Abstract
BACKGROUND
Chronic obstructive pulmonary disease (COPD) and cardiovascular diseases are often comorbid conditions, their co-occurrence yields worse outcomes than either condition alone. This study aimed to investigate COPD impacts on the five-year prognosis of patients with coronary heart disease (CHD) after percutaneous coronary intervention (PCI).
METHODS
Patients with CHD who underwent PCI in 2013 were recruited, and divided into COPD group and non-COPD group. Adverse events occurring among those groups were recorded during the five-year follow-up period after PCI, including all-cause death and cardiogenic death, myocardial infarction, repeated revascularization, as well as stroke and bleeding events. Major adverse cardiac and cerebral events were a composite of all-cause death, myocardial infarction, repeated revascularization and stroke.
RESULTS
A total of 9843 patients were consecutively enrolled, of which 229 patients (2.3%) had COPD. Compared to non-COPD patients, COPD patients were older, along with poorer estimated glomerular filtration rate and lower left ventricular ejection fraction. Five-year follow-up results showed that incidences of all-cause death and cardiogenic death, as well as major adverse cardiac and cerebral events, for the COPD group were significantly higher than for non-COPD group (10.5% vs. 3.9%, 7.4% vs. 2.3%, and 30.1% vs. 22.6%, respectively). COPD was found under multivariate Cox regression analysis, adjusted for confounding factors, to be an independent predictor of all-cause death [odds ratio (OR) = 1.76, 95% CI: 1.15–2.70, P = 0.009] and cardiogenic death (OR = 2.02, 95% CI: 1.21–3.39, P = 0.007).
CONCLUSIONS
COPD is an independent predictive factor for clinical mortality, in which CHD patients with COPD are associated with worse prognosis than CHD patients with non-COPD.
Incidences and mortality of coronary heart disease (CHD) and chronic obstructive pulmonary disease (COPD) have been increasing yearly along with global population aging. Both diseases are becoming the biggest emerging threats for global health. COPD is frequently associated with lowered physical activities, systemic inflammation and increased oxidative stress. It is also one of the most important comorbidities of cardiovascular diseases, in turn resulting in serious consequences for patients with concurrent ischemic heart disease, stroke, arrhythmia, and heart failure.[1]
Previous studies have found that COPD is a risk factor for incidence and mortality likelihood of CHD, in which CHD patients with COPD are at increased risk of hospitalization and death.[2,3] However, large-scale and long-term clinical follow-up studies are lacking to clarify the impact of COPD on CHD patient prognosis. This current study aims to fill in this gap in knowledge, by comparing the incidences of adverse events in CHD patients with COPD or without COPD after percutaneous coronary intervention (PCI) during the five-year follow-up period. The results from our study clarified the impact of COPD on the long-term prognosis of CHD patients who underwent PCI, and highlighted the importance of COPD as an independent predictive factor for adverse post-PCI events.
METHODS
Study Population
Patients with CHD who underwent PCI in 2013 were enrolled and divided into two groups based on the presence or absence of COPD. PCI was administered based on coronary angiography results, and all interventions were conducted according to the standard guidelines.[4] COPD diagnosis was based on the standards listed in the guidelines of the American Thoracic Society/European Respiratory Society.[5] The study was approved by the Institutional Review Board of Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (No.2021-1501) in Beijing, China and in accordance to the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from all study participants.
Patient Follow-up
Incidences of all-cause death and cardiogenic death, as well as myocardial infarction (MI), repeated revascularization (RV), stroke and bleeding events were recorded during the five-year follow-up period. All-cause deaths included deaths caused by any cause, while deaths attributed to a cardiac etiology were considered cardiogenic deaths. MI was defined in accordance with the Third Universal Definition from the American Heart Association,[6] while RV was defined based on the definition from the Academic Research Consortium, entailing the occurrence of multiple revascularization events in response to ischemic events resulting from surgery on any vessel, including PCI.[7] Stroke, including ischemic stroke and bleeding stroke, was diagnosed based on neurological symptoms and imaging data. Bleeding events were quantified according to the Bleeding Academic Research Consortium (BARC) criteria,[8] in which BARC ≥ 2 were included in our study. Major adverse cardiac and cerebral events (MACCEs) were defined as a composite of all-cause death, MI, RV and stroke. All diagnoses and measurements were determined by two independent cardiologists, and disagreement was resolved by consensus.
Statistical Analysis
Continuous variables were presented as mean ± SD, and comparisons between COPD group and non-COPD group were performed using the independent Student’s t-test. Categorical variables were reported as counts (percentages) and the Pearson’s chi-squared test was used to compare groups. Multivariate Cox regression analysis was conducted to clarify whether COPD was independently associated with adverse events, after adjusting for potential confounders which may affect outcomes, including age, sex, body mass index, hypertension, diabetes mellitus, hyperlipidemia, smoking, hemoglobin, platelet count, estimated glomerular filtration rate (eGFR), left ventricular ejection fraction (LVEF), calcium channel blocker (CCB) and proton pump inhibitor use. The results of effect of COPD on clinical outcomes under univariate and multivariate Cox regression analyses were presented as odds ratio (OR) and 95% confidence interval (CI). Kaplan–Meier analysis was performed to assess the cumulative survival proportion among CHD patients with COPD or without COPD. All statistical analyses were performed using SPSS 26.0 (SPSS Inc., IBM, Chicago, IL, USA) and two-sided P-value < 0.05 were considered statistically significant.
RESULTS
Clinical Characteristics
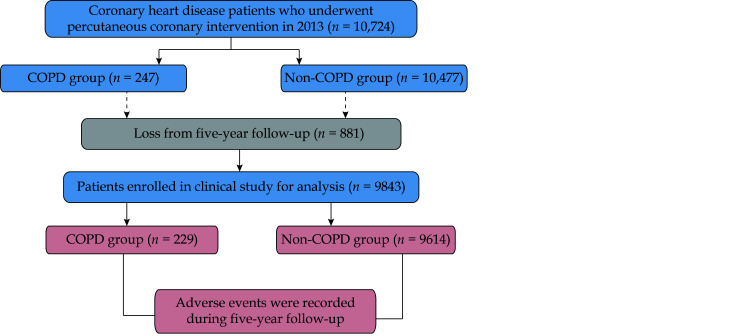
Throughout 2013, 10,724 patients with CHD underwent PCI, and 9843 patients were successfully followed-up during the five-year period, for the follow-up rate of 91.8%. These patients served as the basis for our study (Figure 1). Out of those 9843 patients, 229 patients (2.3%) had COPD and 9614 patients (97.7%) did not. Compared to non-COPD patients, COPD patients were older (65.38 ± 9.13 years vs. 58.27 ± 10.24 years, P < 0.001), had lower hemoglobin levels (136.55 ± 16.03 g/L vs. 141.09 ± 15.84 g/L, P < 0.001), lower platelet counts (194.73 ± 50.27 × 10 9/Lvs. 203.60 ± 54.98 × 109/L, P = 0.016), as well as poorer eGFR (84.09 ± 16.13 mL/min per 1.73 m2 vs. 91.35 ± 15.07 mL/min per 1.73 m2, P < 0.001), lower LVEF (61.65% ± 7.31% vs. 62.77% ± 7.32%, P = 0.025), and more CCB usage (55.9% vs. 48.4%, P = 0.027). No significant differences were found between COPD group and non-COPD group for the other clinical characteristics and medication usages. The clinical characteristics and medication usages for both COPD group and non-COPD group are shown in Table 1.
Figure 1.
Flow chart describing the eligible study population during the five-year follow-up period.
COPD: chronic obstructive pulmonary disease.
Table 1. Clinical and laboratory characteristics of enrolled patients (n = 9843).
| Characteristics | COPD group (n = 229) | Non-COPD group (n = 9614) | P-value |
| Data are presented as means ± SD or n (%). COPD: chronic obstructive pulmonary disease. | |||
| Age, yrs | 65.38 ± 9.13 | 58.27 ± 10.24 | < 0.001 |
| Male | 171 (74.7%) | 7423 (77.2%) | 0.381 |
| Body mass index, kg/m2 | 25.67 ± 3.30 | 25.94 ± 3.15 | 0.188 |
| Coronary heart disease type | |||
| Myocardial infarction | 39 (17.0%) | 1709 (17.8%) | 0.770 |
| Unstable angina | 96 (41.9%) | 4034 (42.0%) | 0.991 |
| Stable coronary artery disease | 94 (41.0%) | 3871 (40.3%) | 0.811 |
| Risk factor | |||
| Current smoking | 137 (59.8%) | 5614 (58.4%) | 0.684 |
| Diabetes mellitus | 67 (29.3%) | 2904 (30.2%) | 0.827 |
| Hypertension | 150 (65.5%) | 6192 (64.4%) | 0.780 |
| Hyperlipidemia | 160 (69.9%) | 6456 (67.2%) | 0.433 |
| Laboratory measurements | |||
| Hemoglobin, g/L | 136.55 ± 16.03 | 141.09 ± 15.84 | < 0.001 |
| Platelet count, × 109/L | 194.73 ± 50.27 | 203.60 ± 54.98 | 0.016 |
| Estimated glomerular filtration rate, mL/min per 1.73 m2 | 84.09 ± 16.13 | 91.35 ± 15.07 | < 0.001 |
| Low-density lipoprotein cholesterol, mmol/L | 2.48 ± 0.86 | 2.51 ± 0.92 | 0.667 |
| Left ventricular ejection fraction, % | 61.65 ± 7.31 | 62.77 ± 7.32 | 0.025 |
| Medications | |||
| Aspirin | 223 (97.4%) | 9491 (98.7%) | 0.127 |
| P2Y12 receptor antagonist | 228 (99.6%) | 9611 (99.9%) | 0.177 |
| Angiotensin-converting enzyme inhibitors/Angiotensin II
receptor blockers |
19 (8.3%) | 740 (7.7%) | 0.707 |
| Beta-blocker | 201 (87.8%) | 8667 (90.1%) | 0.220 |
| Calcium channel blocker | 128 (55.9%) | 4656 (48.4%) | 0.027 |
| Nitrates | 225 (98.3%) | 9398 (97.8%) | 0.821 |
| Statin | 224 (97.8%) | 9218 (95.9%) | 0.175 |
| Proton pump inhibitor | 57 (24.9%) | 1917 (19.9%) | 0.066 |
COPD Impacts on Clinical Outcomes
During the five-year follow-up period, 397 patients (4.0%) died, in which 241 patients (2.4%) were cardiogenic deaths. Additionally, 571 patients (5.8%) had MI, and 1420 patients (14.4%) had RV. The number of stroke events was 364 (3.7%), of which 44 (12.1%) were cerebral hemorrhage, 305 (83.8%) were cerebral infarction, and 15 (4.1%) were transient ischemic attacks. Bleeding events (BARC ≥ 2) occurred in 444 patients (4.5%), of which 332 patients (74.8%), 102 patients (22.9%), and 10 patients (2.3%) were BARC 2, BARC 3, and BARC 5, respectively; BARC 4 was not present in any patients. With respect to bleeding sites, 42 patients (9.5%) had intracranial hemorrhage; 55 patients (12.4%) had visual impairment-causing eye bleeding, 165 patients (37.2%) had gastrointestinal bleeding, 148 patients (33.3%) had bleeding from gums, nose, or skin mucosa, and 34 patients (7.6%) had bleeding from other body sites. MACCEs occurred in 2238 patients (22.7%).
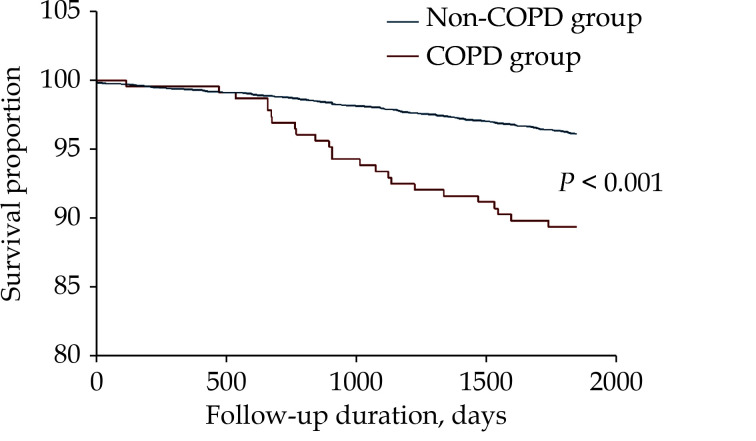
Based on the distribution of those aforementioned findings between COPD group and non-COPD group, we found that the incidences of all-cause death and cardiogenic death, as well as MACCEs among COPD patients were significantly higher than for non-COPD patients (10.5% vs. 3.9%, 7.4% vs. 2.3%, and 30.1% vs. 22.6%, respectively). Table 2 displays the effects of COPD on clinical outcomes under univariate analysis, in which COPD was found to be predictive for those three aforementioned outcomes. The predictive ability of COPD with adverse events was further analyzed under multivariate Cox regression analysis, adjusted for confounding factors, including age, sex, body mass index, hypertension, diabetes mellitus, hyperlipidemia, smoking, hemoglobin, platelet count, eGFR, LVEF, as well as CCB and proton pump inhibitor usage. Under this regression analysis, the presence of COPD was still a significant predictive factor for all-cause death (OR = 1.76, 95% CI: 1.15–2.70, P = 0.009) and cardiogenic death (OR = 2.02, 95% CI: 1.21–3.39, P = 0.007), but not for MACCEs (OR = 1.23, 95% CI: 0.96–1.57, P = 0.106) (Table 2). This finding was further reinforced by Kaplan-Meier analysis depicting that CHD patients with COPD had higher mortality during the five-year follow-up period, compared to CHD patients without COPD (Figure 2).
Table 2. Effect of COPD on clinical outcomes under univariate and multivariate Cox regression analyses.
| Adverse events | COPD group
(n = 229) |
Non-COPD group
(n = 9614) |
Univariate analysis | Multivariate Cox
regression analysis |
|||
| OR (95% CI) | P-value | OR (95% CI) | P-value | ||||
| BARC: Bleeding Academic Research Consortium; CI: confidence interval; COPD: chronic obstructive pulmonary disease; OR: odds ratio. | |||||||
| All-cause death | 24 (10.5%) | 373 (3.9%) | 2.90 (1.87–4.48) | < 0.001 | 1.76 (1.15–2.70) | 0.009 | |
| Cardiogenic death | 17 (7.4%) | 224 (2.3%) | 3.36 (2.02–5.61) | < 0.001 | 2.02 (1.21–3.39) | 0.007 | |
| Myocardial infarction | 12 (5.2%) | 559 (5.8%) | 0.90 (0.50–1.61) | 0.886 | 0.84 (0.46–1.52) | 0.555 | |
| Repeated revascularization | 34 (14.8%) | 1386 (14.4%) | 1.04 (0.72–1.50) | 0.849 | 1.08 (0.76–1.53) | 0.655 | |
| Stroke | 9 (3.9%) | 355 (3.7%) | 1.07 (0.54–2.10) | 0.858 | 0.76 (0.38–1.53) | 0.441 | |
| Bleeding (BARC ≥ 2) | 6 (2.6%) | 438 (4.3%) | 0.60 (0.26–1.35) | 0.249 | 0.52 (0.23–1.16) | 0.109 | |
| Major adverse cardiac and cerebral events | 69 (30.1%) | 2169 (22.6%) | 1.48 (1.12–1.97) | 0.008 | 1.23 (0.96–1.57) | 0.106 | |
Figure 2.
Kaplan-Meier analysis for the cumulative survival proportion among coronary heart disease patients, with or without COPD, during the five-year follow-up period.
COPD: chronic obstructive pulmonary disease.
DISCUSSION
Our study showed CHD patients with COPD were older, as well as having lower hemoglobin levels, platelet counts, LVEF, poorer eGFR, and more CCB usage, compared to those without COPD. Furthermore, the presence of COPD was a significant independent predictor of higher mortality from all-cause death and cardiogenic death, compared to non-COPD patients. These findings are in line with the current literature, such as Hadi, et al.,[9] who reported the presence of additional risk factors among acute coronary syndrome patients with COPD versus with non-COPD, such as older age, as well as higher incidences of diabetes mellitus, hypertension, and hyperlipidemia. Other previous studies have also demonstrated that COPD patients with cardiovascular diseases had impaired left ventricle function, which was closely correlated with decreased exercise tolerance during the cardio-respiratory exercise test, as well as decreased oxygen pulse indices and increased cardiac muscle injury.[10,11] We also found that the COPD group tended to use more CCB, and less beta-blockers than the non-COPD group, though the latter was not statistically significant. This difference was speculated to stem from concerns that beta-blocker usage may lead to bronchospasms in COPD, resulting in patients not receiving guideline-recommended treatments. However, these concerns of possible harm from beta-blockers have little support from the current data; indeed, studies by Rabe, et al.[12] advised the patients should not be denied beta-blockers if required.
The poorer prognostic outcomes, with respect to mortality, among CHD patients with COPD observed in our study were also in line with a wide swath of the current literature. Nishiyama, et al.[13] showed that COPD presence had a significant impact on the prognoses of patients with concurrent non-selective CHD, who were undergoing PCI and coronary artery bypass grafting. Their results showed that during the three-year follow-up period, the incidence of all-cause death and cardiogenic death were higher among those COPD patients than those non-COPD patients.[13] Additionally, Stefan, et al.[14] showed that patients with acute MI with COPD had higher in-hospital and 30-day all-cause mortality than patients without COPD; while Konecny, et al.[15] found that COPD significantly increased both all-cause death and cardiogenic death, as well as MI recurrence rate post-PCI in patients with non-selective CHD. An analysis of ST-segment elevation MI patients, divided into COPD group and non-COPD group, also observed that COPD was an independent predictor of mortality during the three-year follow-up period, as well as being associated with more frequent hospital readmissions for recurrent MI, heart failure, RV, and serious bleeding.[16] This observation was further supported by two systematic review and meta-analyses, conducted by Rothnie’s group and Bundhun’s group, showing a higher occurrence of long-term adverse cardiac events and mortality for CHD patients with COPD.[17,18]
COPD is a type of lung disease characterized by airflow limitation, which had also been shown to be closely related to CHD, via multiple mechanisms. One such mechanism is increased oxidative stress, hypoxia and systemic inflammation among COPD patients, leading to a large number of inflammatory mediators entering the circulation, resulting in eventual impairment of vascular endothelial functioning and subsequent cardiac conduction system instability, thereby increasing the probability of cardiovascular events. Additionally, increased pulmonary artery pressure, caused by COPD eventually leads to right ventricle enlargement, as well as left ventricular diastolic and systolic volume decrease, which all contributes to decreased ejection fraction and cardiac functioning.[19,20] Lastly, the presence of COPD affects CHD treatment, as it often precludes the administration of beta-blockers, the first-line medication for preventing the onset of additional complications in patients with CHD. This is owed to beta-blockers often being withheld from COPD patients with comorbid cardiovascular diseases, due to concerns of them being potentially antagonistic to beta-2 agonists, which are often prescribed for alleviating COPD symptoms.[21] Overall, the presence of COPD exacerbates the progression, and complicates the treatment, in CHD patients, leading to increased risk and poorer clinical prognoses.
LIMITATIONS
There are several limitations that must be noted. Firstly, data about pulmonary function and respiratory drug use which may affect prognosis were not collected in our study, so future pulmonary function and respiratory drug use need to be included as confounding factors for analysis. Secondly, we only tested laboratory indicators at admission, the levels of laboratory indicators may change over follow-up were not available, which may failed to assess the potential impacts on prognosis. Thirdly, it was a single center retrospective observational study, and only including one cohort of patients from a single hospital. Last but not least, our investigation lacks a validation cohort, because of the difficulties related to assembling a replication cohort. So future multicenter prospective studies, with larger sample sizes and involving multiple cohorts, should be conducted to verify our findings.
CONCLUSIONS
In summary, the current study confirmed that CHD patients with COPD have more risk factors and worse clinical prognoses than CHD patients with non-COPD. Therefore, COPD is an independent predictive factor for all-cause death and cardiogenic death.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No.81770365), the Young Scientists Fund of the National Natural Science Foundation of China (No.81900323), National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital, Chinese Academy of Medical Sciences (NCRC2020013), and CAMS Innovation Fund for Medical Sciences (2020-I2M-C&T-B-049). All authors had no conflicts of interest to disclose.
Contributor Information
Jin-Qing YUAN, Email: dr_jinqingyuan@sina.com.
Run-Lin GAO, Email: grl0504@163.com.
References
- 1.Onishi K Total management of chronic obstructive pulmonary disease (COPD) as an independent risk factor for cardiovascular disease. J Cardiol. 2017;70:128–134. doi: 10.1016/j.jjcc.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 2.André S, Conde B, Fragoso E, et al COPD and cardiovascular disease. Pulmonology. 2019;25:168–176. doi: 10.1016/j.pulmoe.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Negewo NA, Gibson PG, McDonald VM COPD and its comorbidities: impact, measurement and mechanisms. Respirology. 2015;20:1160–1171. doi: 10.1111/resp.12642. [DOI] [PubMed] [Google Scholar]
- 4.Wijns W, Kolh P, Danchin N, et al Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–2555. doi: 10.1093/eurheartj/ehq277. [DOI] [PubMed] [Google Scholar]
- 5.Celli BR, MacNee W, ATS/ERS Task Force Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–946. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 6.Thygesen K, Alpert JS, Jaffe AS, et al Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 7.Cutlip DE, Windecker S, Mehran R, et al Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–2351. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 8.Mehran R, Rao SV, Bhatt DL, et al Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123:2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 9.Hadi HA, Zubaid M, Al Mahmeed W, et al Prevalence and prognosis of chronic obstructive pulmonary disease among 8167 Middle Eastern patients with acute coronary syndrome. Clin Cardiol. 2010;33:228–235. doi: 10.1002/clc.20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aisanov Z, Khaltaev N Management of cardiovascular comorbidities in chronic obstructive pulmonary disease patients. J Thorac Dis. 2020;12:2791–2802. doi: 10.21037/jtd.2020.03.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacDonald MI, Shafuddin E, King PT, et al Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease. Lancet Respir Med. 2016;4:138–148. doi: 10.1016/S2213-2600(15)00509-3. [DOI] [PubMed] [Google Scholar]
- 12.Rabe KF, Hurst JR, Suissa S Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27:180057. doi: 10.1183/16000617.0057-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishiyama K, Morimoto T, Furukawa Y, et al Chronic obstructive pulmonary disease-an independent risk factor for long-term cardiac and cardiovascular mortality in patients with ischemic heart disease. Int J Cardiol. 2010;143:178–183. doi: 10.1016/j.ijcard.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Stefan MS, Bannuru RR, Lessard D, et al The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction: a 10-year retrospective observational study. Chest. 2012;141:1441–1448. doi: 10.1378/chest.11-2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konecny T, Somers K, Orban M, et al Interactions between COPD and outcomes after percutaneous coronary intervention. Chest. 2010;138:621–627. doi: 10.1378/chest.10-0300. [DOI] [PubMed] [Google Scholar]
- 16.Campo G, Guastaroba P, Marzocchi A, et al Impact of COPD on long-term outcome after ST-segment elevation myocardial infarction receiving primary percutaneous coronary intervention. Chest. 2013;144:750–757. doi: 10.1378/chest.12-2313. [DOI] [PubMed] [Google Scholar]
- 17.Rothnie KJ, Yan R, Smeeth L, et al Risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMJ Open. 2015;5:e007824. doi: 10.1136/bmjopen-2015-007824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bundhun PK, Gupta C, Xu GM Major adverse cardiac events and mortality in chronic obstructive pulmonary disease following percutaneous coronary intervention: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17:191. doi: 10.1186/s12872-017-0622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang M, Long Y, Liu S, et al Prevalence of cardiovascular events and their risk factors in patients with chronic obstructive pulmonary disease and obstructive sleep apnea overlap syndrome. Front Cardiovasc Med. 2021;8:694806. doi: 10.3389/fcvm.2021.694806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomsen M, Ingebrigtsen TS, Marott JL, et al Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309:2353–2361. doi: 10.1001/jama.2013.5732. [DOI] [PubMed] [Google Scholar]
- 21.Andell P, Erlinge D, Smith JG, et al β-blocker use and mortality in COPD patients after myocardial infarction: a Swedish nationwide observational study. J Am Heart Assoc. 2015;4:e001611. doi: 10.1161/JAHA.114.001611. [DOI] [PMC free article] [PubMed] [Google Scholar]