Abstract
Highly active and durable systemic therapies such as targeted therapy and immunotherapy can convert widespread metastatic disease into oligometastatic status, for which metastasis‐directed local intervention can control and potentially prolong survival. Radiation therapy is an effective therapeutic option for oligometastatic and oligoprogressive disease. Here, we present a case of induced oligometastasis and repeated oligoprogressive lung cancer in which more than 6 years of survival was achieved with a combination of immunotherapy and radiotherapy.
Keywords: immunotherapy, lung cancer, oligometastasis, oligoprogression, radiotherapy
The time line for the clinical course of the patient from diagnosis to last follow‐up with radiographic images

Metastasis‐directed local intervention can control and potentially prolong survival.
Radiation therapy is the effective therapeutic option for oligometastatic and oligoprogressive disease.
Here we present a case of induced oligometastasis and repeated oligoprogressive lung cancer in which more than 6 years of survival was achieved with a combination of immunotherapy and radiotherapy.
INTRODUCTION
As the more effective systemic treatments such as targeted therapy and immunotherapy are available for the treatment of non‐small cell lung cancer (NSCLC), widespread metastatic diseases at diagnosis can be converted to oligometastases (OM), known as induced‐OM. 1 Oligoprogression (OP), defined as limited numbers and/or sites of treatment failure, may also occur during highly active systemic treatment. Aggressive management for these oligometastatic and oligoprogressive NSCLCs should be considered due to potential longer progression‐free survival (PFS) and/or overall survival (OS). Here, we report a case of advanced NSCLC showing immunotherapy induced OM and repeated OPs successfully controlled with radiotherapy.
CASE REPORT
In August 2014, a 56‐year‐old male patient with 60 pack years of smoking presented with a history of a cough for 3 months. Chest x‐ray and chest computed tomography (CT) revealed a right upper lobe (RUL) mass and bilateral numerous lung nodules. After biopsy of the RUL mass by bronchoscopy and subsequent studies, he was diagnosed as stage IVa (cT2bN3M1a) advanced lung adenocarcinoma without driver mutation and negative programmed death‐ligand 1 expression. Systemic chemotherapy commenced with pemetrexed and cisplatin and continued until January 2018 when sixth line paclitaxel and carboplatin showed no more efficacy. During first to sixth lines of chemotherapies, the size of the primary lung mass on RUL and metastatic lung nodules decreased and increased repeatedly. On September 2017, he underwent gamma knife brain surgery for the newly developed single brain metastasis which had been detected on routine brain surveillance. Because all available chemotherapeutic agents had already been used, immunotherapy was the last treatment of choice for this patient. From the initial diagnosis of lung cancer to immediately before immunotherapy, he had a continuously good performance status (ECOG 1) and had been able to continue to work. After four cycles of nivolumab treatment, most metastatic lung nodules had markedly decreased in size or disappeared and the primary lung mass had slightly decreased. After 16 cycles of nivolumab treatment, most of the smaller metastatic nodules had disappeared but the primary mass in the RUL and metastatic mass in the left lower lobe (LLL) had increased. There was no evidence of extra‐thoracic metastasis and mediastinal lymphadenopathy on PET‐CT and brain magnetic resonance imaging (MRI). We considered this situation as induced‐OM and intensity modulated radiotherapy (IMRT) was performed on both masses. After 30th, 38th and 55th cycles of nivolumab treatment, repeated OPs occurred in the LUL as a single nodule on two occasions and lastly on the right third rib. These OPs were controlled successfully by IMRT. As of January 2021, the patient was still on nivolumab therapy without progression (only fibrotic scar changes were present at RT sites) (Figure 1).
FIGURE 1.
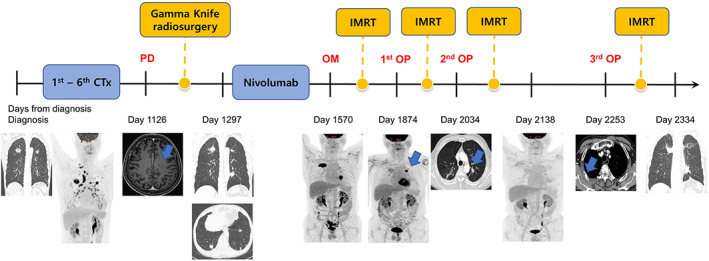
The timeline for the clinical course of the patient from diagnosis to last follow‐up with radiographic images. CTx, chemotherapy; IMRT, intensity modulated radiotherapy; OM, oligometastases; OP, oligoprogression; PD, progressive disease
DISCUSSION
The concept of OM status was proposed and popularized as a subset of patients with limited metastases became known and compared to those who had been given systemic treatment alone, had longer survival by definite treatment for these metastatic sites. 1 Some patients with initially widely metastatic disease could be oligometastatic after systemic therapy, so‐called induced OM. On the other hand, during highly effective systemic therapy such as targeted therapy, we often experience patients with progression only in limited sites. We define this situation as OP. Prevalence of OPs during immunotherapy has been reported to be 10%–20% when treatment of first‐line and more settings were all included, 2 relatively less common than targeted therapy. Having a relatively low response rate, immunotherapy shows a very effective and durable response for some patients. Through the basic studies and clinical trials, it has been shown that immunogenicity of tumors can change dynamically and are influenced by radiotherapy and chemotherapy. 3 Based on these concepts, combination strategies of immunotherapy with radiotherapy and chemotherapy have been tried with promising results, especially for patients with lung cancers. 3 , 4 In the case reported here, our patient showed a dramatic response to nivolumab which converted widespread metastatic to OM status. Initial PD‐L1 expression was negative, but this might have been changed by several lines of cytotoxic chemotherapy. In prospective clinical trials, OM treated with systemic plus consolidation therapy (surgery or radiotherapy) showed better PFS than systemic therapy alone. 4 Therefore, to extend PFS, radiotherapies were delivered to all (two) metastatic lesions and nivolumab treatment continued. 5 First OP occurred about 1 year after first radiotherapy and subsequent second, and third OPs were also successfully controlled by radiotherapy. Since single extrathoracic brain metastasis was treated by gamma knife surgery, no other extrathoracic metastasis was found during follow‐up. From this case, we were able to confirm that integration of radiotherapy with immunotherapy might augment the effectiveness of immunotherapy and repeated OPs could be controlled by repetitive radiotherapies. We also determined that even if repeated OPs occur, immunotherapy can be continued as long as OPs are controlled.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Lee HY, Kim SH, Lee HY, Lee Y‐M, Han JY, Cho H, et al. Successful treatment of induced oligometastasis and repeated oligoprogression of advanced lung adenocarcinoma with immunotherapy and radiotherapy. Thorac Cancer. 2022;13(13):1998–2000. 10.1111/1759-7714.14479
REFERENCES
- 1. Stephens SJ, Moravan MJ, Salama JK. Managing patients with oligometastatic non‐small‐cell lung cancer. J Oncol Pract. 2018;14:23–31. [DOI] [PubMed] [Google Scholar]
- 2. Rheinheimer S, Heussel CP, Mayer P, Gaissmaier L, Bozorgmehr F, Winter H, et al. Oligoprogressive non‐small‐cell lung cancer under treatment with PD‐(L)1 inhibitors. Cancer. 2020;12:1046. 10.3390/cancers12041046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lazzari C, Karachaliou N, Bulotta A, Viganó M, Mirabile A, Brioschi E, et al. Combination of immunotherapy with chemotherapy and radiotherapy in lung cancer: is this the beginning of the end for cancer? Ther Adv Med Oncol. 2018;10:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab after chemoradiotherapy in stage III non‐small‐cell lung cancer. N Engl J Med. 2017;377:1919–29. [DOI] [PubMed] [Google Scholar]
- 5. Pitroda SP, Chmura SJ, Weichselbaum RR. Integration of radiotherapy and immunotherapy for treatment of oligometastases. Lancet Oncol. 2019;20:e434–42. [DOI] [PubMed] [Google Scholar]


