Abstract
Objective
To report a case of early pregnancy loss successfully managed by hysteroscopic resection, review the literature comparing hysteroscopic resection to dilation and curettage for retained products of conception, and review potential advantages of hysteroscopic resection over dilation and curettage for management of early pregnancy loss.
Design
Case report.
Setting
Private practice.
Patient(s)
One woman with early pregnancy loss.
Intervention(s)
Hysteroscopic resection using a mechanical morcellation device.
Main Outcome Measure(s)
Complete uterine evacuation after hysteroscopic resection as demonstrated by a normal transvaginal ultrasound and cessation of bleeding 2 weeks after surgery.
Result(s)
The hysteroscopic fluid deficit was 365 ml, with minimal blood loss. Products of conception were confirmed on pathologic examination. There were no intraoperative or postoperative complications. A saline infusion sonogram obtained 4 months after surgery demonstrated a normal endometrial cavity with no intrauterine adhesions.
Conclusion(s)
Surgical management of early pregnancy loss may be complicated by retained products of conception (RPOC) or intrauterine adhesion formation, which can lead to adverse fertility outcomes in the future. Hysteroscopic resection of RPOC has been associated with fewer cases of intrauterine adhesions, more cases of complete tissue removal, and earlier time to conception compared with dilation and curettage. Early pregnancy loss can also be characterized as RPOC with potentially similar benefits from hysteroscopic resection. Thus, hysteroscopic resection can be considered as an alternative surgical technique for management of early pregnancy loss. This case report demonstrates the successful application of hysteroscopic resection in a case of early pregnancy loss.
Key Words: Early pregnancy loss, hysteroscopy, infertility, intrauterine adhesions, retained products of conception
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/posts/xfre-d-21-00179
Introduction
Early pregnancy loss (EPL) occurs in 10% of all clinically recognized pregnancies. It can be managed expectantly, medically, or surgically. Medical management has a high success rate, especially for early gestations, with a low risk of intrauterine adhesions (IUAs). For women who elect surgical management, one of the potential complications is retained products of conception (RPOC), which occurs in 1% of surgically managed cases (1). However, this incidence may underestimate the true rate of RPOC because many patients are asymptomatic and, thus, not routinely evaluated for RPOC. Left untreated, RPOC may be asymptomatic or may lead to infection, postpartum hemorrhage, abnormal uterine bleeding, and/or IUAs (2, 3, 4).
Another potential complication after surgical management of EPL is IUA formation. Intrauterine adhesions may be asymptomatic or may cause amenorrhea or hypomenorrhea, recurrent pregnancy loss, infertility, preterm delivery, and/or abnormal placentation in future pregnancies (4, 5, 6, 7, 8). In a systematic review, the pooled prevalence of IUAs was 19% after a spontaneous abortion, with 42% characterized as moderate to severe IUAs. There were no IUAs in the patients managed expectantly or medically (9). The major risk factor for IUAs is a history of intrauterine instrumentation, particularly in pregnancy or in the immediate postpartum or postabortal period (10). Westendorp (11) found that the incidence of IUAs was 40% after a postpartum dilation and curettage (D and C) or repeat D and C for persistent RPOC. The risk of IUAs is also higher in women with a history of recurrent pregnancy loss. The incidence of IUAs was 32% in women with a history of 3 or more spontaneous abortions, with 58% of them classified as severe (12). Women with a history of more than 1 spontaneous abortion had a twofold risk of IUAs (odds ratio 2.08; 95% confidence interval [CI]: 1.25–3.48) compared with women with a history of 1 previous spontaneous abortion. Women with a history of multiple D and C procedures are also at an increased risk of IUAs. Women with a history of more than 1 D and C had a twofold risk of IUAs (odds ratio 2.06; 95% CI: 1.23–3.46) compared with women with a history of 1 previous D and C (9).
Hysteroscopic resection (HR) has been well described in the literature for management of RPOC. It has been shown to have a low complication rate, low IUA rate, high future pregnancy rate, and high success rate of complete tissue removal (13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23). In a systematic review by Hooker et al. (24) that compared HR to D and C for RPOC, there was a lower risk of IUAs, a lower risk of incomplete tissue evacuation, and a shorter time to conception in the HR group. There were no differences in conception, live birth, or miscarriage rates (Table 1) (24). Despite these benefits, HR is not commonly performed for the surgical management of EPL.
Table 1.
Summary of studies comparing hysteroscopic resection to dilation and curettage for treatment of retained products of conception.
| Author, year | Study design | Sample size (n) | HR cohort outcomes: % | D&C cohort outcomes: % | P value |
|---|---|---|---|---|---|
| Hooker et al. (24), 2016 | S | 339 (10 cohort studies) HR (147) D&C (192) |
IUA: 13 | IUA: 30 | <.001 |
| Incomplete evacuation: 1 | Incomplete evacuation: 29 | <.0001 | |||
| No complications | Complications: 1.4 | NS | |||
| Conception rate: 82.4 | Conception rate: 81 | NS | |||
| Live birth rate: 88 | Live birth rate: 91.6 | NS | |||
| Miscarriage rate: 14.8 | Miscarriage rate: 14.3 | NS | |||
| Rein et al. (25), 2011 | P | HR (53) D&C (42) |
IUA: 4.2 | IUA: 30.8 | <.001 |
| Time to conception: 27 mo | Time to conception: 34 mo | <.05 | |||
| Conception rate: 68.8 | Conception rate: 59.9 | <.05 | |||
| Live birth rate: 83.9 | Live birth rate: 77.3 | NS | |||
| Miscarriage rate: 9.7 | Miscarriage rate: 13.6 | NS | |||
| Cohen et al. (26), 2001 | R | HR (46) D&C (24) |
Required second hysteroscopy 0 | Required hysteroscopy for persistent trophoblastic tissue 21 | |
| Time to conception: 7.3 mo | Time to conception: 11 mo | <.05 | |||
| Conception rate: 82.4 | Conception rate: 62.5 | NS | |||
| Live birth rate: 71.4 | Live birth rate: 70 | NS | |||
| Miscarriage rate: 7.1 | Miscarriage rate: 30 | NS | |||
| No complications | No complications | NS | |||
| Ben-Ami et al. (27), 2014 | R | HR (83) D&C (94) |
Infertility: 12 | Infertility: 24.5 | <.05 |
| Time to conception: 7.4 mo | Time to conception: 12.9 mo | <.05 | |||
| Conception rate: 92.8 | Conception rate: 92.6 | NS | |||
| Live birth rate: 87 | Live birth rate: 95.4 | NS | |||
| Miscarriage rate: 20.8 | Miscarriage rate: 12.6 | NS | |||
| Smorgick et al. (28), 2018 | R | HR (134) D&C (27) |
Live birth rate: 56 | Live birth rate: 70.4 | NS |
| Miscarriage rate: 18.7 | Miscarriage rate: 19.4 | NS | |||
| Recurrent RPOC: 11.9 | Recurrent RPOC: 33.3 | <.05 | |||
| Abnormal placentationa: 23.9 | Abnormal placentationa: 44.4 | <.05 |
Note: HR = hysteroscopic resection; D&C = dilation and curettage; S = systematic review; P = prospective; R = retrospective; IUA = intrauterine adhesions; RPOC = retained products of conception; NS = not statistically significant.
Placenta accreta or need for manual extraction immediately after vaginal delivery for retained placenta
Case report
The patient provided written consent for publication.
A 33-year–old G4P1021 presented for pregnancy confirmation at a gestational age of 6 weeks. She denied vaginal bleeding and cramping. She had a history of 2 prior 1st-trimester pregnancy losses with 2 prior D and Cs. Transvaginal ultrasound showed a fetal pole measuring 0.35 cm with no cardiac motion. Repeat ultrasound 2 weeks later again showed the absence of cardiac motion and no change in crown-rump length. She elected surgical management with HR (Supplemental Video [available online] and Figs. 1 and 2). The hysteroscopic fluid deficit was 365 ml with minimal blood loss. There were no intraoperative or postoperative complications. Products of conception were confirmed on pathologic examination. Unfortunately, the tissue was sent in Formalin, and hence genetic testing could not be performed. Complete tissue evacuation was confirmed by a thin endometrial lining measuring 8.2 mm without vascularity on pelvic ultrasound 2 weeks after surgery, and the patient reported resolution of vaginal bleeding. A saline infusion sonogram obtained 4 months after surgery demonstrated a normal endometrial cavity with no IUAs.
Figure 1.
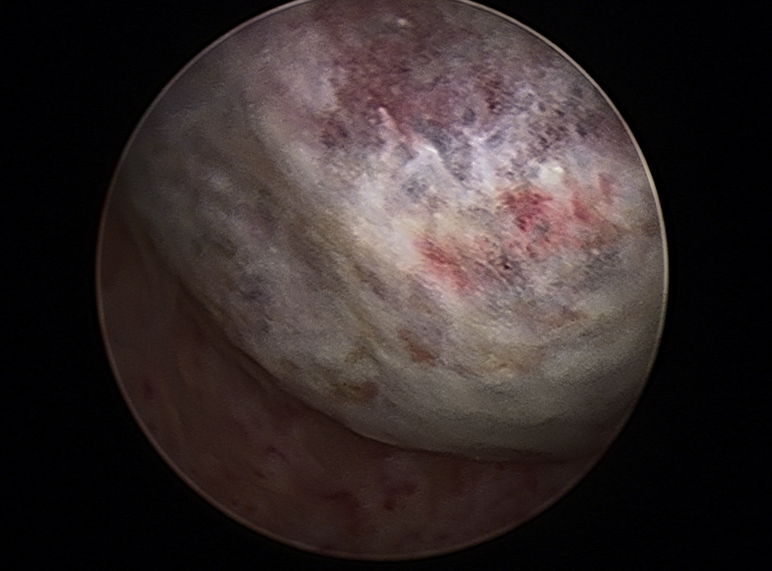
Hysteroscopic findings before resection.
Figure 2.
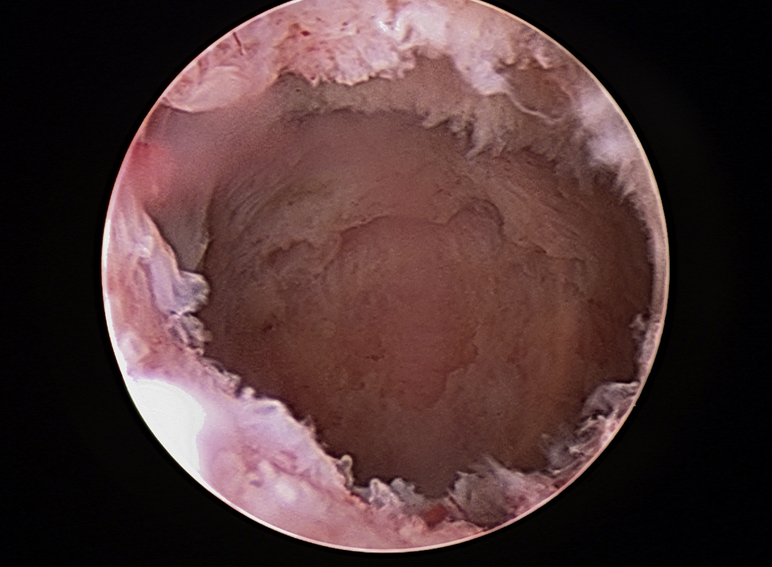
Uterine cavity after hysteroscopic evacuation.
The procedure was performed under general anesthesia in the operating room with the Truclear Elite mini (Medtronic) hysteroscopic tissue removal system. Two hundred milligrams of oral doxycycline was given before surgery. Ten milliliters of dilute (20 units in 100 ml normal saline) vasopressin was injected into the cervix, and 1 g of intravenous tranexamic acid was given during surgery before resection to reduce bleeding and fluid absorption. No mechanical dilation was needed before the insertion of a 0-degree operative hysteroscope with an outer diameter of 6 mm. Opening pressure was set to 80 mm Hg using normal saline as the distension medium. The outflow tract was connected to a wall suction to remove blood and debris for optimal operative field visualization. The soft tissue shaver was introduced into the uterine cavity, and the gestational tissue was mechanically resected and suctioned into the device until no products of conception remained. (Supplemental Video)
Discussion
Intrauterine adhesions form during the healing process between 2 opposing surfaces because of injury to the basalis layer of the endometrium, which can cause partial or complete obliteration of the uterine cavity (6). Hysteroscopic resection may be less traumatic to the uterus than D and C by limiting the area of disruption to only the affected endometrium, thus decreasing the risk of IUA formation.
Hysteroscopic resection allows for more cases of complete removal of products of conception by visual confirmation of complete evacuation. This, in turn, may decrease the risk of future IUA formation and avoid the need for repeat uterine instrumentation, which has the highest rate of IUAs (11). Hysteroscopic resection also allows for the removal of tissue from hard-to-reach areas, such as the uterine cornua, which may be missed during a blind procedure using a rigid curette. Intrauterine adhesions in this area can have particularly negative effects on fertility by causing tubal ostia occlusion.
Numerous studies have demonstrated improved outcomes when comparing HR to D and C for the treatment of RPOC. Rein et al. (25) found that the incidence of IUAs after HR for RPOC was lower, pregnancy rates were higher (particularly for women under the age of 35 years), and the time to conception was shorter compared with those who underwent D and C. A study by Cohen et al. (26) found that 21% of women who initially underwent D and C for RPOC eventually required a second hysteroscopy for persistent trophoblastic tissue. None of the women who initially underwent HR required a second surgery. In a retrospective review by Ben-Ami et al. (27), women who underwent D and C for RPOC had a higher rate of new-onset infertility because of IUAs and tubal occlusion than the women who underwent HR. Smorgick et al. (28) found that women undergoing D and C for RPOC had an increased risk of recurrent RPOC and abnormal placentation in future pregnancies compared with those who underwent HR (Table 1).
Other benefits of HR over D and C include a higher yield for satisfactory genetic testing results. Chromosomal abnormalities account for 50% of EPL cases (1). Thus, chromosomal testing is indicated in patients with recurrent pregnancy loss. It has been shown that HR provides a higher yield of satisfactory fetal chromosomal testing compared with that provided by D and C because of a lower incidence of maternal decidua contamination (88.5% vs. 65%, P<.001) (29). This provides further indirect evidence that HR minimizes disruption of the endometrium compared with D and C.
Operative hysteroscopy provides the additional advantage of simultaneously evaluating the uterine cavity for congenital uterine anomalies (i.e., a uterine septum) and intrauterine pathology (i.e., submucosal fibroids), which may be the underlying etiology of EPL and associated with an increased risk of RPOC (26). In 1 study, 22% (95% CI: 15.3%–30.6%) of women with a history of spontaneous abortion were found to have a congenital or acquired uterine abnormality. The risk was significantly higher in women with more than 1 previous spontaneous abortion compared with that in women with 1 previous spontaneous abortion (29.4% vs. 12.5%, P<.0001) (9). Operative hysteroscopy may result in more cases of complete evacuation and a lower risk of uterine perforation compared with blind D and C, particularly in cases involving uterine anomalies (26).
Applying this technique to cases of EPL may be technically more challenging than applying this technique to cases of RPOC because of vascularity of the gestational tissue. For this reason, we limit the selection of cases to only those of early first trimester losses (i.e., 6–7 weeks gestation) and exclude elective termination of pregnancy. S.Y. routinely uses intracervical vasopressin and intravenous tranexamic acid during surgery. Intracervical vasopressin has been shown to decrease blood loss and fluid absorption during hysteroscopic myomectomy (30), whereas tranexamic acid has been shown to decrease trauma-related blood loss because of its antifibrinolytic activity (31).
In conclusion, operative hysteroscopy techniques can be successfully applied to the surgical management of EPL. Although there are no existing studies on the outcomes after HR for EPL, HR has been shown to have improved outcomes over D and C in cases of RPOC. These same benefits may apply to cases of EPL, which can also be characterized as RPOC. These advantages are particularly important in patients with concerns for IUA formation, such as those with a history of previous D and C procedures, infertility, or recurrent pregnancy loss. It may be preferable for patients at risk for RPOC, such as those with a history of RPOC. It may also be advantageous in women with congenital uterine anomalies or structural intracavity lesions for decreasing the risk of uterine perforation and incomplete tissue evacuation.
Limitations of this case study include the lack of long-term pregnancy and fertility outcomes. It is important to note that there is an increased cost and operating time associated with this technique compared with traditional D and C. Although HR has been shown to have fewer cases of IUAs and more cases of complete tissue evacuation, there were no statistically significant differences in future pregnancy and fertility outcomes, with the exception of a shorter time to conception in the HR group (24). Thus, the clinical implications of the advantages of HR over D and C are unclear. Existing studies comparing HR with D and C for RPOC are mostly retrospective in nature, and there are no randomized controlled trials comparing the 2 techniques. More studies involving HR for EPL and long-term fertility and pregnancy outcomes, as well as a cost-benefit analysis, are needed.
Footnotes
S.Y. has reports honoraria from Medtronic. C.E.M. reports consulting fees, honoraria, and travel support from Medtronic. Medtronic did not provide funding nor was involved in the production of this manuscript.
Supplementary Data
Hysteroscopic resection of early pregnancy loss
Hysteroscopic resection for management of early pregnancy loss
Creator(s): Stacy Young, MD and Charles E. Miller, MD
References
- 1.ACOG practice bulletin no. 200 summary: early pregnancy loss. Obstet Gynecol. 2018;132:1311–1313. doi: 10.1097/AOG.0000000000002900. [DOI] [PubMed] [Google Scholar]
- 2.Ikhena D.E., Bortoletto P., Lawson A.K., Confino R., Marsh E., Milad M., et al. Reproductive outcomes after hysteroscopic resection of retained products of conception. J Minim Invasive Gynecol. 2016;23:1070–1074. doi: 10.1016/j.jmig.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Ami I., Ofir T., Melcer Y., Smorgick N., Schneider D., Pansky M., et al. Infertility following retained products of conception: is it the surgical procedure or the presence of trophoblastic tissue? Eur J Obstet Gynecol Reprod Biol. 2014;182:132–135. doi: 10.1016/j.ejogrb.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Yu D., Wong Y.M., Cheong Y., Xia E., Li T.C. Asherman syndrome—one century later. Fertil Steril. 2008;89:759–779. doi: 10.1016/j.fertnstert.2008.02.096. [DOI] [PubMed] [Google Scholar]
- 5.Deans R., Abbott J. Review of intrauterine adhesions. J Minim Invasive Gynecol. 2010;17:555–569. doi: 10.1016/j.jmig.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Salazar C.A., Isaacson K., Morris S. A comprehensive review of Asherman’s syndrome: causes, symptoms and treatment options. Curr Opin Obstet Gynecol. 2017;29:249–256. doi: 10.1097/GCO.0000000000000378. [DOI] [PubMed] [Google Scholar]
- 7.Tam T., Placek J., Juarez L. Hysteroscopic evacuation of retained products of conception. J Obstet Gynaecol. 2016;36:1004–1005. doi: 10.1080/01443615.2016.1233948. [DOI] [PubMed] [Google Scholar]
- 8.March C.M. Asherman’s syndrome. Semin Reprod Med. 2011;29:83–94. doi: 10.1055/s-0031-1272470. [DOI] [PubMed] [Google Scholar]
- 9.Hooker A.B., Lemmers M., Thurkow A.L., Heymans M.W., Opmeer B.C., Brölmann H.A.M., et al. Systematic review and meta-analysis of intrauterine adhesions after miscarriage: prevalence, risk factors and long-term reproductive outcome. Hum Reprod Update. 2014;20:262–278. doi: 10.1093/humupd/dmt045. [DOI] [PubMed] [Google Scholar]
- 10.Schenker J.G., Margalioth E.J. Intrauterine adhesions: an updated appraisal. Fertil Steril. 1982;37:593–610. doi: 10.1016/s0015-0282(16)46268-0. [DOI] [PubMed] [Google Scholar]
- 11.Westendorp I.C., Ankum W.M., Mol B.W., Vonk J. Prevalence of Asherman’s syndrome after secondary removal of placental remnants or a repeat curettage for incomplete abortion. Hum Reprod. 1998;13:3347–3350. doi: 10.1093/humrep/13.12.3347. [DOI] [PubMed] [Google Scholar]
- 12.Friedler S., Margalioth E.J., Kafka I., Yaffe H. Incidence of post-abortion intra-uterine adhesions evaluated by hysteroscopy—a prospective study. Hum Reprod. 1993;8:442–444. doi: 10.1093/oxfordjournals.humrep.a138068. [DOI] [PubMed] [Google Scholar]
- 13.Capmas P., Lobersztajn A., Duminil L., Barral T., Pourcelot A.G., Fernandez H. Operative hysteroscopy for retained products of conception: efficacy and subsequent fertility. J Gynecol Obstet Hum Reprod. 2019;48:151–154. doi: 10.1016/j.jogoh.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Sonnier L., Torre A., Broux P., Fauconnier A., Huchon C. Evaluation of fertility after operative hysteroscopy to remove retained products of conception. Eur J Obstet Gynecol Reprod Biol. 2017;211:98–102. doi: 10.1016/j.ejogrb.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Smorgick N., Kostin S., Tzur T., Levinsohn-Tavor O., Maymon R., Vaknin Z. Is hysteroscopy the best surgical approach for removal of retained products of conception following surgical termination of pregnancy? J Obstet Gynaecol Can. 2020;42:953–956. doi: 10.1016/j.jogc.2020.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Golan A., Dishi M., Shalev A., Keidar R., Ginath S., Sagiv R. Operative hysteroscopy to remove retained products of conception: novel treatment of an old problem. J Minim Invasive Gynecol. 2011;18:100–103. doi: 10.1016/j.jmig.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Kar S. Hysteroscopy in the diagnosis & management of persistent retained products of conception (RPOC) J Minim Invasive Gynecol. 2015;22:S122–S123. doi: 10.1016/j.jmig.2015.08.359. [DOI] [PubMed] [Google Scholar]
- 18.Smorgick N., Levinsohn-Tavor O., Ben-Ami I., Maymon R., Pansky M., Vaknin Z. Hysteroscopic removal of retained products of conception following first trimester medical abortion. Gynecol Minim Invasive Ther. 2017;6:183–185. doi: 10.1016/j.gmit.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Wessel S., Coryn N., van Vliet H., Schoot B., Weyers S., Hamerlynck T. Reproductive and obstetric outcomes after hysteroscopic removal of retained products of conception. J Minim Invasive Gynecol. 2020;27:840–846. doi: 10.1016/j.jmig.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Vitale S.G., Parry J.P., Carugno J., Cholkeri-Singh A., Corte L.D., Cianci S., et al. Surgical and reproductive outcomes after hysteroscopic removal of retained products of conception: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021;28:204–217. doi: 10.1016/j.jmig.2020.10.028. [DOI] [PubMed] [Google Scholar]
- 21.Smorgick N., Barel O., Fuchs N., Ben-Ami I., Pansky M., Vaknin Z. Hysteroscopic management of retained products of conception: meta-analysis and literature review. Eur J Obstet Gynecol Reprod Biol. 2014;173:19–22. doi: 10.1016/j.ejogrb.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 22.Faivre E., Deffieux X., Mrazguia C., Gervaise A., Chauveaud-Lambling A., Frydman R., et al. Hysteroscopic management of residual trophoblastic tissue and reproductive outcome: a pilot study. J Minim Invasive Gynecol. 2009;16:487–490. doi: 10.1016/j.jmig.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Goldenberg M., Schiff E., Achiron R., Lipitz S., Mashiach S. Managing residual trophoblastic tissue. Hysteroscopy for directing curettage. J Reprod Med. 1997;42:26–28. [PubMed] [Google Scholar]
- 24.Hooker A.B., Aydin H., Brölmann H.A.M., Huirne J.A.F. Long-term complications and reproductive outcome after the management of retained products of conception: a systematic review. Fertil Steril. 2016;105:156–164.e2. doi: 10.1016/j.fertnstert.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 25.Rein D.T., Schmidt T., Hess A.P., Volkmer A., Schöndorf T., Breidenbach M. Hysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettage. J Minim Invasive Gynecol. 2011;18:774–778. doi: 10.1016/j.jmig.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S.B., Kalter-Ferber A., Weisz B.S., Zalel Y., Seidman D.S., Mashiach S., et al. Hysteroscopy may be the method of choice for management of residual trophoblastic tissue. J Am Assoc Gynecol Laparosc. 2001;8:199–202. doi: 10.1016/s1074-3804(05)60577-4. [DOI] [PubMed] [Google Scholar]
- 27.Ben-Ami I., Melcer Y., Smorgick N., Schneider D., Pansky M., Halperin R. A comparison of reproductive outcomes following hysteroscopic management versus dilatation and curettage of retained products of conception. Int J Gynaecol Obstet. 2014;127:86–89. doi: 10.1016/j.ijgo.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Smorgick N., Mittler A., Ben-Ami I., Maymon R., Vaknin Z., Pansky M. Retained products of conception: what is the risk for recurrence on subsequent pregnancies? Eur J Obstet Gynecol Reprod Biol. 2018;224:1–5. doi: 10.1016/j.ejogrb.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 29.Cholkeri-Singh A., Zamfirova I., Miller C.E. Increased fetal chromosome detection with the use of operative hysteroscopy during evacuation of products of conception for diagnosed miscarriage. J Minim Invasive Gynecol. 2020;27:160–165. doi: 10.1016/j.jmig.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 30.Phillips D.R., Nathanson H.G., Milim S.J., Haselkorn J.S., Khapra A., Ross P.L. The effect of dilute vasopressin solution on blood loss during operative hysteroscopy: a randomized controlled trial. Obstet Gynecol. 1996;88:761–766. doi: 10.1016/0029-7844(96)00282-7. [DOI] [PubMed] [Google Scholar]
- 31.Shakur H., Roberts I., Bautista R., Caballero J., Coats T., Dewan Y., et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hysteroscopic resection of early pregnancy loss
Hysteroscopic resection for management of early pregnancy loss
Creator(s): Stacy Young, MD and Charles E. Miller, MD