Abstract
Introduction
Correctly identifying people with suspected stroke is essential for ensuring rapid treatment. Our aims were to determine the sensitivity of emergency dispatcher and paramedic identification of patients with stroke, the factors associated with correct identification, and whether there were any implications for hospital arrival times.
Methods
Observational study using patient‐level data from the Australian Stroke Clinical Registry (2015–2017) linked with ambulance and emergency department records for the state of Victoria. The registry diagnosis was the reference standard to compare with the provisional diagnoses made by emergency services personnel classified as “suspected” and “not suspected” stroke/transient ischemic attack (TIA). Multivariable logistic and quintile regressions were used to determine factors associated with correct identification and timely arrival to hospital.
Results
Overall, 4717 (64%) were matched to ambulance transport records (median age: 73 years, 43% female). Stroke/TIA was suspected in 56% of registrants by call‐takers and 69% by paramedics. Older patients (75+ years) (adjusted odds ratio [aOR]: 0.61; 95% confidence interval [CI]: 0.49–0.75), females (aOR: 0.86; 95% CI: 0.75–0.99), those with severe stroke or intracerebral hemorrhage were less often suspected as stroke. Cases identified as stroke had a shorter arrival time to hospital (unadjusted median minutes: stroke, 54 [43, 72] vs not stroke, 66 [51, 89]).
Conclusions
Emergency dispatchers and paramedics identified over half of patients with stroke in the prehospital setting. Important patient characteristics, such as being female and those having a severe stroke, were found that may enable refinement of prehospital ambulance protocols and dispatcher/paramedic education. Those correctly identified as stroke, arrived earlier to hospital optimizing their chances of receiving time‐critical treatments.
Keywords: ambulances, big data, emergency medical services, paramedics, prehospital, registries, sensitivity, stroke
1. INTRODUCTION
1.1. Background
Emergency medical services (EMS) have a crucial role in the stroke chain of survival by providing urgent medical assessment and transport to hospital. Ensuring access to time‐critical reperfusion treatment and organized care in stroke units significantly reduces patient disability or mortality after stroke. 1 Accurate and timely recognition of stroke‐like symptoms in patients suspected with stroke in the prehospital setting improves patient outcomes. 1 , 2 , 3 In Australia, it is estimated that 71% of patients with stroke are transported by ambulance to hospitals capable of providing reperfusion therapies. 4
1.2. Importance
EMS personnel can facilitate the rapid identification, assessment, triage and prenotification of hospitals for patients with suspected stroke. 3 , 5 Although several studies have been conducted to assess the accurate identification of patients with stroke in the prehospital setting, 6 , 7 it's unclear how patient, clinical, and system factors influence the identification of stroke by EMS personnel. 6 , 8
1.3. Goals of the study
The goals of this study were to (1) determine the sensitivity of emergency dispatcher and paramedic (collectively EMS personnel) identification of patients with stroke, (2) understand the factors associated with EMS personnel recognition of patients with stroke in the prehospital setting, and (3) identify whether there were any implications for time to hospital arrival.
1.4. Methods
1.4.1. Study design
This is a retrospective, observational study using patient‐level data from the Australian Stroke Clinical Registry (AuSCR), linked with data from Ambulance Victoria (AV) and the Victorian Emergency Minimum Dataset (VEMD). Ethics approval for this study was provided by the Monash University Human Research Ethics Committee (MUHREC 12770).
1.4.2. Study setting
Ambulance Victoria is the sole provider of EMS in the state of Victoria, covering a landmass of 227,038 square kilometres. 9 The ambulance service operates on a 2‐tiered response system consisting of advanced life support and intensive care paramedics. 10 Non‐clinical EMS dispatchers (Certificate II/III in Emergency Communications) use the Medical Priority Dispatch System (MPDS; International Academies of Emergency Dispatch, Salt Lake City, Utah, United States) to identify patients with suspected stroke (MPDS Card 28). This emergency call‐taking service is provided by the Emergency Services Telecommunications Authority, which is a separate entity to AV. For on‐scene patient assessment where stroke is suspected, paramedics are recommended to use the Melbourne Ambulance Stroke Screening (MASS) tool, transport to appropriate destination (thrombolyzing, endovascular clot retrieval or neurosurgical stroke center) and notify (general radio) the hospital in advance of their arrival in addition to their standard assessment and management protocols. The MASS is a validated tool and its strengths are reported elsewhere. 11 , 12
In Australia, it is recommended that the initial contact with the health system for patients with suspected stroke is through a nationally‐used emergency telephone number (Triple Zero: 000). 13 The emergency dispatchers interview the callers to determine the nature of the call and type of incident and assign the urgency of response required based on predetermined dispatch criteria. Priority cases are quickly identified, and an emergency ambulance is dispatched for time‐dependent cases (immediate response—lights and sirens). 14 Cases considered to be non‐urgent are further assessed (secondary triage) by a paramedic or registered nurse who may dispatch an emergency ambulance or provide alternate options to an emergency ambulance (eg, referral to a doctor or pharmacist, or advice for self‐management). 10
During the period of this study, patients suspected of stroke by emergency dispatchers were assigned a stroke primary complaint, which could either be a priority 1 (lights and sirens, stroke symptom onset less than 6 hours), priority 2 (urgent), or a priority 3 ambulance dispatch (non‐urgent, symptom onset more than 6 hours).
1.4.3. Data sources
Briefly, we identified stroke cases from the AuSCR. The AuSCR is a national, voluntary, clinical quality disease registry designed to systematically and routinely collect data on all patients with stroke or transient ischemic attack (TIA) admitted to participating hospitals. 15 , 20 The primary purpose of collecting these nationally representative data on all stroke admissions is to monitor and improve the quality of stroke care. 16 Registrants are routinely followed up between 90 and 180 days after stroke. 15
Ambulance Victoria collects data for patient management, monitoring performance measurement and research purposes. In 2008, AV completed its rollout of electronic patient care records (ePCR) across the state. 17 Operational data are collected during dispatch processes (eg, priority dispatch) and clinical information are collected by paramedics during patient care provision and management. The data are stored in an integrated data warehouse. 17 The ePCR records includes demographic information, case time series information, pickup location, symptoms, vital signs and preexisting conditions, plus paramedic diagnosis and clinical management information.
The VEMD is an emergency data set collected according to the processes specified in the Emergency Department Care National Minimum Data Set standards. 18 It is a data set that includes information provided to state government on emergency department presentations at Victorian public hospitals. The data collected include demographic, administrative, and clinical information. The VEMD data set is obtained to enable comparisons of ED operations and management (particularly access to services).
The Bottom Line
The Bottom Line: Correct identification of stroke or transient ischemic attack (TIA) is essential for ensuring rapid treatment. In this analysis of 4255 strokes and TIAs identified from linked Australian stroke, ambulance, and emergency department records, emergency dispatchers, and paramedics suspected stroke or TIA in 56% and 69%, respectively. Age >75 years, female sex, and those with severe stroke or intracerebral hemorrhage were less often suspected as stroke or TIA. These findings lay the foundation for novel stroke identification strategies.
As Australian residents do not have a single unique health identifier, AuSCR registrants’ personal identifiers (names, date of birth [DOB], date of arrival at ED) were submitted to the AV Centre for Research and Evaluation for matching. 19 Detailed methods for this linkage have been published. 20 Briefly, a probabilistic (“fuzzy”) data linkage algorithm was employed using Stata (StataCorp, Texas, United States) and WinPure Clean & Match Enterprise (version 7.3.6.1, WinPure, New York, United States) software. Data were linked and verified in several stages (Figure 1) using different criteria in order to maximize the linkage rate. In the first stage, matching was performed using full name, DOB, and date of arrival at ED or date of admission and match scores >0.75 were assumed to be true matches. In the second stage, variables were the three first letters of first and last names, DOB, and the date of the call receipt (used to match to date of arrival at ED or date of admission) and match scores of ≥ 80% resulted in the observations being linked together. In the final stage, additional records identified in Stage 2 were added to the merged records from Stage 1. Manual review of both matches and non‐matches was performed to ensure linkage accuracy.
FIGURE 1.
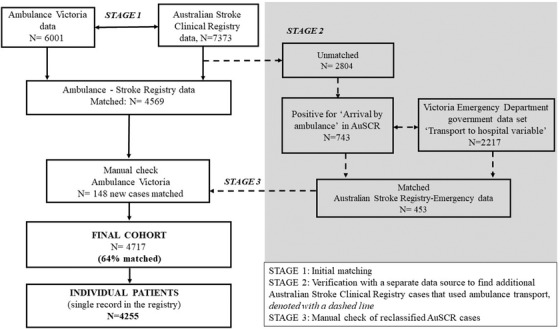
Linkage and merging of the stroke registry data with ambulance and emergency records. AuSCR, Australian Stroke Clinical Registry
1.4.4. EMS dispatcher and personnel identification of suspected stroke
Emergency dispatchers identified suspected strokes through the interview of callers to the national emergency telephone number as described above. The type of event in the ambulance records recorded by the emergency dispatchers was coded as “suspected stroke” (MPDS version 12.2 Event Type 28A1C – 28C12Z) or “other suspected conditions” for all other events. Our goal was to focus on the ability of the emergency dispatchers to identify stroke cases using the MPDS algorithm. The final primary assessments recorded by paramedics during patient management at the scene (“intracranial hemorrhage,” “stroke,” “subarachnoid hemorrhage,” and “TIA”) were coded as “suspected stroke” and all other assessments were coded as “other suspected conditions.” Though subarachnoid hemorrhages are not counted in the AuSCR (may present differently, including with thunderclap headache alone), these were included based on paramedic suspicion of stroke at the scene. TIA is relevant to include in this study because the symptoms experienced in the prehospital setting can be the same as stroke, and it is appropriate to call for an emergency ambulance even though symptoms are transient but may last up to 24 hours. 21 For simplicity, in the prehospital setting all will be referred to as “suspected stroke” to encapsulate patients with stroke or TIA.
1.4.5. Selection of subjects
The study included confirmed stroke patients ≥18 years in the AuSCR registry who arrived at the hospital by EMS between January 2015 and October 2017. We excluded patients with an onset of stroke during their hospital admission for another condition or if they had been transferred between hospitals.
1.4.6. Outcomes
The primary outcome of this study was to determine the sensitivity of correct identification of stroke by EMS personnel (emergency dispatchers and paramedics) and to determine the factors associated with correct identification of stroke in the prehospital setting. The AuSCR diagnosis confirmed in hospital was used as the reference standard to compare the provisional diagnoses made by ambulance personnel.
Our secondary outcome was to determine the time intervals at various points in the evaluation and management of these patients. We considered “time zero” for each patient as time from when call was received. We examined time intervals between patients suspected of stroke compared to patients not suspected of stroke as follows: calling for an ambulance to arrival at scene, calling for ambulance to arrival at patient, arrival at scene to loading patient onto stretcher, time from loading patient to arrival at hospital, time from arrival at hospital door to off stretcher, time from arrival at hospital door, calling for an ambulance to arrival at hospital, and arrival at scene to ambulance arriving at hospital.
1.4.7. Data analysis
We divided the data set into two groups: EMS suspected stroke and not suspected stroke. We compared patient demographics, type of stroke, stroke severity (inability to walk admission), documented previous stroke, time of onset of symptoms (within 4.5 vs beyond 4.5 hours), place of residence (rural vs metropolitan), born in Australia, and whether an interpreter was required at the time of the call. These variables were selected based on literature, theory, logical reasoning, their importance in biological relationships, and correct identification of stroke and availability for analysis. We used the Accessibility/Remoteness Index of Australia to classify remoteness of patient's place of residence (metropolitan vs regional). 22 Ability to walk at the time of hospital admission (coded as yes/no) was used as a proxy for stroke severity. 23
Categorical variables were summarized as frequencies and percentages and continuous variables as median and interquartile range. Differences in characteristics between patients suspected of stroke and patients not suspected of stroke, and other variables were compared using Kruskal‐Wallis tests for continuous variables (eg, call receipt to arrival at hospital) and Pearson's X 2 tests for categorical variables. We determined the sensitivity for correct stroke identification by EMS dispatchers and personnel.
Using logistic regression, we identified factors associated with correct call‐taker identification of stroke. To identify a parsimonious set of variables independently associated with correct identification of stroke by EMS personnel, we identified all variables that were statistically significant on univariate analysis and entered them into a multivariable model. We repeated the analysis to identify factors independently associated with correct paramedic identification of stroke.
We conducted quantile regression analyses to identify differences in time metrics between patients suspected of stroke and patients not suspected of stroke. We undertook sensitivity analyses of factors associated with correctly identifying stroke using the final multivariable regression models comprising all variables investigated. All analyses were performed using Stata/SE (version 15.0, StataCorp, Texas, United States). A p < 0.05 was considered statistically significant.
1.5. Results
Overall, there were 4717 (64% of 7373) patient admissions for stroke recorded from the registry that had a corresponding record with the ambulance data (Figure 1). This analysis was performed on 4255 unique patients (denominator) with a single record in the registry.
1.5.1. Emergency dispatchers’ stroke suspicion
Patient characteristics according to suspicion of stroke by emergency dispatchers are displayed in Table 1. Emergency dispatchers suspected 2383 (56%) patients as having a stroke. Other conditions suspected by emergency dispatchers were unconsciousness (11%), falls 4%, chest pain (4%), breathing problems (2%), headaches (1%), and convulsions or seizures (1%) (Table S1). Females and those who required an interpreter during the emergency telephone call were less likely to be identified by emergency dispatchers as having a stroke compared to males or those who did not require an interpreter, respectively. Patients with stroke symptom onset less than 4.5 hours and who were born in Australia were more likely to be suspected as having a stroke. Emergency dispatchers were less likely to suspect stroke in patients with intracerebral hemorrhage and those who were later determined to be unable to walk on admission. Patients who were suspected of stroke by emergency dispatchers were more likely to have a Code 1 immediate (light and sirens) ambulance response and more often had the highest transport priority compared to those not suspected of stroke (Table 2). Those not suspected of stroke by emergency dispatchers had a slower response time of 11 minutes for paramedic arrival at scene.
TABLE 1.
Characteristics of AuSCR confirmed stroke patients, and associations with correct emergency dispatcher identification of stroke
|
Emergency dispatchers Suspected stroke/TIA N = 2383 N (%) |
Emergency dispatchers No suspected stroke/TIA N = 1872 N (%) |
Unadjusted analyses OR (95% CI) |
Adjusted analyses aOR (95% CI) |
|
|---|---|---|---|---|
| Female | 951 (40) | 847 (45) | 0.80 (0.71–0.91) | 0.86 (0.75–0.99) |
| Age (in years) | ||||
| Less than 65 | 684 (29) | 478 (26) | Reference | Reference |
| 65–74 | 781 (33) | 569 (31) | 0.96 (0.82–1.12) | 1.03 (0.86–1.23) |
| 75+ | 918 (39) | 825 (44) | 0.78 (0.67–0.90) | 0.87 (0.73–1.03) |
| Born in Australia | 1513 (63) | 1130 (60) | 1.14 (1.01–1.29) | 1.09 (0.93–1.27) |
| Interpreter required a | 137 (6) | 149 (8) | 0.70 (0.55–0.90) | 0.92 (0.70–1.22) |
| Onset of symptoms <4.5 hours | 1253 (54) | 725 (40) | 1.76 (1.55–1.99) | 1.77 (1.54–2.02) |
| Type of stroke b | ||||
| Ischemic | 1516 (65) | 1206 (66) | Reference | Reference |
| Intracerebral hemorrhage | 215 (9) | 277 (15) | 0.62 (0.51–0.75) | 0.61 (0.49–0.75) |
| Transient ischemic attack | 547 (23) | 301 (17) | 1.45 (1.23–1.70) | 1.25 (1.03–1.51) |
| Undetermined | 55 (2) | 39 (2) | 1.12 (0.74–1.70) | 1.06 (0.69–1.62) |
| Severe stroke (Unable to walk on admission) | 900 (38) | 475 (25) | 1.79 (1.56–2.04) | 1.60 (1.38–1.86) |
| Documented previous stroke c | 491 (23) | 353 (21) | 1.09 (0.93–1.27) | 1.12 (0.95–1.31) |
| Patient residing in regional area d | 909 (38) | 707 (38) | 1.01 (0.90–1.15) | 0.95 (0.82–1.09) |
Abbreviations: aOR: adjusted odds ratio; CI, confidence interval; OR, odds ratio; TIA, transient ischemic attack.
Bold text indicates significant p < 0.05.
a<1% missing.
b<3% missing.
c11% missing.
dRemoteness area defined as Accessibility and Remoteness Index of Australia (ARIA).
TABLE 2.
Dispatch practices according to suspicion of stroke by emergency dispatchers
|
Suspected stroke/TIA N (%) |
No suspected stroke/TIA N (%) |
Unadjusted OR (95% CI) | |
|---|---|---|---|
| Overall | 2383 (56%) | 1872 (44%) | |
| Ambulance dispatch priority a | |||
| Lights and sirens (within 15 minutes) | 2305 (97) | 1111 (61) | Reference |
| Urgent (within 30 minutes) | 46 (2) | 507 (28) | 0.04 (0.03–0.06) |
| Non‐urgent (within 60 minutes) | 32 (1) | 205 (11) | 0.08 (0.05–0.11) |
| Transport priority b | |||
| Highest priority (time sensitive) | 1289 (55) | 800 (45) | Reference |
| Medium priority (non‐time sensitive) | 1057 (45) | 980 (55) | 0.67 (0.59–0.76) |
Abbreviations: CI, confidence interval; OR, odds ratio; TIA, transient ischemic attack.
Bold text indicates significant p < 0.05.
a<1% missing.
b3% missing.
1.5.2. On‐scene paramedics’ stroke suspicion
Paramedics suspected 2919 (69%) eligible patients in AuSCR as having a stroke. Factors associated with paramedics correctly identifying stroke in the prehospital setting are presented in Table 3. According to the unadjusted analyses those suspected of stroke by paramedics had earlier symptom onset to assessment times compared to those not suspected of stroke (see Table 4).
TABLE 3.
Characteristics of AuSCR confirmed stroke patients and associations with correct paramedic identification of stroke
|
Suspected stroke/TIA N = 2919 N (%) |
No suspected stroke/TIA N = 1336 N (%) |
Unadjusted analyses OR (95% CI) |
Adjusted analyses aOR (95% CI) |
|
|---|---|---|---|---|
| Female | 1203 (41) | 595 (45) | 0.87 (0.77–0.99) | 0.88 (0.76–1.03) |
| Age (in years) | ||||
| Less than 65 | 764 (26) | 398 (30) | Reference | Reference |
| 65–74 | 922 (32) | 428 (32) | 1.12 (0.95–1.33) | 1.11 (0.92–1.34) |
| 75+ | 1233 (42) | 510 (38) | 1.26 (1.07–1.48) | 1.29 (1.07–1.54) |
| Born in Australia | 1816 (62) | 827 (62) | 1.01 (0.89–1.16) | 0.99 (0.84–1.17) |
| Interpreter required a | 184 (6) | 102 (8) | 0.81 (0.63–1.05) | 0.86 (0.64–1.17) |
| Onset of symptoms <4.5 hours b | 1533 (53) | 445 (34) | 2.21 (1.93–2.53) | 2.40 (2.07–2.78) |
| Type of stroke | ||||
| Ischemic | 1891 (66) | 831 (64) | Reference | Reference |
| Intracerebral hemorrhage | 334 (12) | 158 (13) | 0.93 (0.76–1.14) | 0.88 (0.70–1.11) |
| Transient ischemic attack | 571 (20) | 277 (21) | 0.91 (0.77–1.07) | 0.84 (0.69–1.02) |
| Undetermined | 59 (2) | 35 (3) | 0.74 (0.48–1.13) | 0.73 (0.47–1.16) |
| Severe stroke (unable to walk on admission) | 1985 (68) | 895 (67) | 1.04 (0.90–1.19) | 1.07 (0.92–1.26) |
| Documented previous stroke c | 603 (23) | 241 (21) | 1.17 (0.99–1.39) | 1.16 (0.97–1.38) |
| Patient residing in regional area d | 1134 (39) | 482 (36) | 1.12 (0.98–1.28) | 1.16 (0.99–1.36) |
Abbreviations: aOR: adjusted odds ratio; CI, confidence interval; OR, odds ratio; TIA, transient ischemic attack.
Bold text indicates significant p < 0.05.
a<1% missing.
b2% missing.
c11% missing.
dRemoteness area defined as Accessibility and Remoteness Index of Australia (ARIA).
TABLE 4.
Response and hospital transportation time metrices according to correct identification of stroke
| Time metrics | Correctly identified as stroke/TIA | Differencea | p value | |
|---|---|---|---|---|
| Yes | No | |||
| Cases involving emergency dispatchers | N = 2383 | N = 1872 | ||
| Call received to ambulance arriving at scene |
N = 2303 12 (9, 16) |
N = 1764 14 (10, 25) |
‐2.00 (‐2.48 to ‐1.52) |
<0.001 |
| Call received to ambulance getting to patient |
N = 2302 13 (10, 17) |
N = 1763 16 (11, 27) |
‐3.00 (‐3.62 to ‐2.38) |
<0.001 |
| Call receipt to arriving hospital |
N = 2069 55 (44, 72) |
N = 1535 68 (52, 92) |
‐12.40 (‐14.30 to ‐10.51) |
<0.001 |
| Cases involving paramedics | N = 2919 | N = 1336 | ||
| Arrival at scene to loading patient on stretcher |
N = 2805 16 (12, 22) |
N = 1192 19 (13, 25) |
‐3.00 (‐3.83 to ‐2.17) |
<0.001 |
| Loading patient on stretcher to arriving at hospital |
N = 2518 24 (16, 36) |
N = 1041 28 (20, 42) |
‐3.57 (‐4.91 to ‐2.23) |
<0.001 |
| Hospital arrival to off stretcher |
N = 2,514 13 (6, 21) |
N = 1023 15 (7, 25) |
‐2.27 (‐3.29 to ‐1.25) |
<0.001 |
| Hospital arrival to patient clearance |
N = 2542 41 (29, 54) |
N = 1081 31 (26, 55) |
2.00 (0.4 to 3.61) |
0.060 |
| Call receipt to arriving hospital |
N = 2541 56 (45, 76) |
N = 1083 68 (52,92) |
‐11.82 (‐13 to ‐9.75) |
<0.001 |
| Cases involving both EMS dispatchers and paramedics | N = 1947 | N = 2308 | ||
| Arrival at scene to loading patient on stretcher |
N = 1867 15 (11, 20) |
N = 2131 19 (14, 25) |
‐4.00 (‐4.64 to ‐3.36) |
<0.001 |
| Loading patient on stretcher to arriving at hospital |
N = 1680 24 (17, 36) |
N = 1879 26 (18, 40) |
‐1.90 (‐3.15 to ‐0.65) |
<0.001 |
| Hospital arrival to off stretcher |
N = 1678 13 (6, 21) |
N = 1859 14 (6, 24) |
‐1.43 (‐2.34 to ‐0.49) |
0.003 |
| Hospital arrival to patient clearance |
N = 1696 40 (29, 52) |
N = 1927 41 (28, 56) |
‐1.00 (‐2.49 to 0.55) |
0.213 |
| Call receipt to arriving hospital |
N = 1695 54 (43, 72) |
N = 1929 66 (50, 89) |
‐11.56 (‐13.56 to ‐9.56) |
<0.001 |
Abbreviation: TIA, transient ischemic attack.
Data summarized as medians and interquartile ranges (25th percentile, 75th percentile).
aGroup median difference, interquartile range obtained from quantile regression.
The adjusted analysis of factors associated with call‐takers or paramedics correctly identifying patients with stroke are presented in Tables 1 and 3 and were generally consistent with the univariable analyses with the exception of those who were born in Australia and required an interpreter. Compared with patients who were not identified as having a stroke by emergency dispatchers only, those identified as having as stroke had better response times for all the time metrics investigated. However, for cases involving paramedics only, those who were identified as having stroke had better response times for all time metrices except for “hospital arrival to patient clearance.” The results were similar for those identified by both call‐takers and paramedics (Table 4).
Results were slightly different when analyses of differences in response times between cases identified and those not identified to be stroke by emergency dispatchers were stratified according to whether the patient was conscious or not. Among those who were unconscious, arrival at scene to loading patient on stretcher, hospital arrival to patient getting off stretcher, and call receipt to arrival at hospital were significantly faster for patients identified as stroke, compared to those not identified as stroke. In contrast, among those who were unconscious, all time metrics were significantly different with exception of call received to ambulance getting to patient and hospital arrival to patient clearance (Tables S2 and S3). Results were similar when analyses were stratified by ability to walk on admission.
1.5.3. Limitations
Our study has some limitations that need acknowledgment. First, we were unable to determine if the patient's education level, patient's knowledge, and awareness of the signs of stroke were likely to affect their ability to communicate their symptoms to emergency dispatchers or treating paramedics. It is also possible that patients who do recognize their stroke symptoms are likely to choose alternative pathways such as presenting directly to hospital. Authors of a study from Australia have reported that patient with less severe stroke symptoms were more likely to use other means of transport than an ambulance for transport to hospital. 24 Second, not all TIAs that present to hospital are included in AuSCR, participation is voluntary, and full coverage of all stroke cases was not possible, limiting the generalizability of the findings. Third, we used “ability to walk admission” as a proxy for stroke severity instead of the National Institute of Health Stroke Scale (NIHSS). The NIHSS considers patient comorbidities and frailty and, therefore, would have strengthened our findings. 25 Our finding for the transport time should be interpreted with caution as these results may not be generalizable to other settings.
Finally, the “taking an ambulance” variable in the AuSCR may be unreliable. Of the records that were not merged between the AuSCR and ambulance records, we found additional records that indicated arrival by ambulance that should have been in the registry. Conversely, the registry and the emergency data set included patients using an ambulance with no records in the ambulance data set (Figure 1). These data cleaning procedures highlight additional advantages of linked data that enable (1) identification of where improvements to documentation or data collection may be needed, and (2) the ability to verify variables that are common to each data set and update records before analysis.
1.6. Discussion
Our study identifies the factors independently associated with correct identification of stroke in the prehospital setting. Using the MPDS, the sensitivity of emergency dispatchers identifying patients with stroke was just over half. The identification of suspected stroke by the call taking algorithm is an area for further improvement based on this research. Our findings are consistent with evidence from previous studies that found the sensitivity of emergency dispatcher identification of stroke through the use of the MPDS varies between 31% and 66%. 26 , 27 , 28 The current findings also indicate that the MPDS may be suboptimal in identifying patients with stroke especially those with severe symptoms. 29 Further investigation into the reasons for these findings are needed such as whether additional training or refinement of the MPDS card is required.
As anticipated, there was greater sensitivity by paramedics who can physically assess patients. Patients identified with suspected stroke, particularly those with stroke symptom onset within 4.5 hours, arrived sooner at hospital. Those suspected of stroke received higher priority ambulance dispatch and had shorter time metrics such as onset to emergency call, ambulance arrival at scene, and arriving at hospital door. We expected prompt arrival at hospital for those patients with stroke symptom onset within 6 hours as the ambulance dispatch matrix responds more slowly to calls not deemed time sensitive. Our results are consistent with findings from authors of a similar Victorian study, which reported that identification of patients with suspected stroke by paramedics was associated with reduced times from ambulance call to hospital arrival. 30 The effectiveness of acute stroke treatment is time sensitive. The early identification of patients with stroke is likely to increase the proportion of patients eligible for reperfusion treatment. This is important as early recognition of stroke symptoms expedites hyperacute stroke care.
We found females, older patients (75 years and above), those with severe stroke (unable to walk on admission), or those with hemorrhagic stroke were less likely to be identified as having a stroke in the prehospital setting. There are several reasons that may explain the low recognition of patients with severe stroke in the prehospital setting. For instance, patients with more severe stroke may be less likely to answer questions or explain their symptoms to the call‐takers. There is also evidence that patients with stroke who had fallen or collapsed were less likely to be identified as having a stroke. 8 , 31 In prior research from Taiwan, 32 it was found that approximately 50% of calls made to emergency services were made by family members. In addition, female patients have been reported by some authors to experience more severe stroke, yet exhibit atypical stroke symptoms such as altered mental status, altered consciousness, impaired speech, trouble walking, or collapse as common symptoms for stroke at presentation compared to men. 33 , 34 , 35 Our study contributes evidence in support of adoption of severity measures to ensure patients with severe symptoms are not missed in the prehospital setting.
In conclusion, we found that just over half of patients with stroke were accurately detected in the prehospital setting, and those correctly suspected of stroke arrived earlier to hospital. Important patient characteristics were identified that may be used to refine prehospital protocols to identify more patients with stroke and ensure they arrive as soon as possible to hospital. Future research is needed that focusses on interventions that improve the rates of stroke identification in the prehospital setting.
CONFLICTS OF INTEREST
Dominique A. Cadilhac reports educational grants from Boehringer Ingelhiem, Allergan and Medtronic paid to her institution and unrelated to this study. Dominique A. Cadilhac is also the Data Custodian for the Australian Stroke Clinical Registry. Monique F. Kilkenny is a member of the Management Committee for AuSCR and reports an educational grant Allergan paid to her institution and unrelated to this study. The other authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
Amminadab L. Eliakundu was the lead author and was responsible for data analysis and writing of the manuscript. Karen Smith, Monique F. Kilkenny, Joosup Kim, Kathleen L. Bagot, Emily Andrew, Shelley Cox, Christopher F. Bladin, Michael Stephenson, Lauren Pesavento, Lauren Sanders, Ben Clissold, Henry Ma, and Dominique A. Cadilhac contributed to the study design, interpretation of the data, and editing of the manuscript for intellectual content.
Supporting information
Supporting Information
ACKNOWLEDGMENTS
We acknowledge members of the Australian Stroke Clinical Registry (AuSCR) Steering Committee, staff from the Florey Institute of Neuroscience and Mental Health who manage the AuSCR, and the hospital clinicians and patients who contribute data to the AuSCR. We also acknowledge the Data Linkage Units from Victoria, and the Ambulance Victoria Centre for Research and Evaluation who linked and provided access to the data used in this study.
Biography
Amminadab Eliakundu, MClinEpi, is a PhD candidate in the Translational Public Health and Evaluation Division, Department of Medicine, in the School of Clinical Sciences at Monash University in Victoria, Australia. He is an experienced cardiac scientist and researcher with more than 5 years of experience working in the health and research sectors.
Eliakundu AL, Cadilhac DA Dominique.Cadilhac@monash.edu, Kim J, et al. Determining the sensitivity of emergency dispatcher and paramedic diagnosis of stroke: statewide registry linkage study. JACEP Open. 2022;3:e12750. 10.1002/emp2.12750
Supervising Editor: Henry Wang, MD, MS.
REFERENCES
- 1. Australian clinical guidelines for stroke management ‐ chapter 3 of 8: acute medical and surgical management. Stroke Foundation; 2021. [Google Scholar]
- 2. Flynn D, Francis R, Robalino S, et al. A review of enhanced paramedic roles during and after hospital handover of stroke, myocardial infarction and trauma patients. BMC Emerg Med. 2017;17(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mould‐Millman NK, Meese H, Alattas I, et al. Accuracy of prehospital identification of stroke in a large stroke belt municipality. Prehosp Emerg Care. 2018;22(6):734‐742. [DOI] [PubMed] [Google Scholar]
- 4. National Stroke Foundation . National stroke audit: acute services report. Melbourne, Australia; 2017. [Google Scholar]
- 5. Middleton S, Grimley R, Alexandrov AW. Triage, treatment, and transfer: evidence‐based clinical practice recommendations and models of nursing care for the first 72 hours of admission to hospital for acute stroke. Stroke. 2015;46(2):e18‐e25. [DOI] [PubMed] [Google Scholar]
- 6. Ramanujam P, Guluma KZ, Castillo EM, et al. Accuracy of stroke recognition by emergency medical dispatchers and paramedics ‐ San Diego experience. Prehosp Emerg Care. 2008;12(3):307‐313. [DOI] [PubMed] [Google Scholar]
- 7. Jia J, Band R, Abboud ME, et al. Accuracy of emergency medical services dispatcher and crew diagnosis of stroke in clinical practice. Front Neurol. 2017;8(466).1‐5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones SP, Carter B, Ford GA, et al. The identification of acute stroke: an analysis of emergency calls. Int J Stroke. 2013;8(6):408‐412. [DOI] [PubMed] [Google Scholar]
- 9. Geoscience Australia . Area of Australia ‐ states and territories. ACT (Australia). Government of Australia. [cited on 3/2/2020]. Available from: https://www.ga.gov.au/scientific‐topics/national‐location‐information/dimensions/area‐of‐australia‐states‐and‐territories
- 10. Eastwood K, Morgans A, Stoelwinder J, et al. Patient and case characteristics associated with ‘no paramedic treatment’ for low‐acuity cases referred for emergency ambulance dispatch following a secondary telephone triage: a retrospective cohort study. Scand J Trauma Resusc Emerg Med. 2018;26(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Antipova D, Eadie L, Macaden A, et al. Diagnostic accuracy of clinical tools for assessment of acute stroke: a systematic review. BMC Emerg Med. 2019;19(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bray J, Martin J, Cooper G, et al. An Interventional study to improve paramedic diagnosis of stroke. Prehosp Emerg Care. 2005;9(3):297‐302. [DOI] [PubMed] [Google Scholar]
- 13. National Stroke Foundation . Australian clinical guidelines for stroke management ‐ chapter 3 of 8: acute medical and surgical management. Melbourne, Australia; 2017. [Google Scholar]
- 14. Delivering our patients the right care, at the right time, at the right place: revised clinical response model evaluation report. Ambulance Victoria; 2017. [Google Scholar]
- 15. Cadilhac D, Lannin N, Anderson C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5(3):217‐226. [DOI] [PubMed] [Google Scholar]
- 16. Andrew NE, Sundararajan V, Thrift AG, et al. Addressing the challenges of cross‐jurisdictional data linkage between a national clinical quality registry and government‐held health data. Aust N Z J Public Health. 2016;40(5):436‐442. [DOI] [PubMed] [Google Scholar]
- 17. Cox S, Martin R, Somaia P, et al. The development of a data‐matching algorithm to define the ‘case patient’. Aust Health Rev. 2013;37(1):54‐59. [DOI] [PubMed] [Google Scholar]
- 18. Department of Health and Human Services . Victorian Emergency Minimum Dataset (VEMD) user manual. 18th ed. Melbourne (Australia): The Victorian Government. 2013. [Google Scholar]
- 19. Kilkenny M, Kim J, Andrew N, et al. Maximising data value and avoiding data waste: a validation study in stroke research. Med J Aust. 2019;210(1):27‐31. [DOI] [PubMed] [Google Scholar]
- 20. Eliakundu A, Smith K, Kilkenny M, et al. Linking data from the Australian Stroke Clinical Registry with ambulance and emergency administrative data in Victoria. INQUIRY. 2022;59:1‐8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mendelson SJ, Prabhakaran S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: a review. JAMA. 2021;325(11):1088‐1098. [DOI] [PubMed] [Google Scholar]
- 22. Australian Bureau of Statistics. Remoteness classification (ASGS‐RA) Canberra 2019. Available from: https://meteor.aihw.gov.au/content/index.phtml/itemId/697105 [Google Scholar]
- 23. Counsell C, Dennis M, McDowall M, et al. Predicting outcome after acute and subacute stroke: development and validation of new prognostic models. Stroke. 2002;33(4):1041‐1047. [DOI] [PubMed] [Google Scholar]
- 24. Eliakundu AL, Cadilhac DA, Kim J, et al. Factors associated with arrival by ambulance for patients with stroke: a multicentre, national data linkage study. Australas Emerg Care. 2021;24(3):167‐173. [DOI] [PubMed] [Google Scholar]
- 25. Lyden P. Using the national institutes of health stroke scale. Stroke. 2017;48(2):513‐519. [DOI] [PubMed] [Google Scholar]
- 26. Rosamond WD, Evenson KR, Schroeder EB, et al. Calling emergency medical services for acute stroke. Prehosp Emerg Care. 2005;9(1):19‐23. [DOI] [PubMed] [Google Scholar]
- 27. Deakin CD, Alasaad M, King P, et al. Is ambulance telephone triage using advanced medical priority dispatch protocols able to identify patients with acute stroke correctly? Emerg Med J. 2009;26(6):442‐445. [DOI] [PubMed] [Google Scholar]
- 28. Viereck S, Møller TP, Iversen HK, et al. Medical dispatchers recognise substantial amount of acute stroke during emergency calls. Scand J Trauma Resusc Emerg Med. 2016;24:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Buck BH, Starkman S, Eckstein M, et al. Dispatcher recognition of stroke using the national academy medical priority dispatch system. Stroke. 2009;40(6):2027‐2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mosley I, Nicol M, Donnan G, et al. The impact of ambulance practice on acute stroke care. Stroke. 2007;38(10):2765‐2770. [DOI] [PubMed] [Google Scholar]
- 31. Mattila OS, Puolakka T, Ritvonen J, et al. Targets for improving dispatcher identification of acute stroke. Int J Stroke. 2019;14(4):409‐416. [DOI] [PubMed] [Google Scholar]
- 32. Hsieh M‐J, Chien K‐L, Sun J‐T, et al. The effect and associated factors of dispatcher recognition of stroke: a retrospective observational study. J Formos Med Assoc. 2018;117(10):902‐908. [DOI] [PubMed] [Google Scholar]
- 33. Berglund A, Heikkilä K, Bohm K, et al. Factors facilitating or hampering nurses identification of stroke in emergency calls. J Adv Nurs. 2015;71(11):2609‐2621. [DOI] [PubMed] [Google Scholar]
- 34. Bushnell CD, Chaturvedi S, Gage KR, et al. Sex differences in stroke: challenges and opportunities. J Cereb Blood Flow Metab. 2018;38(12):2179‐2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gall SL, Donnan G, Dewey HM, et al. Sex differences in presentation, severity, and management of stroke in a population‐based study. Neurology. 2010;74(12):975‐981. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


