Abstract
The COVID-19 pandemic and the resulting societal restrictions have had negative implications for mental health in the general population. The aims of the present longitudinal study were (i) to investigate changes in psychopathological symptoms and psychological well-being in a sample of Italian individuals surveyed at different points of the pandemic and (ii) to evaluate the potential risk and protective factors associated with the psychopathological outcomes. Self-reported data on psychiatric symptoms, and psychological well-being were collected in March 2020 (T0, the lockdown phase), in May 2020 (T1, the end of the lockdown phase), and in November 2020 (T2, the second wave of COVID-19 infection). 1258 participants (Mage=23.43, SDage=6.45; 75.4% female) were recruited at T0. Of these, 712 also completed the T1 survey, and 369 also completed the T2 survey. A significant decrease in anxiety, depressive, posttraumatic, and obsessive-compulsive symptoms and a significant increase in psychological well-being were observed from T0 to T1. All psychopathological symptoms increased, and psychological well-being decreased significantly from T1 to T2. Several demographic, psychological and COVID-19-related factors emerged as predictors over the course of the pandemic. The current findings indicated that psychological health covaried with the intensity of the COVID-19 pandemic and the associated societal restrictions.
Keywords: Anxiety, COVID-19, Depression, Longitudinal design, Stress, Obsessive-compulsive symptoms, Psychological well-being
1. Introduction
Several authors (e.g., Guazzini et al., 2022) reported an increased risk of mental health problems among the general population in countries around the world in which the rapid spread of COVID-19 forced the government to put in place restrictive measures to limit disease dissemination. The Italian government introduced confinement measures from March 2020 to the beginning of May 2020, including a lockdown, contact restrictions, the closure of educational institutions, and the closure of nonessential workplaces. Before the beginning of the country-wide lockdown in March 2020, the most affected area was the North, in which some cities (e.g., Codogno in Lombardy) were already under quarantine from the end of February 2020; in that period, research was focused on analysing the impact of COVID-19 disease in the northern area of Italy (e.g., Lasalvia et al., 2020).
Several authors have highlighted the effects of social distancing measures on the mental health of the Italian population during the lockdown phase (from 8 March 2020 to 4 May 2020). For example, Amerio et al. (2021), in a study comparing the period before lockdown with the lockdown phase in a representative sample of 6.003 Italian adults, found a significant increase in depression and anxiety symptoms, poor sleep quality, and a lower quality of life. In general, during the lockdown phase (also called the “first wave of infection”), many countries reported an increased incidence of psychopathological issues such as anxiety, depressive symptoms and posttraumatic stress disorder symptoms (e.g., Gonzalez-Sanguino et al., 2020; Mazza et al., 2020; McPherson et al., 2021; Pierce et al., 2020; Tian et al., 2020; Wang et al., 2020).
A recent meta-analysis showed a positive association between quarantine and anxiety, depression, and stress symptoms, with the longer quarantine time associated with the highest symptomatology (Jin et al., 2021). The effects of quarantine on the population's mental health were previously studied during the outbreak of other diseases, such as Ebola, Middle East respiratory syndrome (MERS), and severe acute respiratory syndrome (SARS). For instance, a rapid review by Brooks et al. (2020) found the highest posttraumatic stress symptoms, psychological distress, irritability, insomnia, low mood, anxiety and depressive symptoms in individuals from the general population who were quarantined.
On May 4th, 2020, Italy started the “second phase”, coinciding with the end of the lockdown phase; in this phase, most working places were reopened, and open-air sports and social activities in small groups were allowed in combination with contact tracing and widespread testing activity. The reopening phase consequently led to a new rise in infections, which led Italy to the “second wave” of the pandemic that started in November 2020; in this phase, the government chose to divide the nation into “zones” based on the number of infections to avoid another generalized lockdown (for more, see Chirico et al., 2021).
A study on Italy's infection incidence during the first and second waves of the pandemic showed that in those areas in which there was a high rate of infection in the first wave, the rate was lower during the second wave, and vice versa; the authors speculated on the possibility that individuals who lived in areas more severely hit by the pandemic during the lockdown phase may have significantly changed their behavior during the second phase (Vinceti et al., 2021).
Several risk factors for developing mental health issues during the pandemic have been identified. First, the populations identified as more vulnerable to developing psychological distress or having pre-existing conditions exacerbated were individuals with chronic or psychiatric illness (Chatterjee et al., 2020; Qiu et al., 2020). For instance, a preliminary study on a sample of patients with obsessive-compulsive disorder showed that after the quarantine, the patients reported a significant increase in obsession and compulsion severity, and participants in remission reported symptoms related to a fear of contamination (Prestia et al., 2020). Additionally, hospital workers (Lasalvia et al., 2020; Lixia et al., 2022), youths (Amendola et al., 2020) and elders (Vinkers et al., 2020) were considered at high risk. Additional sociodemographic variables that have been shown to be risk factors for COVID-19 were being female (Qui et al., 2020; Mazza et al., 2020; Zhou et al., 2020), having a low education level (Qui et al., 2020; Zhou et al., 2020), family income instability (Cao et al.,2020), having infected or deceased family members (Preti et al., 2021; Rossi et al., 2020), being in quarantine due to COVID-19 infection and other stressful events such as the loss of a job or finances (Rossi et al., 2020). Previous research also showed the impact of stressful events on quality of life (e.g., Fernandez et al., 2015), and recent research has reported the impact of quarantine during the COVID-19 pandemic on quality of life, showing that females and elderly individuals were the populations most at risk of experiencing a lower quality of life (Ferreira et al., 2021). Moreover, a three-wave panel survey of the population in Denmark showed a significant decrease in psychological well-being from April 2020 to December 2020 (Sønderskov et al., 2021) and a recent study identified the fear of contracting the virus as a strong risk factor in developing stress-related conditions during the COVID-19 pandemic (Hagger et al., 2020). Finally, a three-wave longitudinal study resulting in the three lockdowns in Slovenia showed a decrease in psychological well-being and an increase in COVID-19 related anxiety from wave 1 to wave 3 especially for those individuals who perceived wave 2 and wave 3 as more stressful than wave 1 (Kozina et al., 2022).
Meanwhile, a new phenomenon named the “infodemic” emerged during the COVID-19 pandemic, referring to a worldwide epidemic of misinformation and conspiracy theories disseminated through various media (The Lancet Infectious Diseases, 2020). Several studies have addressed the impact of the infodemic on psychological issues such as PTSD, anxiety, depressive symptoms, loneliness, and fear (e.g., Dubey et al., 2020; Pian et al., 2021; Tagliabue et al., 2020; Tasnim et al., 2020). Moreover, frequently seeking health information contributes to the generation anxiety symptoms and worry (Norr et al., 2014). A study on 770 individuals infected with COVID-19 with clinically stable conditions showed that the predictors of depression and a lower quality of life were having a family member infected with COVID-19, being severely infected themselves, being male and frequently searching social media for information about COVID-19 (Ma et al., 2020).
Finally, confirming that the COVID-19 pandemic has caused worldwide physical but also psychological health issues, systematic reviews and meta-analyses reported significant higher levels of depression, anxiety, insomnia, post-traumatic stress disorder and psychological distress as short-term consequences of the COVID-19 pandemic equally high across affected countries (Cénat et al., 2021; Salari et al., 2020).
1.1. The current study
Various studies longitudinally explored the population's mental health on successive time points from the beginning of the pandemic (e.g., Kozina et al., 2022; Sønderskov et al., 2021). However, the vast majority of these studies focused on specific psychiatric symptoms (e.g., anxiety) or included samples with pre-existing mental health problems. Moreover, the vast majority of the studies conducted in Italy – even if very sound from a methodological point of view - included just two waves (e.g., Benfante et al., 2022; Guazzini et al., 2022; Medda et al., 2022). Furthermore, only few studies explored the impact of COVID-19 on the general population by also considering well-being (rather than the mere absence of psychiatric symptoms) on successive time points. For this reason the present study aimed to evaluate changes a broad range of psychopathological symptoms (i.e., anxiety, depressive symptoms, posttraumatic symptoms, obsessive-compulsive symptoms) and psychological well-being in a sample of Italian individuals between three different periods of the pandemic: (i) the lockdown phase (T0-March 2020) (ii) the second phase of the pandemic (T1-May 2020) in which there was a decrease of infections and the lockdown ceased, and (iii) the second wave of infection (T3, November 2020), where the number of cases raised again and Italy was divided in “zones” according to the numbers of infected people in each region. Consistently with previous studies (Mazza et al., 2020, Sønderskov et al., 2021), we expected that psychopathological symptoms and psychological well-being would covary with the intensity of the COVID-19 pandemic and the associated societal restrictions. Specifically, anxiety, depressive symptoms, posttraumatic symptoms, and obsessive-compulsive symptoms were expected to decrease from T0 and T1 and increase from T1 and T2, whereas psychological well-being was expected to increase from T0 to T1 and decrease from T1 to T2.
Secondly, the present study aimed to investigate potential risk and protective factors of psychopathological outcomes at T0, T1 and T2. In line with previous evidence (e. g. Amendola et al., 2020; Dubey et al., 2020; Guzi et al., 2020; Hagger et al., 2020; Lasalvia et al., 2020; Mazza et al., 2020) we hypothesized that age (lower or elder), gender (being females), being a healthcare worker, having ceased work, being concerned about contracting the virus and a high frequency of searching information about COVID-19 might act as risk factors for the increase of psychopathological symptoms and the decrease of psychological well-being at T0 and T2.
2. Methods
2.1. Participants and procedure
Data were collected from March 2020 to November 2020, resulting in an 8-month, three-wave, longitudinal, web-based survey of mental health outcomes in a sample of Italian people during the COVID-19 pandemic. At baseline, during the lockdown phase (T0; data collected from March 25th 2020 to April 1st 2020), we recruited 1258 participants aged between 18 and 70 years (Mage= 23.43, SDage= 6.45; 75.4% female). Of these, 56.6% (n = 712; Mage = 23.9, SDage = 6.70; 78.9% female) also completed the second survey at the beginning of phase 2, which coincided with the end of lockdown (T1, data collected from May 21st 2020 to June 9th 2020). Finally, 369 participants (Mage = 24.65, SDage = 7.20; 79.1% female) completed the third survey at T2 (data collected from November 24th 2020 to January 21st 2021), when there was a significant increase in the number of cases in Italy (the second wave of infection). The sample characteristics are shown in Table 1 .
Table 1.
Sample characteristics at T0, T1 and T2.
| T0 (n = 1258) | T1 (n = 712) | T1 (n = 369) | |
|---|---|---|---|
| Mean Age | 23.43 ± 6.45 | 23.90 ± 6.70 | 24.64 ± 7.20 |
| %Female | 75.4% | 78.9% | 79.1% |
| Geographical Area (Italy) | |||
| % North | 53.3% | 54.2% | 56.4% |
| % Center | 24.2% | 27.2% | 27.9% |
| % South | 22.5% | 18.5% | 15.7% |
| Sentimental status | |||
| % Single | 21.4% | 26.5% | 27.9% |
| % In a relationship | 67.5% | 60.1% | 12.2% |
| % Having a cohabiting partner | 6.5% | 8.8% | 48.8% |
| % Married | 3.7% | 3.8% | 9.8% |
| % Divorced | 0.7% | 0.6% | 1.4% |
| % Widowed | 0.1% | 0.1% | / |
| Occupation | |||
| % Students | 55.5% | 52.1% | 47.7% |
| % Working students | 5.5% | 16.4% | 19.2% |
| % Workers | 28.5% | 20.8% | 22.8% |
| % Healthcare workers | 2.3% | 2.2% | 3.8% |
| % Unoccupied | 8.1% | 8.4% | 6.0% |
| % Retired | 0.1% | / | 0.5% |
Participants were recruited through advertisements on social network groups, and they were informed that participation was voluntary and anonymous and that confidentiality was guaranteed. A web link directed the participants to the study website, and after giving their informed consent, a unique alphanumeric code was created for each participant to ensure that they paired the answers to the posttest anonymously. Then, demographic information, information about their experience with COVID-19 (e.g., worry, seeking information, knowing people who have contracted the virus), and self-report questionnaires were collected. The survey has a completation time of approximately 30 min. No remunerative reward was given. T0 participants were contacted by email to complete the survey at T1 and T2. An automatic reminder was send by email to minimize the risk of drop-out.
2.2. Measures
2.2.1. Information about COVID-19 experiences and the lockdown phase
Information about the participants’ COVID-19 experiences was collected at T0, T1 and T2; the participants were asked if they lived alone during the quarantine, if they had ceased working due to the COVID-19 pandemic, if they knew people who had been infected with the virus, and if they felt safe. Moreover, they were asked about their level of fear of contracting the virus, the frequency of searching for information regarding COVID-19 (general research, disease symptoms, and the number of infected and deceased people), their beliefs about whether COVID-19 can lead to death, their concerns about the situation in Italy, and, finally, the pleasantness of cohabitation. Moreover, at T1 and T2, the participants were asked if they experienced economic difficulties due to the pandemic period, and only at T2 was it required to declare if they lived in the “red zone”, which in Italy was considered the region at highest risk and with the most restrictions.
2.2.2. Anxiety symptoms
The Italian version (Sica and Ghisi, 2007) of the Beck Anxiety Inventory (BAI; Beck et al., 1988) was used to measure anxiety symptoms. The 21 items of this self-report measure rate a person's experiences over the past week on a Likert scale ranging from 0 (“Not at all”) to 3 (“Severely – it bothered me a lot”) and investigate the frequency of common symptoms of anxiety (e.g., an inability to relax, difficulty in breathing, nervousness). Higher scores indicate a higher level of anxiety symptoms (score range 0−63). The Italian BAI showed very good internal consistency (Sica and Ghisi, 2007). Cronbach's alphas for the current study were .92 (T0), .91 (T1) and .92 (T2).
2.2.3. Depressive symptoms
The Italian version (Sica and Ghisi, 2007) of the Beck Depression Inventory-II (BDI-II; Beck et al., 1996) was used to measure depressive symptoms. This self-report measure encompasses 21 items that measure the severity of depressive symptoms (e.g., sadness, a loss of pleasure, feelings of punishment) on a 4-point Likert scale. Higher scores indicate a higher severity of depression, with 17 considered as a cut-off score for clinical warning (score range 0−63). The Italian BAI showed good psychometric properties (Sica and Ghisi, 2007). Cronbach's alphas for the current study were .89 (T0), .92 (T1) and .92 (T2).
2.2.4. Obsessive-Compulsive symptoms
The Italian version (Melli et al., 2015) of the Dimensional Obsessive-Compulsive Scale (DOCS; Abramowitz et al., 2010) was used to assess obsessive-compulsive symptoms. The DOCS is a 20-item self-report measure that assesses four dimensions of OC symptoms: contamination, responsibility, unacceptable thoughts, and symmetry. All the answers are given on a four-point Likert scale ranging from 0 to 3. For each dimension, higher scores indicate the occurrence of more symptoms. The Italian DOCS showed good psychometric properties (Melli et al., 2014). Cronbach's alphas for the current study were .92 (T0), .93 (T1) and .93 (T2).
2.2.5. Posttraumatic Stress Disorder symptoms
The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Weathers et al., 2013 ) is a 20-item self-report measure used to assess posttraumatic stress disorder (PTSD) symptoms conceptualized within the four symptom clusters (intrusion; avoidance; cognition and emotions; hyperarousal) reported in the DSM-5 (American Psychiatric Association, 2013). Participants rated how much a problem described in the item statement bothered them over the past month using a 5-point Likert scale (0= not at all; 5= extremely). Item scores are summed to yield a total score ranging from 0 to 80. The PCL-5 appears to be an effective and reliable tool for screening PTSD symptoms (Brewin, 2005). Since an Italian version of the questionnaire was not available at the time of data collection, the Italian translation of the PCL-5 was obtained using a back-translation procedure. Cronbach's alphas for the current study were .94 (T0), .95 (T1) and .95 (T2).
2.2.6. Psychological well-being
The Italian version (De Sio et al., 2017) of the 5-item World Health Organization Five Well-Being Index (WHO-5; WHO, 1998) was used to measure participants’ psychological well-being. Each item is rated on a 6-point Likert scale (1= all the time; 6= at no time), with higher scores indicating a higher sense of well-being (score range 0−25). The Italian version (De Sio et al., 2017) of the WHO-5 showed good psychometric properties. Cronbach's alphas for the current study were .83 (T0), .88 (T1) and .89 (T2).
2.3. Statistical analysis
Descriptive statistics were calculated for the baseline, first wave and second wave data. The data collected at T0, T1 and T2 were compared pairwise by repeated-measures ANOVA and t-tests. A series of multiple regression analyses was performed to examine the potential risk factors and protective factors for the mental health outcomes. All analyses were performed using SPSS 23 statistical software (IBM Corp.).
3. Results
3.1. Descriptive statistics
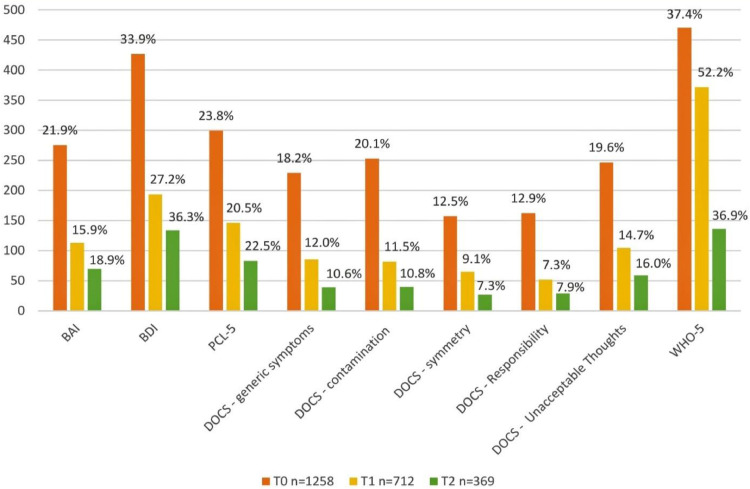
Descriptive statistics of information about the participants’ COVID-19 experiences at T0, T1 and T2 are presented in Table 2 , while those concerning anxiety, depressive symptoms, posttraumatic symptoms, obsessive-compulsive symptoms, and psychological well-being are shown in Fig. 1 .
Table 2.
Descriptive statistics concerning information about the participants’ COVID-19 experiences at T0, T1 and T2.
| T0 (n=1258) | T1 (n=712) | T2 (n=369) | |
|---|---|---|---|
| Living alone | |||
| yes | 4.4% | 5.1% | 4,90% |
| no | 95.6% | 94.9% | 95.1% |
| Having ceased to work | |||
| yes | 47.1% | 15.4% | 24.6% |
| no | 52.9% | 84.6% | 75.4% |
| Knowing people who had been infected | |||
| yes | 35.6% | 56.3% | 93.8% |
| no | 64.4% | 43.7% | 6.2% |
| Feeling safe | |||
| yes | 70.7% | 68.3% | 5.7% |
| no | 5.2% | 3.2% | 61.5% |
| not enough | 24.1% | 28.5% | 32.8% |
| Concern regarding contracting the virus | |||
| low (1-2) | 35.6% | 46.3% | 15.8% |
| medium (3) | 40.3% | 37.8% | 59.8% |
| high (4-5) | 24.1% | 15.8% | 24.4% |
| Frequency of searching information about COVID-19 | |||
| low (1-2) | 25.6% | 64.2% | 46.3% |
| medium (3) | 23.3% | 18.3% | 32.5% |
| high (4-5) | 51.2% | 17.5% | 21.1% |
| Worry for the Italian situation | |||
| low (1-2) | 1.5% | 7.3% | 2.7% |
| medium (3) | 16.1% | 32.3% | 22.0% |
| high (4-5) | 82.4% | 60.4% | 75.4% |
| Pleasantness of cohabitation | |||
| low (1-2) | 17.4% | 14.7% | 12.2% |
| medium (3) | 31.6% | 31.6% | 33.3% |
| high (4-5) | 51.8% | 53.7% | 54.5% |
| Economic issues at T1 and T2 | |||
| yes | / | 26.7% | 77.0% |
| no | / | 73.3% | 23.0% |
| Living in "Red zone" at T2 | |||
| yes | / | / | 45.5% |
| no | / | / | 66.7% |
Fig. 1.
Descriptive statistics of severe anxiety, depressive, posttraumatic, obsessive-compulsive symptoms, and low well-being at T0, T1 and T2.
Notes BAI = Back Anxiety Inventory; BDI = Beck Depression Inventory; PCL-5 = Posttraumatic Stress Disorder Checklist for DSM-5; DOCS = Dimensional Obsessive-Compulsive Scale; WHO-5 = World Health Organization Five Well-Being Index
3.2. Comparison of psychological health status between T0, T1, and T2
A repeated-measures ANOVA showed that the mean BAI, BDI, DOCS, PCL-5 and WHO-5 scores differed significantly across the three time points, as shown in Table 3 . Regarding anxiety, depressive symptoms, posttraumatic symptoms and psychological well-being, there was a statistically significant difference between T0 and T1 (BAI: t = 5.47, p <.001, Cohen's d = .18; BDI: t = 6.01, p <.001, Cohen's d = .18; PCL-5: t = 4.60, p<.001, Cohen's d = .14; WHO-5: t = -7.92, p <.001, Cohen's d = .32) and between T1 and T2 (BAI: t = -2.89, p = .004, Cohen's d = .23; BDI: t = -.17, p<.001, Cohen's d = .12; PCL-5: t = -3.30, p<.001, Cohen's d = .26; WHO-5: t = 5.72, p <.001, Cohen's d = .45), whereas there was no difference between T0 and T2.
Table 3.
Comparisons of anxiety, depressive, obsessive-compulsive, posttraumatic symptoms and psychological well-being between T0, T1 and T2.
| T0 March 2020 n = 1258 | T1 May 2020 n =712 | T2 November 2020n = 369 | ||||
|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | F | p | ηp2 | |
| Anxiety symptoms | 13.85 ± 10.37 | 12.14 ± 10.27 | 13.81 ± 10.81 | 4.196 | .016 | .027 |
| Depressive symptoms | 11.29 ± 9.03 | 9.65 ± 8.26 | 12.34 ± 9.44 | 11.443 | <.001 | .069 |
| Obsessive-Compulsive symptoms | 15.47 ± 10.60 | 13.90 ± 10.80 | 13.64 ± 10.37 | 3.789 | .024 | .024 |
| Posttraumatic Stress Disorder symptoms | 20.84 ± 16.02 | 17.95 ± 15.00 | 21.06 ± 15.81 | 6.325 | .002 | .040 |
| Psychological well-being | 11.01 ± 5.05 | 12.89 ± 4.95 | 10.60 ± 4.72 | 18.735 | <.001 | .108 |
Concerning obsessive-compulsive symptoms, there was a statistically significant difference between T0 and T1 (t= 6.19; p <.001; Cohen's d=.20) and T0 and T2 (t= 2.81; p=.006; Cohen's d=.22) but not between T1 and T2.
3.3. Predictors of psychopathological symptoms and psychological well-being at T0 and T2
A series of multiple regression analyses (Table 4 ) was performed to evaluate the ability of age, sex, living in northern Italy, being a health care worker, being in a relationship, living alone, having ceased to work due to the pandemic, being concerned about the possibility of contracting the virus, knowing people who have been infected, worrying about the situation in Italy, the frequency of searching for information about COVID-19, the perception of being safe and the pleasantness of cohabitation to predict anxiety, depressive symptoms, obsessive-compulsive symptoms, posttraumatic symptoms and psychological well-being, based on data collected at T0 and T2. After performing preliminary analyses to ensure that there was no violation of the assumptions of normality, linearity and multicollinearity, significant regression equations were found for T0 and T2.
Table 4.
Predictors of psychopathological symptoms and psychological well-being at T0 and T2.
| Criterion variables | The first survey (T0, March 2020 – lockdown phase) N=1258 | The third survey (T2, November 2020 – second wave of infection) N=369 | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety symptoms | Depressive symptoms | Obsessive-Compulsvie symptoms | Posttraumatic Stress Disorder symptoms | Psycholiiogical well-being | Anxiety symptoms | Depressive symptoms | Obsessive-Compulsvie symptoms | Posttraumatic Stress Disorder symptoms | Psychological well-being | |||||||||||
| β | t | β | t | β | t | β | t | β | t | β | t | β | t | β | t | β | t | β | t | |
| Age | -.17* | -2.12 | -.25* | -2.94 | .01 | .08 | -.17* | -2.01 | .04 | .41 | -.15* | -2.91 | -.14* | -2.72 | -.05 | -1.01 | -.14* | -2.57 | -.04 | -.80 |
| Female | .23* | 3.04 | .09 | 1.26 | .00 | .06 | .07 | .95 | -.15 | -1.90 | .20⁎⁎ | 4.10 | .11* | 2.29 | .05 | 1.08 | .13* | 2.53 | -.06 | -1.14 |
| Living in Northern Italy | .01 | .20 | -.12 | -1.62 | -.00 | -.02 | -.02 | -.28 | .11 | 1.41 | .02 | .53 | .00 | .08 | -.04 | -.75 | .03 | .72 | -.05 | -1.04 |
| Healthcare worker | -.13 | -1.69 | -.00 | -.02 | .00 | .02 | -.04 | -.51 | .01 | .19 | -.02 | -.31 | -.06 | -1.24 | -.02 | -.34 | -.01 | -.28 | .06 | 1.12 |
| Being in a relationship | -.03 | -.37 | -.16 | -1.89 | -.10 | -1.10 | -.09 | -1.00 | .13 | 1.46 | -.02 | -.37 | -.03 | -.64 | -.06 | -1.27 | -.09 | -1.80 | .12* | 2.33 |
| Living alone | .02 | .26 | .00 | -.00 | -.08 | -.92 | .03 | .41 | -.08 | -.88 | .06 | 1.17 | .01 | .28 | .02 | .38 | .01 | .26 | .02 | .36 |
| Having ceased to work | .04 | .52 | -.06 | -.79 | -.15 | -1.71 | -.08 | -1.04 | .05 | .66 | .12* | 2.67 | .16* | 3.40 | .13* | 2.76 | .11* | 2.33 | -.11* | -2.36 |
| Concern about contracting the virus | .27* | 3.26 | .05 | .68 | .18* | 1.99 | .05 | .58 | -.07 | -.76 | .01 | .13 | -.03 | -.58 | .09 | 1.64 | -.08 | -1.44 | .01 | .16 |
| Knowing people who have been infected with the virus | .13 | 1.76 | -.00 | -.04 | .09 | 1.14 | .08 | 1.10 | -.06 | -.76 | .03 | .61 | .03 | .76 | -.04 | -.76 | .05 | 1.07 | -.15* | -3.11 |
| Worry for the Italian situation | .06 | .82 | .15 | 1.89 | .13 | 1.51 | .12 | 1.53 | -.07 | -.81 | .16* | 3.19 | .16* | 3.24 | .08 | 1.68 | .12* | 2.27 | -.10* | -1.92 |
| Frequency of searching for information regarding COVID-19 | .17* | 2.30 | .07 | .95 | .10 | 1.24 | .23* | 2.97 | -.09 | -1.19 | .12* | 2.47 | .07 | 1.43 | .11* | 2.11 | .11* | 2.20 | -.04 | -.82 |
| Perception of being safe | -.07 | -.96 | -.00 | -.09 | -.15 | -1.81 | -.07 | -.85 | .11 | 1.31 | -.30⁎⁎ | -5.88 | -.27⁎⁎ | -5.29 | -.32⁎⁎ | -6.06 | -.31⁎⁎ | -5.72 | .22⁎⁎ | 4.25 |
| Pleasantness of cohabitation | -.18* | -2.50 | -.37⁎⁎ | -5.00 | -.06 | -.74 | -.31⁎⁎ | -4.18 | .30⁎⁎ | 3.86 | -.14* | -2.87 | -.27⁎⁎ | -5.70 | -.16* | -3.26 | -.19⁎⁎ | -3.77 | .32⁎⁎ | 6.51 |
p<.001
p<.05;
Concerning the predictors of anxiety symptoms, the model at T0 (F = 5.512, p < .001) predicted 33% of the variance. Anxiety symptoms were negatively predicted by age and the pleasantness of cohabitation and positively predicted by sex (female), concern about contracting the virus and the frequency of searching for information about COVID-19. At T2 (F = 12.148; p < .001; R2 = .32), age and the pleasantness of cohabitation still negatively predicted anxiety symptoms, as did the perception of being safe, while being female, having ceased to work due to the pandemic, worrying about the situation in Italy and the frequency of searching for information regarding COVID-19 positively predicted higher anxiety symptoms.
Regarding depressive symptoms, the model at T0 (F = 4.156, p<.001) predicted 27% of the variance. Age and the pleasantness of cohabitation negatively predicted high depressive symptoms. At T2, the model continued to be significant (F = 12.641, p<.001), with an R2 of.33, indicating that age, the perception of being safe and the pleasantness of cohabitation negatively predicted depressive symptoms, while being female, having ceased to work due to the pandemic and worrying about the situation in Italy positively predicted high depressive symptoms.
Obsessive and compulsive symptoms were positively predicted only by concerns about contracting the virus at T0 (F = 2.521; p <.05; R2 =.186), while at T2 (F = 10.570; p<.001; R2=.297), the perception of being safe and the pleasantness of cohabitation negatively predicted high obsessive-compulsive symptoms, whereas having ceased to work and the frequency of searching for information regarding COVID-19 positively predicted high obsessive-compulsive symptoms.
Age and the pleasantness of cohabitation negatively predicted posttraumatic symptoms at T0 (F = 4.106; p <.001; R2=.272). Age, the pleasantness of cohabitation and the perception of being safe negatively predicted posttraumatic symptoms at T2 (F = 9.631; p<.001; R2=.280), while being female, having ceased to work, worrying about the situation in Italy and the frequency of searching for information regarding COVID-19 positively predicted posttraumatic symptoms.
Psychological well-being was positively predicted by the pleasantness of cohabitation at T0 (F = 3.058; p <.05; R2 =.218). At T2 (F = 10.309; p<.001; R2=.29), it was negatively predicted by having ceased to work due to the pandemic, knowing people who had been infected with the virus and worrying about the situation in Italy, and it was positively predicted by being in a relationship, the perception of being safe and the pleasantness of cohabitation.
4. Discussion
The present study investigated the impact of COVID-19 on psychological health in a sample of Italian adults at three different points in the pandemic: the lockdown phase (T0, March 2020), the end of lockdown/beginning of the second phase (T1, May 2020) and the second wave of infection (T2, November 2020). Specifically, changes in the levels of anxiety, depressive symptoms, obsessive-compulsive symptoms, posttraumatic symptoms, and psychological well-being from T0 to T1 and from T1 to T2 were explored. We observed (i) a significant decrease in anxiety, depressive symptoms, posttraumatic symptoms and obsessive-compulsive symptoms and a significant increase in psychological well-being from March 2020 (T0, lockdown phase) to May 2020 (T1, end of lockdown); (ii) psychopathological symptoms (with the exception of obsessive-compulsive symptoms) significantly increased, and psychological well-being significantly decreased from May 2020 (T1, end of lockdown) to November 2020 (T2, second wave of infection); (iii) there were no changes between March 2020 (T0, lockdown phase) and November 2020 (T2, second wave of infection), except for obsessive compulsive symptoms, which significantly decreased. Consistent with previous studies (Mazza et al., 2020; Sønderskov et al., 2021), the current findings indicated that psychopathological symptoms and psychological well-being covaried with the intensity of the COVID-19 pandemic and the associated societal restrictions.
Previous studies using data collected during the lockdown phase in Italy showed high scores for anxiety, depression, and posttraumatic symptoms and low scores for psychological well-being (Di Blasi et al., 2021; Forte et al., 2020; Mazza et al., 2020; Rossi et al., 2020; Somma et al., 2020) during the first weeks of the pandemic. These results were also confirmed by the international literature (e.g., Krishnamoorthy et al., 2020; Wang et al., 2020), demonstrating that the pandemic crisis produced similar responses in the populations around the world. The reduction in psychological well-being and the increase in psychopathological symptoms observed in the current study, although not in line with a previous study conducted in a sample of Italian women (Di Blasi et al., 2021), are compatible with the development of the COVID-19 pandemic. Indeed, a second wave of infection and the adoption of new societal restrictions (i.e., the creation of different “zones” in the country based on the number of infected individuals) started in November 2020. Based on our data, by November 2020, the psychological health of our sample of Italian people had dropped to the level observed at the spring apex of the pandemic in March 2020. This result is consistent with the data collected in Danish (Sønderskov et al., 2021) and English (Creswell et al., 2021) populations.
In the current study, several demographic, psychological and COVID-19-related factors emerged as predictors of psychological health over the course of the ongoing pandemic. As hypothesized, being female and younger predicted psychopathological symptoms both during the lockdown phase (March 2020) and during the “second wave” of COVID-19 (November 2020). These results are in line with those previously reported regarding age and sex (female) being risk factors for mental health problems during the COVID-19 pandemic (e.g., Amendola et al., 2020; Di Blasi et al., 2021; Huang and Zhao, 2020; Rossi et al., 2020). Consistent with previous evidence (Cao et al., 2020; Lades et al., 2020; Somma et al., 2020), the frequency of searching for information about COVID-19 was positively correlated with psychopathological symptoms in both of the examined pandemic periods. Some “time-specific” predictors of psychological health emerged. Whereas concerns about contracting COVID-19 predicted (anxiety) symptoms during the lockdown, having ceased to work and the general preoccupation with the situation in Italy (e.g., national economic and health care consequences) emerged as relevant predictors of psychopathological symptoms and psychological well-being during the “second wave” of COVID-19. These latter results were previously confirmed by studies on the first wave of the pandemic (Cao et al., 2020; Mehulić and Kamenov, 2021; Rossi et al., 2020). Regarding protective factors, the pleasantness of cohabitation was negatively associated with all psychopathological symptoms and positively associated with psychological well-being, both during the lockdown phase and during the “second wave” of COVID-19. It is plausible to assume that the pleasantness of cohabitation could be linked to perceived social support, which emerged as a protective factor for depressive symptoms during the pandemic (Mariani et al., 2020). Finally, the perception of being safe was a protective factor for psychopathological symptoms and psychological well-being specifically during the “second wave” of COVID-19.
Contrary to our hypothesis and to what was previously reported (e.g., Vizheh et al., 2020; for a systematic review, see Vindegaard and Benros, 2020), our research did not find that being a health care worker predicted having psychopathological symptoms. However, this population was underrepresented in the current study as only 3% of our participants were health care workers.
4.1. Limitations and future research
To the best of our knowledge, this is the first three-wave longitudinal study investigating the effects of the COVID-19 pandemic on psychological health in a sample of Italian people. Nevertheless, there are some limitations. First, the high dropout rate and the inclusion of respondents who completed the questionnaire in all three data collection periods may have produced a selection/survivorship bias. The low response rate could be explained by the fact that participants did not receive any compensation for participating in the study. Moreover, the long period considered (10 months) and the length of the survey (30 mins) might have influenced the participation rate. Future studies might implement more retention strategies (see for example Teague et al., 2018) in order to avoid a high dropout rate. Second, most of the participants were females, young adults and students, which is not representative of the entire Italian population. Third, our data are based only on self-reported questionnaires and referred only to the first year of the COVID-19 pandemic. Further longitudinal studies involving other types of populations, such as health care workers, elderly individuals, and individuals with psychiatric difficulties, are needed.
4.2. Conclusion
Overall, our study reported a rather prolonged negative impact of the COVID-19 pandemic on psychological health and well-being in a general population, based on prospectively collected data. Several important risk factors and protective factors emerged, suggesting some general population-based interventions to reduce the negative mental health impacts of COVID-19. These include providing reliable COVID-19 information to alleviate anxiety and fear, limiting loneliness, and promoting alternative forms of social interactions to increase perceived social support. Digital interventions focused on enhancing effective coping strategies and reducing stress that also take into account the timing of the interventions (i.e., at the start, middle or plateau stages of the pandemic) could be promising.
In general, the current findings suggested that the measures adopted by governments to contrast the pandemic in different periods (e. g., lockdown, social distancing) might need to be accompanied by psychological intervention in order to contain the long-term psychological health costs. For instance, psychoeducation about the potential short and long term negative effects of pandemics on psychological well-being could be provided. Moreover, implementing empirically supported strategies to assist in managing stress and minimizing concomitant mental health problems should become a priority. For example, digital health strategies, especially mobile health technology, significantly support health care systems by promoting individuals’ self-surveillance, self-monitoring, high quality freely available resources, and self-efficacy (e.g., Fagherazzi et al., 2020). Additionally, information about the pandemic might be distressing for certain individuals because both the content of such information (i. e., number of infected, deaths, ICU admissions, etc.) and the high rate of fake news might contribute to increased anxiety and depressive symptoms (Moghanibashi-Mansourieh et al., 2020; Zhou et al., 2020). Helping individuals in choosing institutional/trusted sources for finding information and avoiding negative and fake news could be important to promote healthy behaviors (Banerjee et al., 2020). In this vein, Health Beliefs Model (Becker and Maiman, 1975)-based interventions could be particularly relevant since they mitigate behaviors influenced by perceived health threats which provoke anxiety and fear, reinforcing individuals’ perceived benefits and self-efficacy (e.g., Kim et al., 2012).
CRediT authorship contribution statement
Giulia Fioravanti: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Sara Bocci Benucci: Formal analysis, Writing – original draft. Alfonso Prostamo: Conceptualization, Investigation. Vanessa Banchi: Conceptualization, Investigation. Silvia Casale: Writing – review & editing, Supervision.
Declaration of Competing Interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Abramowitz J.S., Deacon B.J., Olatunji B.O., Wheaton M.G., Berman N.C., Losardo D., Timpano K.R., McGrath P.B., Riemann B.C., Adams T., Björgvinsson T., Storch E.A., Hale L.R. Assessment of obsessive-compulsive symptom dimensions: development and evaluation of the dimensional obsessive-compulsive scale. Psychol. Assess. 2010;(1):22. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]
- Amendola S., Spensieri V., Hengartner MP., Cerutti R. Mental health of Italian adults during COVID-19 pandemic. Br. J. Health Psychol. 2020;26(2):644–656. doi: 10.1111/bjhp.1250. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596.
- Amerio A., Lugo A., Stival C., Fanucchi T., Gorini G., Pacifici R., Odone A., Serafini G., Gallus S. COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J. Affect. Disord. 2021;292:398–404. doi: 10.1016/J.JAD.2021.05.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee D. The COVID-19 outbreak:crucial role the psychiatrists can play. Asian J. Psychiatry. 2020:50. doi: 10.1016/J.AJP.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; 1996. Manual for the Beck Depression Inventory–II. [Google Scholar]
- Becker M.H., Maiman L.A. Sociobehavioral determinants of compliance with health and medical care recommendations. Med. Care. 1975;13(1):10–24. doi: 10.1097/00005650-197501000-00002. [DOI] [PubMed] [Google Scholar]
- Benfante A., Tesio V., Di Tella M., Romeo A., Castelli L. From the first to the second wave of COVID-19: anxiety, de-pressive, and post-traumatic stress symptoms in the Italian population. Int. J. Environ. Res. Public Health. 2022;19:1239. doi: 10.3390/ijerph19031239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin C.R. Systematic review of screening instruments for adults at risk of PTSD. J. Trauma Stress. 2005;18(1):53–62. doi: 10.1002/JTS.20007. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet N. Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle R.P. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee SS., Barikar CM., Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico F., Sacco A., Fatebenefratelli A., Hospital F., Magnavita N. Coronavirus disease 2019: the second wave in Italy. J. Health Res. 2021;35(4):359–363. doi: 10.1108/JHR-10-2020-0514. [DOI] [Google Scholar]
- Creswell C., Shum A., Pearcey S., Skripkauskaite S., Patalay P., Waite P. Young people's mental health during the COVID-19 pandemic. Lancet Child Adolesc. Health. 2021;5(8):535–537. doi: 10.1016/S2352-4642(21)00177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Blasi M., Gullo S., Mancinelli E., Freda M.F., Esposito G., Gelo O.C.G., Lagetto G., Giordano C., Mazzeschi C., Pazzagli C., Salcuni S., lo Coco G. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. J. Affect. Disord. 2021;284:18–26. doi: 10.1016/J.JAD.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Blasi M., Albano G., Bassi G., Mancinelli E., Giordano C., Mazzeschi C., Pazzagli C., Salcuni S., lo Coco G., Gelo O.C.G., Lagetto G., Freda M.F., Esposito G., Caci B., Merenda A., Salerno L. Factors related to women's psychological distress during the COVID-19 pandemic: evidence from a two-wave longitudinal study. Int. J. Environ. Res. Public Health. 2021;18(21):11656. doi: 10.3390/IJERPH182111656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Sio S., Cedrone F., Sanità D., Ricci P., Corbosiero P., di Traglia M., Greco E., Stansfeld S. Quality of life in workers and stress: gender differences in exposure to psychosocial risks and perceived well-being. Biomed. Res. Int. 2017 doi: 10.1155/2017/7340781. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabet. Metab. Syndr. 2020;14(5):779–788. doi: 10.1016/J.DSX.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagherazzi G., Goetzinger C., Rashid M.A., Aguayo G.A., Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. J. Med. Internet Res. 2020;22:e19284. doi: 10.2196/19284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira L.N., Pereira L.N., da Fé Brás M., Ilchuk K. Quality of life under the COVID-19 quarantine. Qual. Life Res. 2021;30(5):1389–1405. doi: 10.1007/S11136-020-02724-X/TABLES/7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez A., Garcia-Alonso J., Royo-Pastor C., Garrell-Corbera I., Rengel-Chica J., et al. Effects of the economic crisis and social support on health-related quality of life: frst wave of a longitudinal study in Spain. Br. J. Gen. Pract. 2015;65(632):198–203. doi: 10.3399/bjgp15X684025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forte G., Favieri F., Tambelli R., Casagrande M. The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian population. J. Clin. Med. 2020;9(6):1802. doi: 10.3390/JCM9061802. 2020, Vol. 9, Page 1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C., Ausin B., Castellanos M., Saiz J., López-Gómez A., Ugidos C., Munoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guazzini A., Pesce A., Marotta L., Duradoni M. Through the second wave: analysis of the psychological and perceptive changes in the italian population during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2022;19:1635. doi: 10.3390/ijerph19031635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzi M., Pedraza P., Tijdens K. Publications Office of the European Union; 2020. Life dissatisfaction and anxiety in COVID-19 pandemic. [DOI] [Google Scholar]
- Hagger M.S., Keech J.J., Hamilton K. Managing stressduringthe coronavirus disease 2019 pandemic and beyond: reappraisal and mindset approaches. Stress Health. 2020;36(3):396–401. doi: 10.1002/smi.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/J.PSYCHRES.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., Sun T., Zheng P., An J. Mass quarantine and mental health during COVID-19: a meta-analysis. J. Affect. Disord. 2021;295:1335–1346. doi: 10.1016/J.JAD.2021.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.S., Ahn J., No J.K. Applying the health belief model to college students’ health behavior. Nutr. Res. Pract. 2012;6:551–558. doi: 10.4162/nrp.2012.6.6.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozina A., Peras I., Veldin M., Pivec T. The psychologicalresponse and perception of stress during the COVID-19 pandemic in Slovenia: threewave repeated cross-sectional study. Stress Health. 2022:1–11. doi: 10.1002/smi.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293 doi: 10.1016/J.PSYCHRES.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lades L.K., Laffan K., Daly M., Delaney L. Daily emotional well-being during the COVID-19 pandemic. Br. J. Health Psychol. 2020;25(4):902–911. doi: 10.1111/BJHP.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Bonetto C., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Amaddeo F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol. Psychiatr. Sci. 2020;30 doi: 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lixia W., Xiaoming X., Lei S., Su H., Wo W., Xin F., Jianmei C., Qi Z., Ming A., Li K. A cross-sectional study of the psychological status of 33,706 hospital workers at the late stage of the COVID-19 outbreak. J. Affect. Disord. 2022;297:156–168. doi: 10.1016/J.JAD.2021.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y.F., Li W., Deng H.B., Wang L., Wang Y., Wang P.H., Bo H.X., Cao J., Wang Y., Zhu L.Y., Yang Y., Cheung T., Ng C.H., Wu X., Xiang Y.T. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/J.JAD.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani R., Renzi A., di Trani M., Trabucchi G., Danskin K., Tambelli R. The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the coronavirus pandemic (COVID-19) lockdown. Front. Psychiatry. 2020;11:1195. doi: 10.3389/fpsyt.2020.587724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17(9):3165. doi: 10.3390/IJERPH17093165. 2020, Vol. 17, Page 3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson K.E., McAloney-Kocaman K., McGlinchey E., Faeth P., Armour C. Longitudinal analysis of the UK COVID-19 psychological wellbeing study: trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiatry Res. 2021;304 doi: 10.1016/j.psychres.2021.114138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medda E., Toccaceli V., Gigantesco A., Picardi A., Fagnani C., Stazi M.A. The COVID-19 pandemic inItaly: depressive symptoms immediately before and after the first lockdown. J. Affect. Disord. 2022;298:202–208. doi: 10.1016/j.jad.2021.10.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehulić J., Kamenov Ž. Mental health in affectionate, antagonistic, and ambivalent relationships during the COVID-19 pandemic: a latent profile analysis. Front. Psychol. 2021;12:3578. doi: 10.3389/FPSYG.2021.631615/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melli G., Chiorri C., Bulli F., Carraresi C., Stopani E., Abramowitz J. Factor congruence and psychometric properties of the Italian version of the dimensional obsessive-compulsive scale (DOCS) across non-clinical and clinical samples. J. Psychopathol. Behav. Assess. 2015;37(2) doi: 10.1007/s10862-014-9450-1. [DOI] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry. 2020;51 doi: 10.1016/J.AJP.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norr A.M., Capron D.W., Schmidt N.B. Medical information seeking: impact on riskfor anxiety psychopathology. J. Behav. Ther. Exp. Psychiatry. 2014;45(3):402–407. doi: 10.1016/J.JBTEP.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Pian W., Chi J., Ma F. The causes, impacts andcountermeasures of COVID-19 “Infodemic”: a systematic review using narrative synthesis. Inform. Process. Manag. 2021;(6):58. doi: 10.1016/J.IPM.2021.102713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestia D., Pozza A., Olcese M., Escelsior A., Dettore D., Amore M. The impact of theCOVID-19 pandemic on patients with OCD:effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020;291 doi: 10.1016/J.PSYCHRES.2020.113213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti E., di Pierro R., Perego G., Bottini M., Casini E., Ierardi E., Madeddu F., Mazzetti M., Riva Crugnola C., Taranto P., Mattei V.di. Short-term psychological consequences of the COVID-19 pandemic: results of the first wave of an ecological daily study in the Italian population. Psychiatry Res. 2021;305 doi: 10.1016/J.PSYCHRES.2021.114206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Xie1 B., Wu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gener. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., di Marco A., Rossi A., Siracusano A., di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and metaanalysis. Glob.Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica C., Ghisi M. In: Leading-edge psychological tests and testing research. Lange M.A., editor. Nova Science Publishers; 2007. The Italian versions of the beck anxiety inventory and the beck depression inventory-II: Psychometric properties and discriminant power; pp. 27–50. [Google Scholar]
- Somma A., Gialdi G., Krueger R.F., Markon K.E., Frau C., Lovallo S., Fossati A. Dysfunctional personality features, non-scientifically supported causal beliefs, and emotional problems during the first month of the COVID-19 pandemic in Italy. Personal. Indivi. Differ. 2020;165 doi: 10.1016/J.PAID.2020.110139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Vistisen H.T., Østergaard S.D. Variation in psychological well-being and symptoms of anxiety and depression during the COVID-19 pandemic: results from a three-wave panel survey. Acta Neuropsychiatr. 2021;33(3):156–159. doi: 10.1017/NEU.2020.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagliabue F., Galassi L., Mariani P. The “Pandemic” of Disinformation in COVID-19. SN Comprehen. Clin. Med. 2020;2(9):1287–1289. doi: 10.1007/S42399-020-00439-1. 2020 2:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasnim S., Hossain M., Mazumder H. Impact of rumors and misinformation on COVID-19 in social media. J. Prevent. Med. Public Health. 2020;53(3):171. doi: 10.3961/JPMPH.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teague S., Youssef G.J., Macdonald J.A., Sciberras E., Shatte A., Fuller-Tyszkiewicz M., Greenwood C., McIntosh J., Olsson C.A., Hutchinson D. Retention strategies in longitudinal cohort studies: a systematic review and meta-analysis. BMC Med. Res. Methods. 2018;18(1) doi: 10.1186/S12874-018-0586-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet Infectious Diseases The Covid-19 infodemic. Lancet Infect. Dis. 2020;20:875. doi: 10.1016/S1473-3099(20)30565-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinceti M., Filippini T., Rothman K.J., di Federico S., Orsini N. SARS-CoV-2 infection incidence during the first and second COVID-19 waves in Italy. Environ. Res. 2021;197 doi: 10.1016/J.ENVRES.2021.111097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinkers C.H., van Amelsvoort T., Bisson J.I., Branchi I., Cryan J.F., Domschke K., Howes O.D., Manchia M., Pinto L., de Quervain D., Schmidt M.v., van der Wee N.J.A. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020;35:12–16. doi: 10.1016/J.EURONEURO.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/J.BBI.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizheh M., Qorbani M., Arzaghi S.M., Muhidin S., Javanmard Z., Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J. Diabet. Metabol. Disord. 2020;19(2):1967–1978. doi: 10.1007/S40200-020-00643-9/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/IJERPH17051729. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. PTSD checklist for DSM-5 (PCL-5). Scale available from the national center for PTSD. http://www.ptsd.va.gov
- WHO Use of well-being measures in primary health care-the DepCare project health for all. Target. 1998;12:E60246. [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]