Abstract
A 39-year-old woman with progressive bilateral visual decline was diagnosed as having Bietti crystalline dystrophy in 2008. The disease course was monitored with optical coherence tomography until 2021. During the last routine eye examination in 2021, a full-thickness, slightly eccentric, visually asymptomatic macular hole with an intact foveola was noted in the left eye. No surgical treatment was recommended. The pathogenesis of full-thickness macular hole remained unclear as there were only subtle signs of prior very mild macular edema and vitreomacular interface abnormality. A degenerative process was also possible.
Keywords: Bietti crystalline dystrophy, macula, macular hole, optical coherence tomography
Introduction
Bietti crystalline dystrophy (BCD) is a rare, genetically determined retinal dystrophy characterized by shiny yellow crystalline deposits in the retina and less frequently in the limbus, together with progressive chorioretinal atrophy mainly commencing at the posterior pole.1,2,3
Rare macular complications previously reported in patients with BCD include macular hole,4,5,6,7 cystoid macular edema,8 subfoveal neurosensorial detachment,9 and macular neovascular membrane.10,11,12
We hereby report the longitudinal optical coherence tomography (OCT) follow-up of a woman who developed a unilateral full-thickness macular hole 13 years after the first examination.
Case Presentation
In 2008, we examined a 39-year-old otherwise healthy woman who presented with bilateral progressive visual decline of at least 10 years’ duration. There was no family history, consanguinity, or similarly affected family member. On examination, best corrected visual acuity was 6/10 on Snellen chart bilaterally. Crystalline deposits were observed in the superior corneal limbus of both eyes. Intraocular pressure was 16 mmHg bilaterally. Fundus examination and fluorescein angiography revealed scattered, refractile retinal deposits at the posterior pole and surrounding retina in association with areas of retina pigment epithelium (RPE) atrophy in both eyes (Figure 1 A-D). On OCT, intraretinal hyperreflective dots, bright plaques over the Bruch’s membrane-RPE complex, and outer retinal tubulations were detected (Figure 1 E,F). Our clinical diagnosis was BCD and we examined the patient several times between 2008 and 2018 and obtained consecutive OCT images (Figure 2 A-H).
Figure 1.
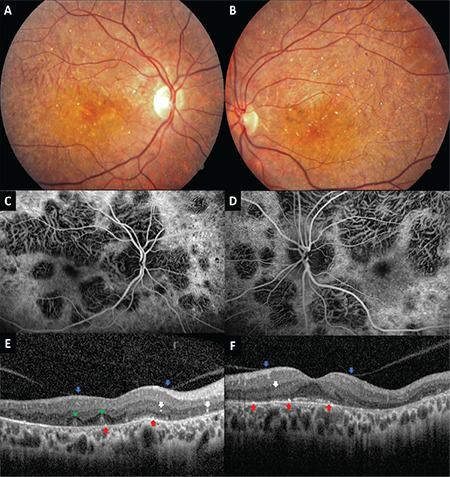
Examination in 2008. Color fundus images of the right (A) and left (B) eyes show scattered intraretinal crystals at the posterior pole with subtle chorioretinal atrophy. Composite venous phase fluorescein angiogram of the right (C) and left (D) eyes reveal patchy hypofluorescent areas corresponding to areas of chorioretinal atrophy. Optical coherence tomographic sections from the right (E) and left (F) eyes demonstrate a few hyperreflective dots corresponding to intraretinal crystals (white arrows), vitreoretinal adhesions (blue arrows), outer retinal tubulations (green arrowheads) and bright plaques on top of the
Figure 2.
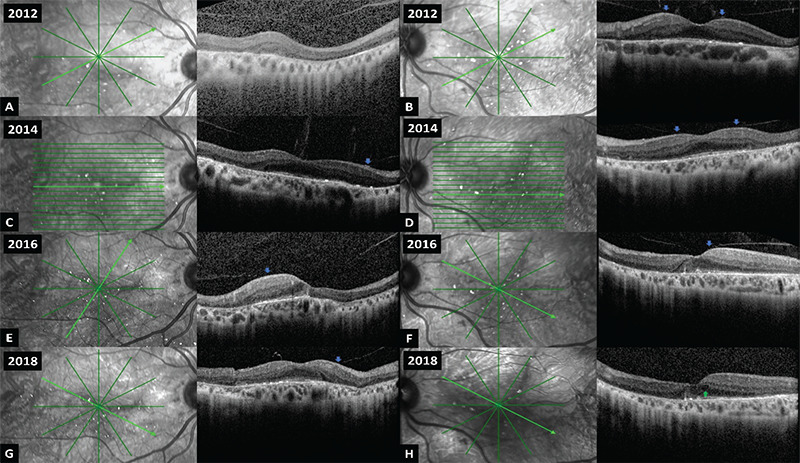
Consecutive optical coherence tomographic sections with related reflectance images taken from the right (A, C, E, G) and left (B, D, F, H) eyes between 2012 and 2018. Note the subtle cystic macular changes in the left eye (green arrow). Vitreoretinal adhesions are marked with blue arrows
The patient recently underwent an ophthalmic examination in December 2021 following a long COVID-related interruption. However, she denied any recent visual symptoms. Her best-corrected visual acuity was Snellen 4/10 in the right eye with correction of -2.00 -2.25x15 and 6/10 in the left eye with correction of -3.75 -1.00x150 (sphere, cylinder x axis). Anterior segment examination was unremarkable bilaterally. We noted advanced chorioretinal atrophy and reduced number of retinal crystalline deposits at the both posterior pole (Figure 3 A-D). However, serial OCT sections and en-face OCT angiography slabs revealed a slightly eccentric full-thickness macular hole with an intact foveola in the left eye (Figure 4 A-G). As the patient was asymptomatic and the appearance of hole was only observed in two consecutive B-scans 132 µm apart, surgery was not recommended, and we advised her to have more frequent visits.
Figure 3.

Examination in 2021. Color fundus images of the right (A) and left (B) eyes show marked chorioretinal atrophy and near complete absence of intraretinal crystals at the posterior pole. Fundus autofluorescence images of the right (C) and left (D) eyes demonstrate extensive hypoautofluorescent areas
Figure 4.
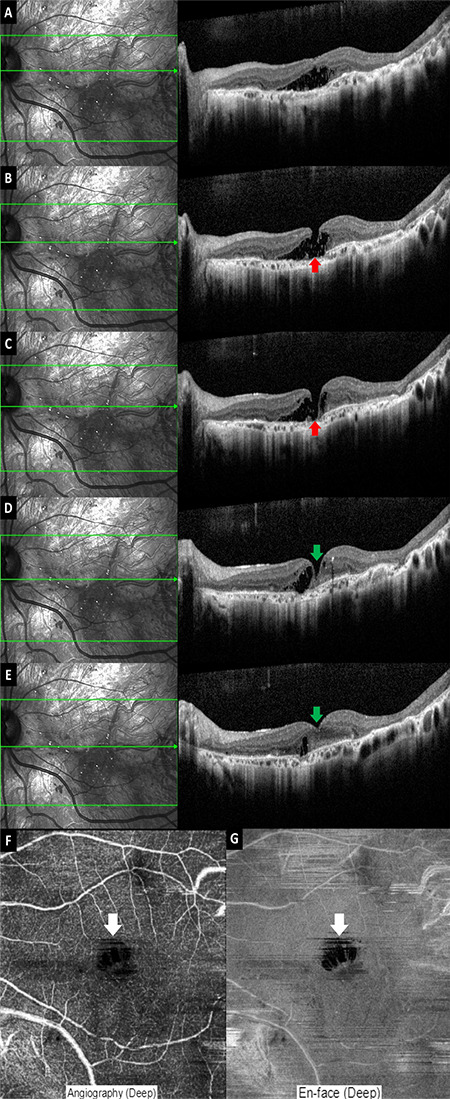
Consecutive optical coherence tomographic sections taken in the left eye at 132-µm intervals (A-E) show the full-thickness eccentric hole (red arrows) with the intact foveola (green arrows). Optical coherence tomography angiographic section (F) and en-face image (G) of deep vascular plexus slabs reveal a central flow void corresponding to the hole (white arrows)
Discussion
Partial and full-thickness macular defects can by caused by tractional forces on the fovea or may arise from anomalous posterior vitreous detachment and contraction of an epiretinal membrane. In addition, cystoid macular edema and high myopia can also lead to macular hole formation.13
There are only a few anecdotal reports of macular holes in patients with BCD and thus, its pathogenesis is still somewhat obscure. Bagolini and Ioli-Spada4 reported a series of eight patients with BCD, of whom two were previously followed by Bietti. One of these patients was a 31-year-old highly myopic woman with bilateral retinal detachment and a unilateral macular hole. We previously reported a 21-year-old man who developed a stage 4 full-thickness unilateral macular hole with surrounding macular detachment three years after initial examination.5 Ji et al.6 reported bilateral macular holes in a 32-year-old man with stage 3 BCD according to Yuzawa’s1 clinical disease staging. No surgery was performed, and the authors did not elaborate on the pathogenetic mechanism of the macular hole development. Nourinia et al.7 described a 42-year-old man who was followed for 10 years and developed a unilateral full-thickness macular hole. Pars plana vitrectomy with internal limiting membrane peeling and gas injection was performed, and the hole was closed successfully following the surgery.
The pathogenesis of full-thickness macular hole formation is not clear in the present case. We reanalyzed all of the previous OCT sections from the left eye and noticed very mild macular edema and vitreomacular interface abnormality in some of the sections. It is likely that a degenerative process might have also been a factor in the hole formation. Talib et al.14 shared their observations in a case with choroideremia and unilateral full-thickness macular hole and argued that chronic low-grade inflammation originating from the outer retinal cells might have contributed to the hole formation. On the other hand, Müller cells might have a role as they transmit the traction forces from the inner to outer retina, leading to central photoreceptor layer defects and even neurosensorial retinal detachment.13
We elected to follow the patient for the time being as the patient was asymptomatic, most likely due to slight eccentric location of the full-thickness hole with the intact foveola. Her left eye had also less chorioretinal atrophy when compared to the fellow eye and was the better-seeing eye.
Full-thickness macular hole is very rarely observed in association with BCD and has a yet undetermined and possibly multifactorial pathogenesis. We recommend frequent ophthalmic examinations and careful tomographic monitoring in patients with BCD to detect any macular changes, including macular hole.
Footnotes
Ethics
Informed Consent: Obtained.
Peer-review: Externally and internally peer reviewed.
Authorship Contributions
Concept: A.O.S., M.K., R.A., Design: A.O.S., M.K., R.A., Data Collection or Processing: A.O.S., M.K., R.A., Analysis or Interpretation: A.O.S., M.K., R.A., Literature Search: A.O.S., M.K., R.A., Writing: A.O.S., M.K., R.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Yuzawa M, Mae Y, Matsui M. Bietti’s crystalline retinopathy. Ophthalmic Paediatr Genet. 1986;7:9–20. doi: 10.3109/13816818609058037. [DOI] [PubMed] [Google Scholar]
- 2.Osman Saatci A, Can Doruk H. An Overview of Rare and Unusual Clinical Features of Bietti’s Crystalline Dystrophy. Med Hypothesis Discov Innov Ophthalmol. 2014;3:51–56. [PMC free article] [PubMed] [Google Scholar]
- 3.Bozkurt B, Ozturk BT, Kerimoglu H, Irkec M, Pekel H. In vivo confocal microscopic findings of 2 patients with Bietti crystalline corneoretinal dystrophy. Cornea. 2010;29:590–593. doi: 10.1097/ICO.0b013e3181be22ee. [DOI] [PubMed] [Google Scholar]
- 4.Bagolini B, Ioli-Spada G. Bietti’s tapetoretinal degeneration with marginal corneal dystrophy. Am J Ophthalmol. 1968;65:53–60. doi: 10.1016/0002-9394(68)91028-3. [DOI] [PubMed] [Google Scholar]
- 5.Saatci AO, Yaman A, Berk AT, Söylev MF. Macular hole formation in Bietti’s crystalline retinopathy. A case report. Ophthalmic Genet. 1997;18:139–141. doi: 10.3109/13816819709057127. [DOI] [PubMed] [Google Scholar]
- 6.Ji SX, Yin XL, He XG, Yuan RD, Ye J, Liu SZ, Gan XM, Dong Y. Bietti crystalline dystrophy with bilateral macular holes. Retin Cases Brief Rep. 2009;3:361–363. doi: 10.1097/ICB.0b013e3181780832. [DOI] [PubMed] [Google Scholar]
- 7.Nourinia R, Dehghan MH, Fekri S. Outcome of Macular Hole Surgery in Bietti Crystalline Dystrophy. J Ophthalmic Vis Res. 2017;12:338–341. doi: 10.4103/jovr.jovr_154_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saatci AO, Doruk HC, Yaman A. Cystoid Macular Edema in Bietti’s Crystalline Retinopathy. Case Rep Ophthalmol Med. 2014;2014:964892. doi: 10.1155/2014/964892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padhi TR, Kesarwani S, Jalali S. Bietti crystalline retinal dystrophy with subfoveal neurosensory detachment and congenital tortuosity of retinal vessels: case report. Doc Ophthalmol. 2011;122:199–206. doi: 10.1007/s10633-011-9274-1. [DOI] [PubMed] [Google Scholar]
- 10.Atmaca LS, Muftuoglu O, Atmaca-Sonmez P. Peripapillary choroidal neovascularization in Bietti crystalline retinopathy. Eye (Lond). 2007;21:839–842. doi: 10.1038/sj.eye.6702673. [DOI] [PubMed] [Google Scholar]
- 11.Nachiappan K, Krishnan T, Madhavan J. Ranibizumab for choroidal neovascular membrane in a rare case of Bietti’s crystalline dystrophy: a case report. Indian J Ophthalmol. 2012;60:207–209. doi: 10.4103/0301-4738.95873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobat SG, Gul FC, Yusufoglu E. Bietti crystalline dystrophy and choroidal neovascularization in childhood. Int J Ophthalmol. 2019;12:1514–1516. doi: 10.18240/ijo.2019.09.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bringmann A, Unterlauft JD, Barth T, Wiedemann R, Rehak M, Wiedemann P. Müller cells and astrocytes in tractional macular disorders. Prog Retin Eye Res. 2022;86:100977. doi: 10.1016/j.preteyeres.2021.100977. [DOI] [PubMed] [Google Scholar]
- 14.Talib M, Koetsier LS, MacLaren RE, Boon CJF. Outcome of Full-Thickness Macular Hole Surgery in Choroideremia. Genes (Basel). 2017;8:187. doi: 10.3390/genes8070187. [DOI] [PMC free article] [PubMed] [Google Scholar]


