Abstract
Aim:
To analyze the impact of the COVID-19 pandemic on US healthcare resource utilization.
Methods:
Optum claims data were used to compare all-cause healthcare visits and healthcare spending for selected diseases between the prepandemic and pandemic periods. Telemedicine use was only assessed for the pandemic period owing to data availability.
Results:
During the first wave of the pandemic, all-cause healthcare visits across all selected disease areas displayed a rapid decline compared with the prepandemic period, followed by a period of recovery. A reduction in outpatient and home healthcare spending was observed, whereas inpatient and prescription spending increased.
Conclusion:
Changes in healthcare resource utilization trends were observed during the pandemic. The magnitude of these changes can inform subsequent studies that utilize COVID-19-era data.
Keywords: : COVID-19, HCRU, healthcare spending, hospital visits, Optum claims, outpatient visits, real-world data, telemedicine
The emergence of COVID-19 at the end of 2019 caused a large global outbreak. The World Health Organization announced that COVID-19 was a public health emergency of international concern in January 2020 [1] and declared the outbreak to be a pandemic on 11 March 2020 [2]. As of 20 January 2022, >236 million COVID-19 cases were estimated to have occurred worldwide, resulting in >5 million deaths. Of these, the USA is estimated to account for >67 million cases and >800,000 deaths [3].
Since the start of the pandemic, there has been a change in the interactions between patients and healthcare systems. This can mainly be attributed to three key factors. First, new governmental and health policies were introduced in response to the pandemic. In the USA, new health policies included federal and state ‘stay-at-home’ recommendations as well as a ban on international travel for areas considered to be of high risk. Additionally, new legislation was passed to increase healthcare accessibility and enable individuals to seek medical attention more easily for both COVID-19 and any other ongoing or newly arising conditions. This included the Coronavirus Preparedness and Response Supplemental Appropriations Act (2020) [4] and the temporary waiver of certain requirements for Medicare, Medicaid and the Health Insurance Portability and Accountability Act (1996) [5], under section 1135 of the Social Security Act. These developments aimed to increase healthcare coverage during the pandemic period and encourage the use of telemedicine alternatives by incorporating reimbursement into public and private insurance plans. Second, there was a change in healthcare prioritization and resource allocation: resources (including hospital beds, staff and equipment) were diverted away from other disease areas and reallocated to COVID-19 patient care [6,7]. Patients with COVID-19 were often associated with increased healthcare resource utilization (HCRU) due to extended lengths of stay in critical care units and increased requirements for specialist medical equipment and staff [8]. Third, psychosocial factors and behaviors, such as a fear of the virus and a desire to not place excess burden on the healthcare system, meant that individuals often refrained from accessing medical care for other conditions [9].
To date, the literature has focused on the initial lockdown period, showing decreased hospital admissions across outpatient [10], inpatient [11,12] and emergency departments (EDs) [13]. Conversely, telemedicine use is reported to have increased [14]. Cancer and cardiovascular disease are prevalent worldwide and predispose patients to more severe clinical outcomes from COVID-19 [15,16]. Moreover, the risk of adverse outcomes for cardiovascular disease has been compounded by the effects of the COVID-19 pandemic on healthcare systems and the disruptions caused to routine care [17]. Therefore, these comorbidities have been explored more extensively than others. In addition, many studies utilize data from a small number of healthcare centers, with few obtaining data representative of a national population-wide perspective.
This retrospective observational study used real-world data from the Optum de-identified Clinformatics Data Mart to provide additional insight into US HCRU data during the COVID-19 pandemic in 2020. Contrary to previous smaller scale research, this study explored HCRU across various disease areas and over an extended time period while simultaneously providing a nationwide perspective.
Materials & methods
Data source
Deidentified patient-specific claims data for this retrospective observational study were obtained from the Optum de-identified Clinformatics Data Mart (MN, USA). This is an administrative claims database in the USA containing standardized billing codes used by healthcare providers such as physicians, hospitals and pharmacies for healthcare payer reimbursement. Population characteristics data consisted of age (18–29, 30–39, 40–49, 50–59, 60–69, 70–79 and ≥80 years), sex (male or female), geographical region and insurance type (commercial or Medicare) (Supplementary Tables 1 & 2).
Sample & cohort selection
Sample selection and outcome variable creation were carried out using Instant Health Data software (Panalgo; MA, USA). Sample selection was conducted by taking a random 25% sample (17,840,591 patients) from the total population found in the database (71,342,430 patients). The study consisted of prepandemic (1 March 2019–29 February 2020) and pandemic (1 March 2020–28 February 2021) time periods, which allowed for a direct comparison. A start date of 1 March 2020 was chosen for the pandemic period because it coincided with the declaration of COVID-19 as a pandemic and signified the beginning of rising COVID-19 cases in the USA. Patients were included in the study if they had an encounter with the healthcare system captured in the database during the prepandemic or pandemic period (4,423,465 patients). These encounters represented distinct interactions between the patient and the healthcare system. All encounters were captured under the patient’s principal diagnosis. Each encounter could contain multiple records which in turn could contain multiple events. Patients with COVID-19 were not explicitly included or excluded from this study. An algorithm was applied to assign service location and to group records in a way that better reflected real-world clinically relevant medical encounters. All patients were required to have continuous healthcare enrolment for the 24-month study period, including both the prepandemic and pandemic periods, resulting in a final study population of 2,137,057 patients.
We assessed HCRU in the following indications: chronic heart failure (CHF; n = 93,359; 4.37%), high cholesterol (n = 635,053; 29.72%), atherosclerotic cardiovascular disease (ASCVD; n = 425,664; 19.92%), major depressive disorder (MDD; n = 328,773; 15.38%), psoriasis (n = 35,506; 1.66%), relapsing multiple sclerosis (MS; n = 8282; 0.39%) and wet age-related macular degeneration (AMD; n = 19,623; 0.92%). Oncology areas included breast cancer (n = 39,391; 1.84%), lung cancer (n = 11,477; 0.54%) and chronic lymphocytic leukemia (CLL; n = 4681; 0.22%) (International Classification of Diseases, 10th Revision [ICD-10], codes are available in Supplementary Table 3). Disease areas of interest for the study were selected based on Novartis’ pipeline pharmaceutical and oncology compounds. Cohorts for each disease area were created in Instant Health Data (IHD) by using the ICD-10 clinical modification diagnosis codes for patient identification. Patients who received a diagnosis of a disease of interest at any point during the prepandemic and pandemic periods were included. Although not representative of all diseases, these selected indications represent major diseases that are spread across several different therapeutic areas. Each indication included patients of both insurance types, with Medicare being the predominant insurance type across the selected disease areas (Supplementary Tables 1 & 2).
Outcomes
The primary outcome of this study was the impact of the COVID-19 pandemic on all-cause healthcare visits through comparison of the pandemic and prepandemic periods for the specified disease areas. In-person visits were disaggregated into three categories: outpatient, inpatient and ED. Outpatient services included any medical care or hospital service provided to a patient without admission or overnight stay. This covered a wide range of medical services including primary care, diagnostics and procedures undertaken for an unadmitted patient. Inpatient visits were classified as any medical service in which the individual was formally admitted to hospital requiring an overnight stay. Inpatient visits could be elective, urgent or via referral from other healthcare areas such as the ED. ED visits were classified as the services provided within hospitals to patients seeking unplanned or urgent medical care.
The total annualized visits for both the prepandemic and pandemic study periods were measured. The overall percentage change between the two periods was calculated from these values for each disease area. For interpretation, any overall percentage change of <1% was not considered meaningful. In addition, the average percentage change across the selected disease areas between the two periods was calculated for each in-person healthcare visit category. For the comparison of weekly trends across selected disease areas, the weekly percentage change between the two periods was calculated and presented as a weekly distribution.
The secondary outcomes of this study included trends in the use of telemedicine in the pandemic period. Owing to a lack of telemedicine use, billing code availability and inclusion in payer reimbursement in the prepandemic period, a comparison between the two study periods could not be made for telemedicine use. However, the analysis allowed us to track the change in telemedicine use during the pandemic period itself. To allow for comparison across disease areas and to account for varying levels of prevalence and total visit counts, the weekly telemedicine visits for each disease area were calculated as a percentage of the total telemedicine visits for each disease area in the pandemic period. The change in healthcare spending between the prepandemic and pandemic periods was also assessed. For each disease area, separate totals for the categories of outpatient, inpatient, home healthcare and prescription spending were calculated. Costs were standardized by Optum using standard pricing algorithms to account for differences in pricing across health plans and provider contracts. Healthcare spending for outpatient, inpatient and home healthcare was calculated using the standard cost variable (STD_COST; defined as amount paid) in the defined service location (mapped using the HCFA place of service) within the defined time period [18]. The STD_COST variable was inflated to the most recent standard cost year (STD_COST_YR) available in the data source using the inflation algorithm and cost factors defined by Optum. Costs were only mapped from records found in the Optum medical claims table. Prescription spending was calculated using the STD_COST within the designated time period in the Optum prescription claims table. The medication type was set to ‘prescribed’. Inflation factors were selected based on the ‘pharmacy’ type of service. Because different payment mechanisms are used for each category of provider service, Optum created different approaches for standardized pricing for each of the following major service categories (facility inpatient, facility outpatient, professional/ancillary services and pharmacy costs). Facility inpatient services are based on the Medicare Severity Diagnosis Related Group (DRG). Facility outpatient services are based on the Centers for Medicare and Medicaid Services (CMS) Outpatient Prospective Payment System. Professional and ancillary services are estimated using a resource-based value scale, which monetizes the CMS relative value units. Estimated costs from pharmacy are based on the pricing from the First Databank and adjusted according to therapeutic category and generic indicator [18].
To allow for comparison across different spending categories and different disease areas, healthcare spending was calculated as the average total spending per patient. The percentage change in spending was calculated for each spending category and each disease area.
Results
Outpatient visits
Percentage reductions in the number of outpatient visits were observed between the prepandemic and pandemic periods for most disease areas, ranging from 10.57% (relapsing MS) to 1.51% (psoriasis). However, outpatient visits for patients with MDD and lung cancer increased, displaying an average percentage increase of 7.04% and 8.94%, respectively (Supplementary Table 4). Visits for patients with CLL displayed little change (0.47%).
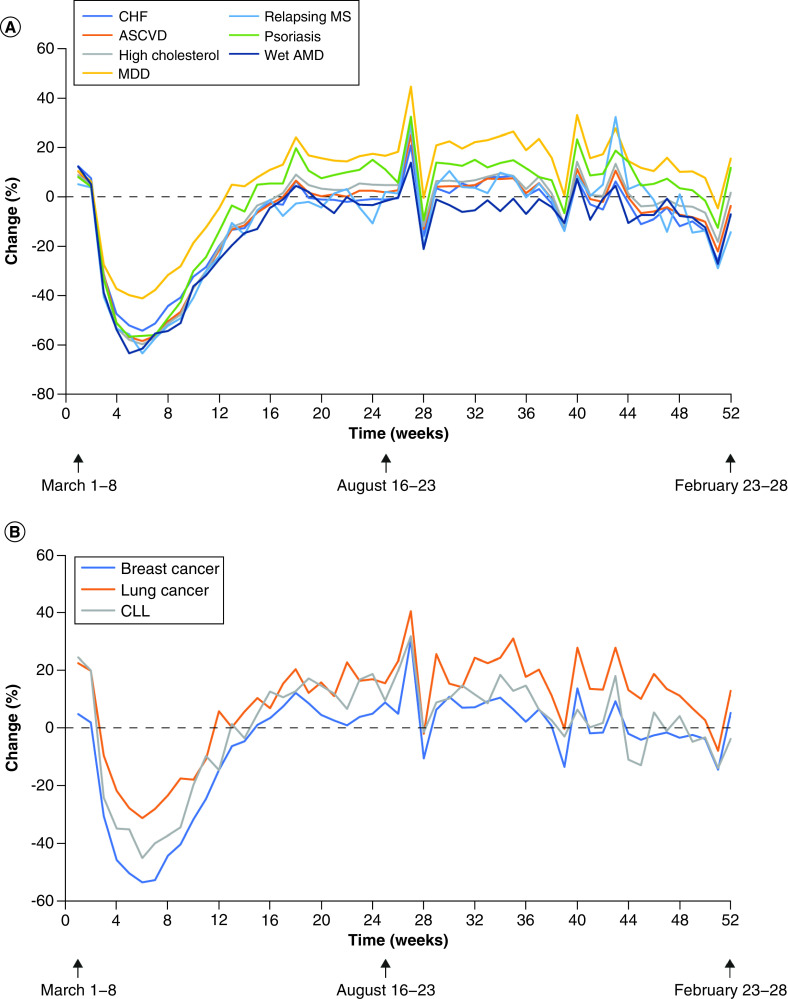
There was a general trend of reduction in outpatient visits over the pandemic period across all disease areas (Figure 1). Between week 3 (14–21 March 2020) and week 6 (4–11 April 2020), a dramatic reduction in outpatient visits was observed, followed by a recovery in weekly outpatient visits to prepandemic levels by week 26 for all selected disease areas. Thereafter, visitation numbers across disease areas consistently recovered and remained above prepandemic levels.
Figure 1. . Weekly percentage change in outpatient visits between the prepandemic (black line at 0% change indicates mean value) and pandemic periods.
(A) Pharmaceutical disease areas. (B) Oncology disease areas.
AMD: Age-related macular degeneration; ASCVD: Atherosclerotic cardiovascular disease; CHF: Chronic heart failure; CLL: Chronic lymphocytic leukemia; MDD: Major depressive disorder; MS: Multiple sclerosis.
Inpatient visits
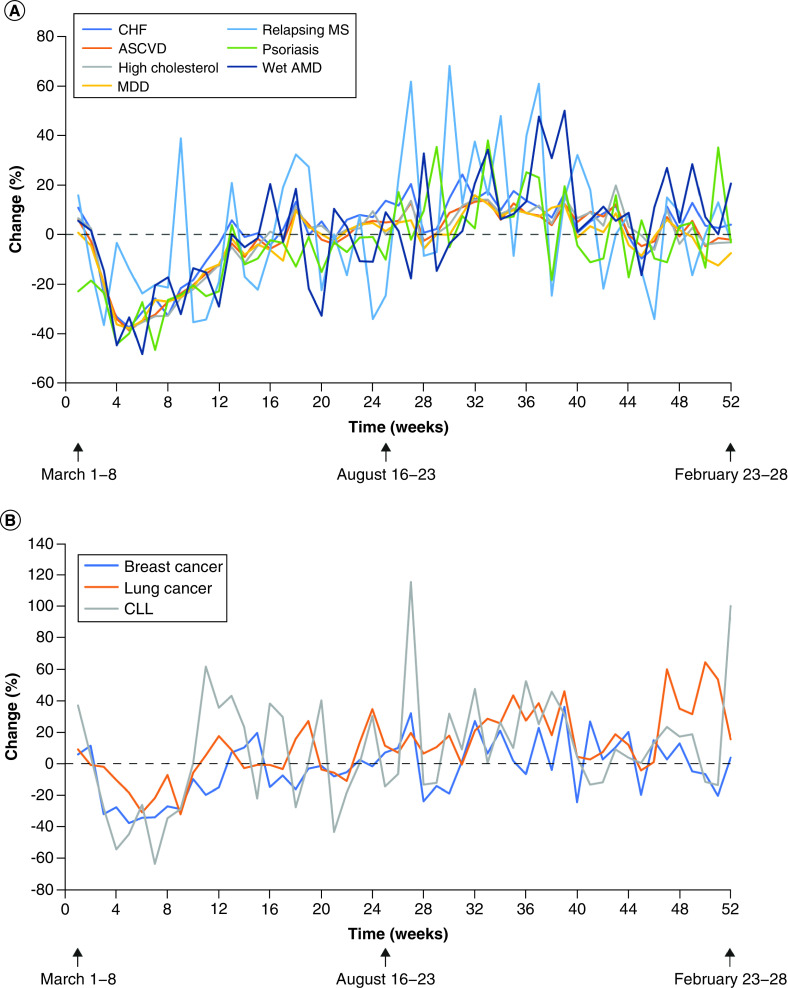
Across the selected disease areas, little change was observed in annual inpatient visits during the pandemic period. The disease area with the greatest percentage reduction in inpatient visits was psoriasis, which demonstrated a 6.43% decline compared with prepandemic visits. Other disease areas that demonstrated noticeable reductions included MDD (4.10%) and breast cancer (3.86%). Conversely, inpatient visits for lung cancer and CLL increased overall during the pandemic, with respective increases of 10.44% and 3.39% (Supplementary Table 5). Whereas inpatient visits for relapsing MS, wet AMD and CHF showed little overall change, levels for these disease areas did display an initial decline early in the pandemic period, followed by a recovery to their respective prepandemic levels.
Overall, in the early stages of the pandemic period (week 1), inpatient visit numbers were similar to prepandemic levels for most disease areas except for psoriasis, which displayed a 23.21% decline. For most selected disease areas, the decline in inpatient visits began at week 2 and reached a nadir between weeks 4 and 7. Recovery to prepandemic levels was observed for all selected disease areas by week 17 (Figure 2).
Figure 2. . Weekly percentage change in inpatient visits between the prepandemic (black line at 0% change indicates mean value) and pandemic periods.
(A) Pharmaceutical disease areas. (B) Oncology disease areas.
AMD: Age-related macular degeneration; ASCVD: Atherosclerotic cardiovascular disease; CHF: Chronic heart failure; CLL: Chronic lymphocytic leukemia; MDD: Major depressive disorder; MS: Multiple sclerosis.
ED visits
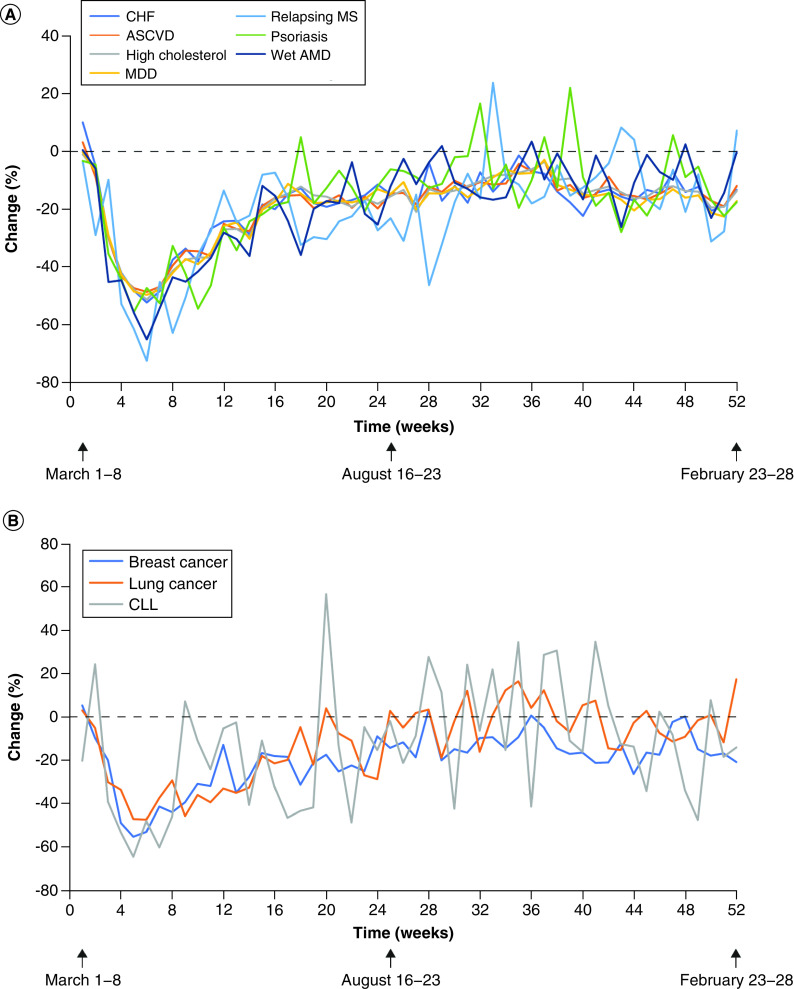
All selected disease areas exhibited reductions in ED visits, with the greatest total percentage changes observed for relapsing MS (22.65%), breast cancer (20.09%) and MDD (19.61%) (Supplementary Table 6).
Except for CLL, the number of ED visits at the start of the pandemic period was similar to that observed in the prepandemic period (Figure 3). Following an early reduction between week 3 (14–21 March 2020) and week 6 (4–11 April 2020), all disease areas entered a recovery period lasting until week 52. Overall, ED visits did not recover to prepandemic levels as fully as outpatient and inpatient visits by the end of the study period. Whereas CLL, psoriasis, relapsing MS and lung cancer did recover to prepandemic levels at certain time points during the pandemic period, other disease areas did not. Instead, these disease areas consistently displayed a 20–30% reduction in ED visits (Figure 3).
Figure 3. . Weekly percentage change in emergency department visits between the prepandemic (black line at 0% change indicates mean value) and pandemic periods.
(A) Pharmaceutical disease areas. (B) Oncology disease areas.
AMD: Age-related macular degeneration; ASCVD: Atherosclerotic cardiovascular disease; CHF: Chronic heart failure; CLL: Chronic lymphocytic leukemia; MDD: Major depressive disorder; MS: Multiple sclerosis.
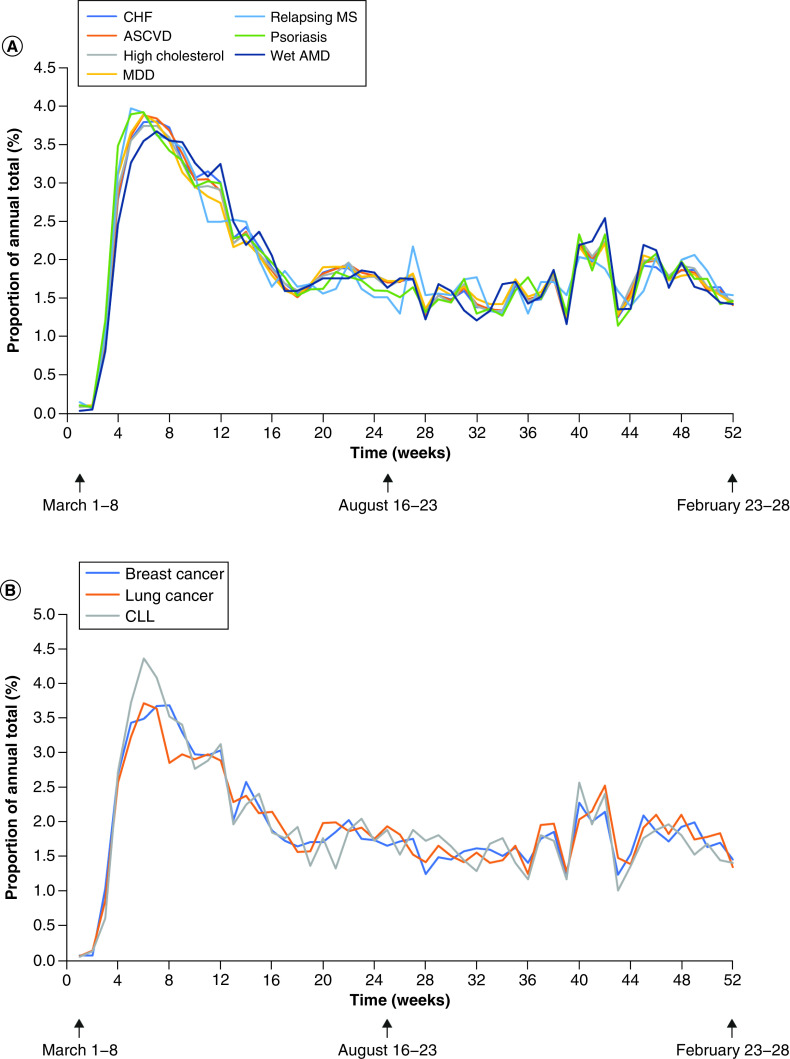
Telemedicine
A rapid rise in telemedicine use began after week 2 of the pandemic and peaked at week 6. There was a subsequent reduction between week 7 and week 18, which plateaued from week 19 until week 39. After this, a small increase was observed again between week 40 and week 43. This pattern was consistent across all selected disease areas (Figure 4).
Figure 4. . Weekly distribution of the total telemedicine visits as a percentage of annual telemedicine visits during the pandemic period.
(A) Pharmaceutical disease areas. (B) Oncology disease areas.
AMD: Age-related macular degeneration; ASCVD: Atherosclerotic cardiovascular disease; CHF: Chronic heart failure; CLL: Chronic lymphocytic leukemia; MDD: Major depressive disorder; MS: Multiple sclerosis.
Healthcare spending
A decrease of 16.16% on the average outpatient spending per patient was observed during the pandemic period. Although all selected disease areas exhibited reduced outpatient spending, wet AMD (26.68%) and relapsing MS (25.40%) exhibited the greatest percentage change (Figure 5A).
Figure 5. . Mean healthcare spending per patient across disease areas in the prepandemic and pandemic periods.
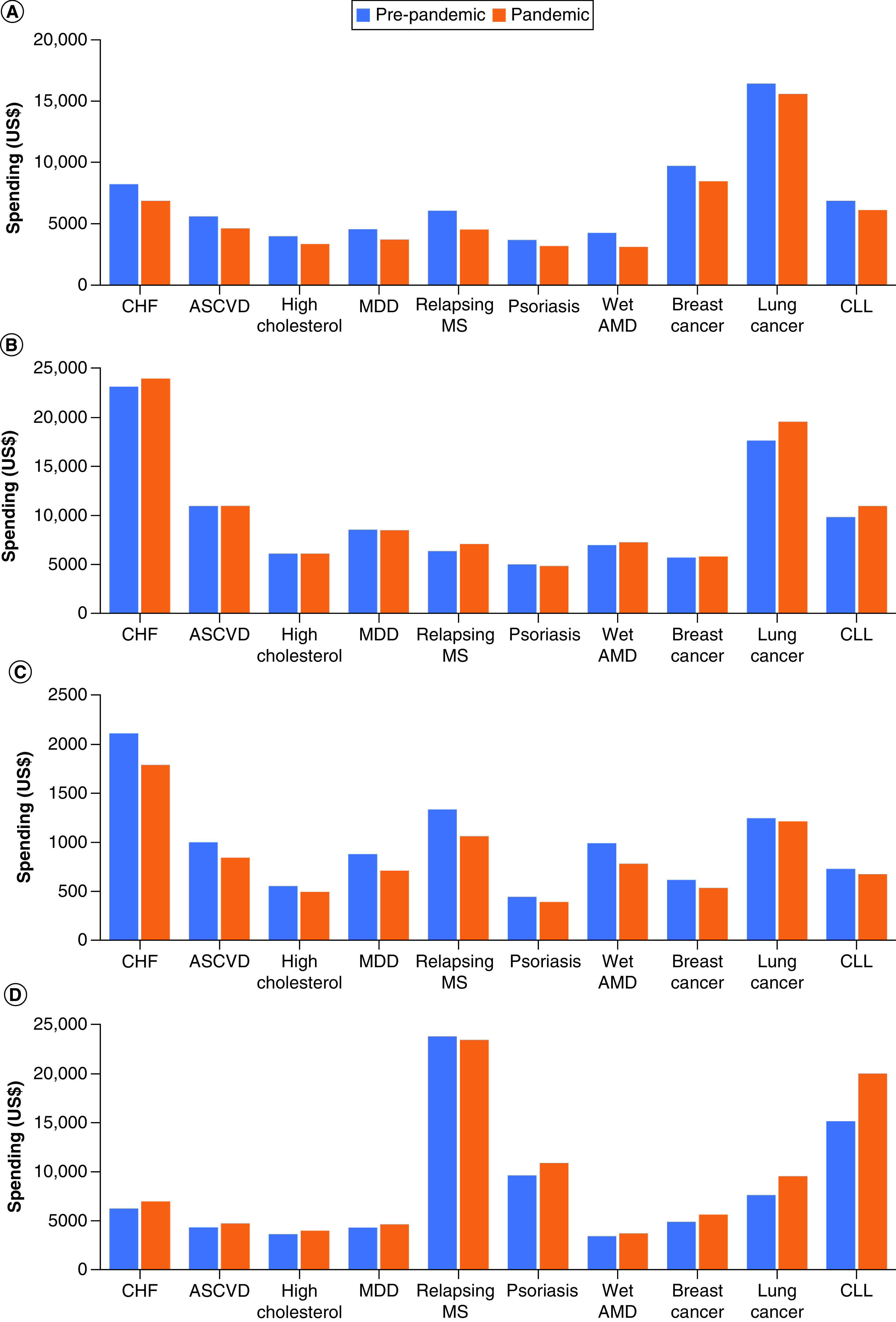
(A) Outpatient spending. (B) Inpatient spending. (C) Home healthcare spending. (D) Prescription spending.
AMD: Age-related macular degeneration; ASCVD: Atherosclerotic cardiovascular disease; CHF: Chronic heart failure; CLL: Chronic lymphocytic leukemia; MDD: Major depressive disorder; MS: Multiple sclerosis.
The average inpatient spending per patient increased by 4.01% during the pandemic. Psoriasis exhibited a decrease in spending of 3.11%, whereas ASCVD, MDD and high cholesterol showed negligible changes; however, all other disease areas demonstrated an increase in inpatient spending, with CLL, relapsing MS and lung cancer experiencing the greatest percentage increase in mean inpatient spending per person (11.59%, 11.45% and 10.90%, respectively) (Figure 5B).
Home healthcare spending was also reduced across all selected disease areas. Overall, the average home healthcare spending per patient was reduced by 13.68% during the pandemic (Figure 5C).
Finally, the average prescription spending per person increased during the pandemic period across most selected disease areas, with a mean percentage increase of 13.04%. The greatest increase in prescription spending was in CLL (31.86%), followed by lung cancer (25.49%). Relapsing MS was the sole disease area to exhibit a reduction in prescription spending (1.42%) (Figure 5D).
Discussion
Patient concerns about COVID-19 infection may have caused a reduction in the number of hospital visits
This study evaluated the impact of the COVID-19 pandemic on HCRU across multiple disease areas in the USA. Perhaps unsurprisingly, there was a reduced number of hospital visits of all types during the pandemic compared with the prepandemic period. More specifically, outpatient, inpatient and ED visits across all selected disease areas displayed a rapid decline in numbers during the early pandemic period, followed by a period of recovery that started at approximately week 7. Out of the three types of visit included in the study (outpatient, inpatient and ED), ED visits displayed the greatest reduction across all disease areas, whereas inpatient visits showed little reduction. Reports from California [19] and across the USA [13] showed similar patterns of reduced visitation numbers during the early pandemic period, with one study reporting an overall decline of 42% in ED visits between 29 March and 25 April 2020 compared with the same period in 2019 [13]. The changes observed in the number of ED visits can likely be attributed to government recommendations advising the public to only visit the ED when necessary, in addition to general concerns about COVID-19 infection.
Furthermore, the reductions in visits observed in this study for certain disease areas such as CHF and ASCVD are concerning: this would suggest that individuals with these conditions avoided ED interactions and delayed care, which could potentially have resulted in increased morbidity and mortality [13]. Although not covered in this study, future studies should aim to explore the long-term impact of the COVID-19 pandemic on ASCVD and cancer.
The reduction in outpatient visits was expected because many primary care services were considered nonessential and face-to-face visits were halted at the start of the pandemic. In-person services were provided only in essential cases – often to those with concerning symptoms or for whom face-to-face monitoring was vital. In the case of inpatient visits, admissions for urgent conditions were expected to remain stable throughout the pandemic because they are often considered essential. In contrast, visits for less urgent conditions and elective surgeries could be delayed until a recovery in the pandemic was observed. Indeed, the resumption of elective surgery coincided with the recovery of inpatient visits for all disease areas to prepandemic levels.
Interestingly, despite showing an initial reduction between week 3 and week 7, both outpatient and inpatient visits for lung cancer recovered and displayed consistently higher weekly numbers during the pandemic compared with the prepandemic period from approximately week 12. This is surprising because patients with cancer are considered to be at high risk from COVID-19 and would have been encouraged to remain at home [20]. In addition, many healthcare providers responded to the pandemic by adjusting care services, such as delaying surgeries and switching to telemedicine [20]. Certain types of cancer such as lung cancer and CLL can cause increased morbidity unless immediately diagnosed and treated [21]. However, patients with early-stage cancers such as breast cancer might be more resilient to delays [21]. It is therefore possible that in the case of lung cancer and CLL, the benefits of maintaining planned therapies and the risks associated with a delay in treatment outweighed the risk of COVID-19 infection.
Similarly, following the initial reduction period, outpatient visits for MDD and psoriasis significantly increased during the pandemic period. The observed trends for MDD can likely be attributed to the adverse effects of the COVID-19 pandemic on mental health. In addition to economic lockdowns, stay-at-home orders and experiences with the virus (e.g., bereavement) acting as contributors to psychological distress, the interruptions in care during the early pandemic period may have exacerbated the condition of patients with existing MDD [22]. The psychological distress caused by the pandemic coupled with stay-at-home orders could have acted as the catalysts for exacerbations of pre-existing cases of psoriasis, prompting outpatient visits. Indeed, stress has been established as a trigger for the onset or aggravation of psoriasis [23].
Telemedicine use increased during the early pandemic period
The data showed a rise in the use of telemedicine codes for reimbursement between week 3 and week 6 of the pandemic period, which coincided with the start of the US lockdown period and the decline of in-person visits. The rapid uptake of telemedicine observed during the pandemic was facilitated by regulatory changes that led to the expansion of reimbursement for such services [14]. The benefits of telemedicine have been documented previously; in addition to reducing the risk of COVID-19 infections, telemedicine has been found to result in similar health outcomes as in-person delivery of care [24]. Furthermore, telemedicine can be used to increase access to healthcare in underserved geographical areas while at the same time reducing the cost to individuals who would otherwise have to travel significant distances to access in-person care [25]. However, despite its potential, a recent study on telemedicine uptake during the early pandemic period has shown that rural areas in particular experienced significant logistic challenges in implementing telemedicine [26].
Telemedicine data used in this study need to be interpreted with caution because coverage expansion for medical insurance providers, Medicare and Medicaid was not mandatory or universal across all states in 2020 [27]. This heterogeneous coverage between states may have resulted in vulnerable individuals being unable to access telemedicine during the early stages of the pandemic. Furthermore, there was an initial lack of billing code availability (usually used by payers to process claims and determine reimbursement amounts); new billing codes may not have been adopted promptly, and, consequently, telemedicine services conducted during the pandemic period may have been coded using previous ‘in-person’ billing codes. This could potentially have led to an underestimation of telemedicine use.
Telemedicine visits constituted a small proportion of overall interactions within the healthcare system. The decline in telemedicine use as restrictions eased reinforces previous evidence that most healthcare users and healthcare providers have a preference for in-person visits [28,29]. Many hurdles (including technological and legal barriers) still need to be overcome if telemedicine is to have a more permanent place in healthcare systems and patient care pathways.
The COVID-19 pandemic was associated with decreased home & outpatient healthcare spending in the selected disease areas
Across the selected disease areas, home healthcare exhibited a reduction in average spending per person. This could largely be due to restrictions preventing licensed healthcare professionals from entering patients’ houses to provide home healthcare services. Similarly, a reduction in outpatient spending was observed, coinciding with reductions in outpatient visits across most disease areas.
Interestingly, there was an increase in inpatient spending. This is contrary to previous reports [30] and was unexpected. Such heightened spending could reflect increased COVID-19 testing efforts or the increased demand for previously deferred services once lockdown measures had been lifted.
Likewise, an increase in prescription spending per person across all disease areas of interest was observed. This may simply be due to the annual increase in drug costs [31] or due to increased prescription use to prevent disease progression while inpatient procedures were postponed. On a positive note, this suggests that patients were still able to obtain the medications that they required during the pandemic, despite restricted access to healthcare systems.
Future research should consider the changes in HCRU data during the pandemic period
Overall, the results of this study demonstrated the influence that the COVID-19 pandemic had on HCRU for selected disease areas. The changes in HCRU noted during the COVID-19 pandemic are important for ongoing and future HCRU and cost studies because data produced during the pandemic period may be significantly different from those generated in previous years. Future studies are likely to be affected in several ways. For instance, studies that assume healthcare access and HCRU remain stable over time, or even experience a linear trend, are likely to be vulnerable to bias related to the pandemic. During the pandemic period, these assumptions would no longer be fulfilled, thus making results inaccurate [32]. Additionally, the global nature of the pandemic means that it would not be possible for studies to adjust for these data differences by including unaffected areas as controls [32]. Disease areas that experience seasonal variation are even more at risk of this potential bias and inaccuracy. Nevertheless, various strategies could potentially be used to mitigate the risk of this type of bias. First, the pandemic period could be excluded from the analyses of studies relying on healthcare data that might have been affected. Challenges with this approach could arise because the ongoing pandemic and potential appearance of new COVID-19 variants might complicate the identification of the time period for exclusion. Imputing for the pandemic period could be an alternative solution. Observational studies could potentially minimize bias by using synthetic controls [32]. A silver bullet for these issues is unlikely to exist; however, it is essential that ongoing and future studies take into consideration the data disruptions observed during the COVID-19 pandemic and incorporate appropriate plans into their study designs and analyses.
Limitations
The data available represents commercial and Medicare claims made in the US healthcare system for payer reimbursement of selected diseases. However, not all claims are accepted for reimbursement; therefore, absolute values could be overestimated. This problem is relevant for both prepandemic and pandemic data and, consequently, does not affect comparisons made between the two time periods. Claims data do not represent the most recent 6-month period owing to the time lag in data availability. Outside of administrative limitations, data availability is restricted to measures recorded in the Optum claims database, which prevented the inclusion of some patient outcomes in this study. Similarly, those relying on Medicaid health coverage are not included. The lack of Medicaid data is important to consider when interpreting findings, given that COVID-19 indirectly resulted in increased unemployment and financial hardship [33,34]. Furthermore, the impacts of mortality are not reflected in the study owing to the 24-month patient follow-up requirement in the inclusion criteria. Finally, claims data do not contain socioeconomic information about patients; as a consequence, sample weighting for statistical analysis is not possible.
Although disease areas of interest were selected based on Novartis’ pipeline pharmaceutical and oncology compounds, the resulting population was largely characterized by patients who were >65 years of age, with Medicare being the predominant insurance type. This is an important factor when interpreting findings, because alternative choices of disease areas that are more prevalent in those <65 years of age might have exhibited different results.
Using only a 1-year prepandemic period sets up a type of bias in the selection of eligible patients to assess the before and after effects, but this limitation was chosen to be an adequate comparator period that allows for a large enough sample size in some of the smaller disease areas.
Conclusion
Unsurprisingly, the COVID-19 pandemic had a significant impact on HCRU data. Future research that considers utilizing HCRU data from the COVID-19 era should account for this fact by either excluding the period altogether, through imputation techniques, through the use of appropriate sensitivity analyses or through other methods. In any case, awareness of the issue followed by prespecification of the chosen method will be critical. Telemedicine presents a promising alternative to face-to-face visits, and the pandemic provided a springboard for the acceleration of virtual healthcare technology. However, the use of telemedicine declined as in-person healthcare was resumed, indicating that more research into healthcare preferences and patient behavior is required for telemedicine to be included permanently in future care pathways. Finally, whereas the decline in hospital visits was reflected in the reduction of healthcare spending (aside from inpatient spending), prescription spending increased during the pandemic period; this potentially indicates that patients retained access to their required medications during the pandemic.
The present study will contribute to future healthcare planning and resource allocation to protect patient access to care in the long term, both in the event of a future pandemic and as part of the postpandemic recovery. Furthermore, the disruption in real-world data reported here can position this study as a benchmark for future researchers wishing to use COVID-19–era data from the Optum Clinformatics Data Mart claims database.
Summary points.
Since the start of the COVID-19 pandemic, there have been changes in the interactions between patients and healthcare systems.
This retrospective observational study used real-world data from the Optum Clinformatics Data Mart to provide additional insight into US healthcare resource utilization data during the pandemic.
The number of healthcare visits across all selected disease areas displayed a rapid decline during the early pandemic period compared with the prepandemic period, followed by a period of recovery.
The observed uptake of telemedicine during the pandemic was facilitated by regulatory changes that led to the expansion of reimbursement for such services.
An increase in prescription spending per person was observed across all disease areas of interest during the pandemic period compared with the prepandemic period, whereas home and outpatient healthcare spending decreased.
This study will contribute to healthcare planning and resource allocation to protect patient access to care.
Future and ongoing studies that rely on healthcare data should acknowledge data disruptions caused by the COVID-19 pandemic and evaluate potential pitfalls accordingly.
Supplementary Material
Footnotes
Supplementary data
To view the supplementary data that accompany this paper please visit the journal website at: www.futuremedicine.com/doi/suppl/10.2217/cer-2022-0059
Author contributions
All authors have fulfilled the authorship criteria and accept accountability for all content. Each author has significantly contributed to, reviewed and approved the manuscript.
Financial & competing interests disclosure
Development of this manuscript was funded by Novartis Pharma AG. All authors are employees of Novartis. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Medical writing support was provided by Eleni Tente of PharmaGenesis London, London, UK, with funding from Novartis Pharma AG.
Open access
This work is licensed under the Attribution-NonCommercial-NoDerivatives 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.World Health Organization. WHO Director-General’s Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV) (2021). www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov)
- 2.World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 – 11 March 2020 (2021). www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.World Health Organization. WHO Coronavirus (COVID-19) Dashboard (2021). https://covid19.who.int/
- 4.Congress.gov. H.R.6074 – Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. (2020). www.congress.gov/bill/116th-congress/house-bill/6074
- 5.Congress.gov. H.R.3103 – Health Insurance Portability and Accountability Act of 1996:104th Congress (1995–1996). (1996). www.congress.gov/bill/104th-congress/house-bill/3103
- 6.Haut ER, Leeds IL, Livingston DH. The effect on trauma care secondary to the COVID-19 pandemic: collateral damage from diversion of resources. Ann. Surg. 272(3), e204 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diegoli H, Magalhães PS, Martins SC et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 51(8), 2315–2321 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janke AT, Mei H, Rothenberg C, Becher RD, Lin Z, Venkatesh AK. Analysis of hospital resource availability and COVID-19 mortality across the United States. J. Hosp. Med. 16(4), 211–214 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Emergency Physicians. Public Poll: Emergency Care Concerns Amidst COVID-19 (2020). www.emergencyphysicians.org/article/covid19/public-poll-emergency-care-concerns-amidst-covid-19
- 10.The Commonwealth Fund. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases (2021). www.commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge
- 11.Butt AA, Kartha AB, Masoodi NA et al. Hospital admission rates, length of stay, and in-hospital mortality for common acute care conditions in COVID-19 vs. pre-COVID-19 era. Public Health 189, 6–11 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Rosa S, Spaccarotella C, Basso C et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 41(22), 2083–2088 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartnett KP, Kite-Powell A, Devies J et al. Impact of the COVID-19 pandemic on emergency department visits – United States. MMWR Morb. Mortal. Wkly. Rep. 69(23), 699 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; • This study showed the change in emergency department visit numbers in response to the first wave of the pandemic.
- 14.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern. Med. 181(3), 388–391 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 5(7), 751–753 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323(18), 1775–1776 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Califf RM. Avoiding the coming tsunami of common, chronic disease: what the lessons of the COVID-19 pandemic can teach us. Circulation 143(19), 1831–1834 (2021). [DOI] [PubMed] [Google Scholar]
- 18.Optum’s de-identifed Clinformatics® Data Mart Database (2007–2021).
- 19.Wong L, Hawkins J, Langness S, Murrell K, Iris P, Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020(1), 1–12 (2020). [Google Scholar]; • This study described the efforts taken in a community hospital to understand and combat the public health concern of contracting COVID-19, which led to the decrease of emergency department visits.
- 20.Patt D, Gordan L, Diaz M et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin. Cancer Inform. 4, 1059–1071 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]; • This study demonstrated the substantial decrease in hospital visits and healthcare services for cancer in response to the COVID-19 pandemic.
- 21.Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A war on two fronts: cancer care in the time of COVID-19. Ann. Intern. Med. 172(11), 756–758 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahl KG, Correll CU. Management of patients with severe mental illness during the coronavirus disease 2019 pandemic. JAMA Psychiatry 77(9), 977–978 (2020). [DOI] [PubMed] [Google Scholar]
- 23.Garcovich S, Bersani F, Chiricozzi A, De Simone C. Mass quarantine measures in the time of COVID-19 pandemic: psychosocial implications for chronic skin conditions and a call for qualitative studies. J. Eur. Acad. Dermatol. Venereol. 34(7), e293–e294 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015(9), CD002098 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]; • This study outlined the benefits associated with the use of telemedicine.
- 25.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 231(2), 216–222 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demeke HB, Merali S, Marks S et al. Trends in use of telehealth among health centers during the COVID-19 pandemic – United States. MMWR Morb. Mortal. Wkly. Rep. 70(7), 240 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Commonwealth Fund. States’ Actions to Expand Telemedicine Access During COVID-19 and Future Policy Considerations (2021). www.commonwealthfund.org/publications/issue-briefs/2021/jun/states-actions-expand-telemedicine-access-covid-19
- 28.Browne JA. Leveraging early discharge and telehealth technology to safely conserve resources and minimize personal contact during COVID-19 in an arthroplasty practice. J. Arthroplasty 36(7), S52–S55 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shirke MM, Shaikh SA, Harky A. Implications of telemedicine in oncology during the COVID-19 pandemic. Acta Biomed. 91(3), e2020022 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McWilliams JM, Russo A, Mehrotra A. Implications of early health care spending reductions for expected spending as the COVID-19 pandemic evolves. JAMA Intern. Med. 181(1), 118–120 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]; • This study explored the potential effects of the COVID-19 pandemic for future healthcare spending.
- 31.Hwang TJ, Dusetzina SB, Feng J, Maini L, Kesselheim AS. Price increases of protected-class drugs in Medicare Part D, relative to inflation, 2012–2017. JAMA 322(3), 267–269 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shioda K, Weinberger DM, Mori M. Navigating through health care data disrupted by the COVID-19 pandemic. JAMA Intern. Med. 180(12), 1569–1570 (2020). [DOI] [PubMed] [Google Scholar]; •• The authors outlined the potential challenges associated with healthcare data disrupted by the COVID-19 pandemic for future studies.
- 33.Gangopadhyaya A, Garrett AB. Unemployment, Health Insurance, and the COVID-19 Recession Urban Institute, DC, USA: (2020). [Google Scholar]
- 34.Woolhandler S, Himmelstein DU. Intersecting US epidemics: COVID-19 and lack of health insurance. Ann. Intern. Med. 173(1), 63–64 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.