Abstract
Background:
Antisocial personality disorder (ASPD) incurs a high cost to society due to the high risk of violent and nonviolent offenses associated with this personality disorder, thus making the examination of the etiology and the onset of ASPD an important public health concern.
Method:
The present study consisted of five waves of data collection of the Harlem Longitudinal Development Study (N=674). In the Cox proportional hazard model, latent multiple substance use trajectories from mid-adolescence to emerging adulthood (mean age 14 to mean age 24) were used as a predictor for the onset of ASPD during emerging adulthood to the mid-thirties (mean age 24 to mean age 36). The control variables were gender, ethnicity, problem behaviors, and victimization.
Results:
In the multiple Cox proportional hazard model, the high (HR = 2.74, p<0.001) and the increasing frequency of (HR = 2.55, p<0.001) use on alcohol, cigarette, and cannabis latent trajectory groups were associated with an increased hazard of ASPD onset as compared with the no or low frequency of use on alcohol, cigarette, and cannabis latent trajectory group after controlling for demographic factors and earlier problem behaviors as well as victimization.
Conclusions:
The implications of this study for the prediction of adult ASPD onset time may focus on the early use of alcohol, cigarette, and cannabis from mid adolescence to emerging adulthood.
Keywords: Antisocial personality disorders, Harlem Longitudinal Development Study, problem behaviors, substance use, survival analysis, victimization
Introduction
Antisocial personality disorder (ASPD) is a disorder characterized by an enduring pattern of behaviors showing a lack of regard for the rights of others. Its onset is typically in childhood in the form of conduct disorder and it continues through adolescence and adulthood. ASPD typically peaks during young adulthood and into the early forties (ages 24–44).1 It is estimated that 0.2–3.3% of the population are affected by ASPD1; however, estimates vary markedly by gender as well as population. For example, ASPD is diagnosed more frequently in men than in women.2 Population estimate for men was 5.5%; for women, it was 1.9%.3 In terms of race/ethnicity, the prevalence of personality disorders including ASPD among African Americans (14.7%) was somewhat lower than among Latinos (17.2%).4 ASPD incurs a high cost to society due to the high risk of violent and nonviolent offending behaviors associated with this personality disorder,5 thus making the examination of the etiology and the onset of ASPD an important public health concern.
ASPD is associated with two personality trait variables: impulsiveness and aggressiveness,6 both have also been associated with adolescent problem behavior and are characteristic of childhood conduct disorder.7 In fact, impaired self-control, a hallmark of ASPD, is one of the major contributing factors to violent and criminal behaviors that are often associated with ASPD.8 For example, ASPD has been found to be related to risk-taking behaviors, such as betting and impulsivity.9 These same personality traits are also related to the problematic use of substances.10,11 Indeed, a longitudinal study based on a large community sample found that, compared with members of the group consisting of only occasional alcohol use, those in the group which included participants reporting high levels of alcohol, cigarette, and cannabis use had significantly greater odds of having ASPD.12
In addition to impulsivity and substance use, notably physical and/or sexual victimization are related to ASPD. For example, a study of heterosexual couples found that ASPD was linked to significantly higher levels of perpetration of intimate partner violence and victimization.13 In another study of incarcerated women and men, those who had a history of physical trauma were five times more likely to be diagnosed with ASPD than those without such a history.14 In a related vein, those with ASPD reported a high frequency of severe physical and sexual abuse in childhood.15
Research showing associations of ASPD with its correlates uses the ASPD measures of which assessed at one point in time. It is, therefore, not known when the onset of ASPD occurred. The current study sought to fill this gap by assessing ASPD at four points in time, between emerging adulthood (mean age 24) and adulthood (mean age 36). This study design overcomes a limitation of previous findings reported in the literature in terms of the limited number of time points for measuring ASPD. Moreover, from a methodological perspective, there are no study design that employs the latent trajectory analysis (for longitudinal substance use) and survival analysis (for onset of ASPD) to elucidate the associations of earlier correlates, such as substance use (alcohol, cigarette, cannabis), victimization (physical, sexual), problem behaviors (risk taking, rule breaking), and demographic factors (gender, ethnicity) with later ASPD.
We hypothesized that problem behaviors in mid adolescence, victimization in late adolescence, and higher or increasing substance use from mid-adolescence to emerging adulthood (mean age 14 to mean age 24) would be associated with an increased hazard of ASPD onset during emerging adulthood to the mid-thirties (mean age 24 to mean age 36).
Method
Participants
The present study consisted of five waves of data collection of the Harlem Longitudinal Development Study. About a half of the participants were African Americans (52%), and other half were Latinxs (48%). The study began in 1990 (Time 1; T1) when participants were mean age 14.1 years (SD = 1.3 years; N=1,332). Participants were originally recruited from public schools in the East Harlem area of New York City. The second wave of data collection took place in 1994–1996 (Time 2; T2) when participants were mean age 19.2 (SD = 1.5; N=1,190). At Time 3 (T3; 2000–2001), the sample size was reduced (N=662) due to budgetary restrictions, and participants were randomly selected from those who had participated at T2 (mean age=24.4; SD = 1.3). At time 4 (T4; 2001–2003), participants were mean age 27.1 (SD = 1.4; N=475). At time 5 (T5; 2004–2006), participants were mean age 29.2 (SD = 1.4; N=838). Data collection at time 6 (T6) took place in 2011–2013 when participants were mean age 35.9 years (SD = 1.3; N=674). At T1, questionnaires were administered in the school classrooms via tape players under the supervision of study staff. (Teachers were not present.) At T2, T3, and T4, participants were interviewed in person or by phone if they had moved far away from New York City. At T5 and T6, participants used mailed questionnaires which they self-administered and returned to us de-identified, i.e., data were identified by the participants study code number. At T1 and T2, parents of participants who were under 18 years of age provided passive consent for their child’s participation in the study. Participants who were 18 years or older (i.e., T3–T6) provided signed informed consent forms. The Institutional Review Boards of New York Medical College, the Mount Sinai School of Medicine, and the New York University School of Medicine approved the study’s procedures for data collection. A Certificate of Confidentiality was obtained from the National Institute on Drug Abuse for T1, T2, T3, T5, and T6 and the National Cancer Institute at T4. Additional information regarding the study methodology is available from a previous report.16
Measures
The independent variables in the present study comprised four domains, which consisted of demographic factors, problem behaviors at T1, victimization at T2, and substance use at T1–T3. Demographic factors (at age 39) included gender (male = 1, female = 2) and ethnicity (African America N=1, Latinxs = 2).
The problem behaviors domain (T1) included rule breaking behaviors, a 3 item scale, e.g., “How often do you break your parents’ rules? with answer options: not at all (1), a little (2), somewhat (3), and very much (4) and risk taking behaviors, a 6 item scale, e.g., “Do you like to live dangerously? with answer options: completely false (1), mostly false (2), mostly true (3), completely true (4).
The victimization domain (T2) included physical victimization, a 5-item scale, e.g., “How often have you experienced that someone hit you with a weapon or shot you?” with answer options: never (1), a few times a year or less (2), about once a month (3), and several times a month or more (4) and sexual victimization, a single item, i.e., “Have you been pushed by someone to have sex?” with yes (1) or no (0) answer options.
The substance use domain (T1, T2, T3) included alcohol use, cigarette use, and cannabis use. Alcohol use, a single item, assessing the frequency and quantity of alcohol use in the past 5 years. Answer options were none (0), less than once a week (1), once a week to several times a week (2), 1 or 2 drinks everyday (3), and three or more drinks every day (4). Cigarette use, a single item, assessing the frequency and quantity of cigarette use in the past 5 years. Answer options were none (0), a few cigarettes or less a week (1), 1–5 cigarettes a day (2), about half a pack a day (3), about 1 pack a day (4), about 1 and half packs a day (5), and more than 1 and half packs a day (6). Cannabis use, a single item, assessing the frequency and quantity of cannabis use in the past 5 years. Answer options were never (0), a few times a year or less (1), about once a month (2), several times a month (3), and once a week or more (4).
Antisocial personality disorder
Antisocial personality disorder was assessed at ages 24, 27, 29, and 36 using an adaptation of criteria presented in the DSM-IV.17 The measure of ASPD obtained a score of 1 if a participant answered yes 1 or more on the first following 6 questions (question number 1–6) and if a participant answered yes 3 or more on the last following 7 questions (question number 7–13). Before you were 15 years old, did you: (1) Repeatedly skip school or run away from home overnight?; (2) Repeatedly lie, cheat, “con” others, or steal?; (3) Start fights or bully, threaten, or intimidate others?; (4) Deliberately destroy things or start fires?; (5) Deliberately hurt animals or people?; (6) Force someone to have sex with you? Since you were 15 years old, have you: (7) Done things that are illegal even if you did not get caught (for example, destroying property, shoplifting, stealing, selling drugs, or committing a felony)?; (8) Often lied or “conned” other people to get money or pleasure, or lied just for fun?; (9) Often act on the spur of the moment without stopping to think?; (10) Been in physical fights repeatedly (including physical fight with your spouse or children)?; (11) Exposed others to danger without caring?; (12) Repeatedly behaved in a way that others would consider irresponsible, like failing to pay for things you owed or deliberately not working to support yourself?; (13) Felt no guilt after hurting, mistreating, lying to, or stealing from others, or after damaging property? Otherwise, ASPD obtained a score of 0.
Missing observations and imputation
We had no missing values for ASPD, gender, ethnicity, alcohol use at T1 and T2, cigarette use at T1 and T2, cannabis use at T1 and T2, physical victimization at T2, and sexual victimization at T2. For the other variables, the percentages of missing values were ranged in between less than 1% (rule breaking behaviors at T1, risk taking behaviors at T1) and 28% (alcohol use a T3, cigarette use at T3, cannabis use at T3).
The missing percentages of the missing values for alcohol use a T3, cigarette use at T3, cannabis use at T3 were high, but we used a full likelihood method to construct latent trajectory groups. Therefore, we did not need missing imputation for the substance use variables.
To handle the missing values for rule breaking behaviors at T1 and risk taking behaviors at T1, we applied the random forest18 imputation method which is contemporary multivariate missing values imputation method based on a data mining approach. This random forest imputation method can simultaneously impute missing values of qualitative and quantitative variables. The random forest model continuously updates the imputed variables and assesses its performance between iterations. When the performance has increased, the imputation algorithm stops. The random forest imputation is known to be efficient compared to other imputation methods19–22 without assumptions such as normality, linearity, or homoscedasticity.23 We used the R package “missForest”24 to impute the missing values for rule breaking behaviors at T1and risk taking behaviors at T1.
Analytic procedure
We performed a sensitivity analysis based on a sensitivity index (i.e., q-value)25 by permuting the use of three substances. To perform the sensitivity analysis for each substance use variable individually, we considered a derived alcohol variable. The derived alcohol variable obtained a score of 1 if the response of alcohol use at T1 or at T3 was greater than 1; otherwise 0. This variable reflects the values of the alcohol use for the heavy use group or increasing use group. For the inclusion of alcohol and cigarette use in the model predicting the onset time of ASPD, we performed a sensitivity analysis using the derived alcohol use, average cigarette use, average cannabis use in a Cox PH model controlling for the same covariates. We assessed substance use at three points in time because substance use variables were used as the major predictors of ASPD whereas we assessed gender, ethnicity, problem behaviors, and victimization at one point in time because these variables were used as control variables. We used statistical software Mplus26 to run latent class growth analyses (LCGAs) and growth mixture models (GMMs), and to obtain the latent triple trajectories of alcohol use, cigarette use, and cannabis use from T1 to T3. Each substance use variable at a time point is treated as a censored normal random variable. For subject i in the latent trajectory group g, the use of substance j at time ti is modeled as
where (bgijk) has a 9-dimensional multivariate normal distribution, and ϵgijti is an independent random error. The probability πg is the probability that the trajectory group membership variable Ci = g, that is, the subject belongs to the trajectory group g. Since our model uses a quadratic function in three time points, only fixed effects are considered at individual level. We determined the number of trajectory groups based on multiple criteria including Bayesian Information Criterion (BIC), likelihood ratio tests, entropy, and the smallest class proportion as in Infurna and Grimm.27 The Bayesian posterior probability (BPP) for subject i that belongs to the trajectory group k is denoted by τik = P(Ci = g|yi). In the next step, we employed the semi-parametric Cox proportional hazard (Cox PH) regression model28 which extends survival analysis methods to assess simultaneously the effect of several risk factors on survival time. For each subject, the ASPD variable was measured at four distinct time points, T3, T4, T5, and T6. It is more statistically sound to consider the onset time of ASPD as interval censored data rather than independent right censored data.
The hazard function λ(t|x) with covariate vector x = (x1, …, xp) is assumed to be proportional to a baseline hazard λ0(t) as follow:
The survival function is given by .
The icenReg package29 of statistical software R was then employed to examine how the predictors (i.e., gender, ethnicity, rule breaking behaviors at T1, risk taking behaviors at T1, physical victimization at T2, sexual victimization at T2, and the triple trajectories of alcohol use at T1–T3, cigarette use at T1–T3, and cannabis use at T1–T3) related to the onset of ASPD. Simple Cox PH models for each of the 7 predictors as well as a multiple Cox PH model were conducted (Supplementary material).
To illustrate the effects of the triple trajectories of alcohol use, cigarette use, and cannabis use on the onset of ASPD, we constructed the estimated survival curves based on the nonparametric Kaplan-Meier estimators30 for each of the trajectory group memberships. In addition, we adjusted survival curves by including the covariates that used in the Cox PH model. To conduct the adjusted survival curves, we used the conditional method which is most widely used among other methods.31 These curves were constructed from the average-time values of the interval censored data. For example, when ASPD was found at T4, we considered (T3+T4)/2 as the ASPD onset time. If a subject did not have ASPD until T6, we considered this subject as right censored at T6.
Results
The Monte–Carlo permutation q-value for the increasing group was 0, and the q-value of the heavy use group was 7 × 10−4. More specifically, the q-value of the derived alcohol variable was 0.002, that of average cigarette was 0.039, and that of average cannabis was 0.018, which indicated that all three substances use should be included in the model.
In the standard Cox PH model, the p-values of average cannabis use, average cigarette use, and average alcohol use in the same order were 0.004, 0.017, and 0.79, respectively. However, if we used a categorical alcohol variable, the p-values of the three substances ranged from 0.007 to 0.025 indicating that all three substances seem to have effects on the onset time of ASPD.
Table 1 summarizes the fit statistics for LCGA and GMM models. Based on LCGA models, a 5-group model had the smallest BIC value. However, Vuong-Lo-Mendell-Rubin likelihood ratio test (LMR LRT) and adjusted Vuong-Lo-Mendell-Rubin likelihood ratio test (aLMR LRT) indicated 4- and 5-group models were not significant. Also, a 3-group LCGA model had the greatest entropy value. Based on GMM models, a 3-group model had the smallest BIC value, but LMR LRT or aLMR LRT indicated that a 3-group model was not significant. In addition, all GMM models had at least one class of less than 5% prevalence. Based on the criteria of LMR LRT and aLMR LRT, maximum entropy, minimum prevalence of 5%, 3-group LCGA model appeared the best. Therefore, we selected the 3-group LCGA model to perform survival analysis in the next step. Figure 1 presents the observed trajectories of alcohol use, cigarette use, and cannabis use from age 14–24 and the percentages in each of the three trajectory groups. The mean Bayesian posterior probability (BPP) in each trajectory group ranged from 88% to 93%, which indicated an adequate classification. (See Figure 1.)
Table 1.
Fit statistics for latent class growth analysis (LCGA) and growth mixture model (GMM) for three substances use.
| Class | Class sizes | Parameters | BIC | LMR-LRT | aLMR-LRT | Entropy |
|---|---|---|---|---|---|---|
| LCGA | ||||||
| 1 | 674 | 18 | 12172 | |||
| 2 | 271, 403 | 28 | 11427 | <0.001 | <0.001 | 0.795 |
| 3 | 204, 392, 78 | 38 | 11323 | 0.017 | 0.018 | 0.796 |
| 4 | 82, 286, 182, 124 | 48 | 11306 | 0.226 | 0.226 | 0.722 |
| 5 | 288, 93, 96, 115, 82 | 58 | 11285 | 0.773 | 0.773 | 0.768 |
| 6 | 270, 165, 82, 115, 36, 6 | 68 | 11286 | 0.438 | 0.443 | 0.792 |
| GMM | ||||||
| 1 | 674 | 63 | 13269 | |||
| 2 | 30, 644 | 73 | 12371 | 0.226 | 0.226 | 1.000 |
| 3 | 41, 19, 614 | 83 | 11680 | 0.240 | 0.240 | 1.000 |
| 4 | 522, 117, 6, 29 | 93 | 11715 | 0.225 | 0.225 | 0.987 |
Notes. Class: number of trajectory groups; Class sizes: number of individuals in each group; Parameters: total number of parameters in the model; BIC: Bayesian information criterion; LMR LRT: Vuong-Lo-Mendell-Rubin likelihood ratio test; aLMR LRT: adjusted Vuong-Lo-Mendell-Rubin likelihood ratio test.
Figure 1.
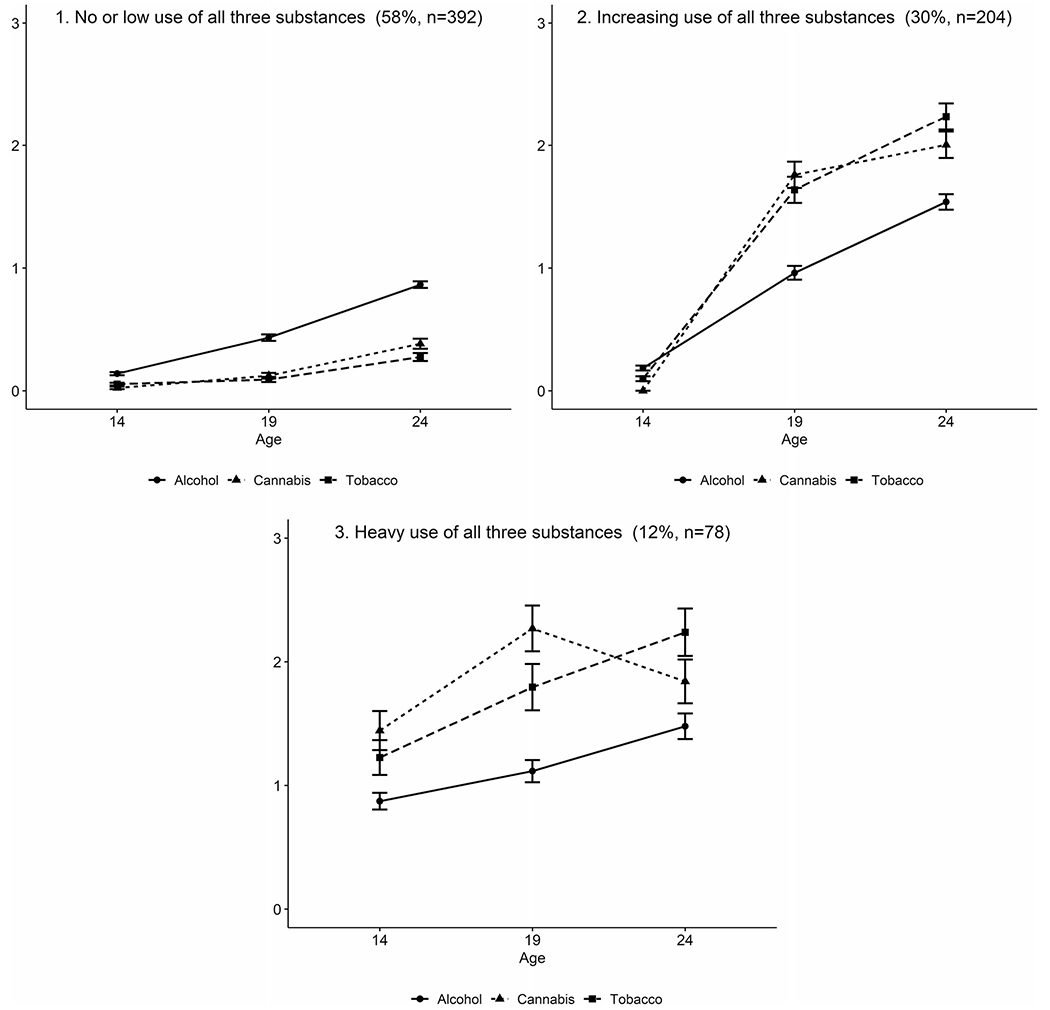
Triple trajectories of alcohol use, cigarette use, and cannabis use from mid adolescence to emerging adulthood (mean age 14-24).
Note. Response options for alcohol use: none (0), less than once a week (1), once a week to several times a week (2), 1 or 2 drinks everyday (3), and three or more drinks every day (4); cigarette use: none (0), a few cigarettes or less a week (1), 1-5 cigarettes a day (2), about half a pack a day (3), about 1 pack a day (4), about 1 and half packs a day (5), and more than 1 and half packs a day (6); and cannabis use: never (0), a few times a year or less (1), about once a month (2), several times a month (3), and once a week or more (4).
The three trajectory groups were (1) High frequency of use on alcohol, cigarette, and cannabis (prevalence 12%, mean BPP = 91%); (2) Increasing frequency of use on alcohol, cigarette, and cannabis (prevalence 30%, mean BPP = 88%); and (3) No or low frequency of use on alcohol, cigarette, and cannabis (prevalence 58%, mean BPP = 93%).
Figure 2 shows the estimated marginal effects of the triple trajectory group memberships on the onset of ASPD by the Kaplan-Meier nonparametric method. Figure 3 presents the adjusted survival curves including same covariates in the Cox PH model by the conditional method. The estimated survival curve of the no or low frequency of use on alcohol, cigarette, and cannabis trajectory group decreased slowly whereas the high frequency of use on alcohol, cigarette, and cannabis and the increasing frequency of use on alcohol, cigarette, and cannabis trajectory groups decreased fast. More specifically, the high- and the increasing frequency of use on alcohol, cigarette, and cannabis trajectory groups had similar patterns until the mid 20s, but the high frequency of use on alcohol, cigarette, and cannabis trajectory group decreased faster than the increasing frequency of use on alcohol, cigarette, and cannabis trajectory group thereafter.
Figure 2.
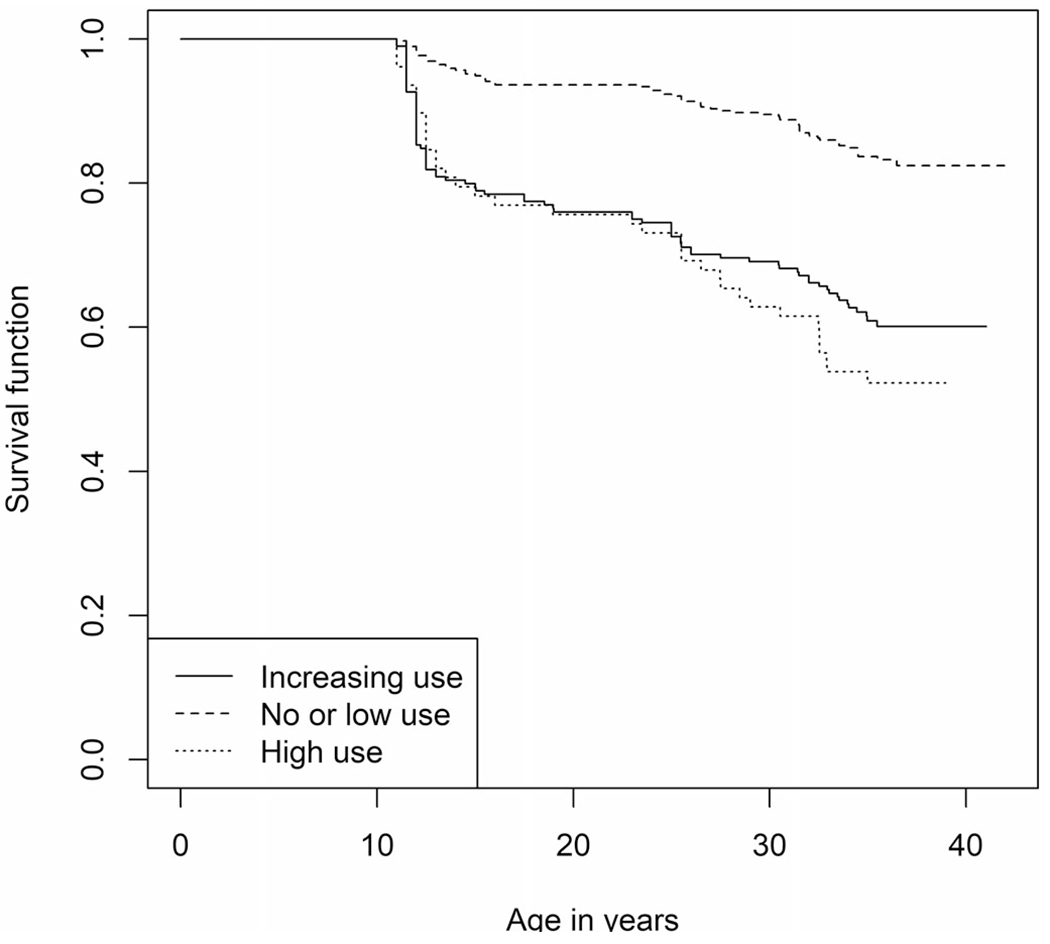
Kaplan-Meier survival curves for the three trajectory groups of substance use.
Figure 3.
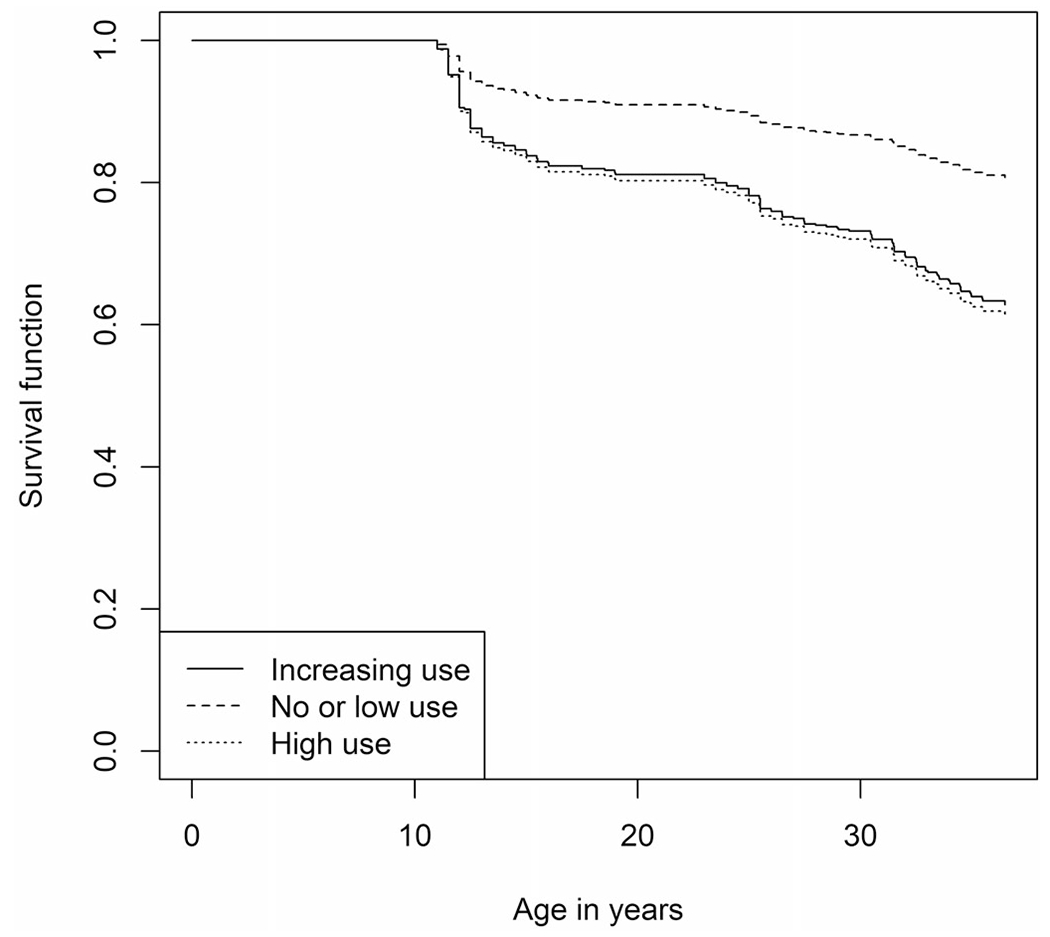
Adjusted survival curves for the three trajectory groups of substances use.
Table 2 presents the regression coefficients (b) and hazard ratios (HR: eb) from the 7 simple Cox Proportional Hazard regression models. The p-values for the simple Cox PH regression models (i.e., 0.071<p-values < 0.93) indicated that there was no violation of the proportional hazard assumption. Male gender was associated with an increased hazard of ASPD onset between T3 and T6 as compared to female gender (HR = 1.97, p<0.001). Risk taking behaviors at T1 (HR = 1.11, p<0.001), rule breaking behaviors at T1 (HR = 1.15, p<0.001), and physical victimization at T2 (HR = 1.13, p<0.001) were associated with an increased hazard of ASPD onset between T3 and T6. As compared with the no or low frequency of use on alcohol, cigarette, and cannabis trajectory group at T1–T3, the high frequency of use on alcohol, cigarette, and cannabis trajectory group at T1-T3 (HR = 4.40, p<0.001), and the increasing frequency of use on alcohol, cigarette, and cannabis trajectory group at T1–T3 (HR = 3.31, p<0.001) were associated with an increased hazard of ASPD onset between T3 and T6.
Table 2.
Parameters from the 7 simple Cox proportional hazard regression models predicting onset time of ASPD.
| Estimate, b | Hazard ratio, eb | Standard error, s.e. | Z-value, Z | p-Value, p | |
|---|---|---|---|---|---|
| Demographic factors | |||||
| aGender | 0.68 | 1.97 | 0.15 | 4.57 | <0.001 |
| bEthnicity | 0.27 | 1.31 | 0.14 | 1.85 | 0.064 |
| Problem behaviors at T1 | |||||
| cRisk-taking behaviors | 0.10 | 1.11 | 0.02 | 5.14 | <0.001 |
| dRule-breaking behaviors | 0.14 | 1.15 | 0.04 | 3.86 | <0.001 |
| Victimization at T2 | |||||
| ePhysical victimization | 0.12 | 1.13 | 0.02 | 5.68 | <0.001 |
| fSexual victimization | 0.10 | 1.11 | 0.18 | 0.54 | 0.59 |
| gTriple trajectories of alcohol use, cigarette use, and cannabis use from T1 through T3 | |||||
| High use | 1.48 | 4.40 | 0.22 | 6.85 | <0.001 |
| Increasing use | 1.20 | 3.31 | 0.19 | 6.29 | <0.001 |
Notes. Baseline: semi-parametric; the number of bootstrap samples = 100. Final log-likelihood and the number of iterations for each of the 7 simple Cox PH regression models.
−588.36 and 41;
−597.11 and 19;
−586.79 and 32;
−588.92 and 17;
−582.77 and 24;
−598.54 and 19;
−567.96 and 41.
Table 3 presents the regression coefficients (b) and hazard ratios (HR: eb) from the multiple Cox Proportional Hazard regression model. The results of the proportional hazards assumption test for a multiple Cox regression model fit were satisfactory (the global test p-value was 0.115, and the smallest p-value was 0.059). Male gender was associated with an increased hazard of ASPD onset between T3 andT6 as compared to female gender (HR = 1.57, p<0.01). Rule breaking behaviors at T1 (HR = 1.08, p<0.05) and physical victimization at T2 (HR = 1.06, p<0.05) were associated with an increased hazard of ASPD onset between T3 and T6. As compared with the no or low frequency of use on alcohol, cigarette, and cannabis trajectory group at T1–T3, the high frequency of use on alcohol, cigarette, and cannabis trajectory group at T1–T3 (HR = 2.74, p<0.001) and the increasing frequency of use on alcohol, cigarette, and cannabis trajectory group at T1-T3 (HR = 2.55, p<0.001) were associated with an increased hazard of ASPD onset between T3 and T6.
Table 3.
Parameters from the multiple Cox proportional hazard regression model predicting onset time of ASPD.
| Estimate, b | Hazard ratio, eb | Standard error, s.e. | Z-value, Z | p-Value, p | |
|---|---|---|---|---|---|
| Demographic factors | |||||
| Gender | 0.45 | 1.57 | 0.17 | 2.72 | 0.007 |
| Ethnicity | 0.12 | 1.13 | 0.16 | 0.77 | 0.44 |
| Problem behaviors at T1 | |||||
| Risk taking behaviors | 0.04 | 1.04 | 0.03 | 1.41 | 0.16 |
| Rule breaking behaviors | 0.08 | 1.08 | 0.04 | 2.04 | 0.04 |
| Victimization at T2 | |||||
| Physical victimization | 0.06 | 1.06 | 0.02 | 2.51 | 0.012 |
| Sexual victimization | −0.13 | 0.88 | 0.20 | −0.65 | 0.52 |
| Triple trajectories of alcohol use, cigarette use, and cannabis use from T1 through T3 | |||||
| High use | 1.01 | 2.74 | 0.28 | 3.65 | <0.001 |
| Increasing use | 0.94 | 2.55 | 0.19 | 4.88 | <0.001 |
Notes. Baseline: semi-parametric; the number of bootstrap samples = 100. Final log-likelihood and the number of iterations for the multiple Cox Proportional Hazard regression model: −551.38 and 47. Maximum variance inflation factors: 1.33.
Discussion
The present study is unique because we examined the trajectories of alcohol, cigarette, cannabis use from mid adolescence through the emerging adulthood, risk taking and rule breaking behaviors in mid adolescence, and physical and sexual victimization in late adolescence to predict the onset of ASPD during the period between emerging adulthood and adulthood among African Americans and Latinxs. Also, it allows us to estimate the hazard of a specific event such as ASPD, since we used the interval censored Cox Proportional Hazard Model for investigating the effect of several variables upon a time specified event (i.e., ASPD) takes to happen. Practically, the structure (e.g., linear or non-linear) of substance use variables is not known to have effects on the outcome variable (e.g., ASPD); nonetheless, our approach can handle some non-linear effects without specifying the non-linear way of association.
In addition, we followed up our adolescent sample to mean age 36 years in order to identify the time of onset for ASPD within several developmental stages. In contrast, the major of prior research has been conducted on samples of either adolescents or adults and not covered a range of developmental periods.
The results supported our hypothesis that earlier problem behaviors, victimization, and substance use were associated with an increased hazard of later onset of ASPD. More specifically, the associations of rule breaking behaviors in mid adolescence, physical victimization in late adolescence, and the use of alcohol, cigarette, and cannabis from mid adolescence through emerging adulthood with onset time of ASPD during emerging adulthood to adulthood were maintained after controlling for all variables used in the present study.
As regards to the association between rule breaking behaviors and ASPD, personality-related disorder (e.g., ASPD) and impulsive aggressive behaviors (e.g., rule breaking behavior) may co-occur by presenting a common underlying disposition. Also, the adult criteria for ASPD is consistent with the criteria for child Conduct Disorder.1 In other words, individuals who break rules often may develop the common personality traits (e.g., impulsiveness, aggressiveness) from childhood to adulthood.
Our research also confirmed that victimization in late adolescence (mean age 19), as measured by experiences of violence and sexual coercion, predicted the onset of ASPD from emerging adulthood to the mid-thirties. Previous research has documented associations between victimization and ASPD, though typically not over such an extended period of time.13–15 Alternatively, studies have examined the link between childhood trauma and adult ASPD.32–35 A study by Gobin et al.,14 for example, found that participants who reported having experienced physical trauma were more likely meet criteria for ASPD than those without such a history. In this study, ASPD was associated with both physical and crime-related victimization, mirroring our own findings. However, this study was cross-sectional in nature, making it difficult to establish a causal relationship.
In terms of a relationship between substance use and ASPD, our findings indicated that members of the high and increasing frequency of use on alcohol, cigarette, and cannabis trajectory groups were more likely to report ASPD in adulthood than were members of the no or low frequency of use on alcohol, cigarette, and cannabis trajectory group. These results are consistent with prior research reporting a comorbidity of substance use disorder and ASPD after adjusted for sociodemographic characteristics and other psychiatric disorders.36 These findings suggest that the high use of all three substances (i.e., alcohol, cigarette, and cannabis) may detract the individual from pro-social behaviors. Substance use and antisocial behaviors may share a common risk marker for externalizing behaviors.37,38 Here, one of our predictors in adolescence, Rule breaking behaviors, could be a possible common risk trait since such behaviors often go along with problems with an individual’s ability to interact with others.
Limitations and strengths
The sample consisted of urban African Americans and Latinxs. Further studies should include other ethnic/racial groups for generalization to the United States population. Our data are also based on self-reports, which can lead to biased results since people may under-report their experiences with antisocial behaviors and/or drug use. However, studies have shown that the use of this type of self-report data yields reliable results.39,40 The measure ASPD may be related to the use of substances rather than an idiopathic or intrinsic disorder. Since alcohol use, cigarette use, and cannabis use often co-occur with other substance use, particularly in adolescents and young adults, there may exist confounding factors unobserved. Lastly, providing more answer options of substance use may lead to results that are more accurate.
Despite these limitations, the study supports and adds to the literature in a number of ways. First, we assess ASPD at four points in time over a span of up to 12 years, whereas most research studies in this area focus on one point in time. The prospective nature of the data allowed us to go beyond a cross-sectional analysis and to consider the temporal sequencing of the variables. Second, a major contribution of the study is a unique set of findings associated with a number of covariates in mid-, late-adolescence, and emerging adulthood as related to the onset time of ASPD beginning in emerging adulthood in a sample of African Americans and Latinxs living in an urban area of New York City. Third, the study design integrated two sophisticated statistical analyses (i.e., latent trajectory analysis and survival analysis) in examining the associations between earlier rule breaking behaviors, physical victimization, and the use of alcohol, cigarette, and cannabis and later ASPD.
Conclusions
The implications of this study for prediction of ASPD onset time may focus on the early rule breaking behaviors in mid adolescence, experiences of physical victimization in late adolescence, and the use of alcohol, cigarette, and cannabis from mid adolescence to emerging adulthood. Rule breaking behaviors should not be ignored at early stages of development as treatment of rule breaking/antisocial behaviors during adolescence may help prevent the development of ASPD. Parent-child interaction therapy and group parent behavior therapy are two effective treatments.41,42 These treatments have been proven effective as they bring combined strategies from family, behaviors, and cognitive-behavioral therapies. In sum, we conclude that treatment programs for ASPD may be implemented in parallel with treatment programs focused on substance use as well as adolescent problem behaviors.
Supplementary Material
Funding
This research was supported by the grant [5K01 DA041609] awarded to Dr. Jung Yeon Lee from the National Institute on Drug Abuse.
Footnotes
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Supplemental data for this article is available online at https://doi.org/10.1080/08897077.2021.1946890.
References
- [1].DSM-5. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- [2].Chun S, Harris A, Carrion M, et al. A psychometric investigation of gender differences and common processes across borderline and antisocial personality disorders. J Abnormal Psychol. 2017;126(1):76–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66(06):677–685. [DOI] [PubMed] [Google Scholar]
- [4].Salas-Wright CP, Kagotho N, Vaughn MG. Mood, anxiety, and personality disorders among first and second-generation immigrants to the United States. Psychiatry Res. 2014;220(3):1028–1036. (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Black DW. The natural history of antisocial personality disorder. Can J Psychiatry. 2015;60(7):309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Patrick CJ, Brislin SJ. Antisocial personality disorder/psychopathy. Encycl Clin Psychol. 2015:1–10. [Google Scholar]
- [7].Jessor R, Jessor S, Jessor SL, Jessor R. Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. Cambridge, MA: Academic Press; 1977. [Google Scholar]
- [8].Gottfredson MR, Hirschi T. A General Theory of Crime. Stanford: Stanford University Press; 1990. [Google Scholar]
- [9].De Brito SA, Viding E, Kumari V, Blackwood N, Hodgins S. Cool and hot executive function impairments in violent offenders with antisocial personality disorder with and without psychopathy. PLoS One. 2013;8(6):e65566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Martinez S, Jones JD, Bisaga A, Comer SD. The effects of nicotine administration and drug cue on impulsivity. Drug Alcohol Depend. 2017;171:e130. [Google Scholar]
- [11].Brook JS, Lee JY, Finch SJ, Brown EN, Brook DW. Long-term consequences of membership in trajectory groups of delinquent behavior in an urban sample: violence, drug use, interpersonal, and neighborhood attributes. Aggress Behav. 2013;39(6):440–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Brook JS, Zhang C, Rubenstone E, Primack BA, Brook DW. Comorbid trajectories of substance use as predictors of antisocial personality disorder, major depressive episode, and generalized anxiety disorder. Addict Behav. 2016;62:114–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kelley ML, Braitman AL. Antisocial personality disorder and physical partner violence among single and dual substance-abusing couples. J Fam Viol. 2016;31(4):423–431. [Google Scholar]
- [14].Gobin RL, Reddy MK, Zlotnick C, Johnson JE. Lifetime trauma victimization and PTSD in relation to psychopathy and antisocial personality disorder in a sample of incarcerated women and men. Int J Prison Health. 2015;11(2):64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kumari V, Gudjonsson GH, Raghuvanshi S, et al. Reduced thalamic volume in men with antisocial personality disorder or schizophrenia and a history of serious violence and childhood abuse. Eur Psychiatry. 2013;28(4):225–234. [DOI] [PubMed] [Google Scholar]
- [16].Lee JY, Brook JS, Finch SJ, Brook DW. Trajectories of marijuana use from adolescence to adulthood predicting unemployment in the mid 30s. Am J Addict. 2015;24(5):452–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].DSM-IV. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- [18].Breiman L Random forests. Machine Learning. 2001;45(1):5–32. [Google Scholar]
- [19].Brock GN, Shaffer JR, Blakesley RE, Lotz MJ, Tseng GC. Which missing value imputation method to use in expression profiles: a comparative study and two selection schemes. BMC Bioinformatics. 2008;9(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Celton M, Malpertuy A, Lelandais G, De Brevern AG. Comparative analysis of missing value imputation methods to improve clustering and interpretation of microarray experiments. BMC Genomics. 2010;11(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Schmitt P, Mandel J, Guedj M. A comparison of six methods for missing data imputation. J Biomet Biostat. 2015;6:1. [Google Scholar]
- [22].Kim J-M, Lee K-J, Kim W Variance estimation by multivariate imputation methods in complex survey designs. MAS. 2017;12(3):195–207. [Google Scholar]
- [23].Rieger A, Hothorn T, Strobl C. Random forests with missing values in the covariates. https://epub.ub.uni-muenchen.de/11481/1/techreport.pdf. Published 2010.
- [24].Stekhoven DJ, Bühlmann P. MissForest-non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–118. [DOI] [PubMed] [Google Scholar]
- [25].Xiong S, He X, He Y, Mu W. Sensitivity analysis using permutations. Statistica Sinica. 2018;28:817–837. [Google Scholar]
- [26].Muthén L, Muthén B. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- [27].Infurna FJ, Grimm KJ. The use of growth mixture modeling for studying resilience to major life stressors in adulthood and old age: lessons for class size and identification and model selection. J Gerontol B Psychol Sci Soc Sci. 2017;73(1):148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].David CR. Regression models and life tables (with discussion). J R Stat Soc. 1972;34:187–220. [Google Scholar]
- [29].Anderson-Bergman C. icenReg: regression models for interval censored data in R. J Stat Soft. 2017;81:23. [Google Scholar]
- [30].Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481. [Google Scholar]
- [31].Therneau TM, Crowson CS, Atkinson EJ. Adjusted survival curves. https://cran.r-project.org/web/packages/survival/vignettes/adjcurve.pdf. Published 2015.
- [32].Afifi TO, Mather A, Boman J, et al. Childhood adversity and personality disorders: results from a nationally representative population-based study. J Psychiatr Res. 2011;45(6):814–822. [DOI] [PubMed] [Google Scholar]
- [33].Battle CL, Shea MT, Johnson DM, et al. Childhood maltreatment associated with adult personality disorders: findings from the Collaborative Longitudinal Personality Disorders Study. J Pers Disord. 2004;18(2):193–211. [DOI] [PubMed] [Google Scholar]
- [34].Bierer LM, Yehuda R, Schmeidler J, et al. Abuse and neglect in childhood: relationship to personality disorder diagnoses. CNS Spectr. 2003;8(10):737–754. [DOI] [PubMed] [Google Scholar]
- [35].Horwitz AV, Widom CS, McLaughlin J, White HR. The impact of childhood abuse and neglect on adult mental health: a prospective study. J Health Soc Behav. 2001;42(2):184–201. [PubMed] [Google Scholar]
- [36].Goldstein RB, Chou SP, Saha TD, et al. The epidemiology of antisocial behavioral syndromes in adulthood: results from the national epidemiologic survey on alcohol and related conditions-III. J Clin Psychiatry. 2017;78(1):90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Palmer RHC, Young SE, Hopfer CJ, et al. Developmental epidemiology of drug use and abuse in adolescence and young adulthood: evidence of generalized risk. Drug Alcohol Depend. 2009;102(1–3):78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937. [DOI] [PubMed] [Google Scholar]
- [39].Harrison L, Martin S, Enev T, Harrington D. Comparing Drug Testing and Self-Report of Drug Use among Youths and Young Adults in the General Population. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. [Google Scholar]
- [40].Ledgerwood DM, Goldberger BA, Risk NK, Lewis CE, Price RK. Comparison between self-report and hair analysis of illicit drug use in a community sample of middle-aged men. Addict Behav. 2008;33(9):1131–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Eyberg SM, Funderburk BW, Hembree-Kigin TL, et al. Parent-child interaction therapy with behavior problem children: one and two year maintenance of treatment effects in the family. Child & Family Behavior Therapy 2001;23(4): 1–20. [Google Scholar]
- [42].Danforth JS, Harvey E, Ulaszek WR, McKee TE. The outcome of group parent training for families of children with attention-deficit hyperactivity disorder and defiant/aggressive behavior. J Behav Ther Exp Psychiatry. 2006;37(3):188–205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


