Abstract
Background
Early studies during the COVID-19 pandemic identify the dissonance between feeling anxious about contracting the illness and the innate desire to serve the sick, as a main stressor for students.
Purpose
The purpose of this study is to better understand psychological stress and self-reported wellness of Physician Assistant (PA), Physical Therapy (PT), dental, and medical students during the early portions of the COVID-19 pandemic.
Methods
We utilized the 10-item Perceived Stress Scale (PSS) together with additional questions to assess self-perceived stress, anxiety, and wellness of healthcare students.
Discussion
There were no significant differences in PSS between professions. As PSS increased (indicating more stress), the odds of answering “worse” versus “same” or “better” to descriptions of anxiety level increased (OR: 2.318).
Conclusion
Student survey respondents experienced similar levels of perceived stress throughout the COVID-19 pandemic. Institutions should consider students’ perceived levels of stress and the many aspects of student wellness that may have been affected by the COVID-19 pandemic.
Keywords: Interdisciplinary, Wellness, Stress, COVID-19 pandemic, Health professions students
1. Introduction
The SARS-CoV-2 virus was first identified on January 9, 2020, as a “novel coronavirus” in Wuhan, China.1 The virus spread quickly, with 750,890 cases globally by March 31, 2020.2 The COVID-19 pandemic brought many challenges to the medical community as it progressed, some of which were resolved quickly, and others that required innovative and unprecedented solutions. One effect of the pandemic that quickly emerged was the tremendous amount of psychological stress and pressure placed on healthcare professionals around the world. Many front-line workers were spending long hours in grueling conditions caring for those with COVID-19, often caring for them in their final moments. Other health care providers who were not on the front lines had different stressors, such as using telemedicine to manage patients remotely, determining the safest way to continue seeing patients in clinic, propelling public health initiatives in their own communities, determining the best steps forward alongside their peers and ever-changing guidelines concerning the SARS-CoV-2 virus and its transmissibility, among many others. While these challenges affected providers around the globe, another unique subset of the medical community faced their own stressors, namely health professions students. Students in all disciplines of healthcare experienced change and uncertainty during the pandemic.
At the University of Nebraska Medical Center, a multidisciplinary academic healthcare institution, many students were transitioned to remote learning by April 1, 2020, roughly one month after the SARS-CoV-2 virus was identified in the United States. For some this meant being pulled from clinical rotations, for others it was a transition to course delivery via Zoom and remote testing. Some students feared the possibility of alterations to their graduation timelines or faced new concerns about employment opportunities post-graduation. For all, it was a disruption in their expected educational process. Prior studies have investigated the impact of pandemics or other disruptive circumstances on the well-being of students in the healthcare professions.3, 4, 5 However, limited research has been done to evaluate the anxiety and stress levels of students across different health care disciplines amidst a stressful event, such as the COVID-19 pandemic.
The purpose of this study is to better understand psychological stress and self-reported wellness of Physician Assistant (PA), Physical Therapy (PT), dental, and medical students during the early portions of COVID-19 pandemic. To this end, our research questions were:
-
1)
Using the Perceived Stress Scale (PSS), how stressed were healthcare students at the beginning of COVID-19? Were there any associated differences in PSS between the students, based on gender, educational program, or year in program?
-
2)
Is there a correlation between a student's perceived anxiety and PSS?
-
3)
What areas of a student's wellness were most negatively affected by the COVID-19 outbreak? Were there any associated differences between the students based on gender, educational program, or year in program?
2. Materials and methods
We surveyed PA, PT, dental, and medical students during the beginning of the COVID-19 pandemic to better understand their self-reported wellness. The survey consisted of 21 fixed-response questions (Supplemental Material 1). The first section consisted of questions related to demographics, including college of study, year in school, and gender. The remaining sections aimed to investigate student's stress, anxiety, and wellness during the COVID-19 pandemic. The Cohen's 10-item Perceived Stress Scale (PSS) was used to evaluate students' self-perceived stress.6 The PSS is a 10-question questionnaire that has been extensively validated to measure the perception of stress of an individual. Several forms of this questionnaire exist; for our study, the 10-question version was utilized.6 Additionally, we asked students about their anxiety and wellness using Likert-type items, some of which were based on the Eight Dimensions of Wellness.7 While we used the Eight Dimensions of Wellness as a guide, it should be noted that because students were self-assessing their own wellness, which can be different for everyone and potentially multifactorial, they were instructed to select all of the wellness categories that had been negatively affected by COVID-19. Further, if their definition of wellness was not included in the list, they were able to select “other” and utilize the text box for their definition. We have adopted the definitions of stress and anxiety from the American Psychological Association, which indicates there are small but relevant differences between them. Stress is an emotion response that is caused by an external trigger. These triggers can be long or short-term and can cause mental and physical symptoms. Anxiety is persistent, excessive worries that do not go away in the absence of a stressor and can lead to physical and mental symptoms similar to stress.8
To develop these questions, we started with a review of the literature regarding the COVID-19 pandemic, in addition to literature related to measuring anxiety/stress of students. Face validity of the survey was established via review by experts in clinical psychology, sociology, psychiatry, biostatistics, education, and the student research team members in each cohort. We piloted the survey with students from each of the health professions programs and edited using an iterative process to improve clarity and reliability. In the end, the PSS met most of our needs, so that is the predominant component of this survey.
A total of 1078 students were recruited via email by members of the student research team in their respective health profession cohorts to participate in the study. Each student team member sent out one reminder to their cohort. Data were collected and managed using REDCap (Research Electronic Data Capture) at UNMC. REDCap is a secure, web-based application designed to support data capture for research studies. The research study and survey were IRB (Institutional Review Board) exempt (IRB #331-20-EX).
The survey was distributed between May 15th and May 29th, 2020. Students were not required to complete all questions in the survey and could leave questions blank. Preliminary data were de-identified by a single investigator. Upon initial review of the data, we noted that the demographic questions related to race, ethnicity, marital status, and parent education, if included, could potentially lead to identification of the respondent. Therefore, we did not include these in our findings/analyses in order to maintain anonymity. De-identified data were analyzed by an expert biostatistician, using descriptive statistics, ANOVA, and logistic regression. The statistical analyses included fixed effects ANOVA models, which consisted of a combination of between-subject factors, including group (program of study), year in program nested within group, and gender. Main effects and interactions were evaluated with type III tests of significance. Differences in pairs of means were adjusted for multiple comparisons with the Tukey procedure when three or more means were present. Proportions of items selected, the result of summing responses from a fixed number of dichotomous items, were evaluated with logistic regression models. The proportional odds logistic regression model was applied with responses having three ordinal levels (re-coded from a five-point Likert scale). All statistical significance tests were two-sided. Tables of counts were made with the TABULATE procedure, and graphical displays were produced with the SGPLOT procedure from SAS/BASE software. Statistical analyses were generated with the GLIMMIX procedure from SAS/STAT software, Version 9.4 (© 2002–2012) of the SAS System for Windows (Cary, NC).
3. Results
In total, 357 UNMC students responded to the survey. A total of 62 responses were excluded due to incomplete data (less than 50% of the survey completed), resulting in a 33.12% response rate. Respondent breakdown by area of study included: 102 medical students, 59 dental students, 54 PT students, 81 PA students. The survey respondents included 92 males, 202 females, and 1 other/prefer not to answer. A complete set of demographic data can be seen in Table 1 .
Table 1.
Demographic data from survey respondents.
| Medical | Dental | Physician Assistant | Physical Therapy | |
|---|---|---|---|---|
| 1st year | 26 | 20 | 33 | 20 |
| 2 nd year | 16 | 21 | 47 | 10 |
| 3rd year | 17 | 13 | 20 | |
| 4th year | 37 | 5 | ||
| TOTAL | 96 | 59 | 80 | 50 |
| Male | 43 | 21 | 14 | 14 |
| Female | 58 | 37 | 67 | 40 |
| TOTALa | 101 | 58 | 81 | 54 |
Differing totals were observed due to incomplete survey responses.
Our first research questions were: Using the PSS, how stressed were healthcare students at the beginning of COVID-19? Were there any associated differences in PSS between the students, based on gender, educational program, or year in program?
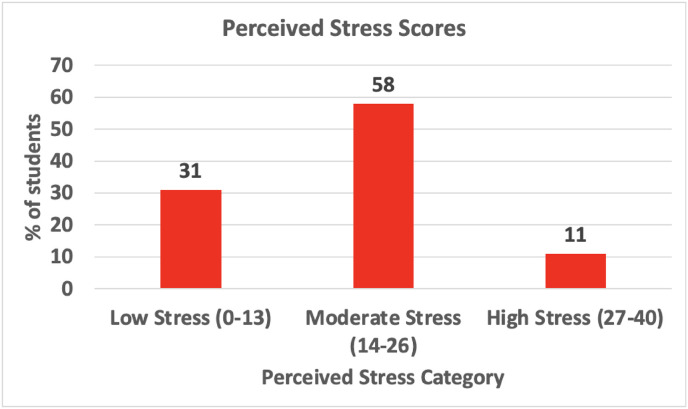
Fig. 1 shows the PSS for all students. Most students fell in the “moderate stress” category (58.0%). Further, there were no statistically significant differences amongst PSS of any of the four programs (Averages: medical = 14.71, dental = 16.84, PA = 18.07, PT = 16.11). No significant difference existed between PSS of males and females (14.51 vs 17.91, respectively). Results comparing years within each program showed no differences except for the PA program. PA students in pre-clinical stages (Year 1) of the program had significantly higher PSS than their counterparts in clinical stages (Year 2) of the program (20.39 vs 15.76, p = .007). Supplemental material 2 shows the distribution of answer responses to the PSS for all students.
Fig. 1.
Perceived stress score for all students based on the 3 categories within Cohen's Perceived Stress Scale (PSS).6 Numerals in () indicate total score ranges on the PSS.
Our second research question was: Is there a correlation between a student's perceived anxiety and PSS?
For all groups, increases in PSS increased the probability of responding “worse” or “much worse” to questions about changes in anxiety level since the start of the COVID-19 pandemic (p < .0001, OR-2.318). The relationship between PSS and probability of anxiety can be seen in Fig. 2 . Among the health professions programs, PA students had a lower probability of responding “worse” or “much worse” than students in the other three programs and a higher probability of responding “better” (Fig. 2).
Fig. 2.
Anxiety level compared to Cohen's Perceived Stress Scale (PSS). Anxiety levels were assessed as changes in anxiety from pre-pandemic to during the pandemic and were categorized as being “better,” “the same,” or “worse.” Comparisons are provided for all health professions students (COM= College of Medicine or medical students, PA = physician assistant students, PT = physical therapy students). The data for medical and dental students were combined because the groups followed virtually the same patterns. PT also very nearly followed the same pattern as medical and dental students.
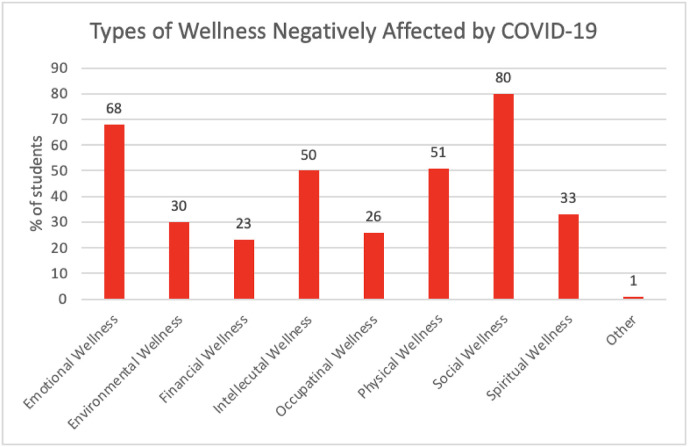
Our third research questions were: What areas of a student's wellness were most negatively affected by the COVID-19 outbreak? Were there any associated differences between the students based on gender, educational program, or year in program?
Students were asked to select all the areas of wellness that they perceived as being negatively affected by COVID-19 (Fig. 3 ). Overwhelmingly, social wellness (80.34%) and emotional wellness (68.5%) were the most frequently chosen among the entire student population. While the least likely to be chosen was financial wellness (23.0%) and occupational wellness (25.8%). Different student groups within the student population had higher proportions of selecting different types of wellness affected. For example, PT students had a lower probability of selecting intellectual wellness compared to medical students (estimate 1.154 (p = .012) and PA students (estimate 1.142 (p = .017). Dental students had a higher probability of selecting occupational wellness compared to PT students (estimate 1.377 (p = .041).
Fig. 3.
Type of wellness negatively affected by COVID-19 for all students.
4. Discussion
After surveying students from multiple programs there was no statistically significant PSS differences between health education programs (dental, medical, PA and PT) and the majority of students reported moderate levels of stress. As students’ PSS increased, the perception of anxiety also increased. Likewise, all UNMC health programs shared similar wellness impacts. Emotional and social wellness were selected as the most negatively impacted form of student wellness across all UNMC students at 68.47% and 80.34% respectively.
Previous studies have shown that the prevalence of anxiety amongst U.S. medical students has risen from 20.3% to 31.1% during the COVID-19 pandemic.9 The findings of this study follow similar trends regarding stress and anxiety of all students surveyed. As for stress analysis, the majority (58%) of UNMC health programs students' fell into the moderate stress category with no significant differences between groups. Does this mean that COVID-19 has affected each field of health equally? That is unlikely; however, this parallel response could be due to all education programs bearing the UNMC badge. Though it is reasonable to assume each program's COVID-19 experiences differed, each was subject to the same UNMC governing body that directed the COVID response.
Previous research indicates stress and anxiety correlate. We saw that these conditions were directly related with perceptions of both stress and anxiety increasing in professional students during the COVID-19 pandemic. The neural overlap between these two has been explained via intermingled emotion circuits.10 Anxiety can often be brought upon by emotions related to the fear of the unknown. Amidst the COVID-19 pandemic, there are many unknowns, similar to previously studied infectious disease outbreaks. A SARS outbreak in Hong Kong, showed that stress induced by the perceived risk of contracting the illness led to anxiety related to fear of the unknown.3 Along with fear of the unknown, healthcare students faced increased anxiety from educational requirements, and clinical duties.11 More work would need to be done to better understand this trend, but one possible area for investigation could be that the length of the program, educational differences, or curriculum organization that each unique program possess is contributing to anxiety levels. To better understand the impact of the COVID-19 pandemic on student anxiety, a standardized measure in the form of the 7-point Generalized Anxiety Disorder Scale could be used along with specifically surveying educational topics.
We did note a significant difference between PSS in pre-clinical vs clinical PA student groups, with the former being significantly higher (20.39 vs 15.76, p = .007). The difference in PSS score between pre-clinical PA students and clinical PA students could have been related to course load/content and the transition that occurred related to in person/online learning. Pre-clinical PA students had a heavy course load, which remained the same when they transitioned from in-person to online learning. Furthermore, it was designed for in-person learning, which could increase stress when course expectations were maintained with only online learning.
Contrastingly, for clinical PA students, when the transition from in-person to online learning occurred, these students were pulled from their rotation sites and enrolled in one online course, which included coursework designed for remote learning and only met once weekly. This was a lighter workload for these students who had previously been spending 40 h a week learning at their clinical sites.
A theme across all programs was that emotional and social wellness were most negatively affected by the COVID-19 pandemic. In all, 192 students noted that their emotional wellness and 227 noted that their social wellness was negatively impacted. Nebraska, like many other states, declared a public lock down prohibiting social gathering in an attempt to stop the spread of COVID.12 The lock down had a significant impact on these areas of wellness. Day-to-day routines were drastically changed. The lives of students participating in clinical education no longer included patient contact and classmate community. With the inability to participate in “normal” social environments for extended periods of time, the negative social and emotional wellness impact is not surprising.
These findings suggest the necessity of institutions and students alike, to recognize and mitigate health professions students' anxiety, stress, and the impact on wellness that a pandemic may cause. This could aid institutions in implementing an effective response and support plan for their students during pandemics and other like situations. Further analysis of the COVID-19 pandemic's impact on health professions students is warranted.
There are several limitations to our study. All students were from a single University. The survey was limited to one point in time with no long-term data. Also, the PSS was the only officially validated, standardized measure used. In the future it would be interesting to conduct this study as students matriculate back to more “traditional” (in our case, in-person) learning, to better understand if these stress and anxiety levels were heightened specifically during the pandemic, or if these levels are persistent among health professions students regardless of pandemic status.
CRediT authorship contribution statement
Jacob Pfeifer: Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing – review & editing. Andrew Egger: Data curation, Investigation, Methodology, Writing – review & editing. Molly Hughes: Data curation, Investigation, Methodology, Writing – review & editing. Lauren Tondl: Data curation, Investigation, Methodology, Writing – review & editing. Robin High: Formal analysis, Visualization, Writing – review & editing. Kari L. Nelson: Conceptualization, Data curation, Investigation, Methodology, Supervision, Writing – review & editing.
Acknowledgements
REDCap at UNMC is supported by the Research IT Office funded by Vice Chancellor for Research (VCR). This publication's contents are the authors' sole responsibility and do not necessarily represent the official views of the VCR and NIH. A special thanks to Dr. Wengel, Dr. Cordts, and Dr. MacArthur in the Department of Psychiatry at UNMC for assistance with the survey design and review of the abstract.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xjep.2022.100531.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Timeline: WHO's COVID-19 response. World health organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline?gclid=Cj0KCQjwse-DBhC7ARIsAI8YcWKUrMTgiP5fFHfBHkz-xTnzc-UGC2p0WqB2dvulzirFvskq5DDjVgsaAp0zEALw_wcB#event-7 Published January 25, 2021.
- 2.Coronavirus Disease 2019 (COVID-19) Situation Report – 71. World Health Organization. Updated March 31, 2020. Accessed April 18, 2021. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200331-sitrep-71-covid-19.pdf?sfvrsn=4360e92b_8.
- 3.Wong J.G., Cheung E.P., Cheung V., et al. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med Teach. 2004;26(7):657–659. doi: 10.1080/01421590400006572. ECF7M39E5HD9CU5P. [DOI] [PubMed] [Google Scholar]
- 4.Arheiam Arheiam, et al. Perceptions of stress among dental students living in a war-affected zone. J Dent Educ. 2019;83(1):48–55. doi: 10.21815/jde.019.006. [DOI] [PubMed] [Google Scholar]
- 5.Al-Rabiaah Abdulkarim, et al. Middle East respiratory syndrome-corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi arabia. J Infect Public Health. 2020 doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 7.Swarbrick M., March A wellness model for clients. Ment Health Spec Interest Q. 1997;20:1–4. [Google Scholar]
- 8.American Psychological Association What's the difference between stress and anxiety? American Psychological Association. https://www.apa.org/topics/stress/anxiety-difference Retrieved March 24, 2022, from.
- 9.Guo Alyssa A., et al. Assessing the psychological impacts of COVID-19 in undergraduate medical students. Int J Environ Res Publ Health. 13 Mar. 2021;18 doi: 10.3390/ijerph18062952. 6 2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daviu Nuria, Bruchas Michael R., Moghaddam Bita, Sandi Carmen, Beyeler Anna. Neurobiological links between stress and anxiety. Neurobiol Stress. 2019;11 doi: 10.1016/j.ynstr.2019.100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dedeilia Aikaterini, et al. Vivo. International Institute of Anticancer Research; 1 June 2020. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. iv.iiarjournals.org/content/34/3_suppl/1603.long. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anthone G. Nebraska Department of Health and Human Services; Omaha, NE: 2020. Directed Health Measure Order 2020-001; pp. 1–4.https://dhhs.ne.gov/Archived%20DHMs/DHM-March%2019-2020.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.