9 females | 3 males, 7 females | 9 females |
| Position | 2 PHC pharmacists, 3 community pharmacists, 5 PHC pharmacy staff | 2 PHC pharmacists, 2 community pharmacists, 5 PHC pharmacy staff | 2 PHC pharmacists, 8 PHC pharmacy staff | 5 community pharmacists, 4 PHC pharmacy staff |
| Training experience | ||||
| – Number of training sessions (range per person) | 1–4 | 1–4 | 1–3 | 1–3 |
| – Training participants | ||||
| Participant characteristics | Seniors (1 time), members of women's organizations (1–3 times), members of religious gathering (1 time), community health representatives/leaders (1 time), general population (1–2 times) | Seniors (1–2 times), members of women's organizations (1–3 times), community health representatives/leaders (1 time), students (1–2 times), general population (1 time) | Seniors (1–2 times), members of women's organizations (1–3 times), community health representatives (1 time), general population (1–2 times) | Community health representatives/leaders (1 time), general population (1–2 times) |
| Number of participants (range) | 30–100 | 15–200 | 15–100 | 15–100 |
Trainers, perceived strategies to implement community training
Pharmacists/pharmacy staff involved in the FGDs had been involved in at least one training session as trainers (range 1–4 sessions per person); while the training sessions were often conducted during community meetings, including meetings of women’s organizations, senior gatherings, religious gatherings, educational sessions at school or community health representative/leader meetings (see Table 1). Responses from the FGDs in relation to the trainers’ perceived strategies to implement training to promote responsible self-medication in Ngawi identified five main themes: building community readiness via well-designed training; policy, regulation and organizational support; access to training in a cultural context; communications media and active learning tools.
Building community readiness via well-designed training
This study indicated the importance of designing appropriate training to build community readiness to practise responsible self-medication. It was suggested that factors directly contributing to training delivery were participant characteristics, training methods, and materials and training resources.
Participant characteristics
Participant characteristics might be linked with learning capacity and motivation. This should be considered when delivering training to promote responsible self-medication. Some of the trainers believed that it would be best for the training to be targeted to specific participant groups, thus the training could be designed accordingly. Community health representatives, community leaders, students or mothers could be considered as the initial targets; these groups generally have higher learning capacity and/or influence, thus having the potential to assist pharmacists to implement community training in their local communities (‘change agents’). This was illustrated by comments from pharmacist 4.4: ‘The first would be community health representatives. Every year, we are given the opportunity to speak at community health representatives meetings – we usually use it to present GeMa CerMat’; pharmacist 2.9: ‘Usually, community leaders would have better capability – even asking extended questions’; pharmacist 4.3: ‘Clearly, I would prioritise mothers; as in general, they were the ones who take the initiative when their children were ill’; and pharmacist 2.8: ‘In my opinion, we need to target high-school students; younger people have higher capability to learn and could assist their family on using medications properly’.
Training methods and materials
Training methods and materials should be made to fit participant characteristics. Due to the oral traditions among the Ngawi communities, some trainers suggested interactive methods with oral and fewer written tasks for the participants, such as using games, question-and-answer sessions, pictures/videos or simulations using medication packages. This was illustrated by comments from pharmacy staff 3.4:,Usually the participants are mothers…they are reluctant to do writing tasks; they want us to do questions and answers…just like discussion’; and pharmacist 2.9: ‘To attract high school students’ interests, I am not using slides instead I am adding some videos’.
Further, a few trainers indicated the importance of developing a range of training guides focusing on specific or local health issues, e.g. anaemia in pregnancy, diarrhoea or the common cold. It was suggested that trainers, to bridge the literacy gap with participants, should use simple language when delivering the material; as pharmacist 1.8 stated: ‘In some cases, we need to adjust – using language that could be easily understood, even using local dialects etc.’.
Training resources
Training resources refers to resources needed to perform self-medication training, including trainers, funding and facilities. Some trainers revealed that the current GeMa CerMat community training is not yet a priority activity of the local health office or the Indonesian Pharmacists Association (Ikatan Apoteker Indonesia [IAI]), thus permanent funding has not been established. To obtain the facilities required for the training, the training was often conducted along with other established community meetings, such as community health representative meetings, religious gatherings, health education sessions (at school) or neighbourhood meetings, as illustrated by pharmacist 2.8: ‘We have routine activities such as providing health education at schools and we usually include GeMa CerMat there’.
Adequate numbers of trainers should be available to facilitate efficient interactive discussion; as pharmacy staff 3.4 stated: ‘Ideally one group is facilitated by one trainer’. Few trainers also perceived the importance of setting skill qualifications for those who are allowed to be trainers, such as pharmacists or having completed the trainers’ briefing, as illustrated by pharmacy staff 4.2: ‘I am a diploma graduate, thus my clinical role is limited, sometimes the participants know more than me. It would be better to have a pharmacist’.
Policy, regulation and organizational supports
Despite the Indonesian government’s initiative, GeMa CerMat community training has not been necessarily translated into the local health office and/or IAI policies and priority programmes. This was illustrated by comments from pharmacist 2.8: ‘At PHC, 60% are primary activities and 40% are supporting activities. Pharmacy is only included within supporting activities’; and pharmacist 4.3: ‘Community pharmacists usually involve (to introduce GeMa CerMat) in their local community activities on their own initiatives’.
Only after the training was viewed as a priority or routine activity within the local health office and/or IAI did some trainers believe that permanent funding would be established for sustained community training. Further, it was suggested that the IAI develop a remuneration system for pharmacists involved as trainers, such as incentives and/or continuing professional development (CPD) credits.
Access to training in a cultural context
Access to training and various cultural influences might affect the implementation of community training. Trainers emphasized the issues of oral language traditions among target communities; this sociocultural context should guide the development of appropriate training methods and materials (see ‘Training methods and material’). In addition, limited access to training—due to isolated and scattered residential areas—was also considered a barrier; as pharmacy staff 1.5 stated: ‘I am residing in an isolated area, in the forest, very rural. Gathering 50 people would be very difficult, (as) they have scattered residences, long distances between them, lots of forest’. Thus it was suggested to involve community health representatives/leaders in local areas to assist in training implementation to reach a broader population.
Communication media
Some trainers indicated the importance of the local health office in collaboration with the IAI to communicate or disseminate the GeMa CerMat programme to increase awareness of the target community; as pharmacist 4.3 stated: ‘On a special occasion, such as World Pharmacist Day, the local IAI could promote “GeMa CerMat”, such as installing banners at pharmacies, sharing via social media, radio etc.’.
Active learning tools
While participatory and interactive training materials might help participants to learn about medications, some concerns were raised regarding community empowerment beyond the training; as pharmacist 1.10 mentioned: ‘Participants need to be subsequently evaluated and continuously encouraged to be careful when using medications’. This situation might imply the need for the training to provide community members with a range of active learning tools to build their critical thinking on the use of medications in their daily life.
The five key strategies identified from the FGDs of trainers could be interpreted as an in-process evaluation as part of a cyclical process (assessment–implementation–evaluation) that allows for continuous improvement of a health programme as described in the PRECEDE–PROCEED model.17 Considering the structure of the Indonesian health system,18 the strategy component of ‘policy, regulation and organizational support’ could be further explained in terms of a pyramid model to represent levels of policy, regulation and support needed while implementing the community training (Figure 1). At the top would be the national policy/regulation related to GeMa CerMat, which is then required to be translated down to the regional and local health offices, and the IAI, to reach the target communities.
Figure 1.
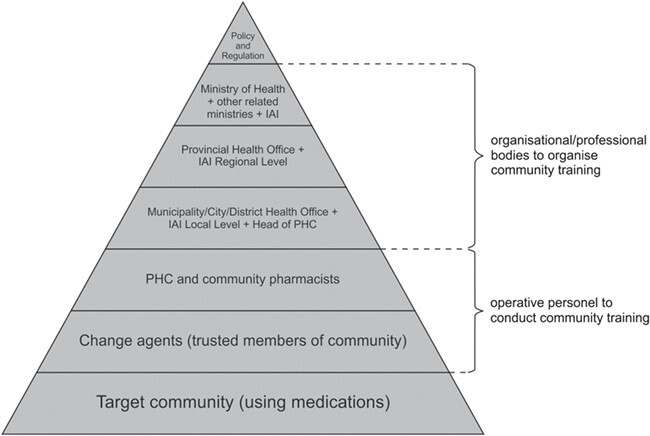
Levels of policy, regulation and organisational support for sustained community training to promote self-medication in Indonesia.
Discussion
Community-based interventions have been identified at the government level as one key strategy to improve the health status of Indonesians. This qualitative study was initiated to follow up pharmacists/pharmacy staff who had previously participated in a trainers’ briefing to explore their views on strategies used to perform community training as an intervention to enhance self-medication in their practice settings. The findings identified five key strategies: building community readiness via well-designed training; policy, regulation and organizational support; access to training in a cultural context; communication media and the inclusion of active learning tools to build critical thinking on the use of medications in everyday life (see Figure 1). These strategies target factors directly related to the training (internal factors) as well as enabling and reinforcing external factors, all of which could produce synergistic effects for a successful implementation.17,19
Building community readiness via a well-designed training model could be seen as a strategy directly related to the training (internal factors). This study indicated that the training should be designed based on group target participant characteristics. Initially the training could target trusted members of the community, such as health representatives/leaders, students or mothers, as they have the potential to assist in the training implementation (‘change agents’) in the household or community groups. This should be facilitated with the development of appropriate training methods and materials. Although the evidence available in the literature was inconclusive on which methods work best for patient education, audio-visual, written materials (prepared at an appropriate reading level), demonstrations (if appropriate for the situation) and the use of mixed methods were considered to be effective.20
While the current training material developed was at the general information level on self-medication use, this could be modified to focus on specific local health groups, such as mothers, or other target participant needs. In addition to common minor illnesses (such as diarrhoea, cough, cold and joint/muscular pain),12,21 the increasing prevalence of diabetes and hypertension in Indonesia also warrants consideration in developing training materials related to a healthy lifestyle. This should provide self-care support to the current priority health programme, GerMas, which was introduced after GeMa CerMat.5 In addition to the improved materials, this study implied the need to provide the training participants with active learning tools. The tools should facilitate community members to be actively and critically able to obtain information from health professionals, for example, ‘Asking 5+’ when obtaining medications:22
Name and composition—what is the name and composition of this medication?
Indication—what is this medication used for?
Directions for use—how do I use this medication?
Side effects—what are the common side effects of this medication?
Storage—how to store this medication?
+ the expiry date.
Past research has suggested a continuous process of discussion, reflection and action, termed ‘critical awareness’ and ‘critical thinking’, forming the basis for approaches for learning and social change.23
Access to training in a cultural context relates to strategies to enable implementation of the training across the district. Considering Indonesia’s communal and paternalistic culture as well as geographic proximity between areas,24,25 it would be best to integrate the educational programme into local community activities, thus the involvement of trusted members of the community, such as community health representatives/leaders, would be of importance. Studies worldwide have reported that pupils can act as agents for health interventions at both the school and local community levels (‘change agents’).25–27 As part of the community, these change agents would be more accessible and acceptable to the local community.26
Furthermore, this study has suggested strategies related to ‘public policy and organizational support’ and ‘communication media’ to reinforce sustained community training (reinforcement factors). Although the Indonesian government initiated GeMa CerMat in 2015,4,11 a key challenge lies in translating the movement into local regulations/policies. Indonesia’s decentralized government system provides districts (kabupaten) and municipalities (kota) with autonomy to manage regional public sectors, including health.28 Hence GeMa CerMat training should become part of the regional health office’s responsibility for supporting and funding GeMa CerMat training performed at the local community level. In addition, the IAI (in collaboration with the local health office) would have a pivotal role in arranging for the training as well as establishing trainers’ accreditation and remuneration systems.
The importance of communication media to promote community training was raised. Literature has suggested that health programmes may benefit from media campaigns to expose large audiences to focused messages over time;26 however, the decision to use a particular medium should first consider the audiences’ socio-economic and cultural backgrounds.29,30 Considering the oral traditions of the target community in this study, the health office and IAI should make use of audio-visual media (e.g. television and radio advertisements) and social media for training publicity.
There are some limitations to this study. This study only included views of pharmacist/pharmacy staff trainers, thus it might not include views from other stakeholders, such as community members or policymakers. However, as the main providers in this initiative, the views of pharmacist/pharmacy staff trainers should provide insight regarding the strategies to promote responsible self-medication in Indonesia. As qualitative data are a product of the views, experiences and perceptions of the respondents, bias can occur if respondents are not sharing their true responses.13 The FGDs, however, were carefully designed to include participants with similar backgrounds and experiences (pharmacist trainers) and to discuss a common issue (implementation strategy), thus creating a non-intimidating environment where participants should have been able to express their true ideas/opinions. To ensure accuracy, the results of this study were provided to the participating trainers (member checking).15 In addition, no new themes emerged at the third FGD, suggesting saturation was reached.13
Conclusions
This study has proposed a multilevel strategy for sustained community training to promote responsible self-medication within an Indonesian context. There is a need for the training to provide active learning tools to help Indonesians engage in learning activities while obtaining their medications in their daily lives. These findings should be used as a basis to develop a range of interventions to support trainers while implementing community training. Future research should focus on the process, impact and outcome evaluation involving all stakeholders to provide comprehensive and sustainable community training to promote responsible self-medication in Indonesia.
Acknowledgements:
We thank all the participants who took part in this study as well as the chief and staff from the East Java Provincial Health Office and Ngawi District Health Office – Ministry of Health Republic of Indonesia and the Centre of Medicines Information and Pharmaceutical Care (CMIPC) – Faculty of Pharmacy Universitas Surabaya for their technical support in making this study possible.
Authors’ contributions:
AP made contributions to the conception and design of the study. AP, YW, ES and IM facilitated the FGDs and transcribed the data. AP, YW, ES, IM and ASW participated in the data analysis. YW wrote the first draft of the manuscript. BS contributed to the design of the study and interpretation of data. All authors were involved in the revisions to the manuscript and final approval of the version to be published.
Funding:
This work was supported by the Ministry of Research, Technology and Higher Education, Republic of Indonesia (grant no. 27/SP-Lit/LPPM-01/Dikti/FF/V/2017).
Competing interests:
None declared.
Ethical approval:
The data collection instrument and methodology used in this study were approved by the ethics committee of the Faculty of Medicine, Islamic University of Indonesia (No. 08/Ka.Kom.Et/70/KE/IX/2016).
References
- 1. Statistics Indonesia (Badan Pusat Statistik – BPS), National Population and Family Planning Board (BKKBN), Ministry of Health Republic of Indonesia (Kementerian Kesehatan – Kemenkes RI), ICF International . Indonesia Demographic and Health Survey 2012. Jakarta: Indonesia BPS, BKKBN, Kemenkes RI and ICF International, 2013. [Google Scholar]
- 2. Ministry of Health Republic of Indonesia (Kementerian Kesehatan Republik Indonesia – Kemenkes RI) . General guidance on healthy Indonesia program. Jakarta: Indonesia Ministry of Health, 2016. [Google Scholar]
- 3. Republic of Indonesia (Pemerintah Republik Indonesia – Pemerintah RI) . The road to National Health Insurance (JKN). Jakarta: Pemerintah RI; 2012. http://www.tnp2k.go.id[accessed 7 January 2019]. [Google Scholar]
- 4. Ministry of Health Republic of Indonesia (Kementerian Kesehatan Republik Indonesia – Kemenkes RI) . SK Menteri Kesehatan RI Nomor HK.02.02/MENKES/427/2015 tentang Gerakan Masyarakat Cerdas Menggunakan Obat (GeMa CerMat). Jakarta: Kemenkes RI, 2015. [Google Scholar]
- 5. President, Republic of Indonesia (President RI) . Instruksi Presiden Republik Indonesia Nomor 1 Tahun 2017: Gerakan Masyarakat Hidup Sehat. Jakarta: President RI, 2017. [Google Scholar]
- 6. World Health Organization . The role of the pharmacist in self-care and self-medication. Geneva: World Health Organization, 1998. [Google Scholar]
- 7. Pharmaceutical Society of Australia . Delivering safe and sustainable clinical services. https://www.dhhs.tas.gov.au/data/assets/pdf_file/0003/194934/Pharmaceutical_Society_of_Australia.pdf[accessed 16 September 2019].
- 8. Statistics Indonesia (Badan Pusat Statistik – BPS) . Persentase penduduk yang mengobati sendiri selama sebulan terakhir menurut provinsi dan jenis obat yang digunakan, 2000–2014. https://www.bps.go.id/linkTableDinamis/view/id/926[accessed 27 December 2018].
- 9. Hughes C, McElnay J, Fleming G. Benefits and risks of self-medication. Drug Saf. 2001;24(14):1027–1037. [DOI] [PubMed] [Google Scholar]
- 10. Ruiz M. Risks of self-medication practices. Curr Drug Saf. 2010;5(4):315–323. [DOI] [PubMed] [Google Scholar]
- 11. Setiadi A, Wibowo Y, Setiawan E, et al. . Evaluation of a community-based training to promote responsible self-medication in East Java, Indonesia. Int J Pharm Pract. 2019;27(1):63–70. [DOI] [PubMed] [Google Scholar]
- 12. Statistics Ngawi (Badan Pusat Statistik – BPS Kabupaten Ngawi) . Kabupaten Ngawi dalam angka 2012. Ngawi: BPS Ngawi, 2012. [Google Scholar]
- 13. Smith F. Research methods in pharmacy practice. London: Pharmaceutical Press, 2002. [Google Scholar]
- 14. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 15. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 16. Shenton A. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004;22(2):63–75. [Google Scholar]
- 17. Green L, Kreuter M. Health promotion planning: an educational and ecological approach. Mountain View, CA: Mayfield, 2005. [Google Scholar]
- 18. Ministry of Health Republic of Indonesia (Kementerian Kesehatan Republik Indonesia – Kemenkes RI) . Peraturan Menteri Kesehatan Republik Indonesia Nomor 75 Tahun 2014: Pusat Kesehatan Masyarakat. Jakarta: Kemenkes RI; p. 2014. [Google Scholar]
- 19. McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. [DOI] [PubMed] [Google Scholar]
- 20. Friedman J, Cosby R, Boyko S, Hatton-Bauer J, Turnbull G. Effective teaching strategies and methods of delivery for patient education: a systematic review and practice guideline recommendations. J Canc Educ, 2011;26(1):12–21. [DOI] [PubMed] [Google Scholar]
- 21. Statistics Jawa Timur (Badan Pusat Statistik – BPS Provinsi Jawa Timur) . Provinsi Jawa Timur dalam angka 2016. Jakarta: BPS, 2016. [Google Scholar]
- 22. Setiadi A, Wibowo Y, Setiawan EIet al. . Modul pengenalan obat swamedikasi edisi 1 (2017), 1st edn. Surabaya: PIOLK Universitas Surabaya and East Java Provincial Health Office, 2017. [Google Scholar]
- 23. Shrestha S. A conceptual model for empowerment of the female health volunteers in Nepal. Educ Health. 2003;16(3):318–327. [DOI] [PubMed] [Google Scholar]
- 24. Moffatt A. Indonesian cultural profile: An initiative of HACC Multicultural Advisory Service. West End, QL, Australia: Diversicare; 2012. http://www.diversicare.com.au/wp-content/uploads/2015/10/Profile_Indonesian.pdf. [Google Scholar]
- 25. Simovska V, Carlson M. Health-promoting changes with children as agents: Findings from a multiple case study research. Health Educ. 2012;112(3):292–304. [Google Scholar]
- 26. Lehman U, Sanders D. Community health workers: what do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcome of using community health workers. Geneva: World Health Organization, 2007. [Google Scholar]
- 27. Clausen L, Schmidt C, Aagaard-Hansen J, Reinbach H, Toft U, Bloch P. Children as visionary change agents in Danish school health promotion. Health Promo Int. 2018. 10.1093/heapro/day049. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization . Country health system profile: Indonesia. Geneva: World Health Organization, 2007. [Google Scholar]
- 29. Wakefield M, Loken B, Hornik R. Use of mass media campaigns to change health behaviour. Lancet. 2010;376(9748):1261–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. O’Mara B. Social media, digital video and health promotion in a culturally and linguistically diverse Australia. Health Promo Int. 2013;28(3):466–476. [DOI] [PubMed] [Google Scholar]


