Abstract
Coronavirus disease 2019 was declared a national emergency in the United States on March 13, 2020, at which time the Children’s National Hospital Emergency Department in Washington, DC, mobilized to develop and implement a unit-based Incident Command System. Anticipating that the unique and challenging nature of this pandemic might require a large interprofessional team, emergency nurses, emergency physicians, and emergency physician assistants were placed in traditional Incident Command System roles to provide an organizational framework for the ED response. This framework served multiple purposes but most importantly it helped to efficiently streamline and coordinate communications within the emergency department, with hospital leadership and with other hospital departments. The focus on intentionally taking an interprofessional approach to assigning Incident Command System roles was key to optimize staff safety, patient care, and clinical efficiency. This paper highlights a unique concept of applying the Incident Command System model to a single hospital department in a disaster scenario, using existing ED staff to function in various roles not typically held during regular operations. Given that policies and procedures can be ever-changing during a pandemic, emergency departments can implement an interprofessional incident command structure to provide a framework for communications and operational planning that allows for agility based on evolving priorities. The Children’s National Hospital ED Incident Command System model established during the coronavirus disease 2019 pandemic can serve as a guide for other emergency departments during a disaster response.
Introduction
Coronavirus disease 2019 (COVID-19), the disease caused by the novel coronavirus, was declared a public health emergency by the World Health Organization on January 30, 2020.1 Subsequently, the District of Columbia reported its first case on March 7, 2020,2 and COVID-19 was deemed a US national emergency on March 13, 2020.3 In response to the declared national emergency, the pediatric emergency department at Children’s National Hospital (CNH) in Washington, DC, implemented an interprofessional unit-based ED Incident Command System (ED ICS) that went into effect on March 14, 2020.
Background
CNH is a 319-bed, freestanding, tertiary hospital serving pediatric patients in District of Columbia, Maryland and Virginia, with an annual ED visit volume of approximately 124,000 with 15,000 admissions. Although initial reports indicated the elderly were primarily affected by COVID-19,4 preparations were also made for a potential surge of pediatric ED patients. Within the first 2 months, CNH treated more than 400 patients diagnosed as having COVID-19 in the emergency department, with 25% requiring hospitalization and, of those, 25% requiring critical care.5 Given the highly transmissible nature of severe acute respiratory syndrome coronavirus 2, staff safety, the acquisition of personal protective equipment (PPE), and education of safety protocols were prioritized. Staying up to date on infection control measures and clearly communicating to staff became paramount and a major impetus for the rapid stand-up of a comprehensive incident command structure.
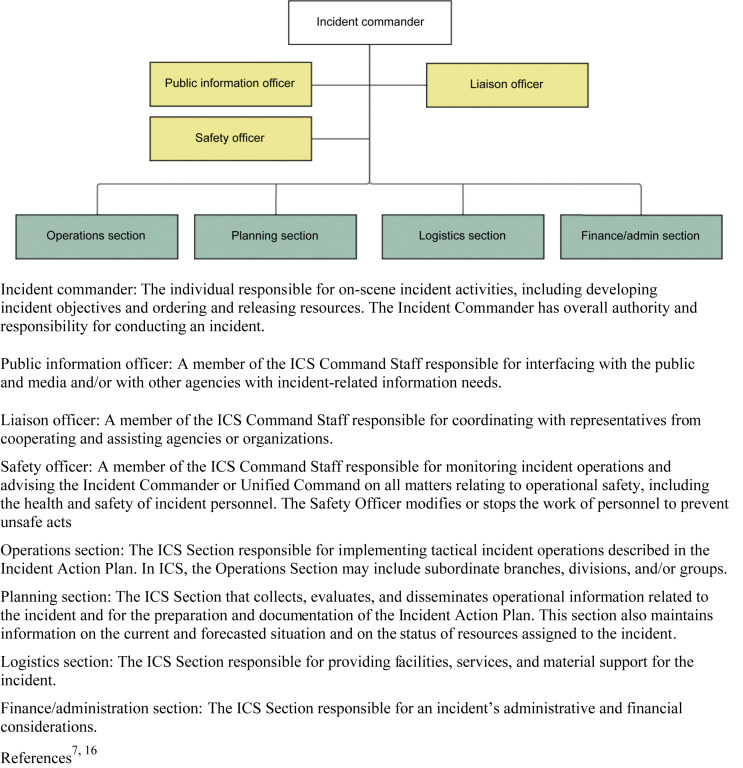
The National Incident Management System was created by the Department of Homeland Security to provide a standardized framework for responding to large-scale incidents.6 The ICS (Figure 1 ) represents a standardized organizational structure often used in emergency management that can be adapted to a variety of situations to reduce redundancy in tasks and allow for a streamlined reporting structure.6, 7, 8, 16 This structure enables effective and efficient incident management by integrating a combination of facilities, equipment, personnel, procedures, and communications operating within a common organizational framework.7 The ICS has 5 major management functions: command, operations, logistics, planning, and finance.8 , 9
Figure 1.
Standard incident command structure. ICS, Incident Command System. (Reproduced with permission from NIMS: frequently asked questions. U.S. Department of Homeland Security. Accessed October 11, 2021. https://www.fema.gov/pdf/emergency/nims/nimsfaqs.pdf; and Glossary of related terms ICs review. Intermediate Incident Command System for Expanding Incidents. Published March 2018. Accessed October 11, 2021. https://training.fema.gov/emiweb/is/icsresource/assets/glossary%20of%20related%20terms.pdf)16
Methods
Incident Command in the Emergency Department
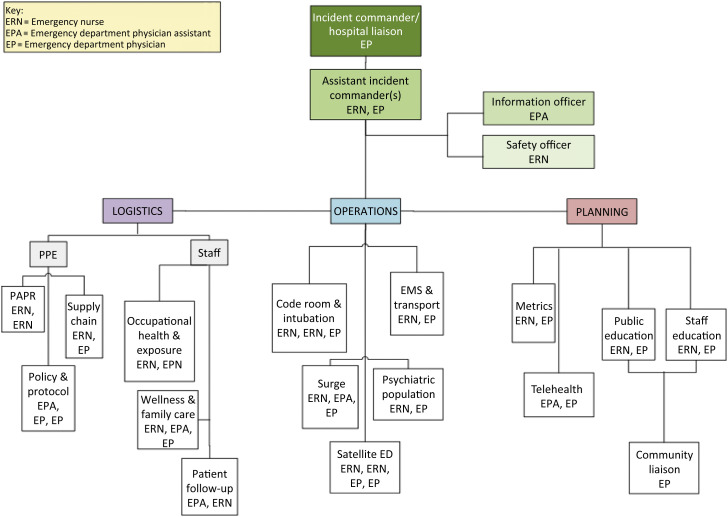
The COVID-19 Incident Command in this pediatric emergency department (Figure 2 ) included an interprofessional team of emergency nurses, emergency physicians, and emergency physician assistants. Multiple groups from the ED ICS worked closely with hospital leadership, infection control, language services, registration, and other hospital departments and stakeholders to develop and lead implementation of policies and plans in the emergency department.
Figure 2.
Children’s National Hospital unit–based interprofessional incident command system. ERN, emergency nurse; EPA, emergency physician assistant; EP, emergency physician.
Command Section
The ED incident commander (IC) reported directly to the hospital COVID-19 ICS. The ED leadership decided to establish an ICS independently, given the frontline status of the emergency department and the need to make rapid decisions as the situation evolved. The finance function of the ED ICS was led by the ED IC. Relevant finance duties/management included tracking staff hours toward COVID-19-specific duties and any supply expenditures. This information was shared with the finance section of the hospital COVID-19 ICS. The ED IC also attended the hospital COVID-19 ICS meetings and was the ED spokesperson to represent at essential city and state forums that were involved in the community-wide response. Two assistant incident commander (AIC) roles were created to focus on the emergency department–specific issues, one an emergency physician leader and one an emergency nurse leader, who worked in tandem throughout the response.
An emergency physician assistant was assigned the information officer role. In this role, they managed a designated COVID-19 email account and helped streamline communications to the department. The IC team also worked closely with a designated safety officer, who was an emergency nurse with extensive ICS training. The safety officer’s primary role was to oversee PPE-related concerns. The fundamental ICS concept that every individual has only one designated supervisor, known as “unity of command,” was strictly adhered to, improving the flow of information, helping with the coordination of operational efforts, and enhancing operational safety.10
Operations Section
The operations section was responsible for all day-to-day activities related to COVID-19 in the emergency department. The surge unit focused on creating a surge plan to increase the capacity for ED patient assessments and management should a large influx of patients overwhelm current capacity.
The psych unit worked with psychiatric services to manage mental health patients by helping to develop testing protocols and guidance for psychiatry admission protocols.
The code room/intubation unit worked in conjunction with the PPE branch, infection control, and the critical care department to develop policies and procedures to keep staff protected during high-risk procedures such as intubations, critical care resuscitations, and aerosolizing procedures.
The patient follow-up unit developed and maintained a system to address the large number of COVID-19 test results that required follow-up in a timely manner. Although test follow-up is an already established process in the emergency department (eg, culture results), the sheer number of COVID tests requiring follow-up necessitated a team to develop a new process to manage the increased workload.11 The education unit prepared COVID-19-specific discharge instructions for families using guidelines from the Centers for Disease Control and Prevention, led staff educational updates, and maintained revisions on informational signage throughout the unit.
The emergency medical services/transport unit worked with prehospital partners and the interfacility transport team to ensure consistency of practice and standardization of protocols for transferring patients from the field or an outside facility. This required extensive coordination among the regional EMS systems, various regional EMS providers, and the interhospital transport team.
Planning Section
The planning section addressed internal and external planning, rapidly creating new teams as the need arose. For example, a telehealth unit was established to improve ED telehealth capabilities focused on virtual patient follow-ups and enhanced caregiver communication via virtual platforms. The community/primary care unit worked with the local referring provider community to inform them of ED policies, facilitate referrals, and communicate follow-up processes.
Logistics Section
The logistics section had 2 primary roles: PPE and staffing. In this pandemic, the rapid standup of the PPE branch was imperative and was overseen by the safety officer. The PPE branch ensured adequate supply of PPE and worked closely with infection control to develop PPE protocols for emergency department–specific, high-risk clinical situations such as caring for patients undergoing an aerosol generating procedure.
The staff branch worked closely with the hospital occupational health department to manage reports of exposures and persons requiring quarantine, oversee changes to the clinical schedules, and address the unique stressors posed by the pandemic. This included connecting staff with mental health resources and facilitating staff connections for childcare. The staff branch also organized regular wellness activities, including virtual happy hours, and managed the distribution of donated food to staff on shift.
Communication Model
Effective communication in any disaster is paramount.12 The COVID-19 pandemic provided a unique challenge, given the vast number of unknowns about the disease, the evolving nature of the level of outbreak, and shifting priorities and recommendations from public health and government officials. Correcting misinformation and being transparent about what was unknown, especially early on, were key features of our communications strategy.
For decades, the American Heart Association and American Academy of Pediatrics have provided guidance on interprofessional communication during a crisis, via certification courses such as Pediatric Advanced Life Support (PALS). Although PALS scenarios are often exercised during smallscale resuscitation events, the same key team dynamic principles were used daily to navigate the COVID-19 pandemic in the emergency department. Closed-loop communication, clear messaging, clear roles, knowing one’s limitations, knowledge sharing, constructive intervention, reevaluation and summarizing, and mutual respect were all familiar practices for ED staff to rely upon and apply during this COVID-19 response.13 Role confusion is another phenomenon identified as uniquely prevalent during crises that is proven alleviated by checklist or job aid amidst an emergency event.14 The clear hierarchy inherent to ICS application not only establishes a who’s-who contact list but also minimizes redundancy by delineating responsibilities at the command, group, and individual levels. Concise definition of roles should be shared with all staff for accountability with top priorities for each role reassessed frequently among ICS team members.
Communication within the ED ICS was shared via a single email distribution list for all members of the ED ICS and a text group for urgent issues. Initially, the ED ICS met daily on video-conference calls run by the AICs. The frequency of these meetings decreased as groups became more self-sustaining, global needs reduced, and the influx of new information to guide policies and practice became more consistent.
It was important that communication to the ED staff was frequent, concise, easily digestible, and readily available. To accomplish this, an email titled “5@5” was used daily to reach the ED staff. At 5 pm each day, the AICs summarized 5 key points regarding the COVID-19 response. This email became a popular and widely used source of information well beyond the ED recipients and at its height included nearly 600 people from multiple departments and executives throughout the hospital. Topics ranged from urgent notifications to inspirational messaging, important process changes, lessons learned, latest science, ED trends in data, free resources available to health care workers, and light-hearted quotes.
To provide a forum for questions, a separate dedicated email account through which staff could send COVID-19-related queries was developed and managed by the information officer. Multiple department-wide virtual town halls were also conducted, which allowed staff to ask the ED ICS team leaders questions directly, engage in real-time discussions, and unwind and socialize with their peers.
Implications for Emergency Nurses
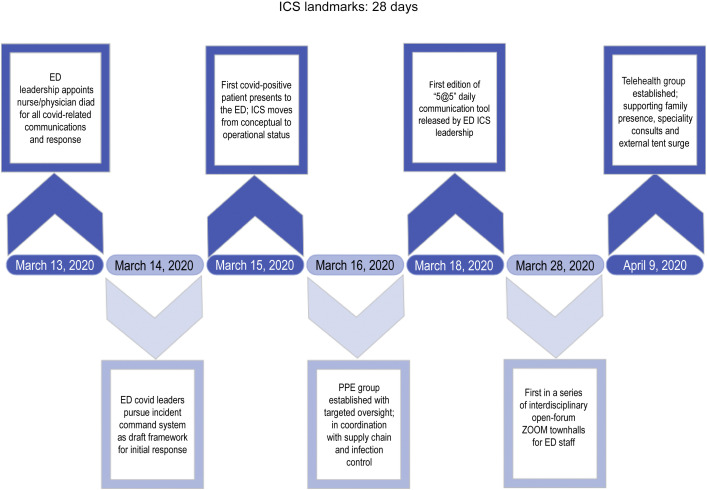
Establishing an interprofessional ICS structure for a disaster such as the COVID-19 pandemic is an efficient and effective way to organize a department-level response, particularly in lieu of the restrictions placed on being able to meet in person and the switch to prioritizing virtual forms of communication during the pandemic. This article describes a unit-based ICS framework implemented during COVID-19 to efficiently streamline and coordinate interdisciplinary communications within the emergency department and with other hospital departments. The ICS was established quickly, with major elements functional within 28 days (Figure 3). The disruption of routine staff meeting schedules and urgency for nimble operational changes to keep up with the evolving hospital and public health guidelines for managing the pandemic culminated in a need for the emergency department to have a leadership framework similar to the hospital and public health department framework. Goals were to optimize staff safety, patient care, and clinical efficiency. Although not formally measured, success with this unit-based framework was determined by positive feedback from staff, low workplace infection rates, reduced redundancy of tasks at the leadership level, and a notable decrease in individual questions and queries from staff as regular communications increased. This unit-based framework for crisis communications and operational planning using established ICS roles can serve as a guide for other emergency departments during a disaster response.
Figure 3.
CNH ED COVID-19 ICS timeline. CNH, Children’s National Hospital; COVID-19, coronavirus disease 2019; ICS, Incident Command System; PPE, personal protective equipment.
Key take-home points are as follows:
-
•
Create an interprofessional approach to ICS leadership (emergency nurses, emergency physicians, emergency physician assistants) that allows for buy-in and perspectives that represent the needs of various disciplines in the emergency department.
-
•
Regularly engage key relevant hospital departments and hospital leadership (eg, infection control, intensive care units, laboratory, medicine).
-
•
Identify liaisons to hospital committees and departments to facilitate bidirectional and streamlined communication.
-
•
Implement relevant ICS units as key issues emerge and retire groups as their goals are met.
-
•
Establish regular meetings with all ICS members and modify the frequency of meetings as the situation evolves.
-
•
Encourage a formal team-dynamics framework, such as that given by the American Heart Association PALS programming, for a template of established, interprofessional communication tools.
-
•
Streamline department-wide communications to convey important, timely, and accurate messaging to aid in information management and mitigate misinformation.
-
•
Create a streamlined system for bidirectional communication between staff and ICS leadership.
Conclusion
COVID-19 has affected every facet of life, both professionally and personally. Establishing an emergency department–focused ICS leadership structure with emergency nurses, emergency physicians, and emergency physician assistants in the early stages of the pandemic was key to success. Although there are other examples of ICS structures during COVID-19,15 this is the first we are aware of in the published literature to specifically highlight the use of an interprofessional unit-level team and not one composed entirely of physicians.13 Although this experience is based on a pediatric emergency department, this framework has broad applicability to any ED setting.
As the COVID-19 pandemic continues to evolve across the US, success in this emergency department’s response was attributed to implementing leadership strategies rooted in an emergency preparedness framework. This experience demonstrates that the ICS structure can serve as a model for leadership in an ED disaster response and the importance of including all disciplines of the clinical team.
Author Disclosures
Conflicts of interest: none to report.
Biographies
Timothy Holtzclaw is Professional Practice Specialist, Emergency Medicine and Trauma Center, Children’s National Hospital, Washington, DC. Twitter:@holtzclaw_tim.
Shaina Derstine Newman is Pediatric Emergency Physician Assistant, Emergency Medicine and Trauma Center, Children’s National Hospital, Washington, DC. ORCID identifier: https://orcid.org/0000-0001-8831-8627.
Matthew Dwyer is Emergency Nurse, Emergency Medicine and Trauma Center, Children’s National Hospital, Washington, DC.
Joelle Simpson is Chief of Emergency Medicine, Emergency Medicine and Trauma Center and Medical Director for Emergency Preparedness, Children's National Hospital, Washington, DC. Associate Professor of Pediatrics & Emergency Medicine, George Washington University School of Medicine & Health Sciences. Twitter:@DrJoSimps. ORCID identifier: https://orcid.org/0000-0003-0629-7995.
Tress Goodwin is Assistant Medical Director for Emergency Preparedness, Emergency Medicine and Trauma Center, Children's National Hospital, Washington, DC. Assistant Professor of Pediatrics & Emergency Medicine, George Washington University School of Medicine & Health Sciences. ORCID identifier: https://orcid.org/0000-0003-0291-2452.
Footnotes
Section Editor: Patricia Kunz Howard, PhD, RN, CEN, CPEN, TCREN, NE-BC, FAEN, FAAN
Send submissions to Patricia Kunz Howard, PhD, RN, CEN, CPEN, TCREN, NE-BC, FAEN, FAAN at: PKHoward@uky.edu.
References
- 1.World Health Organization (WHO). Novel coronavirus (2019-nCoV) situation report-11. Published January 31, 2020. Accessed May 12, 2021. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4s
- 2.Graf H. Father Tim Cole at Christ Church Georgetown, D.C.'s first COVID-19 case, shares his story. ABC7 News. WJLA. Published March 20, 2020. Accessed May 12, 2021. http://wjla.com/news/local/reverend-at-christ-church-georgetown-dcs-first-covid-19-case-shares-his-story
- 3.The Associated Press. ‘Two very big words’: Trump announces national emergency for coronavirus. The New York Times. March 13, 2020. Accessed October 15, 2020. https://www.nytimes.com/video/us/politics/100000007032704/trump-coronavirus-lives
- 4.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeBiasi R.L., Song X., Delaney M., et al. Severe COVID-19 in children and young adults in the Washington, DC metropolitan region. J Pediatr. 2020;223:199–203.e1. doi: 10.1016/j.jpeds.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Incident Management System. What is NIMS? Accessed October 11, 2021. https://www.nh.gov/safety/divisions/hsem/documents/NIMSQA1305.pdf
- 7.U.S. Department of Homeland Security. NIMS: frequently asked questions. Accessed October 11, 2021. https://www.fema.gov/pdf/emergency/nims/nimsfaqs.pdf
- 8.FEMA Emergency Management Institute. ICS review document. Intermediate incident command system for expanding Incidents. Published March 2018. Accessed October 11, 2021. https://training.fema.gov/emiweb/is/icsresource/assets/ics%20review%20document.pdf
- 9.Deal T. Incident command system overview. In: Deal T, Huyck V, Merrick G, Mills C, De Bettencourt M, eds. Beyond Initial Response: Using the National Incident Management System’s Incident Command System. Bloomington; 2010:1-30.
- 10.United States Department of Homeland Security . National Incident Management System. 3rd ed. FEMA; 2017. pp. 25–27. [Google Scholar]
- 11.Newman S., Simpson J., Perritt A., et al. COVID-19 result follow-up process in the pediatric emergency department setting. Disaster Med Public Health Prep. 2020:1–5. doi: 10.1017/dmp.2020.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waring S., Alison L., Carter G., et al. Information sharing in interteam responses to disaster. J Occup Organ Psychol. 2018;91(3):591–619. doi: 10.1111/joop.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Heart Association. Team Dynamics Debriefing Tool, 2020. Published 2020. Accessed February 2, 2022. https://ahainstructornetwork.americanheart.org/AHAECC/Courses/PALS-2020/UCM_506752_2020-Guidelines-PALS-Instructor-Resources.jsp?_requestid=561671
- 14.Renna T.D., Crooks S., Pigford A.-A., et al. Cognitive Aids for Role Definition (CARD) to improve interprofessional team crisis resource management: an exploratory study. J Interprof Care. 2016;30(5):582–590. doi: 10.1080/13561820.2016.1179271. [DOI] [PubMed] [Google Scholar]
- 15.Farcas A., Ko J., Chan J., Malik S., Nono L., Chiampas G. Use of incident command system for disaster preparedness: a model for an emergency department COVID-19 response. Disaster Med Public Health Prep. 2021;15(3):e31–e36. doi: 10.1017/dmp.2020.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Intermediate Incident Command System For Expanding Incidents. Glossary of related terms. Published March 2018. Accessed October 11, 2021. https://training.fema.gov/emiweb/is/icsresource/assets/glossary%20of%20related%20terms.pdfs