Abstract
This randomized, controlled trial tested the impact that hypnosis delivered through immersive virtual reality technology on background pain, anxiety, opioid use, and hospital length of stay in a sample of patients hospitalized for trauma. Participants were randomly assigned to receive either virtual-reality-induced hypnosis, virtual reality for distraction, or usual care during the course of their hospitalization. Mean number of treatment sessions was 3. A total of 153 patients participated in the study. Results indicated no significant differences between the experimental and control conditions on any outcome measures. This study used an early version of virtual reality technology to induce hypnosis and highlighted several important lessons about the challenges of implementation of this technology and how to improve its use in clinical settings.
Keywords: Virtual reality hypnosis, acute pain
Abstract
Die Wirkung der Virtuellen-Realitäts-Hypnose auf durch Trauma verursachten Schmerz und Angst: Lehren aus klinischen Studien.
Shelley A. Wiechman, Mark P. Jensen, Sam R. Sharar, Jason K. Barber, Maryam Soltani, und David R. Patterson
Zusammenfassung: Mit dieser randomisierten, kontrollierten Studie wurde die durch Hypnose vermittelte Wirkung immersiver virtueller Realitätstechnik auf Hintergrundschmerz, Angst, Opioidkonsum und Verweildauer im Krankenhaus bei einer Stichprobe von Patienten untersucht, welche aufgrund von Traumata hospitalisiert worden waren. Die Teilnehmenden wurden nach Zufall für folgende Maßnahmen ausgewählt: entweder für virtuell-realitätsinduzierte Hypnose, virtuelle Realität zur Ablenkung oder nur übliche Krankenhausversorgung. Die durchschnittliche Anzahl der Behandlungen lag bei 3. Insgesamt nahmen 153 Patienten an der Studie teil. Es zeigten sich bei keiner Ergebnismessung signifikante Unterschiede zwischen Experimental- und Kontrollbedingungen. Für diese Studie wurde eine frühe Version der Technologie virtueller Realität zur Hypnoseinduktion eingesetzt und dabei zeigten sich einige wichtige Erkenntnisse über die Herausforderungen bei der Einführung dieser Technologie und wie deren Einsatz im klinischen Bereich zu verbessern sei.
Alida Iost-Peter
Dipl.-Psych.
Impact de l’hypnose en réalité virtuelle sur la douleur et l’anxiété causées par un traumatisme : leçons tirées d’un essai clinique
Shelley A. Wiechman, Mark P. Jensen, Sam R. Sharar, Jason K. Barber, Maryam Soltani, et David R. Patterson
Résumé : Cet essai randomisé et contrôlé a testé l’impact de l’hypnose grâce à la technologie de réalité virtuelle immersive sur la douleur chronique, l’anxiété, la consommation d’opioïdes et la durée du séjour à l’hôpital chez un échantillon de patients hospitalisés pour un traumatisme. Les participants ont été répartis au hasard pour recevoir soit une intervention par hypnose induite par la réalité virtuelle, soit une réalité virtuelle pour la distraction, soit des soins habituels au cours de leur hospitalisation. Le nombre moyen de séances de traitement était de trois. Au total, 153 patients ont participé à l’étude. Les résultats n’ont indiqué aucune différence significative entre les conditions expérimentales et de contrôle sur les mesures de résultats. Cette étude a utilisé une première version de la technologie de réalité virtuelle pour induire l’hypnose et a mis en évidence plusieurs leçons importantes sur les défis de la mise en œuvre de cette technologie et sur les modalités d’amélioration de son utilisation en clinique.
Gerard Fitoussi, M.D.
President-elect of the European Society of Hypnosis
El impacto de la hipnosis en realidad virtual sobre el dolor y la ansiedad causada por trauma: Lecciones aprendidas en un ensayo clínico.
Shelley A. Wiechman, Mark P. Jensen, Sam R. Sharar, Jason K. Barber, Maryam Soltani, y David R. Patterson
Resumen: Este ensayo clínico, randomizado, evaluó el impacto de la hipnosis ejecutada a través de tecnología de realidad virtual inmersiva para dolor, ansiedad, uso de opioides y estancia hospitalaria en una muestra de pacientes hospitalizados por trauma. Los participantes fueron asignados aleatoriamente para recibir hipnosis inducida mediante realidad virtual, realidad virtual de distracción, o el cuidado usual durante el curso de la hospitalización. El número de sesiones promedio fue de 3. Un total de 153 pacientes participaron en el estudio. Los resultados no mostraron diferencias significativas entre los grupos experimental y control en ninguna de las medidas objetivo. Este estudio utilizó una versión inicial de la tecnología de realidad virtual para introducir la hipnosis y enfatiza varias lecciones importantes sobre los retos de implementación de esta tecnología y cómo mejorarla para uso clínico.
Omar Sánchez-Armáss Cappello
Autonomous University of San Luis Potosi, Mexico
Patients who are admitted to either an ICU or acute care from injuries sustained from physical trauma can experience significant pain. This type of pain is often exacerbated by post-trauma surgery and therapeutic treatments of the injury, such as physical therapy. Management of acute pain can be complicated and interventions need to rely on a multimodal approach. Often, trauma centers rely solely on the use of opioids. As the risks of opioid analgesics have become increasingly apparent (Gomes et al., 2018; Strayer et al., 2017), safer alternatives to pain management have become increasingly necessary. Interest in hypnosis has waxed and waned over the last 2 centuries as a potential alternative to drugs since the development of ether (Gauld, 1992). The need for trained clinicians to provide this treatment is a barrier (Patterson et al., 2010). Immersive virtual reality offers a means of pain control that does not require a trained clinician. However, to date, the efficacy of virtual reality analgesia has only been demonstrated for acute pain management, such as that resulting from specific medical procedures such as wound care, or acute pain such as labor pain. Immersive virtual is a potential cost-effective strategy for delivering analgesia without harmful side effects. Here we sought to evaluate the efficacy of an early version of virtual reality hypnosis for treating the problem of pain associated with major physical trauma in hospitalized patients, using a randomized, controlled trial design.
Pain Caused by Physical Trauma
Pain from trauma (and its management) begins in the prehospital and emergency room settings (emergency phase), reaches its peak during hospitalization and associated surgery (acute phase), continues into the outpatient setting (rehabilitation phase), and, in some cases, can persist indefinitely (chronic phase). Further, trauma pain is multidimensional. Ongoing background pain is often present as the injury heals. Procedural pain (Wiechman & Sharar, 2018) results from invasive medical procedures, such as wound care and physical therapy. Breakthrough pain (Wiechman & Sharar, 2018) is an acute increase in pain that often occurs during daily activities or mild exercise. Postoperative pain (Wiechman & Sharar, 2018) is a temporary increase in pain that is due to a recent surgical incision or surgical procedure. This paper focuses on the experience and impact of ongoing background pain in the acute phase. Studies have shown that this component of trauma pain can lead to long-term chronic pain, depression, and also to an increased dependence on opioids (Hooten et al., 2015; Strayer et al., 2017).
Hypnosis
Hypnosis is generally defined as “a state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestions” (Elkins et al., 2015). Research has shown that specific physiological changes occur with hypnotic analgesia, supporting it as a promising approach to acute-pain management. These changes include alterations in: sympathetic responding (De Pascalis & Perrone, 1996), pain-related evoked potentials (Arendt-Nielsen et al., 1990; Barabasz & Lonsdale, 1983; Crawford et al., 1998), brain oscillations (Crawford, 1990), patterns of brain activity (blood-flow mapping) (Price & Barrell, 2000; Rainville et al., 1997), and possible inhibition of nociceptive signals at the spinal cord level (Kiernan et al., 1995). Preliminary clinical studies have also shown hypnosis to be effective at decreasing pain associated with burn-dressing changes (Patterson et al., 1992; Patterson & Ptacek, 1997; Wiechman Askay & Patterson, 2007), bone-marrow aspirations (Liossi & Hatira, 1999), and a variety of surgical procedures (Lang et al., 2000; Patterson & Jensen, 2003). For example, Faymonville delivered hypnosis during surgery and was able to show better pain and anxiety relief than conventional IV sedation and also allowed for a significant reduction in midazolam and alfentanil requirements (Faymonville et al, 1999). Due to the efficacy of hypnosis for treating pain and distress associated with surgery, hypnosis has been shown to decrease operating room costs, as well as reduce overall healthcare costs (Lang et al., 2000). Hypnosis appears to be particularly well suited for treating acute background pain posttrauma; although very little research has been performed evaluating its efficacy for this application.
Primary gaps in the clinical hypnosis literature include finding ways to strengthen the effect size of treatment and generalize its impact to a greater number of patients (Moss & Willmarth, 2019; Patterson et al., 2010). This includes finding new modalities to deliver hypnosis so that the intervention is not dependent upon having a trained therapist available at the bedside. As virtual reality technology has gained popularity and is becoming increasingly accessible, here we evaluate the efficacy of using this technology to deliver hypnotic analgesia.
Virtual Reality Distraction
Immersive virtual reality (VR) is an attention-grabbing, illusory reality created in the mind of the VR user/patient. Immersive VR, which involves a head-mounted display that blocks the user’s view of the real world, gives patients the illusion of “going into” a 3-D, computer-generated environment. The strength of the illusion of “presence,” which is the degree of the patient’s sense of “going inside” the computer-generated virtual environment, is thought to reflect the amount of attention drawn into the virtual world. Because VR is by nature a highly attention-grabbing experience, it has been shown to be an effective psychological pain-control technique that reduces the amount of attention available to process pain (Hoffman et al., 2006; Hoffman, Richards, et al., 2004; Hoffman, Sharar, et al., 2004). Less attention to pain can result in a reduction in perceived pain intensity and unpleasantness. It can also reduce the amount of time patients spend thinking about their pain (corresponding to the sensory, emotional, and cognitive components of the pain experience, respectively).
Combining Virtual Reality and Hypnosis
Combining VR and hypnosis represents a logical and practical progression of the development of both modalities. In our previous publications, we have proposed attention and distraction as the underlying mechanisms behind VR-based analgesia (Hoffman et al., 2006; Sharar et al., 2007). As mentioned previously, we have noted that pain requires conscious attention to be processed. Attention can be drawn away from pain through immersion in the VR environment, where patients think less about pain and report less pain intensity and unpleasantness.
Attentional processes are also regarded as central to hypnosis and hypnotic analgesia. Attention is often described as a critically important step in a hypnotic induction (Crawford, 1994) and is central to hypnotic analgesia, specifically. For example, Crawford has used measures of regional cerebral blood flow to map brain processing during hypnosis and hypnotic analgesia (Crawford, 1989, 1994). Her results show initial greater activity in the areas of the brain that reflect an increase in attentional effort during hypnotic analgesia (Crawford, 1989, 1994).
With attentional mechanisms as a common denominator, the unique attention-grabbing qualities of VR and the suggestion inherent in hypnosis, it would be reasonable to hypothesize a synergistic effect between these modalities. For example, hypnotic suggestion might help relax subjects who are apprehensive about allowing themselves to suspend disbelief and be drawn into a virtual world. Hypnotic suggestion could also be used to deepen a willing subject’s sense of presence in the virtual world. Conversely, VR may be instrumental in facilitating the attentional processes thought to be important for effective hypnotic induction and response to hypnotic suggestions; a subject whose attention has been captured in the virtual environment might be only a short cognitive step away from being more receptive to hypnotic suggestions. However, these potential synergistic and interactive effects, as promising as they may be, remain untested in clinical populations.
Several studies have investigated the comparative mechanisms of VR and hypnosis for experimentally induced pain. In the first one, Patterson and colleagues (Patterson, Hoffman, et al., 2006) compared hypnosis and VR alone and combination, in a 2×2 design with experimentally induced thermal pain in healthy subjects. Both VR and hypnosis resulted in lowered pain ratings, but the combination of these approaches did not result in any improvement when compared to either approach being used alone. More recently, this group of investigators attempted to determine whether hypnotic suggestions might facilitate an analgesic response to immersive VR. Healthy subjects received a thermal pain stimulus at baseline, then each participant received hypnosis or no hypnosis, followed by VR distraction or no VR distraction, during a second aversive stimulus. Participants in the hypnosis condition remained hypnotized during the second brief noxious thermal stimulus. Results showed that audio hypnosis alone resulted in a greater analgesic response than VR distraction alone. However, hypnotic analgesia was not significantly improved by the addition of VR distraction during the pain stimulus.
Virtual Reality Hypnosis
There have been a number of attempts to use virtual reality platforms to provide hypnosis treatment for clinical pain. In four studies, investigators used a virtual world designed to distract patients who had burn injuries from the pain they experienced, by creating an illusion of descending into a canyon (Oneal et al., 2008; Patterson, Wiechman, et al., 2006; Soltani et al., 2011; Teeley et al., 2012). With this approach, as patients descend into a virtual canyon with their eyes open, audiotape instructions encourage them to “…sink deeper into a hypnotic state” as the numbers between one and ten appear in the virtual world. Posthypnotic suggestions for pain relief are provided as patients hover over a virtual lake. Using this approach, one case study reported that a patient with neuropathic pain reported a 36% reduction in pain from pre- to post-VRH session (Oneal et al., 2008). This paradigm has also been used in two additional case reports, one with pain from gluteal hidradenitis (Soltani et al., 2011) and one from a series of patients hospitalized with bone fractures (Teeley et al., 2012). In a controlled trial with a small sample of 48 patients, Patterson, Wiechman, et al., 2006, reported that this version of virtual reality hypnosis was successful in reducing ratings of pain from burn-injury wound debridement. Further, Enea et al. (2014) compared the effects of hypnotic analgesia and virtual reality distraction on experimental pain and found that, although the two treatments were more effective at reducing pain compared to a control group, only high hypnotizables reported hypnotic analgesia. VR distraction reduced pain regardless of hypnotizability. Finally, a recent review of the literature by Rousseaux et al. (2020) concluded that the effects of VRH on pain are inconsistent, and they could not determine that VR added value to hypnosis when they are combined. However, the researchers called for additional randomized clinical trials on VRH for pain management that can help define VRH analgesia guidelines.
As noted previously, there are several potential advantages to using VR for inducing hypnosis. First, such an approach would make the presence of a trained clinician for the hypnosis treatment unnecessary. This could reduce the expense and increase accessibility to hypnotic approaches, thus increasing the number of patients that could be treated. Second, the use of visual stimuli and technology could potentially be particularly useful with patients who may have low trait hypnotizability or absorption skills. Third, this approach may provide a means for inducing hypnosis in people who are hearing impaired, because the virtual environment does not rely on sound as the sole means of hypnotic induction. Given the potential strengths and overall novelty of VR-induced hypnosis, information on the development and potential efficacy of this modality is warranted.
The purpose of the current study was to better understand the potential for VR hypnosis to reduce acute pain associated with severe trauma in a fully powered study, using a sample of hospitalized patients. We hypothesized that patients randomized to a VR hypnosis condition would report greater reductions in postoperative background pain and anxiety and evidence less opioid use and fewer hospitalization days, as compared to trauma patients randomized to VR distraction and usual care conditions.
Method
Participants
The study participants were a sample of patients hospitalized at a major Level 1 trauma center for the care of (1) closed long bone or calcaneus fractures and/or (2) an intraabdominal injury causing blunt force trauma and requiring surgical repair (i.e., laparotomy). These mechanisms of injury are typically caused by motor vehicle collision, assault (gunshot wound, knife, fist), falls, and other forms of accidental and nonaccidental physical trauma. Patients in our sample were not hospitalized for an elective surgery or other medical illnesses (e.g., cancer, cardiovascular disease). The two types of injury in our sample represent the two most frequent US trauma-hospital admissions (DiMaggio et al., 2016). By limiting eligibility to these two trauma causes only, we were able to reduce heterogeneity in the sample by excluding patients with a broad range of other trauma etiologies (e.g., burn injuries, gunshot wounds, facial trauma) that have been studied elsewhere (Wiechman Askay & Patterson, 2008).
The inclusion criteria for the study included the following: aged 18 years or older, hospitalized for orthopedic injuries (closed long bone or calcaneus fractures), and/or intraabdominal injuries requiring a laparotomy or a minimum of 2 days in the hospital, decisional capacity to consent to study, able to communicate verbally, and English speaking. Exclusion criteria consisted of evidence of traumatic brain injury, current delirium, currently receiving prophylaxis for alcohol or drug withdrawal, face/head/neck injuries preventing helmet use, extreme susceptibility to motion sickness, seizure history, body-substance-isolation procedures, incarcerated, homeless, or pregnant. The study was approved by our institutional review board and registered on ClinicalTrials.gov (NCT00739076) in 2008. However, we began enrolling patients in 2007 prior to the existence of the clinical trials registry.
Procedures
In a procedure approved by the University of Washington Internal Review Board, inpatients who were eligible to participate in the study were identified by the research team. They were first approached by a clinical care provider for permission to be approached by research personnel. Those who were interested met with the study research coordinator and invited to participate in the study. Upon explanation of the study, written informed consent was obtained. Baseline data were gathered in the morning, and patients who agreed to participate in the study were randomized into one of three conditions (VRH, VRD, usual care). Since we predicted that there would be no difference between the VRD group and the no-VR group, randomization was weighted as a 2:1:1 ratio. Specifically, 2 (VRH group) to 1 (VRD group) to 1 (no-VR group). Consequently, we have almost twice as many participants in Group 1 (experimental group) as we do in Groups 2 and 3 (control groups).
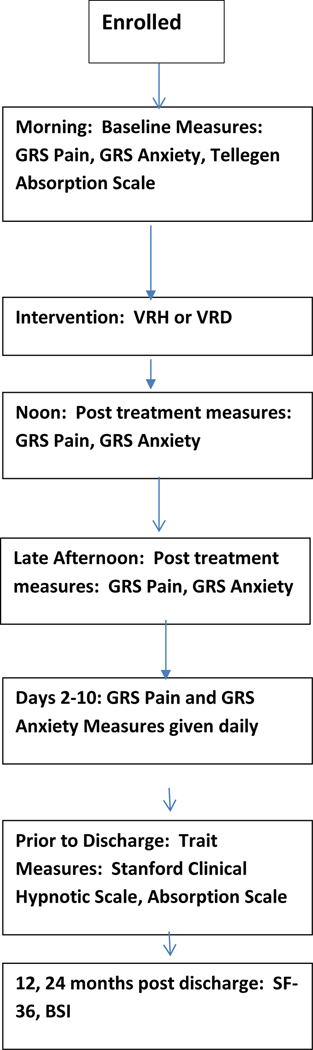
Treatment Conditions
Participants were randomized to one of three groups: (a) VRH group, consisted of VR with posthypnotic suggestions for pain reduction/forgetting about the pain, emotional calm, improved sleep, recalling positive experiences and being more hopeful about the future; (b) VRD group, consisted of VR distraction without hypnotic suggestion to control for participation in a trial and receiving VR; or (c) usual care, a no-treatment with VR control condition in which patients received analgesic care only. More details of each group are found below. On the morning of study participation, all participants were administered the GRS rating scales for average pain intensity in the past 8 hours. Participants in the VRH and VRD groups were then given 40 minutes of VRH or as many minutes as they wanted of VRD. All participants were administered the GRS again at noon and then in the late afternoon. Participants were offered either VRD or VRH once a day during their hospital stay up to 10 days. Participants were then given two follow-up measures (BSI and SF-36) at discharge, 6 months, 12 months, and 24 months postdischarge. See Figure 1, flow through the study.
Figure 1.
Flow through the Study
VR Hypnosis
In VR hypnosis, patients receive a hypnotic induction while drifting through a three-dimensional, computer-generated virtual world (SnowWorld) modified for the current study. Participants begin at the top of an icy canyon and float to the bottom as the program progresses. Using a KaiserXL-50VRhelmet, (www.keo.com) and a “6-degrees-of-freedom” electromagnetic head-tracking device (www.Polhemus.com). The patient can look around in SnowWorld by moving his or her head. While in SnowWorld, the patient goes through the following four stages:
For the first 4 minutes, the patient hovers at the top of the canyon and receives instructions from an audiotape of the principal investigator’s voice. The instructions prepare the patient for what they would experience during the virtual reality hypnosis.
The patient then slowly descends into the canyon and sees increasing large numbers (from 1 to 10) posted on signs in the virtual world.
After passing through a tunnel and some fog, the patient is virtually “floating” over a blue lake with lush green banks. At this stage, the patient receives posthypnotic suggestions for pain control (e.g., “you will feel nothing other than comfort and relaxation”).
The participant then ascends back up the canyon and sees the numbers from 10 to 1 coming out of the induction. Thus, the essential characteristics of hypnosis are integrated into a high-tech, computer-generated world, and the subject is able to participate with their eyes open. This is a passive tool in that patients were not physically active. The total time in VRH was 40 minutes.
VR Distraction
In VR distraction, patients are immersed into SnowWorld and are allowed to interactively “throw” snowballs (by pressing the space bar) at penguins and snowmen as they float down the icy canyon (Hoffman et al., 2009, 2011). This is a more active tool as patients were holding the hand controls and manipulating the environment. Their time in VR lasted as many minutes as they wanted.
Usual Care
Patients in this condition receive the same pain management regimen as those in the treatment groups. Although analgesic administration is not protocol driven and strictly uniform among patients, a standard regimen of limited analgesic, sedative, and sleep-agent options is provided to the resident and attending physicians in trauma and orthopedics who care for these patients, in the form of preprinted analgesic order forms by all care providers. According to these standardized analgesic orders, enrolled patients initially receive intravenous morphine or hydromorphone immediately following injury and/or surgery and transition to oral oxycodone or sustained-release morphine when pain levels and oral intake allow. Oral and IV opioid analgesics may also be administered on a PRN schedule.
Demographic Variables
Demographic information was collected for all participants. These data were extracted from the patient’s medical records and included the following information: age; sex; ethnicity; cause, type, and date of injury; date of hospital admission; date of study initiation; education; vocational and marital status; history of drug and alcohol use; and length of hospitalization.
Pain Intensity
The 0-to-10 Graphic Rating Scale (Scott & Huskisson, 1976) was used to assess pain intensity. It consists of a 100 mm line with 11 hatch marks, each associated with an integer from 0 to 10. Specific hatch marks are also labeled with a verbal descriptor indicating different levels of pain intensity, with 0 = no pain at all, 2 = mild pain, 8 = severe pain, and 10 = excruciating pain. Here, the tool was used to assess average pain intensity over the past 24 hours (e.g., background pain). The GRS is more sensitive than simple categorical pain scales, and patients can easily use them despite having no previous experience with the measure (Scott & Huskisson, 1976). This primary outcome variable was given the morning prior to either VRH or VRD and the afternoon following the intervention. This variable was then averaged over their length of hospitalization up to 10 days. It was not given at discharge, 6, 12 or 24 months postdischarge.
Anxiety
Average anxiety over the previous 24 hours was measured by the same GRS scale described above. It was also given the morning prior to the intervention and postintervention and then was averaged over the course of patients’ inpatient hospitalization.
Opioid Use
We determined ordered ranges of opioid analgesics (i.e., morphine-based drugs) and assessed what has been ordered, what the patient received as part of scheduled care, and what medications were given based on patient request. All opioid pain medications were then converted to opioid equivalents that allowed for a comparison between different drugs. Opioid use was averaged over the course of the hospitalization up to 10 days. It was not assessed past patients’ hospitalization.
Length of Hospitalization
Hospital days were determined at the time of discharge by calculating admission to discharge.
Trait Measures
The patients’ absorption and hypnotizability were assessed with two separate scales administered just prior to discharge. Absorption was measured by the Tellegen Absorption Scale (Tellegen & Attkinson, 1974). This scale consists of 34 true-false items that have been used to assess hypnotic susceptibility in adults. Hypnotizability was measured with the abbreviated form of the Stanford Clinical Hypnotic Scale (SCHS; Morgan & Hilgard, 1978). This scale assesses hypnotizability with five items and is appropriate for participants aged 17 and older.
The Brief Symptom Inventory
The Brief Symptom Inventory (Derogatis & Spencer, 1993) is a 53-item, self-report questionnaire that measures the severity of nine psychological symptom domains (somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism). The measure can also be scored to create three indices of symptomatology, intensity of symptoms and number of reported symptoms (Global Severity Index, Positive Symptom Distress Index, Positive Symptom Total). We used the Global Severity Index for the current study. Higher scores on the BSI scales indicates more severe symptoms. Items are rated on a 5-point scale from 0 (not at all) to 4 (extremely). This measure was given at baseline, discharge, and 6, 12, and 24 months postdischarge.
SF-36
The Medical Outcomes Study 36-item Short Form Health Survey (Ware et al., 1996) was used to assess health-related quality of life. The questionnaire can be scored to create a Physical Component Scale (SF36P) and a Mental Component Scale (SF36M) score. The SF-36 is widely used and has been establish across diverse patient groups (McHorney et al., 1993). Scores scaled on a T metric with a population mean of 50and an SD of 10. Higher scores indicate a better quality of life in each domain. This measure was given at baseline, discharge, and 6, 12, and 24 months postdischarge.
Statistical Analysis
Differences in demographic characteristics among the three treatment arms were assessed for statistical significance using Kruskal-Wallis and Fisher’s exact tests as appropriate. Analysis of our primary hypothesis testing for differences in the four short-term outcomes among the three treatment arms was carried out with standard linear regression modelling. Mathematical transformations were required for anxiety (square-root) and opioid-use and length-of-stay (logarithmic) to better ensure a reasonable assumption of normality of the statistical distributions. Long-term outcome was assessed using mixed-effect linear regression, assuming a linear trend over time with an autoregressive correlation matrix and modelling a random slope and intercept for each subject. Treatment effect was modelled as a single three-category covariate with post hoc adjustment for all pairwise comparisons. All conclusions were evaluated in the context of multiple comparisons per Holm-Bonferroni.
Results
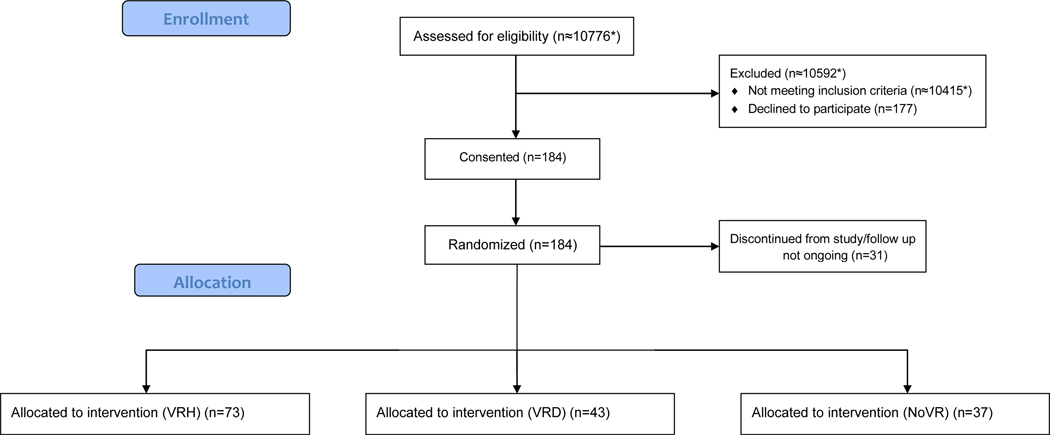
A total of 153 patients participated in the study. The study was adequately powered. Based on preliminary data from our past studies, we would need no more than 10 participants in each arm to achieve 80% power. The majority of the sample were male (71%) with a mean age of 34 (SD=13.5). Seventy-five percent of the sample were Caucasian, and 49% were employed at the time of injury and 51% unemployed or unknown at the time of inclusion in the study. Their average length of stay was 13 days (SD=13.4). As is typical of a trauma center, the mechanism of injury included motor vehicle collision (53%), violence (18%), falls (16%), and “other” types of traumas (13%). See Figure 2 for Consort diagram. See Table 1 for Description of the sample.
Figure 2.
CONSORT Flow Diagram
* We did not record the screening for all time periods for this study. Therefore, we calculated the average number of patients screened per year using known recorded screening data from a similar study.
Table 1.
Description of Sample
| VRH (n=73) | VRD (n=43) | NVR (n=37) | p * | |
|---|---|---|---|---|
|
| ||||
| Age | 33.3 (13.8) | 38.0 (13.9) | 33.8 (12.1) | .15 |
| Male | 46 (63%) | 35 (81%) | 27 (73%) | .10 |
| Caucasian | 56 (77%) | 31 (72%) | 27 (73%) | .84 |
| Education Years | 12.6 (2.4) | 12.7 (2.1) | 13.2 (2.0) | .48 |
| Never Married | 39 (55%) | 20 (47%) | 17 (46%) | .56 |
| Employed/Student | 53 (75%) | 27 (63%) | 27 (73%) | .39 |
| History of Drugs | 21 (30%) | 7 (17%) | 8 (22%) | .29 |
| History of Meth | 24 (34%) | 18 (43%) | 14 (38%) | .63 |
| History of ETOH | 22 (31%) | 18 (43%) | 11 (30%) | .39 |
| Study Days | 3.7 (2.7) | 3.6 (2.0) | 3.9 (2.7) | .80 |
VRH= VR Hypnosis; VRD= VR Distraction; NVR= No VR
Note. Cells report Mean(SD) or N(%); Two subjects missing marital and employment status; Three subjects missing drug/ETOH history
Significance by ANOVA or Fisher’s exact as appropriate
The mean number of sessions of VRH was 3.68 (SD = 2.7) and the mean number of treatment sessions for VRD was 3.58 (SD = 1.9) so there was no significant difference between the groups for number of treatments.
The majority of our sample scored an average of 21.3 (SD= 7.4) on the Tellegen Absorption Scale, falling into the average range of absorption. The average score on the SCHS was a 1.9, indicating a low level of hypnotizability. There were no differences between the groups on either of these measures. It should be noted that there was a considerable amount of missing data for the SCHS, because participants either refused it or were discharged before it could be administered.
There were no significant differences among the experimental and control groups in any of the demographic variables. However, an observed imbalance on drug history (p = .092 was enough for us to include it as a covariate in all our primary regression models, as it was also highly correlated with two of the four outcomes (pain and anxiety).
There were no omnibus or pairwise differences in outcome that were statistically significant for any of the four primary outcomes. The effect showing the most promise was the significance for the three-arm comparison for pain (p = .079), but this effect washed out after adjusting for multiple comparisons (p = .316). Although the differences are weak and not significant, it appears that VRD reported more pain than VRH or usual care. However, they were also taking less opioid medication. Regarding our long-term outcome data of the SF-36 and the BSI, a mixed effects regression was used to test for a difference in linear trends over time among the three treatment arms. Again, there were no differences in any of these outcome measures at 6-, 12-, and 24-month follow-up between the three groups. All groups either improved or stayed the same from discharge to 24-month follow-up..
Discussion
This study investigated whether VR hypnosis was effective in reducing pain intensity, anxiety, and opioid analgesic use in patients hospitalized for significant physical trauma. To our knowledge, this was the first randomized controlled trial on the use of VR hypnosis for trauma pain management, much less pain from any etiology. Although we have previously reported that VR hypnosis successfully reduced procedural pain from burn and other traumatic injuries (Patterson, Wiechman, et al., 2006), this previous study involved a small sample with a different type of pain. In the current study with more subjects, we hypothesized that those patients who received hypnotic suggestions for reduced pain and anxiety through VR hypnosis would report less pain and anxiety, shorter lengths of stay, and require less pain medication than control groups who received VR distraction or usual care. None of these hypotheses were supported.
There are several explanations for the null findings reported here. First, is the possibility that patient selection for their acute pain problem may have counteracted our intents. These patients are expected to heal exponentially and often show diminished pain within the time frame they were evaluated. Second, the VR hypnosis intervention may not have been strong enough to achieve our predicted results. The version of VR hypnosis used in this current study was an early version that did not include more advanced technology or newer graphics. In the VR world, participants floated through a virtual canyon that did not include images that were particularly engaging or relaxing. Although this program was created (and has been previously found to be successful) for patients experiencing acute pain (Patterson, Wiechman, et al., 2006) and hypnotic suggestions were targeted at pain and anxiety, the program was not as sophisticated as the VR technology that people are now more accustomed to and that is potentially more effective. Future studies may want to explore the efficacy of VR hypnosis using “off the shelf” programs that have state of the art graphics but are not tailored to specific pain problems. These programs were not available at the time we began this study. Currently, there are libraries of programs available, either through an app or that are part of the system that is selected for use.
Moreover, when the participants received hypnotic suggestions in this study, they were floating over a virtual lake with their eyes open. With regard to the latter point, it is difficult to compete with the human imagination, even with visual technology that is particularly compelling. Because patients had their eyes open, this might have interfered with their ability to absorb hypnotic suggestions. Thus, one possibility is that the limitations of the technology used, combined with the participants having their eyes open, limited the impact of the intervention.
Another possible explanation for the study’s null findings is related to the nature of trauma care and the difficulty of reducing the background pain that was targeted with this study. Given the complicated nature of trauma care and the chaotic setting of a trauma hospital, ongoing pain may have been a poor target for a psychological intervention. The ongoing background pain that hospitalized trauma patients experience is usually managed with regularly scheduled pain medications (particularly long-acting opioid analgesics) and other medical interventions such as epidural blocks (Wiechman & Sharar, 2019). To date, most studies using VR, hypnosis, or their combination have focused on procedural (i.e., acute) pain. In the current study, we focused on background pain. It should be noted that this study was conducted at a Level I, regional trauma center with a county mission. The hospital environment is fast-paced and highly stimulating. This is not typically a calm environment that is conducive to background-pain management.
The paradigm used in this study represented one of several that can be used to combine hypnosis with immersive VR technology. Potential paradigms include using hypnosis to enhance VR distraction or the opposite, VR distraction to enhance hypnosis. In a recent study, we found that hypnotic suggestions designed to enhance absorption in the VR world could enhance analgesia for experimentally induced pain. Hypnosis and VR can be simultaneously administered, with no attempt for one to facilitate the effects of the other (Patterson, Hoffman, et al., 2006). In the one study that we are aware of, combining these approaches did improve pain reductions.
Clinical Implications
The type of paradigm we tested here was to use VR for both distraction and to deliver hypnosis for background pain. The notion of using immersive virtual reality to deliver hypnosis, or to enhance it, is an elusive, complex process. At this point, we maintain that the endeavor is a worthwhile pursuit as there is a critical need to identify nonpharmacological approaches to manage pain. Consideration of a patient’s coping style (avoidant vs. approach) as well as the level of participation needed for their care are critical to the practical implementation of this technology. For example, virtual reality technology is ideal for patients in situations where they want to escape either procedural or background pain and they do not need to participate in their care (e.g., they can be a passive participant). It is particularly engaging for patients who enjoy video games. Virtual reality can also be useful for patients who have a more avoidant coping style and prefer an immersive, engaging environment for relaxation. Further, programs that use virtual reality to induce hypnosis for pain can be useful in settings where a trained clinician is not available. To fully establish VR-induced hypnosis as an evidence-based treatment for pain, future studies should continue to creatively break down some of the barriers to conducting randomized clinical trials of VR hypnosis in a busy trauma center. Future research is also needed to determine who VR and VRH is appropriate for and in which settings. Finally, it is difficult to maintain a VR system that can keep up with the graphics and technology of the fast-moving gaming world. Given the wide variety of “off the shelf” VR programs now available, future studies should compare these programs to determine the efficacy of the various content. Systems themselves are now affordable and portable so establishing the efficacy of VRH and VR distraction for home use following painful surgery and other procedures is yet to be studied. Virtual reality remains an exciting option for patients experiencing acute pain.
Table 2.
Analysis of Short-Term Outcome
| Descriptives | Statistical Testing | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Measure | Arm | N | Mean (SD) | Contrast | Diff. in Means | Sig. 3 | Sig. 4 | Omnibus Sig. 3 | Omnibus Sig. 4 |
|
| |||||||||
| Pain | VRH | 71 | 45.2 (22.1) | VRH v VRD | −5.78 | .159 | .014 | .284 | .041 |
| VRD | 43 | 51.0 (20.8) | VRH v NVR | 0.78 | .857 | .690 | |||
| NVR | 36 | 44.4 (19.5) | VRD v NVR | 6.56 | .172 | .072 | |||
| Anxiety 1 | VRH | 71 | 29.9 (24.4) | VRH v VRD | −3.38 | .543 | .110 | .789 | .276 |
| VRD | 43 | 33.3 (23.6) | VRH v NVR | −1.23 | .936 | .617 | |||
| NVR | 36 | 31.2 (25.0) | VRD v NVR | 2.15 | .553 | .344 | |||
| Opioid Use 2 | VRH | 69 | 5.41 (7.17) | VRH v VRD | 1.55 | .352 | .520 | .160 | .176 |
| VRD | 43 | 3.85 (2.61) | VRH v NVR | −0.63 | .221 | .166 | |||
| NVR | 37 | 6.04 (6.12) | VRD v NVR | −2.19 | .056 | .069 | |||
| Length of Stay 2 | VRH | 72 | 13.7 (9.5) | VRH v VRD | 0.68 | .478 | .653 | .351 | .471 |
| VRD | 43 | 13.0 (13.1) | VRH v NVR | 2.17 | .153 | .475 | |||
| NVR | 37 | 11.5 (8.4) | VRD v NVR | 1.49 | .495 | .220 | |||
VRH = VR Hypnosis; VRD = VR Distraction; NVR = No VR
Note. No p-values remained statistically significant (p < .05) after adjustment for multiple comparisons (Holm-Bonferonni, m=12 pairwise, m=4 omnibus). Conclusion: There were no significant findings among the study arms for the 4 measures of interest.
Square-root transformation used to achieve normality for significance testing
Log transformation used to achieve normality for significance testing
Statistical significance by ANOVA
Statistical significance by linear regression, adjusting for drug history (as ordered categories)
Table 3.
Long-Term Outcome
| Measure | Time | % Scores Present | VRH | VRD | NVR | p 1 |
|---|---|---|---|---|---|---|
|
| ||||||
| SF-36 Physical | Discharge | 73% | 32 (39) | 21 (30) | 31 (36) | .929 |
| 6 Months | 37% | 56 (26) | 53 (26) | 54 (30) | ||
| 1 Year | 23% | 82 (15) | 51 (34) | 63 (43) | ||
| 2 Years | 21% | 73 (33) | 70 (35) | 68 (39) | ||
| SF-36 Mental | Discharge | 71% | 62 (20) | 61 (20) | 65 (20) | .429 |
| 6 Months | 36% | 61 (25) | 61 (20) | 57 (27) | ||
| 1 Year | 22% | 68 (23) | 62 (26) | 62 (29) | ||
| 2 Years | 21% | 66 (23) | 74 (18) | 65 (30) | ||
| BSI - GSI | Discharge | 71% | 1.0 (0.7) | 1.1 (0.7) | 0.8 (0.5) | .128 |
| 6 Months | 35% | 0.8 (0.8) | 0.9 (0.6) | 1.0 (0.9) | ||
| 1 Year | 23% | 0.7 (0.6) | 1.1 (0.9) | 1.4 (1.3) | ||
| 2 Years | 21% | 0.9 (0.9) | 0.6 (0.5) | 0.9 (1.3) | ||
| BSI - GSI (t) | Discharge | 71% | 64 (11) | 68 (11) | 64 (12) | .911 |
| 6 Months | 35% | 58 (15) | 66 (13) | 64 (17) | ||
| 1 Year | 23% | 58 (15) | 65 (15) | 64 (22) | ||
| 2 Years | 21% | 59 (15) | 59 (14) | 58 (17) | ||
| BSI - PSDI | Discharge | 71% | 1.8 (0.5) | 1.8 (0.6) | 1.8 (0.5) | .620 |
| 6 Months | 35% | 1.5 (0.6) | 1.6 (0.6) | 1.6 (0.6) | ||
| 1 Year | 23% | 1.4 (0.5) | 1.7 (0.9) | 2.0 (1.0) | ||
| 2 Years | 21% | 1.6 (0.7) | 1.4 (0.5) | 1.8 (0.9) | ||
| BSI - PSDI (t) | Discharge | 71% | 61 (8) | 61 (9) | 62 (8) | .907 |
| 6 Months | 35% | 55 (10) | 58 (11) | 57 (11) | ||
| 1 Year | 23% | 54 (8) | 58 (16) | 60 (16) | ||
| 2 Years | 21% | 56 (12) | 55 (12) | 60 (14) | ||
| BSI - PST | Discharge | 71% | 27 (13) | 29 (14) | 24 (15) | .690 |
| 6 Months | 35% | 22 (18) | 28 (15) | 29 (18) | ||
| 1 Year | 23% | 23 (17) | 29 (18) | 31 (22) | ||
| 2 Years | 21% | 22 (18) | 19 (16) | 19 (20) | ||
| BSI - PST (t) | Discharge | 71% | 63 (10) | 66 (12) | 62 (12) | .836 |
| 6 Months | 35% | 58 (16) | 65 (13) | 63 (18) | ||
| 1 Year | 23% | 57 (17) | 65 (16) | 64 (21) | ||
| 2 Years | 21% | 57 (16) | 57 (15) | 55 (17) | ||
Omnibus statistical significance by mixed-effects regression analysis, using a variance-components correlation matrix, testing for a difference in linear trends across time among all study arms
Acknowledgments
Funding: This study was supported by NIH grant number RO1GM042725, RO1AR054115
Footnotes
Declarations of interest: none
Contributor Information
Shelley A. Wiechman, Department of Rehabilitation Medicine, University of Washington
Mark P. Jensen, Department of Rehabilitation Medicine, University of Washington
Sam R. Sharar, Department of Anesthesiology, University of Washington.
Jason K. Barber, Department of Neurosurgery, University of Washington.
Maryam Soltani, Department of Rehabilitation Medicine, University of Washington.
David R. Patterson, Department of Rehabilitation Medicine, University of Washington
xReferences
- Arendt-Nielsen L, Zachariae R, & Bjerring P. (1990). Quantitative evaluation of hypnotically suggested hyperaesthesia and analgesia by painful laser stimulation. Pain, 42(2), 243–251. doi: 10.1016/0304-3959(90)91168-i [DOI] [PubMed] [Google Scholar]
- Barabasz AF, & Lonsdale C. (1983). Effects of hypnosis on P300 olfactory-evoked potential amplitudes. Journal of Abnormal Psychology, 92(4), 520–523. doi: 10.1037//0021-843x.92.4.520 [DOI] [PubMed] [Google Scholar]
- Crawford HJ (1990). Cognitive and psychophysiological correlates of hypnotic responsiveness and hypnosis. In Creative mastery in hypnosis and hypnoanalysis: A Festschrift for Erika Fromm. (pp. 47–54). Lawrence Erlbaum. [Google Scholar]
- Crawford HJ (1994). Brain dynamics and hypnosis: Attentional and disattentional processes. International Journal of Clinincal and Experimental Hypnosis, 42(3), 204–232. doi: 10.1080/00207149408409352 [DOI] [PubMed] [Google Scholar]
- Crawford HJ, Knebel T, Kaplan L, Vendemia JM, Xie M, Jamison S, & Pribram KH (1998). Hypnotic analgesia: 1. Somatosensory event-related potential changes to noxious stimuli and 2. Transfer learning to reduce chronic low back pain. International Journal of Clinocal and Experimental Hypnosis, 46(1), 92–132. doi: 10.1080/00207149808409992 [DOI] [PubMed] [Google Scholar]
- De Pascalis V, & Perrone M. (1996). EEG asymmetry and heart rate during experience of hypnotic analgesia in high and low hypnotizables. International Journal of Psychophysiology, 21(2–3), 163–175. doi: 10.1016/0167-8760(95)00050-x [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Spencer P. (1993). Brief symptom inventory: Pearson. [Google Scholar]
- DiMaggio C, Ayoung-Chee P, Shinseki M, Wilson C, Marshall G, Lee DC, & Frangos S. (2016). Traumatic injury in the United States: In-patient epidemiology 2000–2011. Injury, 47(7), 1393–1403. doi: 10.1016/j.injury.2016.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enea V, Dafinoiu I, Opriş D, & David D. Effects of hypnotic analgesia and virtual reality on the reduction of experimental pain among high and low hypnotizables. International Journal of Clinical and Experimental Hypnosis, 62, 360–377. [DOI] [PubMed] [Google Scholar]
- Elkins GR, Barabasz AF, Council JR, & Spiegel D. (2015). Advancing research and practice: the revised APA division 30 definition of hypnosis. American Journal of Clinical Hypnosis, 57(4):378–385. [DOI] [PubMed] [Google Scholar]
- Faymonville ME, Meurisse M, & Fissette J. (1999). Hypnosedation: A valuable alternative to traditional anaesthetic techniques. Acta Chir Belg, 99, 141–146. [PubMed] [Google Scholar]
- Gauld A. (1992). A history of hypnotism. Cambridge University Press. [Google Scholar]
- Gomes T, Tadrous M, Mamdani MM, Paterson JM, & Juurlink DN (2018). The burden of opioid-related mortality in the United States. JAMA Network Open, 1(2), e180217. doi: 10.1001/jamanetworkopen.2018.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman HG, Chambers GT, Meyer WJ 3rd, Arceneaux LL, Russell WJ, Seibel EJ, Richards TL, Sharar SR, & Patterson DR (2011). Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals Behavioral Medicine, 41(2), 183–191. doi: 10.1007/s12160-010-9248-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman HG, Patterson DR, Soltani M, Teeley A, Miller W, & Sharar SR (2009). Virtual reality pain control during physical therapy range of motion exercises for a patient with multiple blunt force trauma injuries. Cyberpsychology and Behavior, 12(1), 47–49. doi: 10.1089/cpb.2008.0056 [DOI] [PubMed] [Google Scholar]
- Hoffman HG, Richards TL, Bills AR, Van Oostrom T, Magula J, Seibel EJ, & Sharar SR (2006). Using fMRI to study the neural correlates of virtual reality analgesia. CNS Spectrums, 11(1), 45–51. doi: 10.1017/S1092852900024202 [DOI] [PubMed] [Google Scholar]
- Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, & Sharar SR (2004). Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport, 15(8), 1245–1248. doi: 10.1097/01.wnr.0000127826.73576.91 [DOI] [PubMed] [Google Scholar]
- Hoffman HG, Sharar SR, Coda B, Everett JJ, Ciol M, Richards T, & Patterson DR (2004). Manipulating presence influences the magnitude of virtual reality analgesia. Pain, 111(1–2), 162–168. doi: 10.1016/j.pain.2004.06.013 [DOI] [PubMed] [Google Scholar]
- Hooten WM, St Sauver JL, McGree ME, Jacobson DJ, & Warner DO (2015). Incidence and risk factors for progression from short-term to episodic or long-term opioid prescribing: A population-based study. Mayo Clinic Proceedings, 90(7), 850–856. doi: 10.1016/j.mayocp.2015.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiernan BD, Dane JR, Phillips LH, & Price DD (1995). Hypnotic analgesia reduces R-III nociceptive reflex: Further evidence concerning the multifactorial nature of hypnotic analgesia. Pain, 60(1), 39–47. doi: 10.1016/0304-3959(94)00134-z [DOI] [PubMed] [Google Scholar]
- Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, & Spiegel D. (2000). Adjunctive non-pharmacological analgesia for invasive medical procedures: A randomised trial. Lancet, 355(9214), 1486–1490. doi: 10.1016/s0140-6736(00)02162-0 [DOI] [PubMed] [Google Scholar]
- Liossi C, & Hatira P. (1999). Clinical hypnosis versus cognitive behavioral training for pain management with pediatric cancer patients undergoing bone marrow aspirations. International Journal of Clinical and Experimental Hypnosis, 47(2), 104–116. doi: 10.1080/00207149908410025 [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE Jr., & Raczek AE (1993). The MOS 36-Item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31(3), 247–263. doi: 10.1097/00005650-199303000-00006 [DOI] [PubMed] [Google Scholar]
- Morgan AH, & Hilgard JR (1978) The Stanford Hypnotic Clinical Scale for Adults, American Journal of Clinical Hypnosis, 21(2-3), 134–147. DOI: 10.1080/00029157.1978.10403968 [DOI] [PubMed] [Google Scholar]
- Moss D, & Willmarth E. (2019). Hypnosis, anesthesia, pain management, and preparation for medical procedures. Annals of Palliative Medicine, 8(4), 498–503. doi: 10.21037/apm.2019.07.01 [DOI] [PubMed] [Google Scholar]
- Oneal BJ, Patterson DR, Soltani M, Teeley A, & Jensen MP (2008). Virtual reality hypnosis in the treatment of chronic neuropathic pain: A case report. International Journal of Clinical and Experimental Hypnosis, 56(4), 451–462. doi: 10.1080/00207140802255534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson DR, Everett JJ, Burns GL, & Marvin JA (1992). Hypnosis for the treatment of burn pain. Journal of Consulting and Clinical Psychology, 60(5), 713–717. doi: 10.1037//0022-006x.60.5.713 [DOI] [PubMed] [Google Scholar]
- Patterson DR, Hoffman HG, Palacios AG, & Jensen MJ (2006). Analgesic effects of posthypnotic suggestions and virtual reality distraction on thermal pain. Journal of Abnormal Psychology, 115(4), 834–841. doi: 10.1037/0021-843X.115.4.834 [DOI] [PubMed] [Google Scholar]
- Patterson DR, & Jensen MP (2003). Hypnosis and clinical pain. Psychological Bulletin, 129(4), 495–521. doi: 10.1037/0033-2909.129.4.495 [DOI] [PubMed] [Google Scholar]
- Patterson DR, Jensen MP, Wiechman SA, & Sharar SR (2010). Virtual reality hypnosis for pain associated with recovery from physical trauma. International Journal of Clinical and Experimental Hypnosis, 58(3), 288–300. doi: 10.1080/00207141003760595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson DR, & Ptacek JT (1997). Baseline pain as a moderator of hypnotic analgesia for burn injury treatment. Journal of Consulting and Clinical Psychology, 65(1), 60–67. doi: 10.1037//0022-006x.65.1.60 [DOI] [PubMed] [Google Scholar]
- Patterson DR, Wiechman SA, Jensen M, & Sharar SR (2006). Hypnosis delivered through immersive virtual reality for burn pain: A clinical case series. International Journal of Clinical and Experimental Hypnosis, 54(2), 130–142. doi: 10.1080/00207140500528182 [DOI] [PubMed] [Google Scholar]
- Price DD, & Barrell JJ (2000). Mechanisms of analgesia produced by hypnosis and placebo suggestions. Progressive Brain Research, 122, 255–271. doi: 10.1016/s0079-6123(08)62144-5 [DOI] [PubMed] [Google Scholar]
- Rainville P, Duncan GH, Price DD, Carrier B, & Bushnell MC (1997). Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science, 277(5328), 968–971. doi: 10.1126/science.277.5328.968 [DOI] [PubMed] [Google Scholar]
- Rousseaux F, Bicego A, Ledoux D, Massion P, Nyssen AS, Faymonville ME, Laureys S, & Vanhaudenhuyse A. (2020). Hypnosis associated with 3D immersive virtual reality technology in the management of pain: A review of the literature. Journal of Pain Research, 13: 1129–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott J, & Huskisson EC (1976). Graphic representation of pain. Pain, 2(2), 175–184. [PubMed] [Google Scholar]
- Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, & Patterson DR (2007). Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Archives of Physical Medicine and Rehabiitationl, 88(12 Suppl 2), S43–49. doi: 10.1016/j.apmr.2007.09.004 [DOI] [PubMed] [Google Scholar]
- Soltani M, Teeley AM, Wiechman SA, Jensen MP, Sharar SR, & Patterson DR (2011). Virtual reality hypnosis for pain control in a patient with gluteal hidradenitis:a case report. Contemporary Hypnosis Integrated Therapy, 28(2), 142–147. [PMC free article] [PubMed] [Google Scholar]
- Strayer RJ, Motov SM, & Nelson LS (2017). Something for pain: Responsible opioid use in emergency medicine. American Journal of Emergency Medicine, 35(2), 337–341. doi: 10.1016/j.ajem.2016.10.043 [DOI] [PubMed] [Google Scholar]
- Teeley AM, Soltani M, Wiechman SA, Jensen MP, Sharar SR, & Patterson DR (2012). Virtual reality hypnosis pain control in the treatment of multiple fractures: A case series. American Journal of Clinical Hypnosis, 54(3), 184–194. doi: 10.1080/00029157.2011.619593 [DOI] [PubMed] [Google Scholar]
- Tellegen A, & Atkinson G. (1974). Openness to absorbing and self-altering experiences (“absorption”), a trait related to hypnotic susceptibility. Journal of Abnormal Psychology, 83(3), 268–277. 10.1037/h0036681 [DOI] [PubMed] [Google Scholar]
- Ware J Jr., Kosinski M, & Keller SD (1996). A 12-Item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. doi: 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Ware J Jr., Kosinski M, & Keller SD (1996). A 12-Item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. doi: 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Wiechman Askay S, & Patterson DR (2007). Hypnotic analgesia. Expert Review of Neurotherapeutics, 7(12), 1675–1683. doi: 10.1586/14737175.7.12.1675 [DOI] [PubMed] [Google Scholar]
- Wiechman Askay S, & Patterson DR (2008). What are the psychiatric sequelae of burn pain? Current Pain and Headache Reports, 12(2), 94–97. doi: 10.1007/s11916-008-0018-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiechman S, & Sharar S. (2019). Paradigm-based treatment approaches for burn pain control. Up to Date. https://www.uptodate.com/contents/paradigm-based-treatment-approaches-for-burn-pain [Google Scholar]