Abstract
Background
We evaluated clinical features and risk factors for mortality in patients with haematological malignancies and COVID-19.
Methods
Retrospective, case–control (1:3) study in hospitalized patients with COVID-19. Cases were patients with haematological malignancies and COVID-19, controls had COVID-19 without haematological malignancies. Patients were matched for sex, age and time of hospitalization.
Results
Overall, 66 cases and 198 controls were included in the study. Cases had higher prior corticosteroid use, infection rates, thrombocytopenia and neutropenia and more likely received corticosteroids and antibiotics than controls. Cases had higher respiratory deterioration than controls (78.7% vs 65.5%, p = 0.04). Notably, 29% of cases developed respiratory worsening > 10 days after hospital admission, compared to only 5% in controls. Intensive Care Unit admission and mortality were higher in cases than in controls (27% vs 8%, p = 0.002, and 35% vs 10%, p < 0.001).
At multivariable analysis, having haematological malignancy [OR4.76, p < 0.001], chronic corticosteroid therapy [OR3.65, p = 0.004], prior infections [OR57.7, p = 0.006], thrombocytopenia [OR3.03, p < 0.001] and neutropenia [OR31.1, p = 0.001], low albumin levels [OR3.1, p = 0.001] and ≥ 10 days from hospital admission to respiratory worsening [OR3.3, p = 0.002] were independently associated with mortality.
In cases, neutropenia [OR3.1, p < 0.001], prior infections [OR7.7, p < 0.001], ≥ 10 days to respiratory worsening [OR4.1, p < 0.001], multiple myeloma [OR1.5, p = 0.044], the variation of the CT lung score during hospitalization [OR2.6, p = 0.006] and active treatment [OR 4.4, p < 0.001] all were associated with a worse outcome.
Conclusion
An underlying haematological malignancy was associated with a worse clinical outcome in COVID-19 patients. A prolonged clinical monitoring is needed, since respiratory worsening may occur later during hospitalization.
Supplementary Information
The online version contains supplementary material available at 10.1007/s15010-022-01869-w.
Keywords: Haematological malignancy, SARS-CoV2, COVID-19, Multiple myeloma, Non-Hodgkin lymphoma
Introduction
QuerySevere acute respiratory syndrome coronavirus-2 (SARS-CoV2) was first reported in late December 2019 and was recognized as the causative agent of an acute respiratory tract infection named Coronavirus Disease 2019 (COVID-19) [1]. Although most patients were asymptomatic or exhibited mild respiratory symptoms, approximately 8% may require hospitalization and 1% admission in Intensive Care Unit (ICU) [2]. In this context, patients suffering from haematological malignancies were considered an extremely vulnerable group, with a high risk of severe illness [3, 4] due to the prolonged and severe immunosuppression resulting from both chemo-immunotherapy and the underlying disease, which may weaken the immune system [5]. Indeed, the severe immunosuppression and the potential delay in the underlying disease’s treatment due to SARS-CoV2 diagnosis may affect the outcome of patients with haematological malignancies and COVID-19. On the other hand, these patients might also be protected from severe forms of COVID-19 thanks to the lower immune reaction during SARS-CoV2 infection [6, 7].
Although the relation between haematological malignancies and severity of SARS-CoV2 disease has been widely demonstrated, still no clear data on the risk factors of mortality in this special population exist. Furthermore, it is not fully elucidated whether there are differences in the clinical course of COVID-19 disease between patients with or without haematological malignancies.
As a matter of fact, so far the majority of studies have included mixed cohorts combining patients with haematological and solid cancer [3, 8–10]. Whereas, case–control studies, specifically matching subjects with and without haematological malignancies affected by SARS-CoV2, are still rare and include only a few patients [11, 12].
Based on these premises, the primary aim of this case–control study was to evaluate the clinical and prognostic features of patients with haematological malignancies and COVID-19. The secondary aim was to analyse risk factors for in-hospital mortality in this special population, with a particular emphasis on the respiratory worsening during hospitalization.
Materials and methods
From April 2020 to April 2021, a retrospective, single-center, case–control (1:3) study was performed on patients with COVID-19 hospitalized at Azienda Ospedaliero-Universitaria Policlinico Umberto I, Sapienza University of Rome. Cases were patients with haematological malignancies and COVID-19. Controls were patients with COVID-19 but without haematological malignancies. Cases and controls were matched for sex, age (decades) and time of hospitalization (Supplementary Fig. 1).
Inclusion criteria were: i) diagnosis of COVID-19 by means of molecular analyses, ii) hospitalization, and iii) age > 18 years. Patients with haematological disorders other than malignancy and age < 18 years were excluded from the study.
Nasopharyngeal swab samples were collected and SARS-CoV-2 RNA was detected using real-time RT-PCR assay (RealStar SARS-CoV2 RT-PCR, Altona Diagnostics).
For each subject, laboratory and clinical data at hospital admission, as well as treatment data and SARS-CoV-2 RNA time of detection, were collected and recorded anonymously in an electronic database. As for treatment data, antiviral therapy and the choice of using steroids were based on the national, regional and local guidelines available at the time [13, 14] and on clinical judgement, also following consultation with haematologists when appropriate.
In patients with haematological malignancies, the following variables were also collected: type and status of underlying disease, rate and type of active treatment, prior (30 d) chemotherapy, percentage of total lung parenchyma involvement during the disease by means of CT scan, CT score.
Definitions
Severity of infection was defined according to the guidelines available at the time of enrolment [15]. Individuals who tested positive for SARS-CoV2 but had no related symptoms were considered asymptomatic [15].
Use of corticosteroids within the previous 30 days included therapy with prednisone or its equivalent at a dose > 0.5 mg/kg/day for at least 1 month.
Prior infection and antibiotic therapy were defined as a diagnosis of infection and/or the receival of antibiotics in the 30 d prior to hospital admission, respectively.
Thrombocytopenia and neutropenia were defined according to the guidelines [16].
Status of haematological malignancy was defined as new diagnosis, refractory or relapsing disease, according to the guidelines of European Society for Medical Oncology [17].
Prior active treatment included the receival of chemotherapy or immunotherapy, or both, in the previous 90 days. Immunotherapy included the receival of monoclonal antibodies (rituximab, daratumumab, obinutuzumab) and tyrosine kinase inhibitors (imitinib, ibrutinib, ruxolitinib, venetoclax).
Worsening of respiratory conditions was based on the change of PaO2/FiO2 and was defined as: i) the need of supplementary oxygen therapy or ii) the need of increasing oxygen therapy supplementation in a patient with SARS-CoV2 infection for reasons directly related to the infection. A careful evaluation of causes of supplementary oxygen therapy for reasons other than SARS-CoV2 infection (i.e. cardiac failure, bacterial superinfections) was performed. In the case of doubt, a panel discussion was performed.
Time of viral shedding was defined as the number of days from the first viral detection by RT-PCR on nasopharyngeal specimen until the first of two consecutive negative results within 24 h [18].
To understand the dynamic of radiological findings in patients with haematological malignancies, we performed a CT scan at the diagnosis (CT1) and at the time of respiratory worsening (CT2). Two multidetector CT scanners (Somatom Sensation 16 and Somatom Sensation 64; Siemens Healthineers) were used. COVID-19 pneumonia was confirmed by means of the following CT parameters: ground glass opacity, crazy-paving pattern and pulmonary consolidation [19]. A semi-quantitative CT severity score to identify the percentage of lung parenchyma involved by the infective process was therefore calculated. In detail, each lung was divided into upper, middle and lower zones. For each of 3 zone, the extent of anatomic involvement was calculated as follows: 0, no involvement; 1 < 25% involvement; 2, 25–50% involvement; 3, 51–75% involvement; 4 > 75% involvement. The resulting global CT score was the sum of each individual score, ranging from 0 to 24 [20].
The study was approved by the local Ethics Committee (ID Prot. 109/2020).
Statistical analyses
Continuous data were expressed as mean with Standard Deviation (± SD) and categorical data were summarized as number of observations (n) and percentages (%). Differences between groups were evaluated with unpaired T test; difference between proportions was calculated by Chi-square test. Binary logistic regression analysis was used to identify the demographic characteristics and the examined risk factors. Factors with a univariate value of p < 0.05 were included in a stepwise multivariate logistic regression analysis. Missing data for each variable were excluded from the denominator. Univariable analysis was used to identify risk factors for haematological or non-haematological and predictors of all cause 30 day mortality. Baseline predictors possibly associated with the outcome at univariable comparison were considered for multivariable logistic regression to estimate adjusted Odds Ratios (ORs) and 95% Confidence Intervals (95% CI) for the risk factors including the confounding factors (i.e., age, gender). A stepwise backward selection approach was used to select the predictors to include in the final multivariate model. Survival was analysed by Kaplan–Meier curves and the statistical significance of the differences between the two groups was assessed using the log-rank test. Statistical analyses were performed using statistical Program for the Social Sciences (SPSS, version 22, SPSS Inc. Chicago IL, USA) software package.
Results
A total of 264 patients were included in the study (66 cases and 198 controls) (Supplementary Fig. 1). General features of the study population are shown in Table 1. Age, gender distribution and period of hospitalization did not differ between cases and controls, reflecting the correctness of the match. Likewise, infection severity and the PaO2/FiO2 at hospital admission were similar between cases and controls [(asymptomatic 4% vs 6%, p = 0.438, moderate infection 64% vs 64%, p = 0.904, severe infection 27% vs 29%, p = 0.796, critical illness 5% vs 6%, p = 0.619, respectively), 357.0 ± 102.1 vs 352.4 ± 101.0, p = 0.750]. Compared to controls, cases had a higher rate of chronic corticosteroids use and infections in the previous 30 d (39% vs 10%, p < 0.001 and 21% vs 3%, p = 0.001, respectively), as well as higher percentage of thrombocytopenia (39% vs 18%, p = 0.002), neutropenia (14% vs 1%, p = 0.003) and lower albumin levels (35.6 ± 6.7 vs 37.4 ± 5.5 g/dL, p = 0.003). C-reactive protein values did not differ between cases and controls (6.57 ± 8.41 vs 7.06 ± 7.52 mg/dL, p = 0.65).
Table 1.
General features of study population
| Cases (N = 66) |
Controls (N = 198) |
p value | |
|---|---|---|---|
| Demographics | |||
| Gender (Female), n (%) | 32 (48) | 96 (48) | 1.000 |
| Age, mean (SD) | 62.14 (± 15.37) | 61.28 (± 14.4) | 0.697 |
| Steroids in the last 30 days before admission, n (%) | 26 (39) | 19 (10) | < 0.001 |
| Infection in the last 30 days before admission, n (%) | 14 (21) | 5 (3) | 0.001 |
| Antibiotic therapy in the last 30 days (excluded prophylaxis), n (%) | 22 (33) | 69 (35) | 0.883 |
| Antibiotic prophylaxis therapy, n (%) | 24 (36) | 0 (0) | < 0.001 |
| Days of hospitalization, mean (SD) | 31.79 (± 28.04) | 19.16 (± 13.4) | 0.001 |
| Days from symptoms onset to hospitalization, mean (SD) | 5.48 (± 9.03) | 6.72 (± 6.02) | 0.310 |
| Complete vaccination for SARS-CoV-2, n (%) | 1 (1.5) | 1 (0.5) | 0.9 |
| Comorbidities, n (%) | |||
| Hypertension | 23 (35) | 93 (47) | 0.082 |
| Coronary artery disease | 14 (21) | 18 (9) | 0.029 |
| Diabetes | 9 (14) | 33 (17) | 0.547 |
| Chronic obstructive pulmonary disease | 4 (6) | 17 (9) | 0.481 |
| Chronic renal failure | 6 (9) | 10 (5) | 0.302 |
| Disease severity at the admission, n (%) | |||
| Moderate | 42 (64) | 127 (64) | 0.904 |
| Severe | 18 (27) | 57 (29) | 0.796 |
| Critical | 3 (5) | 12 (6) | 0.619 |
| Pneumonia | 55 (83) | 143 (72) | 0.169 |
| Symptoms at the admission, n (%) | |||
| Dyspnea | 26 (39) | 116 (59) | 0.007 |
| Cough | 24 (36) | 100 (51) | 0.044 |
| Asthenia | 28 (42) | 54 (27) | 0.197 |
| Anosmia/ageusia | 4 (6) | 24 (12) | 0.109 |
| Fever | 46 (70) | 159 (80) | 0.099 |
| Conjunctivitis | 2 (3) | 12 (6) | 0.267 |
| Other* | 1 (2) | 0 (0) | 0.322 |
| Asymptomatic | 4 (6) | 7 (4) | 0.438 |
| Respiratory features at the admission, mean (SD) | |||
| SpO2 | 95.6 (± 5.2) | 95.3 (± 3.2) | 0.680 |
| PO2/FiO2 | 357.0 (± 102.1) | 352.4 (± 101) | 0.750 |
| FiO2 | 24.6 (± 8.5) | 24.2 (± 9.3) | 0.737 |
| Laboratory findings at the admission, mean (SD) | |||
| Haemoglobin, g/dl | 11.4 (± 2.0) | 13.4 (± 2.1) | < 0.001 |
| White Blood Cells, × 10˄6/L | 8761.4 (± 10,816.8) | 7762.7 (± 9170.8) | 0.502 |
| Neutrophils, × 10˄6/L | 5697.8 (± 7252.7) | 5610.8 (± 3740.4) | 0.926 |
| Lymphocytes, × 10˄6/L | 2209.4 (± 6128.7) | 1043.0 (± 522.5) | 0.127 |
| Monocytes, × 10˄6/L | 345.5 (± 385.8) | 369.2 (± 194.56) | 0.633 |
| Platelets, × 10˄9/L | 172.6 (± 114.4) | 218.8 (± 830.2) | 0.003 |
| Thrombocytopenia (< 150 × 10˄9/L), n (%) | 26 (± 39) | 35 (± 18) | 0.002 |
| Neutropenia (< 500 × 10˄9/L), n (%) | 9 (± 14) | 1 (± 1) | 0.003 |
| Creatinin, mg/dl | 1.1 (± 1.3) | 1.4 (± 2.3) | 0.318 |
| Albumin, g/dl | 35.6 (± 6.7) | 37.4 (± 5.5) | 0.003 |
| D-dimer, µg/L | 1229.2 (± 1200.3) | 947.7 (± 994) | 0.093 |
| C-Reactive Protein, mg/dL | 6.574 (± 8.417) | 7.062 (± 7.522) | 0.650 |
| Ferritin, µg/L | 1472.2 (± 1903.3) | 752.3 (± 794.1) | 0.008 |
| LDH, U/L | 341.4 (± 160.3) | 311.5 (± 133.1) | 0.174 |
| Procalcitonin, ng/ml | 0.3 (± 0.5) | 0.9 (± 3) | 0.117 |
| Features at the respiratory worsening** | |||
| Worsening during hospitalization, n (%) | 52 (78.7) | 129 (65.5) | 0.04 |
| FiO2 mean (SD) | 39.3 (± 22.1) | 59.8 (± 23.7) | < 0.001 |
| PO2/FiO2, mean (SD) | 259.2 (± 115.8) | 208.7 (± 82.7) | 0.003 |
| Days from symptoms onset to worsening, mean (SD) | 13.20 (± 11.69) | 9.45 (± 5.38) | 0.041 |
| Days from SARS-CoV2 diagnosis to worsening, mean (SD) | 11.63 (± 13.69) | 5.69 (± 4.4) | 0.006 |
| Days from admission to worsening, mean (SD) | 12.3 (± 12.3) | 3.3 (± 3.1) | 0.001 |
| Days from thrombocytopenia to worsening, mean (SD) | 5.7 (± 10.4) | 3.0 (± 2.3) | 0.119 |
| Days from neutropenia to worsening, mean (SD) | 1.2 (± 5.2) | 1.2 (± 5.5) | 0.897 |
| Radiological features, mean (SD) | |||
| Percentage of total lung parenchyma involvement | 39 (26.3) | NA | – |
| Total CT score | 6 (6.2) | NA | – |
| Percentage of lung parenchyma involvement at CT1 | 22.58 (22.19) | NA | – |
| CT score at CT1 | 5.49 (5.55) | NA | – |
| Percentage of lung parenchyma involvement at CT2 | 36.31 (24.55) | NA | – |
| CT score at CT2 | 8.71 (6.02) | NA | – |
| Therapy, n (%) | |||
| Remdesivir | 31 (47) | 79 (40) | 0.250 |
| Enoxaparin | 48 (73) | 161 (81) | 0.234 |
| Corticosteroids | 60 (91) | 145 (73) | < 0.001 |
| Days of corticosteroids | 18.1 (22.9) | 8.1 (4.3) | < 0.001 |
| Baricitinib | 1 (2) | 0 (0) | 0.321 |
| Convalescent plasma | 8 (12) | 0 (0) | 0.004 |
| Antibiotics | 55 (83) | 128 (65) | < 0.001 |
| Outcomes | |||
| Intensive Care Unit admission, n (%) | 18 (27) | 16 (8) | 0.002 |
| In-hospital mortality, n (%) | 23 (35) | 20 (10) | < 0.001 |
| Days of viral shedding, mean (SD) | 35.4 (± 23.4) | 19.4 (± 10.2) | 0.010 |
| Secondary infections, n (%) | 26 (39) | 58 (29) | 0.137 |
| MDRO colonization | 1 (2) | 2 (1) | 0.912 |
| Opportunistic infections | 8 (12) | 0 (0) | 0.004 |
*other include headache, diarrhea and pharyngodynia; **respiratory worsening was defined as: i) the need of supplementary oxygen therapy or ii) the need of increasing oxygen therapy supplementation in a patient with SARS-CoV2 infection for reasons directly related to the infection. A careful evaluation of causes of supplementary oxygen therapy for reasons other than SARS-CoV2 infection (i.e. cardiac failure, bacterial superinfections) was performed. In the case of doubt, a panel discussion was performed. MDRO Multidrug resistant organisms.
Amongst cases, non-Hodgkin lymphoma (NHL) was observed in 27 (41%) of the subjects, followed by multiple myeloma (9, 14%), acute myeloid leukemia (7, 11%), chronic lymphocytic leukemia (7, 11%) and acute lymphocytic leukemia (5, 8%). Fifteen subjects (23%) have received a new diagnosis of haematological malignancy in the last months and, therefore, have not yet started or concluded treatment for the underlying disease, 34 (52%) were in complete or partial remission, 12 (18%) were suffering a relapsing or refractory disease, while 4 (6.1%) still had a not defined disease status. Prior (90 d) active treatment was given in 36 subjects (54.5%) [chemotherapy, n = 17, immunotherapy, n = 9, chemotherapy + immunotherapy, n = 10] and, amongst them, 12 (18%) had received recent (30 d) chemotherapy. Only four patients (6%) had a history of allogeneic stem cell transplantation (Supplementary Table 1).
Concerning the treatment of SARS-CoV2 infection, no differences emerged regarding the use of remdesivir and enoxaparin between cases and controls (47% vs 40%, p = 0.250 and 73% vs 81%, p = 0.234, respectively). In contrast, corticosteroid and antimicrobial therapies were significantly more frequent in cases than in controls (91% vs 73%, p < 0.001 and 83% vs 65%, p < 0.001, respectively). Of note, also the duration of corticosteroids treatment was longer in patients with haematological malignancies (18.1 ± 22.9 vs 8.1 ± 4.3 days, p < 0.001).
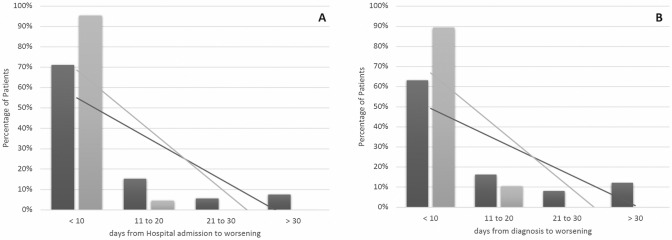
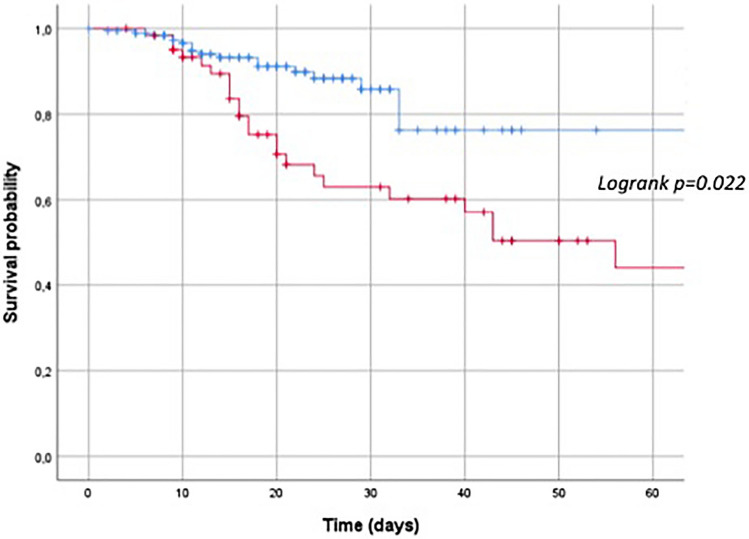
Super-infection rate and colonization by multi-drug resistant pathogens were similar in the two groups, whereas, as expected, opportunistic infections more frequently affected the haematological ones (p = 0.004). Furthermore, cases had a significantly longer duration of hospitalization (31.79 ± 28.04 vs 19.16 ± 13.39 days, p = 0.001) as well as a longer duration of viral shedding (35.4 ± 23.4 vs 19.4 ± 10.2 days, p = 0.010) than controls. Compared to controls, cases experienced higher rates of respiratory deterioration (78.7% vs 65.5%, p = 0.04). Furthermore, the time from symptoms onset, hospital admission and SARS-CoV2 diagnosis to respiratory worsening was significantly longer in cases [13.20 ± 11.69 vs 9.45 ± 5.38 days (p = 0.041), 12.3 ± 12.3 vs 3.3 ± 3.1 days (p = 0.001) and 11.63 ± 13.69 vs 5.69 ± 4.39 days (p = 0.006), respectively], leading to a delayed respiratory deterioration in cases compared to controls. As shown in Fig. 1, 29% of cases developed respiratory worsening more than 10 days after hospital admission, compared to 5% in the control group (Fig. 1, Panel A); likewise, 37% of cases worsened more than 10 days after SARS-CoV2 diagnosis, compared to 11% of controls (Fig. 1, Panel B). Cases had higher rates of ICU admission and in-hospital mortality as compared to controls: 27% vs 8%, (p = 0.002) and 35% vs 10%, (p < 0.001), respectively (Fig. 2).
Fig. 1.
Differences in the respiratory worsening between cases (black column) and controls (grey column). Panel A Differences in the days from hospital admission to respiratory worsening. Panel B Differences in the days from SARS-CoV-2 infection diagnosis to respiratory worsening
Fig. 2.
Cumulative proportion of mortality rate between patients with haematological malignancies. Cases: red line; controls: blue line
At multivariable analysis, having an haematological malignancy (i.e. belonging to the case group) [OR 4.76 (2.4–9.4), p < 0.001], thrombocytopenia at admission [OR 3.03 (1.6–5.6), p < 0.001], neutropenia at admission [OR 31.1 (3.86–250.7), p = 0.001], reduced level of serum albumin [OR 3.1 (2.1–6.6), p = 0.001], chronic corticosteroid use [OR 3.65 (1.49–8.96), p = 0.004], prior infection [OR 57.7 (3.2–1014.4), p = 0.006], low PaO2/FiO2 ratio at the time of respiratory worsening [OR 2.2 (1.3–10.4), p = 0.022] and a longer time to respiratory deterioration [OR 3.3 (2–12.4), p = 0.002] were independent risk factors for in-hospital mortality (Table 2).
Table 2.
Multivariable analysis on independent risk factors for in-hospital mortality in the whole study population
| ORs (95%CI) | P value | |
|---|---|---|
| Haematological malignancy | 4.76 (2.4–9.4) | < 0.001 |
| Thrombocytopenia at hospital admission1 | 3.03 (1.6–5.6) | < 0.001 |
| Neutropenia at hospital admission2 | 31.1 (3.86–250.7) | 0.001 |
| Low albumin at hospital admission3 | 3.1 (2.1–6.6) | 0.001 |
| Days from admission to respiratory worsening* (> 10d) | 3.3 (2–12.4) | 0.002 |
| Corticosteroids treatment | 3.65 (1.49–8.96) | 0.004 |
| Prior (30-d) infection | 57.7 (3.2–1014.4) | 0.006 |
| PO2/FiO2 at respiratory worsening* (< 250) | 2.2 (1.3–10.4) | 0.022 |
1Thrombocytopenia was defined as platelets count < 150 × 10˄9/L; 2Neutropenia was defined as polymorphonuclear leukocytes count < 500 × 10˄9/L; 3level of serum albumin < 3.5 g/dl. *respiratory worsening was defined as: i) the need of supplementary oxygen therapy or ii) the need of increasing oxygen therapy supplementation in a patient with SARS-CoV2 infection for reasons directly related to the infection. A careful evaluation of causes of supplementary oxygen therapy for reasons other than SARS-CoV2 infection (i.e. cardiac failure, bacterial superinfections) was performed. In the case of doubt, a panel discussion was performed
As shown in Table 3, independent risk factors for mortality in patients with haematological malignancies were neutropenia at hospital admission [OR 3.1 (2.9–270), p < 0.001], prior infection [OR 7.7 (3.2–112), p < 0.001], a longer time to respiratory deterioration [OR 4.1 (2.2–12.4), p < 0.001], active treatment [OR 4.4 (1.5–22.3), p < 0.001], multiple myeloma [OR 1.5 (1.1–3.3), p = 0.044], the variation of the total lung parenchyma involvement (CT1-CT2) [OR 2.6 (1.4–4.8), p = 0.004] and the variation of the CT lung score during hospitalization [OR 2.6 (1.2–12.2), p = 0.006].
Table 3.
Analysis of risk factors for in-hospital mortality in patients with haematological malignancies
| ORs (CIs 95%) | P value | |
|---|---|---|
| Thrombocytopenia at hospital admission1 | 1.2 (0.8–7.6) | 0.212 |
| Neutropenia at hospital admission2 | 3.1 (2.9–270) | < 0.001 |
| Low albumin at hospital admission3 | 1.4 (0.9–6.6) | 0.086 |
| Days from admission to respiratory worsening*(> 10d) | 4.1 (2.2–12.4) | < 0.001 |
| Corticosteroids | 1.7 (0.88–9.6) | 0.154 |
| Prior (30 d) infections6 | 7.7 (3.2–112) | < 0.001 |
| PO2/FiO2 at respiratory worsening* (< 250) | 1.2 (0.7–7.2) | 0.082 |
| Days from SARS-CoV-2 diagnosis to respiratory worsening (> 10-d) | 2.8 (1.4–22.1) | 0.014 |
| Percentage of total lung parenchyma involvement variation (CT1-CT2) | 2.6 (1.4–4.8) | 0.004 |
| Total CT score variation (CT1-CT2) | 2.4 (1.2–12.2) | 0.006 |
| Active treatment in the last 90 days | 4.4 (1.5–22.3) | < 0.001 |
| Multiple myeloma | 1.5 (1.1–3.3) | 0.044 |
1Thrombocytopenia was defined as platelets count < 150 × 10˄9/L; 2Neutropenia was defined as polymorphonuclear leukocytes count < 500 × 10˄9/L; 3level of serum albumin < 3.5 g/dl. *respiratory worsening was defined as: i) the need of supplementary oxygen therapy or ii) the need of increasing oxygen therapy supplementation in a patient with SARS-CoV2 infection for reasons directly related to the infection. A careful evaluation of causes of supplementary oxygen therapy for reasons other than SARS-CoV2 infection (i.e. cardiac failure, bacterial superinfections) was performed. In the case of doubt, a panel discussion was performed
In patients under active treatment, those receiving only immunotherapy (n = 9) had a mortality rate of 11.2% (1/9), compared to 29.4% (5/17) and 30% (3/10) of chemotherapy only and chemotherapy + immunotherapy, respectively.
Active treatment [OR 3.2 (1.8–12.3), p < 0.001], the variation of the CT lung score during hospitalization [OR 1.4 (1.1–8.2), p < 0.001], the variation of the total lung parenchyma involvement (CT1-CT2) [OR 1.6 (1.2–6.8), p < 0.001] and non-Hodgkin lymphoma [OR 1.4 (1.1–10.3), p = 0.011] were associated with in-hospital development of respiratory deterioration in cases (Supplementary Table2).
Discussion
Our data support previous observations that, amongst patients with COVID-19, those with haematological malignancies have higher mortality and ICU admission rates than subjects without malignancies [3, 11, 21–24]. Furthermore, they have increased risk in the presence of neutropenia at hospital admission, prior infection, active chemotherapy treatment and multiple myeloma [4, 8].
Nevertheless, in our opinion, the most interesting observation of this report was that i) haematological patients experienced a higher rate of respiratory deterioration than controls, ii) that this complication occurred later during the disease and, notably, iii) that the longer time to respiratory deterioration together with the increase of the CT lung score during hospitalization represented independent risk factors for mortality.
To point out the different clinical course between the two groups, we analysed the PaO2/FiO2 ratio at the time of worsening and we found that haematological patients experienced a higher rate of worsening than controls, although the PaO2/FiO2 ratio at the time of deterioration was still higher than in subjects without malignancies, apparently in contrast with the worse observed outcome. Furthermore, deterioration occurred more than 10 days after hospital admission in 29% of cases and only in 5% of controls. Being a novel aspect of the infection’s clinical course, the finding that haematological patients experienced a delayed respiratory worsening still has no clear explanation. Indeed, on one hand the immunocompromised status may lead the virus to replicate and to persist for a longer time; on the other hand, the immune response to the viral infection is delayed [12, 22, 25]. It may also be speculated that, as far as the restoration of the immune system occurs, for instance after chemotherapy-induced amelioration of the haematological disease, patients experience an excessive inflammatory response, which, eventually, is responsible for the clinical observed deterioration.
Another interesting finding of the present study was the correlation between the respiratory worsening and the radiology pattern in patients with haematological malignancies [26]. Although CT severity score has been shown to be a predictor of death in patients with COVID-19 pneumonia [27, 28], very few data are present regarding the role of this radiological parameter in patients with haematological malignancies. In this special context, we showed that not the CT score itself but its change during hospitalization was predictive of worse outcomes in haematological patients and, therefore, it may be used as a feature of clinical worsening.
Corticosteroids use and duration of treatment were significantly higher in cases than in controls, suggesting that the immune system of this special population is not only affected by the malignancy itself but also by its treatment. Likewise, cases had a higher rate of hypoalbuminemia at hospital admission than controls, confirming its prognostic role for mortality, prolonged viral shedding and coagulopathy during COVID-19 pandemic [18, 29–31] as well as for morbidity and mortality in several malignancies, including the haematological ones [32, 33].
Patients with haematological malignancies often experience prolonged shedding of viral RNA from the upper respiratory tract. In line with this, we showed that duration of viral positivity was significantly longer in patients with haematological malignancies than those without. With the continuous emergence of new variants, this phenomenon may be of significant concern, since it seems to contribute to the selection of sequence SARS-CoV-2 variants within the same host [34–36].
Our study has several limitations. First, its retrospective and single-centre nature. Second, we could not establish with certainty whether the diagnosis of SARS-CoV2 infection would delay the treatment of the haematological malignancy. This leads to a possible additional reason explaining the observed high mortality. Furthermore, groups were not perfectly comparable with regard to therapy; for instance, corticosteroids were used more in cases than in controls because of the haematological disease, even if not indicated for the treatment of COVID-19. Nevertheless, to reduce the possible bias of subjects’ selection, such as the different pandemic waves, we performed a strict match for age, sex and period of hospitalization. The level of the inflammatory marker IL-6 was not systematically measured at hospital admission in all the patients and, therefore, we could not evaluate whether it would have an influence on the observed different clinical course of infection between cases and controls. The low absolute number of haematological patients receiving only immunotherapy did not allow us to perform subgroup analyses for the outcome. At last, we enrolled patients before the onset of SARS-CoV-2 vaccination and/or the introduction of monoclonal antibodies in the clinical practice and therefore our findings could not lead to a generalization of the results. Notwithstanding, we were able to describe the singular clinical course of the infection in this special population and our results may represent the starting point for additional studies evaluating if, and how, the course of the disease has changed after the introduction of vaccination or monoclonal antibodies.
In conclusion, an underlying haematological malignancy was associated with a worse clinical outcome in our COVID-19 patients. Furthermore, haematological patients experienced a peculiar clinical course of the infection. This consisted in a higher rate of worsening and, above all, in a longer time to respiratory deterioration compared to non-haematological ones, which independently predicts mortality. Therefore, a careful and prolonged clinical monitoring is needed in this special population.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Authors thank all the nursing staff for their assistance to patients with COVID-19. Part of this work has been accepted as oral presentation at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (Lisbon, 23–26 April 2022).
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. Authors did not receive funding or grant support.
Data availability and materials
All data relevant to the study are included in the article or uploaded as supplementary information and are available from the corresponding author upon request.
Declarations
Conflict of interest
Authors declare no conflict of interest.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local Institutional Review Board.
Footnotes
The original online version of this article was revised: The given and family names of all authors were incorrectly structured. The corrected author list is given above.
Change history
7/28/2022
A Correction to this paper has been published: 10.1007/s15010-022-01892-x
References
- 1.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020, last access on 19 April 2022
- 2.European Centre for Disease Prevention and Control https://www.ecdc.europa.eu/en/covid-19/latest-evidence/clinical, last access on 19 April 2022
- 3.El-Sharkawi, et al. Haematological cancers and the risk of severe COVID-19: exploration and critical evaluation of the evidence to date. Br J Haematol. 2020;190:336–345. doi: 10.1111/bjh.16956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Passamonti F, Cattaneo C, Arcaini L, et al. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020;7:e737–e745. doi: 10.1016/S2352-3026(20)30251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.García-Suárez J, et al. Impact of hematologic malignancy and type of cancer therapy on COVID-19 severity and mortality: lessons from a large population-based registry study. J Hematol Oncol. 2020;13:133. doi: 10.1186/s13045-020-00970-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thibaud S, Tremblay D, Bhalla S, Zimmerman B, Sigel K, Gabrilove J. 2020 Protective role of Bruton tyrosine kinase inhibitors in patients with chronic lymphocytic leukaemia and COVID-19. Br J Haematol. 2020;190:e73–e76. doi: 10.1111/bjh.16863.Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Treon SP, Castillo JJ, Skarbnik AP, et al. The BTK inhibitor ibrutinib may protect against pulmonary injury in COVID-19-infected patients. Blood. 2020;135:1912–1915. doi: 10.1182/blood.2020006288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martín-Moro F, Marquet J, Piris M, et al. Survival study of hospitalised patients with concurrent COVID-19 and haematological malignancies. Br J Haematol. 2020;190:e16–20. doi: 10.1111/bjh.16801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10:783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rüthrich MM, Giessen-Jung C, Borgmann S, et al. COVID-19 in cancer patients: clinical characteristics and outcome-an analysis of the LEOSS registry. Ann Hematol. 2021;100:383–393. doi: 10.1007/s00277-020-04328-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He W, Chen L, Chen Li, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34:1637–1645. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arcani R, Colle J, Cauchois R, et al. 2021 Clinical characteristics and outcomes of patients with haematologic malignancies and COVID-19 suggest that prolonged SARS-CoV-2 carriage is an important issue. Ann Hematol. 2021;100:2799–2803. doi: 10.1007/s00277-021-04656-z.Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Focà, E., Ripamonti, D., Rizzi, M., Bonfanti, P., Bruno, R., Casari, et al, 2020. Vademecum per la gestione terapeutica e di supporto per pazienti con infezioni da coronavirus COVID19. SIMIT SEZIONE REGIONE LOMBARDIA. edizione 3.0, pp. 1–9. https://www.simit.org/images/regioni/lombardia/comunicazioni/Vademecum%20COVID-19/4.%20vademecum%201.0%20%2001.03.20.pdf.
- 14.Codeluppi M, Ratti G, Nolli M, Campagna A, Marata AM et al. 2020. PROTOCOLLO TERAPEUTICO per la terapia antivirale dei pazienti con infezione da COVID19. Update 21 marzo 2020. Regione Emilia Romagna, Direzione Generale Cura della Persona, Salute e Welfare; pp. 1-8. http://www.fimp-pc.it/wp-content/uploads/2020/03/CC_PROTOCOLLO-TERAPEUTICOCOVID19-RER-finale1.pdf.
- 15.COVID19 Treatment Guidelines aveilable at https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/, last access on 19 April 2022
- 16.Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):56–93. doi: 10.1093/cid/cir073. [DOI] [PubMed] [Google Scholar]
- 17.ESMO guidelines available at https://www.esmo.org/guidelines/haematological-malignancies, last access on 19 April 2022
- 18.CogliatiDezza F, Oliva A, Cancelli F, Savelloni G, Valeri S, Mauro V, Calabretto M, Russo G, Venditti M, Turriziani O, Mastroianni CM. Determinants of prolonged viral RNA shedding in hospitalized patients with SARS-CoV-2 infection. Diagn Microbiol Infect Dis. 2021;100:115347. doi: 10.1016/j.diagmicrobio.2021.115347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296:E55–64. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang QuanQiu, Berger NA, Rong Xu. When hematologic malignancies meet COVID-19 in the United States: infections, death and disparities. Blood Rev. 2021;47:100775. doi: 10.1016/j.blre.2020.100775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanchez-Pina JM, Rodriguez MR, Quismondo NC, et al. Clinical course and risk factors for mortality from COVID-19 in patients with haematological malignancies. Eur J Haematol. 2020;105:597–607. doi: 10.1111/ejh.13493. [DOI] [PubMed] [Google Scholar]
- 23.Pagano L, Salmanton-García J, Marchesi F, et al. COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey (EPICOVIDEHA) J Hematol Oncol. 2021;14:168. doi: 10.1186/s13045-021-01177-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramasamy C, Mishra AK, John KJ, Lal A. Clinical considerations for critically ill COVID-19 cancer patients: A systematic review. World J Clin Cases. 2021;9:8441–8452. doi: 10.12998/wjcc.v9.i28.8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah V, Ko TK, Zuckerman M, et al. Poor outcome and prolonged persistence of SARS-CoV-2 RNA in COVID-19 patients with haematological malignancies; King's College Hospital experience. Br J Haematol. 2020;190:e279–e282. doi: 10.1111/bjh.16935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cattaneo C, Daffini R, Pagani C, et al. Clinical characteristics and risk factors for mortality in hematologic patients affected by COVID-19. Cancer. 2020;126:5069–5076. doi: 10.1002/cncr.33160. [DOI] [PubMed] [Google Scholar]
- 27.Abbasi B, Akhavan R, GhamariKhameneh A, Zandi B, Farrokh D, Pezeshki Rad M, FeyziLaein A, Darvish A, Bijan B. Evaluation of the relationship between inpatient COVID-19 mortality and chest CT severity score. Am J Emerg Med. 2021;45:458–463. doi: 10.1016/j.ajem.2020.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Panebianco V, Andreoli C, Colaiacomo MC, Zingaropoli MA, Ciardi MR, Mastroianni CM, Pugliese F, Alessandri F, Turriziani O, Ricci P, Catalano C. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol. 2020;30:6808–6817. doi: 10.1007/s00330-020-07033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Loffredo L, Campana A, Olivini N, Cotugno N, Palma P, Oliva A, Salvatori G, Zicari AM, Violi F. Hypoalbuminemia and clinical adverse events in children with COVID-19. J Med Virol. 2021;93:2611–2613. doi: 10.1002/jmv.26856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Violi F, Cangemi R, Romiti GF, Ceccarelli G, Oliva A, Alessandri F, Pirro M, Pignatelli P, Lichtner M, Carraro A, Cipollone F, D'ardes D, Pugliese F, Mastroianni CM. Is Albumin Predictor of Mortality in COVID-19? Antioxid Redox Signal. 2021;35:139–142. doi: 10.1089/ars.2020.8142. [DOI] [PubMed] [Google Scholar]
- 31.Violi F, Ceccarelli G, Cangemi R, Alessandri F, D'Ettorre G, Oliva A, Pastori D, Loffredo L, Pignatelli P, Ruberto F, Venditti M, Pugliese F, Mastroianni CM. Hypoalbuminemia, Coagulopathy, and Vascular Disease in COVID-19. Circ Res. 2020;127:400–401. doi: 10.1161/CIRCRESAHA.120.317173. [DOI] [PubMed] [Google Scholar]
- 32.Doucette K, Percival ME, Williams L, Kandahari A, Taylor A, Wang S, Ahn J, Karp JE, Lai C. Hypoalbuminemia as a prognostic biomarker for higher mortality and treatment complications in acute myeloid leukemia. Hematol Oncol. 2021;39:697–706. doi: 10.1002/hon.2925. [DOI] [PubMed] [Google Scholar]
- 33.Schaffrath J, Diederichs T, Unverzagt S, Wass M, Gläser U, Weber T, Binder M, Müller-Tidow C, Müller LP. Correlation of nutrition-associated parameters with non-relapse mortality in allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2021 doi: 10.1007/s00277-021-04736-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baang JH, Smith C, Mirabelli C, Valesano AL, Manthei DM, Bachman MA, Wobus CE, Adams M, Washer L, Martin ET, Lauring AS. Prolonged severe acute respiratory syndrome coronavirus 2 Replication in an immunocompromised patient. J Infect Dis. 2021;223:23–27. doi: 10.1093/infdis/jiaa666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hensley MK, Bain WG, Jacobs J, Nambulli S, Parikh U, Cillo A, Staines B, Heaps A, Sobolewski MD, Rennick LJ, et al. Intractable COVID-19 and Prolonged SARS-CoV-2 Replication in a CAR-T-cell Therapy Recipient A Case Study. Clin Infect Dis. 2021;73:812. doi: 10.1093/cid/ciab072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avanzato VA, Matson MJ, Seifert SN, Pryce R, Williamson BN, Anzick SL, Barbian K, Judson SD, Fischer ER, Martens C, et al. Case study: prolonged infectious SARS-CoV-2 shedding from an asymptomatic immunocompromised individual with cancer. Cell. 2020;183:1901–12.e9. doi: 10.1016/j.cell.2020.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information and are available from the corresponding author upon request.