Abstract
OBJECTIVES:
The objective is to evaluate the association of Solobacterium moorei (S. moorei) to halitosis and to also check for the effects of two different mouth rinses on levels of S. moorei in saliva and tongue coating and its impact on oral halitosis.
MATERIALS AND METHODS:
This was a placebo-controlled parallel study of 160 individuals who were randomized and the study was performed using double-blinded protocol. Enrolled individuals filled a structured questionnaire regarding demographic data, oral hygiene habits, and dietary habits. Full mouth organoleptic odor scores (OLR), volatile sulfur compounds levels, Miyazaki's tongue coating index, and Plaque scores were recorded before intervention (baseline) and after 1-week post treatment. Microbiological samples obtained from the tongue and saliva was investigated for S. moorei levels using real time polymerase chain reaction. Participants were randomly assigned for two test mouth rinses (Melaleuca alternifolia and Chlorhexidine) and placebo groups.
RESULTS:
All salivary and tongue coating samples were tested positive for S. moorei in the halitosis group. One week post-treatment S. moorei counts in saliva and tongue coating samples of test group showed a significant reduction at P < 0.001. Paired t-test results showed that Melaleuca alternifolia was comparable with chlorhexidine in reduction of OLR, and VSC scores (P < 0.001). Salivary levels of S. moorei in Melaleuca alternifolia group showed a higher reduction (5.67 log10 copies/mL) than chlorhexidine group (5.1log10 copies/mL).
CONCLUSION:
S. moorei showed a positive correlation with oral halitosis scores. Both Melaleuca alternifolia and chlorhexidine were equally effective in reducing S. moorei levels and halitosis score.
Keywords: Chlorhexidine, halitosis, portable breath analyzer, solobacterium, tea tree oil
Introduction
Halitosis is the third most common presenting complaint from patients in the dental office, the commonest ones being periodontal disease and dental caries.[1] Overgrowth of bacteria on the dorsal surface of the tongue is usually associated with halitosis in a vast majority of cases.[2] The tongue microbiota is characterized by high proportions of volatile sulfur compounds (VSC) producing anaerobic bacterial species. The primary source of oral malodor is thought to be the dorsal surface in the posterior region of the tongue.[3] The bacteria responsible for this process are the Porphyromonas gingivalis, Treponema denticola, Prevotella intermedia, Porphyromonas endodontalis, Bacteroides loescheii, Enterobacteriaceae, Tannerella forsythia, and Fusobacterium nucleatum.[4,5] Newer advances in the field of microbiology have led to the identification of both cultivable and non-cultivable or unidentified bacterial species. Non-spore-forming, anaerobic Gram-positive bacillus such as the Solobacterium moorei (S. moorei) which was earlier called as Bulleida have been demonstrated to be associated with bacteremia, septicemia, wound infection, and periodontal disease.[5,6,7] Significant numbers of studies have reported positive correlations on the presence of S. moorei in the tongue to oral halitosis.[8] The most basic approach of detecting halitosis is organoleptic scoring, which is subjective in nature and lacks reproducibility, but this method is still considered as “gold standard,” as the human nose can discriminate between a variety of odors. Objective tests for the detection of oral halitosis are gas chromatography and the BANA test (N-benzoyl-DL-arginine-2 naphthylamide test), which are complex and relatively expensive. Currently, various less expensive digital portable gas chromatographs like the Oral Chroma (Nissha FIS.) are available.[9] In the past 10 years, umpteen researches on halitosis have led to an improved understanding of its etiology and treatment [Figure 1]. The advent of many chair-side portable devices has made the objective estimation of the exhaled air possible. Mint (Burlingame), an ultra-portable breath analysis device which is similar to Halimeter (Interscan) utilizes eletrochemical fuel cell sensor technology to measure the VSCs in parts per billion (ppb).[10] Documented studies have shown the antimicrobial and anti-malodor properties of various mouthwashes such as chlorhexidine, chlorine dioxide, essential oil, and cetylpyridinium chloride.[11,12] But up till now, there are limited randomized, clinical trials available which demonstrate the usefulness of natural alternatives such as Melaleuca alternifolia mouth rinse on S. moorei levels in saliva and tongue coating samples. The medical and dental produced have been using tea tree oil (TTO), which is obtained from the leaves of Melaleuca. It exhibits both antibacterial and anti-inflammatory activities mostly because of its active ingredients such as 1, 8-cineole and terpinen-4-ol.[13] Both the 7th European Pharmacopoeia and the European Medicine Agency have acknowledged its use and embedded it in the text as well as included this essential oil in clinical practice.[14] In this context, the present authors hypothesized that a higher halitosis score might be associated with increased S. moorei levels in saliva and tongue coating. Hence, the purpose of this study was to compare Melaleuca alternifolia (TTO) and chlorhexidine mouth rinses by testing their efficacy in reducing VSC scores in mouth air and bacterial counts in saliva and tongue coating.
Figure 1.
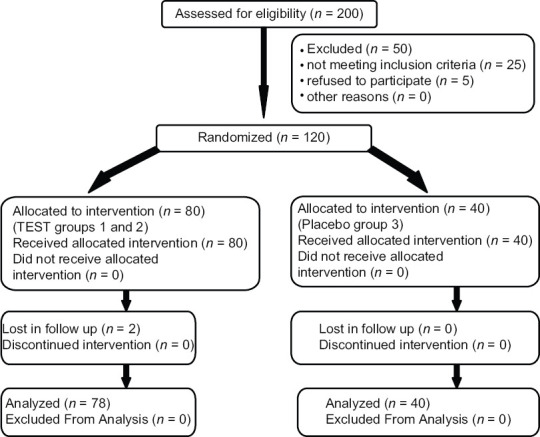
CONSORT flow chart
Materials and Methods
Design of the study
This randomized placebo-controlled study using parallel-arm design was done in a single center using two commercially available mouth rinses. The registration number (CTRI/2019/11/022041).
Source of data
Patients visiting the Department of Periodontology from October 2019 to December 2019 were enrolled for the study. The institutional ethics board approved the protocol designed for the study (BIDS/2015 dated 18/10/2019). Written consent was obtained from all participants after the details of the procedures and the follow-up visit was explained. This protocol was in accord with the declaration of Helsinki of 1973 (as revised in 2002). Individuals with systemic conditions such as diabetes mellitus or kidney disease, liver disease, any bacterial oral infection; pregnant and lactating females; former and current smokers; treatment for oral dryness or xerostomia were excluded from the study. None of the participants received the treatment of periodontal disease within 6 months prior to the study.
Initial visits
During this visit, enrolled individuals were instructed to fill a questionnaire before the clinical examination and measurement of halitosis. Demographic variables such as age, sex, and occupation were noted. Past medical history and oral hygiene habits including brushing technique, use of additional aids for inter-dental cleansing, tongue cleaning, and past periodontal therapy if any were recorded. Preference and choice of food were also asked.
Sample size estimation and grouping
This randomized study included 160 individuals after sample size calculation. The confidence interval was set at 95%, and the power of the study was 85% considering the nonhalitosis and halitosis individuals and testing the efficacy to two test and placebo mouth rinses. The 160 individuals were segregated into two groups based on their halitosis scoring.
1. Halitosis (n = 120); 2. Non halitosis (n = 40).
Assessment of halitosis
Organoleptic method: The individuals were instructed to refrain from odoriferous food, alcohol, and mouth rinses/fresheners from the previous night and come to the outpatient department in the morning after tooth brushing and tongue cleaning. Air was exhaled through the mouth after it had been kept closed for 30 s. The experienced judge (BA) was seated 10 cm away from the participant. Organoleptic scores on a 5-point scale were measured as described by Rosenberg in 1991.[15] The experiment was repeated twice and the average scores were taken for the study. Individuals greater than score 3 were considered as having oral malodor and were included for this study
VSC's estimation: Was done using the Mint device with the smartphone companion app. Only individuals with a score of >3 as measured by the organoleptic method were assessed for VSCs. The pocket-size Mint device pairs with the user's smartphone and uses a proprietary senor array reading of VSCs from the air blown from the user's mouth and shows value in ppb. Based on the detected VSCs, they were graded from A to F. A-being <50 ppb and F-being greater than 354ppb. For this study, we included individuals with VSC scores of >157ppbs.
Examination protocol
Clinical measurements were recorded at the 1st day (baseline) and after 1 week by the same trained examiner. The examiner was blinded to the study groups at all time. Baseline records were also made unavailable for the examiner at the recall visits. The following were the clinical variables.
Collection of salivary samples
Unstimulated whole salivary samples were collected after routine oral hygiene procedures in the morning, and before assessment of periodontal parameters to avoid contamination of saliva with blood. Patients were instructed to spit into the vial every 30 sec. Intervals of 5 min were give between each spit. From this, 0.2 mL of diluted sample was taken in a buffer solution vial which contains Tris-Ethylenediaminetetraacetate (TE buffer).
Collection of tongue coating samples
Isolation was done using cotton rolls which were placed under the tongue. The tongue coating samples were collected by gentle scraping with the help of a sterile wooden spatula in the posterior part after drying the area with blast of air. Then the sample was transferred to vial containing 2 mL of TE buffer. Both the salivary and tongue coating samples were immediately transported to laboratory and processed within 48 h for analysis of S. moorei using real-time polymerase chain reaction (PCR) following standard protocol and instruction by the manufacturers.
Polymerase chain reaction procedure
A standard strain of S. moorei (CCUG 59440) was used in the study. The standard strains were grown on Columbia blood agar; inoculums were put into the Todd Hewitt Broth medium. It was supplemented with 0.001% hemin, 0.0001% Vitamin K, 0.5% Tween-80, 0.2% yeast extract, and 1% glucose, at 37°C under anaerobic condition (N2: H2: CO2/75:10:15). The turbidity of broth was adjusted to 0.5 McFarland standards to obtain the quantity of 108 Colony Forming Unit (CFU)/mL. DNA was extracted from this standard sample. Serial dilutions of this DNA sample were made ranging from 108 to 102 CFU/mL. PCR was run for the standard samples to obtain a standard curve. Standard graph is plotted; cycle threshold (Ct) values versus quantity.
The primers used were
S. moorei-F 5’-CTG TAG AGA TAC AGT AGA GGT TAT C-3’
S. moorei-R 5’-ATT GTA GTA CGT GTG TAG CC-3’.
Polymerase chain reaction analysis
The SYBR Green dye binds with double-stranded DNAs which were specifically amplified by S. moorei specific primers. The fluorescence was captured by the detector and generates a graph in the real plex software as the amount of fluorescence against the number of cycles. The dye emits the fluorescence in the form of peaks. The cycle number at which fluorescence has initiated is called as “Ct value.” Test samples were run and Ct values for respective samples were obtained. Quantities were obtained by plotting Ct value (Cycle number at which peak has been generated) of each sample on standard curve.
Intervention
Was carried out only for the halitosis group (n = 120). After baseline clinical and microbiological examination, the participants were randomly allocated by lottery method to three groups; Group 1 (n = 40) – Melaleuca alternifolia (Tree tea oil), Dessert Essence, US). Group 2 (n = 40) – Chlorhexidine gluconate 0.2% (Maxxio, Alkem Laboratories, India) and Group 3-Placebo (n = 40). Both the mouth rinses and the placebo were put in nontransparent bottles sealed with a screw cap. Labeled mouthrinses including of the two active rinses and the placebo rinse were dispensed to all the participants randomly by the dental hygienist and the individuals who were blinded to the contents of the mouth rinse. The individuals were asked to rinse with undiluted, 10 mL of the allocated mouth rinse, twice a day for half a minute and period of 1 week. For checking with the compliance, the individuals were recalled every alternate day with the bottle and the levels of the mouth rinse were checked by the same hygienist who dispensed the mouth rinse. For the entire study period, all the recruited individuals were provided with regular toothpaste and toothbrush.
Recall visits
All the included individuals (halitosis) were recalled after 7 days and evaluation of halitosis parameters, clinical and microbiological parameters was done as the baseline visits. For the nonhalitosis group of patients, only the baseline statistics was considered. No adverse effects were noted in any of the groups. The placebo group received free samples of chlorhexidine immediately post trial period.
Statistical analysis
Was done using SPSS for Windows, Version 22.0. Armonk, NY, USA. Descriptive Statistics includes the expression of the study variables with categorical data in terms of number and percentage whereas in mean and standard deviation (SD) for continuous data. The One-way ANOVA test followed by Tukey's post hoc analysis was used to compare the mean values of various parameters at pre-test and post-test periods between different study groups. Student paired t-test was used to compare the mean values of various parameters including the copy numbers of salivary and tongue S. moorie counts. Statistical significance was set at P < 0.05. Two individuals were lost in the follow-up so the statistical analysis was carried out for 118 test group and 40 nonhalitosis group.
Results
A total of 158 subjects including 69.4% males and 30.6% females completed the study. The mean age for halitosis group was 33.1 years (SD 11.2; range 20–53 years) and for the nonhalitosis group was 32.3 years (SD 11.4; range 19–59 years), respectively. 100% prevalence of S. moorei was seen in saliva and tongue coating of the halitosis group compared to 16% in the tongue and 24% in saliva in the nonhalitosis group [Table 1].
Table 1.
Baseline prevalence of Solobacterium Moorei in tongue and salivary samples between groups
| Groups | Number of Patients | Age | Gender | SM saliva | SM TC | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Male | Female | Percentage | Counts | Percentage | Counts | |||
| Halitosis | 120 | 33.1 | 112 | 38 | 100 | 9.45 | 100 | 8.75 |
| Nonhalitosis | 40 | 32 | 31 | 19 | 16.6 | 0.83 | 24 | 1.03 |
SM: Solobacterium moorei SM Saliva=SM counts in saliva, SM TC=SM counts in tongue coating
Baseline observation
The mean halitosis score (OLR, VSC), dental plaque and tongue coating scores are tabulated in Table 2 and the mean scores for the test groups (Groups 1, 2, and 3) did not show any significant difference between them. However, the difference between the test and the nonhalitosis groups showed a significant difference for the halitosis score (OLR, VSC) and tongue coating scores at P < 0.001. Clinical results: Both Melaleuca alternifolia (TTO) group and chlorhexidine group showed a significant reduction in the halitosis score (OLR, VSC) at P < 0.001. S. moorei levels of both saliva and tongue showed statistically significant reduction in both the test groups at P < 0.001 when compared to placebo group where the counts of S. moorei marginally increased in both saliva and tongue coating. The mean reduction of OLR scores (1.42) and S. moorei levels (5.67 log10 copies/mL) in saliva was higher in TTO group than the other two groups at P < 0.001. Chlorhexidine group showed higher mean reduction for S. moorei levels in the tongue (2.92 log10 copies/mL) and VSC levels when compared to TTO group (2.34 log10 copies/mL) and the placebo group [Table 3].
Table 2.
Inter group comparison (pre and post)
| Groups | Mean | SD | SE | P | Groups | Mean | SD | SE | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| OLR | 1 | 3.67 | 1.07 | 0.36 | 0.00* | 1 | 2.25 | 0.87 | 0.26 | 0.03 |
| 2 | 3.08 | 0.52 | 0.22 | 2 | 1.92 | 0.52 | 0.18 | |||
| 3 | 2.83 | 0.84 | 0.24 | 3 | 2.83 | 0.84 | 0.24 | |||
| 4 | 1.08 | 0.79 | 0.05 | 4 | 2.25 | 0.62 | 0.15 | |||
| VSC | 1 | 525.75 | 266.35 | 77.11 | 0.00* | 1 | 238.33 | 179.74 | 51.89 | 0.002* |
| 2 | 483.08 | 256.34 | 74.00 | 2 | 180.17 | 120.81 | 34.87 | |||
| 3 | 404.50 | 241.49 | 69.71 | 3 | 388.67 | 245.74 | 73.76 | |||
| 4 | 74.08 | 22.32 | 12.01 | 4 | 109 | 75.33 | 21.74 | |||
| PI | 1 | 1.60 | 0.34 | 0.1 | 0.027 | 1 | 1.15 | 0.20 | 0.07 | 0.93 |
| 2 | 1.55 | 0.18 | 0.07 | 2 | 1.16 | 0.16 | 0.08 | |||
| 3 | 1.27 | 0.31 | 0.05 | 3 | 1.15 | 0.19 | 0.04 | |||
| 4 | 1.45 | 0.26 | 0.1 | 4 | 1.12 | 0.17 | 0.09 | |||
| TCI | 1 | 2.17 | 2.82 | 0.17 | 0.001* | 1 | 1.83 | 0.58 | 0.81 | 0.314 |
| 2 | 1.33 | 0.492 | 0.14 | 2 | 1.08 | 0.29 | 0.08 | |||
| 3 | 1.5 | 0.52 | 0.15 | 3 | 1.42 | 0.51 | 0.15 | |||
| 4 | 0.58 | 0.515 | 0.04 | 4 | 1.33 | 0.49 | 0.14 | |||
| SM saliva | 1 | 9.86 | 2.04 | 2.5 | 0.89 | 1 | 4.19 | 1.66 | 4.18 | <0.001* |
| 2 | 9.23 | 3.51 | 4.76 | 2 | 3.85 | 1.69 | 1.83 | |||
| 3 | 9.36 | 1.37 | 9.93 | 3 | 9.26 | 2.28 | 4.79 | |||
| 4 | 9.15 | 2.08 | 4.88 | 4 | 5.64 | 2.54 | 4.53 | |||
| SM TC | 1 | 8.55 | 1.05 | 2.44 | 0.3 | 1 | 6.21 | 1.29 | 2.32 | <0.001* |
| 2 | 9.73 | 1.46 | 4.59 | 2 | 6.01 | 1.72 | 2.99 | |||
| 3 | 8.92 | 1.6 | 6.21 | 3 | 8.83 | 2.14 | 5.25 | |||
| 4 | 8.79 | 2.09 | 5.54 | 4 | 4.25 | 1.03 | 3.43 |
*Significance P≤0.05. Counts in log 10 copies/ml. SM=Solobacterium moorei, SM Saliva=SM counts in saliva, SM TC=SM counts in tongue coating, OLR=Organoleptic scores, VSC=Volatile sulphur compounds, PI=Plaque index, TC: Tongue coating. TCI=TC index, Group 1: Melaleuca alternifolia (TTO), TTO=Tea tree oil, Group 2=Chlorhexidine, Group 3=Placebo, SD=Standard deviation, SE=Standard error
Table 3.
Comparison of mouth washes on halitosis and Solobacterium moorie levels using student paired t-test
| Variable | Pre | Post | Mean different | P | |
|---|---|---|---|---|---|
| Group 1 | OLR | 3.67 | 2.25 | 1.42 | <0.001* |
| VSC | 525.92 | 238.33 | 287.59 | <0.001* | |
| Mean CT of SM in saliva | 9.86 | 4.19 | 9.86 | <0.001* | |
| Mean CT of SM from TC | 8.55 | 6.21 | 2.34 | <0.001* | |
| PI | 1.21 | 1.15 | 0.06 | <0.001* | |
| TCI | 2.17 | 1.83 | 0.34 | <0.001* | |
| Group 2 | OLR | 3.08 | 1.92 | 1.16 | <0.001* |
| VSC | 483.08 | 180.17 | 302.91 | <0.001* | |
| Mean CT of SM in saliva | 9.36 | 3.85 | 5.51 | <0.001* | |
| Mean CT of SM from TC | 8.92 | 6.00 | 2.92 | <0.001* | |
| PI | 1.29 | 1.15 | 0.14 | <0.001* | |
| TCI | 1.33 | 1.08 | 0.25 | <0.001* | |
| Group 3 | OLR | 2.83 | 2.83 | 0.00 | NA |
| VSC | 404.50 | 388.67 | 15.83 | 0.35 | |
| Mean CT of SM in saliva | 9.15 | 9.26 | −0.11 | 0.54 | |
| Mean CT of SM from TC | 8.79 | 8.83 | −0.04 | 0.61 | |
| PI | 1.13 | 1.12 | 0.02 | 0.001* | |
| TCI | 1.5 | 1.42 | 0.08 | 0.59 |
*Significance P≤0.05. Group 1=Melaleuca alternifolia (TTO), TTO=Tea tree oil, Group 2=Chlorhexidine, Group 3=Placebo, OLR=Organoleptic scores, VSC=Volatile sulphur compounds, SM=Solobacterium moorei, PI=Plaque score, TC=Tongue coating, TCI=Tongue coating index, NA=Statistics not applicable as pretest value is equal to posttest value, CT=Cycle threshold
Inter group comparison
Both TTO group and chlorhexidine group showed statistically significant reduction in all parameters when compared to the placebo group at P < 0.001. TTO group was found to be equally effective as chlorhexidine group for reduction in halitosis score (OLR, VSC), S. moorei levels of tongue and saliva, and tongue coating index score [Tables 2 and 4].
Table 4.
Multiple comparison for mean differences between the groups using Tukey’s honest significant difference post hoc analysis
| Parameters | Group 1 versus Group 2 | Group 1 versus Group 3 | Group 2 versus Group 3 |
|---|---|---|---|
| OLR | 0.68 | 0.01* | 0.02* |
| VSC | 0.25 | 0.001* | 0.001* |
| TCI | 0.46 | <0.05 | <0.04 |
| PI | 1.00 | 0.96 | 0.96 |
| SM saliva | 0.98 | <0.001* | 0.001* |
| SM TC | 0.99 | 0.001* | <0.001* |
*Significance P≤0.05. OLR=Organoleptic scores, VSC=Volatile sulphur compounds, PI=Plaque index, TC=Tongue coating, TCI=Tongue coating index, Group 1=Melaleuca alternifolia (TTO), Group 2=Chlorhexidine, Group 3=Placebo, TTO=Tea tree oil, SM=Solobacterium moorei, SM Saliva=SM counts in saliva, SM TC=SM counts in tongue coating
Discussion
Globally halitosis has a very deep social, economical, and psychological impact on individuals. The formation of VSCs is largely by the breakdown of proteins to sulfur-containing substances by the microbiome in the oral cavity are the most common cause for oral halitosis.[18] Although over 600 species of microorganisms can produce increased VSCs, majority of which are even normal commensal and seen in nonhalitosis individuals.[19] Halitosis is closely related to the presence of S. moorei in the oral cavity. S. moorei produces hydrogen sulfide from the products of protein degradation by specific proteolytic enzymes which can be either derived by the host or derived by the bacteria themselves.[20]
Hence to reduce malodor, it is important to decrease the levels of S. moorei in the mouth. With this background this randomized clinical trial was designed to evaluate the effect of two mouth rinses, one with Melaleuca alternifolia (TTO) and other 0.2% chlorhexidine gluconate, on the malodor and bacterial scores in saliva and tongue coating samples. Among individuals with oral malodor, it has shown that the tongue coating has a significant influence. S. moorei is found along other bacterial species by forming a biofilm on the surface of the tongue making it difficult for the antimicrobial agents to act. To the best of our knowledge, the effect of TTO on salivary S. moorei levels in halitosis individuals has not been previously investigated. In this study, S. moorei was detected in 100% of individuals (both salivary and tongue coating samples) of the halitosis group while in the nonhalitosis group S. moorei levels was almost negligible which is in accordance with the study done by Vancauwenberghe et al. in 2013[8] who reported higher amounts and detection frequency of S. moorei in patients with oral malodor. It has been speculated that the microorganisms of the tongue and saliva have been similar while the dental plaque to be different in halitosis individuals.[21]
The observations in this clinical trial showed significant reduction in S. moorei counts and halitosis score (organoleptic and VSC) in the groups with active mouth rinse than the placebo groups indicating that both Melaleuca alternifolia (TTO), a natural derivative and chlorhexidine an antiseptic mouth rinse are able to reduce or mask the volatile compounds in the mouth and thereby can be of importance in the treatment of halitosis. Of the two tested mouthwashes, TTO has shown more reduction in levels of S. moorei in saliva and OLR scores compared to other two. While the chlorhexidine group showed higher reduction in the levels of S. moorei in tongue and VSC score. This may suggest that TTO may be more or equally effective as chlorhexidine against S. moorei and aid in the treatment of halitosis by reducing the VSC scores. This is in accordance with the study done by Forrer et al. in 2013[22] where he reported that TTO was potent against S moorei strain with concentrations 0.5%. It has also been reported that TTO is effective against wider range of bacterial species, yeast and fungi. The minimum inhibitory concentrations ranges from 0.003% to 2% for various oral bacteria.[23]
Chlorhexidine mouth rinse in our study has shown to be effective against the halitosis-associated bacterium S. moorei. Literature evidence suggests it to be a gold standard for the treatment of oral halitosis due to its broad antimicrobial spectrum and substantivity.[24] The common reported side effects of this rinse are tooth staining, taste disturbance and irritation of the oral mucosa restricts its long term usage.[25] Hence, several clinical studies report a combination of lower concentrations of chlorhexidine and Zinc to be used. This combination has and shown to reduce both VSC levels and bacteria levels.[26,27] Reports have shown that coating on the dorsum of the tongue is related to the bacterial load. This in turn is responsible for increased VSC's production in healthy individuals. Among the tested mouth rinses, chlorhexidine group showed greater reduction in S. moorei counts from tongue coating samples than the TTO group this can be explained by the low substantivity or loss of its antibacterial properties once bounded to oral tissues of the tree tea oil mouth rinse.[28,29] The values of the tongue coating index in our study showed no differences before and after treatment in both the test groups. Based on these observations, one can hypothesize that the composition of the tongue coating with bacteria such as S. moorei rather than the extent of the tongue coating is an important determinant of oral halitosis. Plaque index scores showed significant reductions in all groups during post test period. No significant intergroup differences were seen between the three mouthwashes used in the study. However, chlorhexidine showed more reduction in mean plaque scores which may suggest its use as an effective anti-plaque agent. Rahman et al. in 2014[30] compared the anti-plaque and anti-gingivitis effect of 4 mouthwashes, i.e., Tree Tea Oil, cetylpyridinium chloride (CPC), chlorhexidine and placebo, and reported more plaque reduction in Chlorhexidine and CPC group than TTO and placebo group. Commercial mouth washes used in the treatment of halitosis are many; although some may help in making the malodor the main objective should be of reduction of causative microorganisms which aid in production of VSC's.
This study has some limitation. Although this study was carried in different population and different oral condition, we could have opted for cross over design than parallel design with wash over period which would have made the results more authenticated. Further studies are needed to evaluate and compare various odoriferous chemicals produced by the other oral bacteria and S. moorei to understand the contributions of various microbial nische toward genuine oral halitosis.
Conclusion
The results show that both Melaleuca alternifolia (TTO) and chlorhexidine mouth rinses significantly reduce oral malodor scores and VSC levels after 1 week of usage. The S. moorei levels of saliva and tongue coating are also reduced equally by both chlorhexidine and tree tea oil rinses. Hence, we feel that Melaleuca alternifolia (TTO) mouth rinse is a promising natural alternative to chlorhexidine rinse to treat oral halitosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge Dr. Deepa Bullapa, Department of Bio-statistics for the Statistical analysis.
References
- 1.Hampelska K, Jaworska MM, Babalska ZŁ Karpiński TM. The role of oral microbiota in intra-oral halitosis. J Clin Med. 2020;9:2484. doi: 10.3390/jcm9082484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon DF, Jr, Gibbons RJ. Studies of the predominant cultivable micro-organisms from the human tongue. Arch Oral Biol. 1966;11:627–32. doi: 10.1016/0003-9969(66)90229-9. [DOI] [PubMed] [Google Scholar]
- 3.Barrak I, Stájer A, Gajdács M, Urbán E. Small, but smelly: The importance of Solobacterium moorei in halitosis and other human infections. Heliyon. 2020;6:e05371. doi: 10.1016/j.heliyon.2020.e05371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Awano S, Gohara K, Kurihara E, Ansai T, Takehara T. The relationship between the presence of periodontopathogenic bacteria in saliva and halitosis. Int Dent J. 2002;52(Suppl 3):212–6. doi: 10.1002/j.1875-595x.2002.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 5.Lau SK, Teng JL, Leung KW, Li NK, Ng KH, Chau KY, et al. Bacteremia caused by Solobacterium moorei in a patient with acute proctitis and carcinoma of the cervix. J Clin Microbiol. 2006;44:3031–4. doi: 10.1128/JCM.00555-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detry G, Pierard D, Vandoorslaer K, Wauters G, Avesani V, Glupczynski Y. Septicemia due to Solobacterium moorei in a patient with multiple myeloma. Anaerobe. 2006;12:160–2. doi: 10.1016/j.anaerobe.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Zheng G, Summanen PH, Talan D, Bennion R, Rowlinson MC, Finegold SM. Phenotypic and molecular characterization of Solobacterium moorei isolates from patients with wound infection. J Clin Microbiol. 2010;48:873–6. doi: 10.1128/JCM.01381-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vancauwenberghe F, Dadamio J, Laleman I, Van Tornout M, Teughels W, Coucke W, et al. The role of Solobacterium moorei in oral malodour. J Breath Res. 2013;7:046006. doi: 10.1088/1752-7155/7/4/046006. [DOI] [PubMed] [Google Scholar]
- 9.Rosenberg M, Septon I, Eli I, Bar-Ness R, Gelernter I, Brenner S, et al. Halitosis measurement by an industrial sulphide monitor. J Periodontol. 1991;62:487–9. doi: 10.1902/jop.1991.62.8.487. [DOI] [PubMed] [Google Scholar]
- 10.Shunin Y, Bellucci S, Gopeynko V, Lobanova-shunina T, Kiv A, Dfink , et al. Nanosensor devices for CBRN agents detection; theory and design. In: Nano Structural Materials for Detection of CBRN. NATO science for peace and securities series A. Chemistry and Biology (NAPSA) 2018:169–84. [Google Scholar]
- 11.Paraskevas S. Randomized controlled clinical trials on agents used for chemical plaque control. Int J Dent Hyg. 2005;3:162–78. doi: 10.1111/j.1601-5037.2005.00145.x. [DOI] [PubMed] [Google Scholar]
- 12.Mandel ID. Chemotherapeutic agents for controlling plaque and gingivitis. J Clin Periodontol. 1988;15:488–98. doi: 10.1111/j.1600-051x.1988.tb01020.x. [DOI] [PubMed] [Google Scholar]
- 13.Salvatori C, Barchi L, Guzzo F, Gargari M. A comparative study of antibacterial and anti-inflammatory effects of mouthrinse containing tea tree oil. Oral Implantol (Rome) 2017;10:59–70. doi: 10.11138/orl/2017.10.1.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.European Medicines Agency. London: EMA; 2013. Assessment Report on Melaleuca alternifolia (Maiden and Betch) Cheel, M. linariifolia Smith, M. dissitiflora F. Mueller and/or Other Species of Melaleuca, Aetheroleum. [Google Scholar]
- 15.Rosenberg M. Clinical assessment of bad breath: Current concepts. J Am Dent Assoc. 1996;127:475–82. doi: 10.14219/jada.archive.1996.0239. [DOI] [PubMed] [Google Scholar]
- 16.Shimizu T, Ueda T, Sakurai K. New method for evaluation of tongue-coating status. J Oral Rehabil. 2007;34:442–7. doi: 10.1111/j.1365-2842.2007.01733.x. [DOI] [PubMed] [Google Scholar]
- 17.Loe H. The gingival index, the plaque index and the retention index system. J Periodontol. 1967;38:610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 18.Kazor CE, Mitchell PM, Lee AM, Stokes LN, Loesche WJ, Dewhirst FE, et al. Diversity of bacterial populations on the tongue dorsa of patients with halitosis and healthy patients. J Clin Microbiol. 2003;41:558–63. doi: 10.1128/JCM.41.2.558-563.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Boever EH, Loesche WJ. Assessing the contribution of anaerobic microflora of the tongue to oral malodor. J Am Dent Assoc. 1995;126:1384–93. doi: 10.14219/jada.archive.1995.0049. [DOI] [PubMed] [Google Scholar]
- 20.Tanabe S, Grenier D. Characterization of volatile sulfur compound production by Solobacterium moorei. Arch Oral Biol. 2012;57:1639–43. doi: 10.1016/j.archoralbio.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Mager DL, Ximenez-Fyvie LA, Haffajee AD, Socransky SS. Distribution of selected bacterial species on intraoral surfaces. J Clin Periodontol. 2003;30:644–54. doi: 10.1034/j.1600-051x.2003.00376.x. [DOI] [PubMed] [Google Scholar]
- 22.Forrer M, Kulik EM, Filippi A, Waltimo T. The antimicrobial activity of alpha-bisabolol and tea tree oil against Solobacterium moorei, a Gram-positive bacterium associated with halitosis. Arch Oral Biol. 2013;58:10–6. doi: 10.1016/j.archoralbio.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Hammer KA, Dry L, Johnson M, Michalak EM, Carson CF, Riley TV. Susceptibility of oral bacteria to Melaleuca alternifolia (tea tree) oil in vitro. Oral Microbiol Immunol. 2003;18:389–92. doi: 10.1046/j.0902-0055.2003.00105.x. [DOI] [PubMed] [Google Scholar]
- 24.Pedrazzi V V, do Nascimento C, Mardegan Issa JP, Fedorowicz Z. Interventions for managing halitosis (Protocol) Cochrane database of systematic reviews. 2016;5:1–9. [Google Scholar]
- 25.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79:119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 26.Young A, Jonski G, Rölla G. Combined effect of zinc ions and cationic antibacterial agents on intraoral volatile sulphur compounds (VSC) Int Dent J. 2003;53:237–42. doi: 10.1111/j.1875-595x.2003.tb00751.x. [DOI] [PubMed] [Google Scholar]
- 27.Saad S, Greenman J, Shaw H. Comparative effects of various commercially available mouthrinse formulations on oral malodor. Oral Dis. 2011;17:180–6. doi: 10.1111/j.1601-0825.2010.01714.x. [DOI] [PubMed] [Google Scholar]
- 28.Carson CF, Riley TV. Antimicrobial activity of the major components of the essential oil of Melaleuca alternifolia. J Appl Bacteriol. 1995;78:264–9. doi: 10.1111/j.1365-2672.1995.tb05025.x. [DOI] [PubMed] [Google Scholar]
- 29.May J, Chan CH, King A, Williams L, French GL. Time-kill studies of tea tree oils on clinical isolates. J Antimicrob Chemother. 2000;45:639–43. doi: 10.1093/jac/45.5.639. [DOI] [PubMed] [Google Scholar]
- 30.Rahman B, Alkawas S, Al Zubaidi EA, Adel OI, Hawas N. Comparative antiplaque and antigingivitis effectiveness of tea tree oil mouthwash and a cetylpyridinium chloride mouthwash: A randomized controlled crossover study. Contemp Clin Dent. 2014;5:466–70. doi: 10.4103/0976-237X.142813. [DOI] [PMC free article] [PubMed] [Google Scholar]


