Abstract
This case report describes a patient with acute appendicitis presenting with Cullen's sign and Grey Turner sign. This case highlights the importance of the recognition of Cullen's sign and Grey Turner sign in patients with acute appendicitis to prevent life‐threatening complications such as perforation and sepsis.
![]()
Keywords: appendicitis, Cullen's sign, Grey Turner sign
A 65‐year‐old Japanese man had presented himself to the outpatient clinic with 1‐day history of progressively worsened right flank pain. He also complained of anorexia and nausea. He had no previous history of traumatic injury and had never received anticoagulant therapy; he only occasionally drank alcohol. On physical examination, his blood pressure was 150/119 mmHg, his heart rate was 109 beats per minute, his respiratory rate was 16 breaths per minute, and his body temperature was 37.3°C. Notable examination findings included severe tenderness in his right flank with muscle guarding and ecchymoses in the right flank (Grey Turner sign) and periumbilical regions (Cullen's sign; Figure 1). Laboratory findings showed an elevated white blood cell level (14.1 × 109/L), a normal red blood cell level (5.5 × 1012/L), and a normal platelet count (19.4 × 109/L). The blood urea nitrogen level was 22.1 mg/dl (normal: 8.0–22.0 mg/dl), the serum calcium level was 9.2 mg/dl (normal: 8.4–10.2 mg/dl), the lactate dehydrogenase level was 164 U/ml (normal: 120–145 U/ml), the serum lipase level was 8 U/ml (normal: 11–59 U/ml), the serum amylase level was 35 U/ml (normal: 35–125 U/ml), the prothrombin time was 12.5%, and the serum C‐reactive protein level was 18.2 mg/dl (normal: ≤0.14 mg/dl). Urinalysis was unremarkable. Contrast‐enhanced computed tomography showed no enlargement of the pancreas or a common bile duct stone, but revealed an enlarged appendix with a diameter of 10 mm and a wall thickening of 2 mm, the tip of which was in contact with the parietal peritoneum (Figure S1). These findings were consistent with acute appendicitis. Additionally, a slight thickening of the parietal peritoneum, which was suggestive of inflammation, was observed. After initiation of antimicrobial therapy, laparoscopic appendectomy was performed because the patient was deemed to be at high risk of perforation and sepsis. During the procedure, the severely inflamed appendix adhered to the right anterolateral parietal peritoneum was found (Figure 2). The patient had excellent postoperative course without complications, and the ecchymotic regions gradually disappeared.
FIGURE 1.
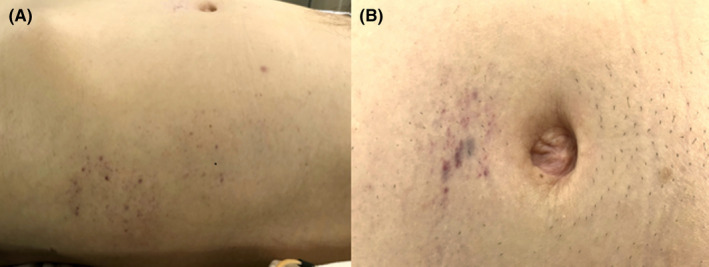
Physical examination showed ecchymoses (A) in the right flank (Grey Turner sign) and (B) around the periumbilical region (Cullen's sign)
FIGURE 2.
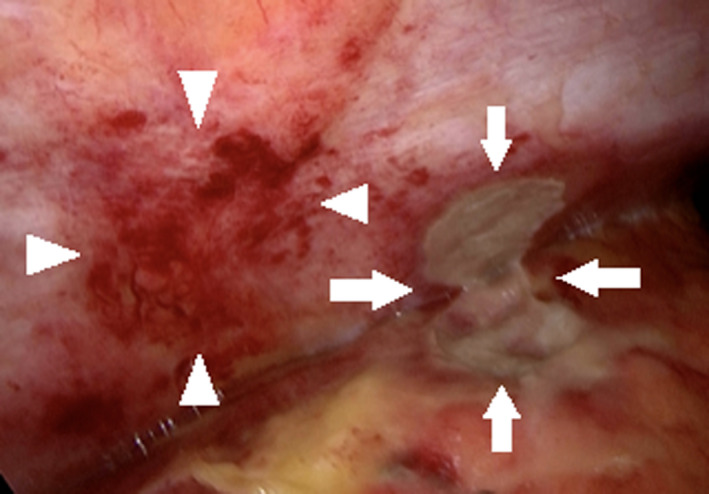
Laparoscopy showed that the severely inflamed appendix (white arrows) adhered to the right anterior parietal peritoneum. The hemorrhage of the anterolateral parietal peritoneum was observed (white arrowheads)
Cullen's sign and Grey Turner sign are ecchymoses of the periumbilical region and the flank and are classically observed in patients with acute pancreatitis, suggesting the presence of pancreatic necrosis. 1 Cullen's sign is produced when retroperitoneal bleeding diffuses into the falciform ligament and the subcutaneous umbilical tissues through the connective tissue of the round ligament complex, whereas, Grey Turner sign is observed when the hemorrhagic fluid diffuses into the quadratus lumborum muscle and the surrounding subcutaneous tissues via a defect in the transversalis fascia. 2 Although a previous study reported several causes of Cullen's sign, 3 to our knowledge, this was the first reported case of Cullen's and Grey Turner signs in a patient with acute appendicitis. In this case, the appendicitis may cause inflammation to the anterolateral parietal peritoneum and the falciform ligament, resulting in the hemorrhage of subcutaneous tissues around the umbilical and flank regions.
The key message obtained from this particular case is that physicians should also consider for the evaluation of acute appendicitis for those patients diagnosed with abdominal pain accompanied by periumbilical and flank ecchymoses because such symptoms may indicate the progression of inflammation to the surrounding peritoneum and connective tissues, leading to the life‐threatening complications such as perforation and sepsis. 4
CONFLICT OF INTERESTS
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
INFORMED CONSENT
We obtained informed consent for publication from the patient.
Supporting information
Figure S1
Acknowledgments
None.
Kashiwagi R, Shimamura Y, Imamura K. Uncommon etiology of Cullen's sign and Grey Turner sign. J Gen Fam Med. 2022;23:282–283. 10.1002/jgf2.533
REFERENCES
- 1. Dickson AP, Imrie CW. The incidence of body wall ecchymosis in acute pancreatitis. Surg Gynecol Obstet. 1984;159(4):343–7. [PubMed] [Google Scholar]
- 2. Bem J, Bradley EL. Subcutaneous manifestations of severe acute pancreatitis. Pancreas. 1998;16(4):551–5. [DOI] [PubMed] [Google Scholar]
- 3. Rahbour G, Ullah MR, Yassin N, Thomas GP. Cullen's sign ‐ case report with a review of the literature. Int J Surg Case Rep. 2012;3(5):143–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. United Kingdom National Surgical Research Collaborative , Bhangu A. Safety of short, in‐hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta‐analysis. Ann Surg 2014;245(5):894. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1


