Abstract
Background
Machete cut fracture is a unique subset of open fracture. The sharp force of a wielded machete that cleanly divides soft tissue envelope with minimal or no contusion results in an open fracture wound that is relatively less prone to infection. However, in resource-limited settings, the wound infection rate after machete cut fracture is relatively high. This study aimed to determine the risk factors for wound infection after extremity machete cut fractures in a Nigerian setting.
Methods
We undertook a retrospective analysis of the patients who were seen in the Emergency room of two tertiary hospitals in Nigeria with a machete cut extremity fracture from 2009 to 2018. The association of wound infection with population and wound characteristics as well as intervention related factors were evaluated. Statistical significant factors for wound infection in the Univariable analysis were entered into a Multivariable regression analysis to evaluate the risk of each factor when adjusted to other factors.
Results
There were 113 machete-cut fractured bones in 67 eligible patients and wound infection was a complication in 45 (39.8%) of the cases (95%CI 30.3 – 49.7%).The factors significantly associated with high wound infection rate were smoking, haematocrit < 30%, fractures sustained outdoors, lower extremity fractures, a wound size of >5cm in length, injury-to-hospital arrival interval > 6hrs. Multivariable regression analysis identified wound size >5 cm (aOR 14.142, 95%CI (2.716 - 73.636); p = 0.002), injury-to- hospital arrival interval later than 6hrs (aOR 4.410, 95% CI (1.003-19.394); p = 0.050) and administration of antibiotics later than 3hrs of injury (aOR 5.736, 95%CI (aOR1.362 - 24.151; p = 0.017) as independent risk factors for wound infection.
Conclusion
Wound infection after open fractures caused by machetecut is more likely to occur in patients that present later than six hours after injury, wounds more than 5cm in length and delayed antibiotic administration. Appropriate treatment protocols can be instituted with this knowledge.
Keywords: Machete cut, open fracture, wound infection, risk factor
African relevance
• Machete is a common farming tool, game hunting as well as a weapon of assault and self -defence in Africa. Intentional and accidental machete injury is common, and 16- 20% of the cases are associated with an open fracture.
• Wound infection compounds the burden of fracture caused by machete cut and its rate is relatively high in resource-limited setting.
• This study has identified the risk factors for wound infection after machete-cut fractures and the findings can facilitate preventive strategies and tailored interventions in the African setting.
Introduction
Machete is a common domestic and farm tool as well as a weapon of assault in African sub- regions. Machete injury either intentional or accidental is common among the general population in resource-limited settings [1]. An open fracture is a component of morbidity associated with machete injuries; it accounts for 16-20% of machete injuries in the civilian trauma setting in resource-limited countries [1,2]. Recently published reports indicate machete cut fracture accounted for 9% of open extremity fractures in a Nigerian-setting and 69% of machete-related upper extremity injuries requiring in-patient admission in a Level one trauma centre in the USA [3,4]. Machete-cut fracture, like open fractures from other mechanisms of injury, is prone to wound contamination and infectious complications that can results in short and long term morbidity and mortality [5,6]. Thus, wound infection prevention is one of the goals in the management of fractures caused by machete cuts.
Overall, the wound infection rate after open fracture varies from 7 to 63% [[7], [8], [9], [10], [11]]. Previous studies have shown that there are environmental, host and injury-related predisposing factors for the infectious complications after open fractures [6,7,12]. Also, there is a positive correlation between wound infection rate and higher Gustilo Anderson grade of open fractures [7]. However, the mechanism of injury in over 98% of fractures in these previous studies involved blunt force trauma (road traffic injuries, falls, sports injury etc) and firearm injury [[8], [9], [10],12]. The injury mechanism in machete cut fracture is quite different from those caused by blunt trauma and firearm, where soft tissue crushing and devitalisation often occur [6,8,14]. The sharp force trauma of a wielded machete that cleanly divides soft tissue envelope resulting in open wounds of varying sizes with very minimal or no contusion is a unique feature of these fractures [13]. A recently published report indicates that wound infection rate after open extremity injury correlates positively with the severity of soft tissue crushing and devitalisation [15]. It implies that a relatively low wound infection rate is more likely from the guillotine type of injury associated with machete cut fractures. Non-evidence of wound infection in a case series of machete cut fractures reported by Rymaszewski et al. in Glasgow, Scotland, is consistent with a low rate of wound infection expected in this type of fracture [13]. However, a recently published report indicates that the prevalence of wound infection after machete cut fractures was 34% in a resource-limited setting [16]. Also, Serra et al in Caribbean reported a wound infection rate of 14.4% in a case series of forearm fractures caused by machete cut [5]. It suggests that there may be factors that come to play in the relatively high rate of wound infection after machete cut fractures in resource-limited settings.
The unique feature of machete cut fracture underscores the importance of detailed knowledge about the predisposing factors for wound infection as it can facilitate preventive strategies and tailored intervention to ensure optimum care. However, there is dearth of data on wound infection and its predisposing factors after machete cut fractures. The relatively high incidence of machete cut fracture wound infection in resource-limited settings and the paucity of data necessitated this study. Thus, this study aimed to determine the risk factors for wound infection after extremity fractures caused by machete cut in the Nigerian setting.
Methods
This study was conducted in two tertiary Hospitals, Alex Ekwueme Federal University Teaching Hospital Abakaliki and National Orthopaedic Hospital Enugu, in South East Nigeria. The former is one of the teaching hospitals in Nigeria and the latter one of the three regional Orthopaedic and trauma centres in Nigeria. This was a hospital-based retrospective analysis of the patients with machete cut fractures who presented in the Emergency room over a period of 10 years (1st January 2009 to 31st December 2018).
All patients of all age groups with machete cut fractures involving any of the bones in the extremities including the bones of the pectoral and pelvic girdles that were treated, discharged and followed up for 3months or had wound infection before self-discharge against advice or death were included. The following cases of machete-cut fractures were excluded from this analysis: patients with a machete cut fracture involving bones of the axial skeleton(skull, spine thoracic cage etc.), patients brought in dead, dead on arrival or in less than 72 hours of injury and there was no documented evidence of wound infection. Patients that left the hospital against medical advice with no evidence of wound infection at the time of self-discharge were also excluded.
All the cases of machete cut fractures seen in the hospitals within the period were identified from the hospital admission database and the patients’ journals retrieved. Relevant information on population characteristics, type of fracture and size of the open wound, aetiology, season and location of the injury in addition to intervention-related factors and outcome were obtained from the patient journal.
For statistical analysis, the cases of machete cut fractures were classified into five age groups (0-17, 18-39, 40-65 and >65years), male and female, single and married and the presence or absence of co- morbid factors such as HIV infection, Diabetes Mellitus and immunosuppressive therapy. The cases of machete cut fractures were further classified as shown in Table 1. The fractures were also classified by morphological type into incomplete, transverse, oblique and communited fractures. For analysis, the cases were grouped into three based on definitive fracture care / immobilization: Conservative care (application of cast and other external splints), external fixation (application of external fixators or percutaneous Kirschner wire fixation) and internal fixation (using plate and screws, intramedullary nails, cerclage or Kirschner wires). The cases were also classified into three groups based on the type wound closure (primary closure, delayed primary closure, and secondary closure). Pre hospital care in this study was defined as care (at the scene, en route, home, primary health facility, patent medicine store) given to the patient before presentation to the trauma centres.
Table 1.
Probable risk factors and classification of cases of machete-cut fractures for statistical analysis
| Probable risk factors | Basis of grouping | Group 1 | Group 2 |
|---|---|---|---|
| Smoking | History of cigarette smoking | Yes | No |
| Alcohol | History of alcohol consumption | Yes | No |
| Haematocrit | Haematocrit within 24hours of hospital admission | <30% | ≥30% |
| Location | Geographical location of injury | Rural | Urban |
| Scene of injury | Indoor /outdoor injury | Outdoor | Indoor |
| Season | Relative humidity at time of injury | Dry | Wet |
| Anatomical region | The extremity involved | Upper | Lower |
| Pre-hospital care | Care prior to presentation | Yes | No |
| Injury- antibiotic interval | Injury –administration of antibiotics interval | ≤ 3hrs | >3hrs |
| Injury –hospital interval | Injury to hospital admission interval | ≤ 6hrs | > 6hrs |
| Wound size | Length of the open wound | ≤5cm | >5cm |
| Aetiology | Aetiological factors | Intentional | Accidental |
Wound infection was defined as documented evidence of purulent discharge, cellulitis or positive wound culture within three months of injury. Based on this outcome, patients were classified into two based on the absence (no) and presence (yes) of wound infection after machete cut fracture.
A serial coordinated multidisciplinary team approach involving emergency physicians, surgeons (orthopaedic, plastic and reconstructive and vascular surgeons), anaesthetists, radiologists, nurses, physiotherapist and others as the case demanded was the modality of care in all the patients. Patients presenting to the hospitals with extremity fractures caused by machete cut were admitted in the Emergency unit for resuscitation. Empirical parenteral antibiotics (Ceftriaxone and Metronidazole) and tetanus toxoid were administered within thirty minutes of arrival to the hospital. Antibiotics were adjusted as necessary based on the result of wound culture and antibiogram. Patients underwent a wound assessment ± judicious debridement then wound irrigation with adequate amounts of normal saline. Apparently clean wound presenting within six hours of injury were closed primarily. The wound presenting later than 6hours or apparently contaminated was left open and inspected after 48 hours; thereafter it was either closed or dressed daily in the surgical ward with normal saline and povidone iodine until it was clean and good enough for delayed primary closure / secondary closure or split skin grafting. The method of definitive immobilization of fractures was dependent on multiple factors that included type of bone involved, the type and grade of open fracture and associated soft tissue injury. Plaster of Paris (POP)/ Scotch cast were used for incomplete fractures, undisplaced fractures and after manipulation of some stable displaced fracture. Other conservative modes of immobilization were collar and cuff and broad arm sling. Emergency / primary external fixation and percutaneous Kirschner wire fixation were applied when indicated. All the internal fixation of fractures with plate and screws, intramedullary nails, and cerclage wires were delayed until there was neither clinical nor microbiological evidence of wound contamination or infection.
Data analysis was carried out using Statistical Package for Social sciences SPSS version 20 (SPSS Inc; Chicago, Illinois., USA). The population, wound and fracture characteristics as well as intervention-related factors were cross tabulated against wound infection. Then Univariable analysis was carried out and p value set at ≤0.05. The significant factors that emerged from the Univariable analysis were entered into a step wise logistic regression model for multivariable analysis to evaluate the risk of each factor when adjusted to other factors. In the multivariable analysis, statistical significance was set at p value ≤0.05.
The Research Ethics Committee of the hospitals approved the study and also waived the need for written informed consent for this retrospective analysis of anonymised patient data.
Results
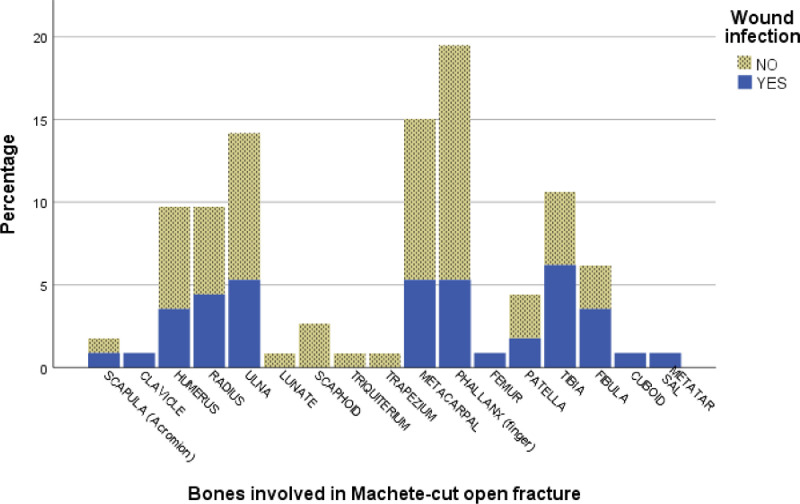
Within the period under review, 73 patients presented with machete cut fractures, 67 of them with 113 bones involved in the fracture met the inclusion criteria for this study; hence in the analysis some of the data refers to machete cut extremity fractures in 113 cases. Of these 67 patients, 22, 9, 1 and 1 of them had fractures in 2, 3, 4 and 6 bones respectively. The three top bones involved were finger phalanx, metacarpal and ulna as shown in Fig. 1. Wound infection was a complication in 45 of these 113 cases of machete cut fracture, giving a wound infection rate of 39.8% (95% Confidence Interval 30.3- 49.7%).
Fig. 1.
Distribution of machete-cut fractures by type of bone and wound infection
The wound infection rates by the Population, Location, Aetiology, Injury variables and the intervention- related variables in the analysis are as shown in Tables 2 and 3.
Table 2.
Wound infection by the Population, Location, Aetiology and Injury Variables
| Variables Age | Wound infection NO (%) | Wound infection YES (%) | Total (%) |
|---|---|---|---|
| 0-17 | 6(66.7) | 3(33.3) | 9(8.0) |
| 18-39 | 49(57.6) | 36(42.4) | 85(75.2) |
| 40-65 | 9(75.0) | 3(25.0) | 12(10.6) |
| >65 | 4(57.1) | 3(42.9) | 7(6.2) |
| Sex | |||
| Male | 56(57.1) | 42(42.9) | 98(86.7) |
| Female | 12(80.0) | 3(20.0) | 15(13.3) |
| Alcohol | |||
| No | 37(62.7) | 22(37.3) | 59(52.2) |
| Yes | 31(57.4) | 23(42.6) | 54(47.8) |
| Smoking | |||
| No | 56(65.9) | 29(34.1) | 85(75.2) |
| Yes | 12(42.9) | 16(57.1) | 28(24.8) |
| Haematocrit | |||
| ≥30% | 46(70.8) | 19(29.2) | 64(57.5) |
| <30% | 22(45.9) | 26(54.1) | 48(42.5) |
| Aetiology | |||
| Intentional | 66(61.1) | 42(38.9) | 108(95.6) |
| Accidental | 2(40.0) | 3(60.0) | 5(4.4) |
| Season | |||
| Dry | 37(59.7) | 25(40.3) | 62(54.9) |
| Wet | 31(60.8) | 20(39.2) | 51(45.1) |
| Locality | |||
| Urban area | 37(63.8) | 21(36.2) | 58(51.3) |
| Rural area | 31(56.4) | 24(43.6) | 55(48.7) |
| Scene of injury | |||
| Indoor | 14(93.3) | 1(6.7) | 15(13.3) |
| Outdoor | 54(55.1) | 44(44.9) | 98(86.7) |
| Anatomical region | |||
| Upper extremity | 58(66.7) | 29(33.3) | 87(77.0) |
| Lower extremity | 10(38.5) | 16(61.5) | 26(23.0) |
| Type of fracture | |||
| Incomplete fractures | 6(54.5) | 5(45.5) | 11(9.7) |
| Transverse | 38(66.7) | 19(33.3) | 57(50.4) |
| Oblique | 20(57.1) | 15(42.9) | 35(31.0) |
| Comminuted | 4((40.0) | 6(60.0) | 10(8.8) |
| Wound size(cm) | |||
| ≤5 | 33(84.6) | 6(15.4) | 39(34.5) |
| >5 | 35(47.3) | 39(52.7) | 74(65.5) |
Table 3.
Wound infection by Intervention related variables
| Variables | Wound infection NO (%) | Wound infection YES (%) | Total (%) |
|---|---|---|---|
| Pre-hospital care | |||
| No | 42(58.3) | 30(41.7) | 72(63.7) |
| Yes | 26(63.4) | 15(36.6) | 41(36.6) |
| Injury -hospital interval (hr) | |||
| 0-6 | 58(79.5) | 15(20.5) | 73(64.6) |
| >6 | 10(25.0) | 30(75.0) | 40(35.4) |
| Injury -antibiotics interval (hr) | |||
| ≤ 3 | 30(90.9) | 3(9.1) | 33(29.2) |
| ≥ 3 | 38(47.5) | 42 (52.5) | 80(70.8) |
| Wound Care | |||
| Primary closure | 28(80.0) | 7(20.0) | 35(31.0) |
| Delayed primary closure | 39(55.7) | 31(44.2) | 70(61.9) |
| Secondary closure | 1(12.5) | 7(87.5) | 8(7.1) |
| Definitive fracture care | |||
| Conservatives (cast, splints) | 28(57.1) | 21(42.9) | 49(43.4) |
| External fixation | 28(58.3) | 20(41.7) | 48(42.5) |
| Internal fixation | 12(75.0) | 4(25.0) | 16(14.2) |
In Table 2, wound infection rate was respectively higher among smokers and patient that presented with Haematocrit of <30% on admission compared to non-smokers and those with Haematocrit >30%. The incidence of wound infection triples when the wound size is >5cm in length; it doubles in the lower extremity wounds compared to the upper extremity ones. There was none with HIV infection, diabetes mellitus or immunosuppressive therapy as co-morbidity. In Table 3, the wound infection rate triples among patient that arrived hospital >6hr after injury.
In the Univariable analysis, cigarette smoking, Haematocrit <30% on admission, scene of injury (outdoor), wound size >5cm in length, injury- to –hospital arrival interval >6hrs and antibiotic administration >3hrs after injury were identified as factors associated with high rate of wound infection after extremity fracture caused by machete cut as shown in Table 4.
Table 4.
Univariable and Multivariable predictors of wound infection after machete cut extremity fracture
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | p Value | AOR(95% CI) | p Value |
| Age | 0.69 | |||
| 18-39 | 1.469 (.344 – 6.271) | 0.603 | ||
| 40-65 | .667 (.099 - 4.478) | 0.677 | ||
| >65 | 1.500 (.195 – 11.536) | 0.697 | ||
| Sex | 3.000 (.796 – 11.308) | 0.105 | ||
| Alcohol | .801 (.377 – 1.704) | 0.565 | ||
| Smoking | 2.575 (1.076 – 6.161) | 0.034 | 2.746 (.586 – 13.044) | 0.199 |
| Haematocrit | .349 (.160 - .762) | 0.008 | .649 (.191 – 2.208) | 0.489 |
| Aetiology | .424 (0.068-2.646) | 0.359 | ||
| Season | .955 (.448 – 2.036) | 0.905 | ||
| Locality | 1.364 (.641 – 2.904) | 0.421 | ||
| Scene of injury | .088 (.011 - .693) | 0.021 | 4.477 (.286 – 70.30) | 0.286 |
| Anatomical region | 3.200 (1.292 – 7.927) | 0.012 | 1.903 (.447 – 8.099) | 0.384 |
| Type of fracture | 0.373 | |||
| Transverse | 1.209 (.522 – 2.797) | 0.658 | ||
| Oblique | 3.102 (.816 – 11.789) | 0.096 | ||
| Comminuted | .591 (.058 – 6.029) | 0.657 | ||
| Wound size (cm) | 6.129 (2.295 – 16.367) | 0.001 | 14.142 (2.716 – 73.630) | 0.002 |
| Pre hospital care | .808 (.367 - 1.779) | 0.596 | ||
| Injury – hospital interval | 11.600 (4,653 – 28.920) | 0.001 | 4.410 (1.003-19.394) | 0.05 |
| Injury – antibiotics interval | 17.630 (5.645 - 55.063) | 0.001 | 5.736 (1.362 – 24.151) | 0.017 |
| Wound care | 0.005 | |||
| Delayed primary closure | .036 (.004 - .340) | 0.004 | 4.086 (.885 – 18.860) | 0.071 |
| Secondary closure | .114 (.013 - .973) | 0.047 | 4.531 (.277 – 74.072) | 0.289 |
| Definitive fracture care | 0.435 | |||
| External fixation | .444 (.125 -1.575) | 0.209 | ||
| Internal fixation | .952 (.452 – 2.132) | 0.906 |
OR= Odd Ratio; CI = Confidence Interval; AOR= Adjusted Odd Ratio
The result of Multivariable regression analysis to determine the risk of each factor when adjusted to other factors was also summarized as shown in Table 4. In the analysis, wound size >5cm in length (aOR 14.142, 95%CI (2.716 - 73.636); p< 0.002), injury- to-hospital arrival interval (aOR 4.410, 95% CI (1.003-19.394); p = 0.050) and injury-to -antibiotic administration interval >3hrs injury (aOR 5.736, 95%CI (aOR1.362 - 24.151; p< 0.017) were identified as independent risk factors for wound infection.
Machete cut fractures with an open wound size of >5cm were 14.142 times more likely to be complicated by infection than the ones with wound size ≤5cm in length. The odds of wound infection was respectively 4.4 and 5.7 in the fractures with injury-to-hospital arrival interval >6hrs and antibiotics administration later the 3hours of injury compared to the reference category. The multivariable logistic regression model was found to be an appropriate model (Chi square 66.047; degree of freedom =9; p value <0.001) and Hosmer Lemeshow goodness of fit test (p =.760) revealed no significant departure from a good fit.
Discussion
The prevalence of wound infection in this study is similar to the overall wound infection rate after machete cut fractures in a recently published report from a resource-limited setting [16]. However, it is quite different from the non-evidence of wound infection found in a series of eight patients with extremity fractures caused by machete cuts reported by Raymszwseski et.al in Glasgow [13]. The exact reason for the difference is not evident. However, the population size in this study is eight times larger than the size of the case series reported; a sample size of only eight cases is relatively small and accounts for the difference in wound infection rates.
The injury-to-hospital arrival interval is potentially related to the timeliness of emergency trauma care such as resuscitation, appropriate wound care and other interventions to prevent infectious complications of open extremity injuries such as tetanus toxoid and antibiotics administration [15]. The result of this study indicates that the initial basic intervention when administered within the first six hours of machete cut fracture is important in limiting wound infection. Robson et al. demonstrated that the bacteria in acute traumatic wound take an average of 5.17hrs to reach a critical number (>105) per gram of tissue, which is the threshold for wound infection [17]. Hence, initial wound care within six hours of open injury to forestall wound infectious complications is widely accepted as the best practice. Thus, an injury-to- hospital arrival interval >6hrs identified as an independent risk factor for wound infection after machete cut extremity fracture is not surprising. In a resource-limited setting, injury to hospital arrival interval later than 6hours is common among victims of machete cut fractures [16]. Therefore, measures aimed at improving the rate of early presentation of patients with machete-cut fractures to a hospital with a capacity for prompt and adequate care is important and should be one of the top priorities in wound infection preventive strategies in this setting.
In this study, a significantly higher wound infection rate observed in cases where antibiotics treatment was initiated later than 3hours compared to within 3hours from the time of injury is similar to the finding reported by Patzakis et al for open fracture wounds [7]. However, Patzakis et al also noted that the role of early antibiotic in the prevention of open fracture wound infection is limited in highly contaminated and devitalized tissues [7]. It implies that early antibiotic is more important in limiting infection in wounds with minimal or no devitalized tissues as in open machete cut fracture wounds. Therefore, administration of antibiotics later than 3 hours identified in this study as an independent risk factor for wound infection after machete cut extremity fracture confirms the report of Patzakis et al on the role of early antibiotics in the prevention of infection in open fracture wound with minimal devitalized tissues. Thus, initiation of empirical antibiotic treatment as early as within the first three hours of injury is an important step towards preventing wound infection after machete-cut fractures.
Published studies have shown that there is an association between the wound size and the incidence of infectious complication in open extremity injuries [[17], [18], [19], [20]]. In this study, there is a positive correlation between wound size and infection rate, and the wound size identified as an independent risk factor for wound infection confirms the findings in these previous reports. In open fractures where wound contamination is more often than not the norm, this implies, the larger the size of the machete wound the greater the surface area for potential contaminants and the risk of wound infection
Besides these three independent predictors of wound infection in machete cut open fractures, the other important and significantly associated factors that are modifiable need to be highlighted. Castillo et al demonstrated that current and previous smokers compared to non-smokers are significantly at a higher risk of wound infection after open fractures [21]. Furthermore, a recent systematic review indicates smokers are at increased risk of infectious complications after open extremity fractures [22]. In this study, the positive association between smoking and a high wound infection rate is in keeping with the finding in these previous reports. Thus, counselling and advising patients against smoking should be considered in machete wound infection preventive measures. Haemorrhage resulting in varying amounts of acute blood loss is a common complication of machete injury [1]. Haematocrit of < 30% that is significantly associated with high wound infection rate in this study suggests that the control of haemorrhage as well as judicious replacement of blood loss and correction of anaemia are also important measures in reducing wound infection rate after machete cut fractures.
As a hospital based study, the data may not represent the entire population of machete cut extremity fractures. Despite this limitation, the findings in this study are important and can facilitate prevention and treatment strategies to contain wound infection after these fractures.
Conclusion
Wound infection after open fractures caused by machete-cut is more likely to occur in patients that present later than six hours after injury, wounds that are more than 5cm in length and delayed antibiotic administration. Appropriate treatment protocols can be instituted with this knowledge.
Dissemination of results
The results of this study were shared with staff members after the collection and analysis of data in an informal presentation.
Authors’ contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: NIO contributed 50%, MCC contributed 8%, FNA contributed 8%, CGN, AAA, PIA, ANE, and OAL each contributed 6.8%. All authors approved the version to be published and agreed to be accountable for all aspects of the work
Declaration of Competing Interest
The authors declare no conflict of interest
References
- 1.Omoke NI, Madubueze CC. Machete injuries as seen in a Nigerian Teaching hospital. Injury. 2010;41(1):120–124. doi: 10.1016/j.injury.2009.08.023. https://doi.org/10.1016/j.injury.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Jones JK, Kommu SA. Survey of cutlass (Collins) injuries seen in the emergency department of the Queen Elizabeth hospital in Barbados. West Indian Med J. 2002;51(3):157–159. [PubMed] [Google Scholar]
- 3.Omoke NI, Ekumankama FO. Incidence and pattern of extremity fractures seen in accident and emergency department of a Nigerian teaching hospital. Nig J Surg. 2020;26:28–39. doi: 10.4103/njs.NJS_42_19. https://www.nigerianjsurg.com/text.asp?2020/26/1/28/277968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donnally CJ, III, W Hannay, DA Rapp, N Lekic, SD Dodds. Machete injuries to the upper extremity. Arch Orthop Trauma Surgery. 2017;137:1615–1621. doi: 10.1007/s00402-017-2783-y. DOI: 10.1007/s00402-017-2783-y. [DOI] [PubMed] [Google Scholar]
- 5.Serra C, Cousin A, Delattre O. Orthopaedic proceedings. 2008. Forearm fractures caused by machete wounds. [cited 2020 May 10]; 90-B SUPP_II, 283-283. Available from https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.90BSUPP_II.0900283a. [Google Scholar]
- 6.Kim PH, Leopold SS. Gustilo-Anderson classification. Clin Orthop Relat Res. 2012;470:3270–3274. doi: 10.1007/s11999-012-2376-6. doi: 10.1007/s11999-012-2376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989;243:36–40. [PubMed] [Google Scholar]
- 8.Ibeanusi SEB, Obalum DC. Open fractures treated in a regional trauma centre in nigeria: presentation and outcome - a prospective observational study. Int Arch Orthop Surg 2019. 2019;2(1):007. doi.org/10.23937/iaos-2017/1710007. [Google Scholar]
- 9.Spencer J, Smith A, Woods D. The effect of time delay on infection in open long-bone fractures: a 5-year prospective audit from a district general hospital. Ann R Coll Surg Engl. 2004;86(2):108–112. doi: 10.1308/003588404322827491. Doi: 10.1308/003588404322827491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odatuwa-Omagbaemi DO. Open fractures: epidemiological pattern, initial management and challenges in a sub-urban teaching hospital in Nigeria. Pan Afri Med J. 2019;33:234. doi: 10.11604/pamj.2019.33.234.18141. doi:10.11604/pamj.2019.33.234.18141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chezian SV, Achar TS. Prevalence of infections among compound fractures in orthopaedic ward of a tertiary health care hospital in South India. Int J Sci Res. 2019;8(6):21–23. Doi:10.36106/ijsr. [Google Scholar]
- 12.Matos MA, Lima LG, de Oliveira LA A. Predisposing factors for early infection in patients with open fractures and proposal for a risk score. J Orthop Traumatol. 2015;16:195–201. doi: 10.1007/s10195-015-0345-z. https://doi.org/10.1007/s10195-015-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rymaszewski JM, Caullay JM. Bony lacerations caused by Assault. J Bone Joint Surg. Br. 1984;66(1):89–92. doi: 10.1302/0301-620X.66B1.6693485. Doi: 10.1302/0301-620X.66B1.6693485. [DOI] [PubMed] [Google Scholar]
- 14.Tosti R, Rehman S. Surgical management principles of gunshot-related fractures. Orthop Clin North Am. 2013;44(4):529–540. doi: 10.1016/j.ocl.2013.06.006. Doi: 10.1016/j.ocl.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Omoke NI, Nwigwe CG. An analysis of risk factors associated with traumatic extremity amputation stump wound infection in a Nigerian setting. Int Orthop. 2012;11(36):2327–2332. doi: 10.1007/s00264-012-1641-3. https://doi.org/10.1007/s00264-012-1641-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Omoke NI, Lasebikan OA, Ahaotu FN., et al. Analysis of machete cut fractures in Nigerian civilian trauma setting. Sci Rep. 2021;11:76. doi: 10.1038/s41598-020-79981-w. https://doi.org/10.1038/s41598-020-79981-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robson MC, Duke WF, Krizek TJ. Rapid bacterial screening in the treatment of civilian wounds. J Surg Res. 1973;14(5):426–430. doi: 10.1016/0022-4804(73)90049-8. Doi: 10.1016/0022-4804(73)90049-8. [DOI] [PubMed] [Google Scholar]
- 18.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453–458. [PubMed] [Google Scholar]
- 19.Hollander JE, Singer AJ, Valentine SM, Shofer FS. Risk factors for infection in patients with traumatic lacerations. Acad Emerg Med. 2001;8(7):716–720. doi: 10.1111/j.1553-2712.2001.tb00190.x. Doi: 10.1111/j.1553-2712.2001.tb00190.x. [DOI] [PubMed] [Google Scholar]
- 20.Quinn JV, Polevoi SK, Kohn MA. Traumatic lacerations: what are the risks for infection and has the ‘golden period’ of laceration care disappeared. Emerg Med J. 2014;31:96–100. doi: 10.1136/emermed-2012-202143. Doi: 10.1136/emermed-2012-202143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castillo RC, Bosse MJ, Mackenzie EJ, Brendan Patterson BM. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fracture. J. Orthop Trauma. 2005;19(3):151–157. doi: 10.1097/00005131-200503000-00001. Doi: 10.1097/00005131-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Kortram K, Bezstarosti H, Metsemakers W, Raschke M J, Van Lieshout EM, Verhofstad M HJ. Risk factors for infectious complications after open fractures; a systematic review and meta-analysis International Orthopaedics (SICOT) 41, 1965–1982 (2017) [cited 2020 May10]. Available from https://doi.org/10.1007/s00264-017-3556-5 [DOI] [PubMed]