Abstract
Background
Cases with varus knee osteoarthritis (OA) often present concomitant ankle joint deformity and poor tibial plafond inclination (TPI) in the coronal plane. Although changes to the TPI with respect to the ground after open wedge high tibial osteotomy (OWHTO) have been described, reports on the relationship between the correction angle and severity of knee joint line obliquity (KJLO) are scarce. This study aimed to examine the correlation between the correction angle after OWHTO and the change in knee and ankle inclination with respect to the floor.
Methods
Between January 2016 and December 2019, 39 knees in 39 patients (mean age, 58.3 ± 9.7 years; male, 14 knees; female, 25 knees) underwent OWHTO for varus knee OA. The mean duration of follow up was 30.1 ± 9.8 months. Radiological severity of OA was evaluated for those with Kellgren-Lawrence grade 1–3. Preoperative and 1-year postoperative radiographs were used to examine the postoperative femorotibial angle, hip-knee angle, KJLO, TPI, talar tilt (TT), position of weight bearing line of the tibial plateau width (WBL ratio; %), and the relationship between the pre-to postoperative changes in each measured value and intraoperative correction angle. The relationship between the pre-to postoperative changes in each measured value and intraoperative correction angle were evaluated. Clinical evaluations were conducted before and 2 years after OWHTO using the Knee Injury and Osteoarthritis Outcome Score (KOOS) subscale of pain.
Results
The mean pre-to post-operative changes were 3.2 ± 2.2 for KJLO and 3.1 ± 2.5 for TPI, both demonstrating significant differences as well as significant correlations with the correction angle. The knee joint demonstrated postoperative changes in the valgus direction and none in the varus direction with respect to the floor in all cases. Furthermore, the sum of changes to the KJLO and TPI showed a positive correlation that approximates the change in the correction angle. The mean pre- and postoperative 2-year KOOS subscale of pain were 50.2 ± 10.2 and 82.3 ± 9.1. There were no correlations between preoperative TPI, pre-to postoperative change in TPI, and 2-year postoperative of KOOS subscale of pain.
Conclusion
For those who underwent OWHTO for varus OA, the knee joint changed from a preoperative varus malalignment to mild valgus malalignment, and the ankle joint tended to improve from a preoperative valgus malalignment to the postoperative neutral alignment with respect to the floor. Although a positive correlation was found in which the correction angle approximates the sum of changes to the KJLO and TPI, no significant difference was found between changes in KJLO and TPI nor in the ratio between the correction angle and changes in each measured value.
Keywords: Open wedge high tibial osteotomy, Knee joint line obliquity, Distal tibial plafond inclination
1. Introduction
In order to achieve good and stable clinical results in open wedge high tibial osteotomy (OWHTO), it is important to obtain an accurate coronal alignment using the Fujisawa Point.1 However, the planned intraoperative correction angle is sometimes unattainable despite being performed according to the preoperative plan, leading to under- or over-correction. Previous reports have suggested other important factors to consider for achieving an ideal correction for OWHTO, including the role of soft tissues around the knee joint such as the joint line convergence angle (JLCA), as well as the effect of the ankle joint and hindfoot alignment.2, 3, 4
Many cases with varus knee osteoarthritis (OA) present concomitant ankle joint deformity and poor tibial plafond inclination (TPI) in the coronal plane.5,6 A previous report has described that the coronal plane alignment associated with knee varus OA shows a tendency to cause the distal tibial articular surface to tilt laterally with respect to the floor (varus).7 Open wedge high tibial osteotomy (OWHTO) for varus deformity of the knee is a useful treatment option for highly active patients with mild varus deformity8, 9, 10; on the other hand, marked changes to the postoperative knee joint line obliquity (KJLO) can occur and induce shear stress due to its non-physiological articular surface,11 which may adversely affect clinical results. However, not all correction angles affect the KJLO, and the compensation for the correction of the ankle joint and foot could potentially be at play.8 Although previous reports have described changes to the TPI with respect to the floor after OWHTO,2,3,12,13 few studies have reported on the relationship between the correction angle and severity of KJLO. The purpose of this study is to examine the correlation between the correction angle after OWHTO and the change in knee and ankle inclination angles with respect to the floor at our hospital. We hypothesized that changes in postoperative joint inclination of the knee and ankle can be predicted by the correction angle and preoperative joint inclination to prevent non-physiological joint inclination and over- or under-correction after OWHTO.
2. Materials and methods
2.1. Diagnosis and clinical assessment
Between January 2016 and December 2019, a total of 39 knees in 39 patients (male, 14 knee; female, 25 knees) underwent OWHTO for varus knee OA. The mean age was 58.3 ± 9.7 (32–74) years. The mean duration of follow up was 30.1 ± 9.8 (19–61) months. The mean body mass index (kg/m2) was 24.7 ± 2.8 (range 20.1–28.7). The patient characteristics are summarized in Table 1. There were no patients lost to follow up.
Table 1.
Patient demographic characteristics (n=39).
| Age (years) | 58.3 ± 9.7(32–74) |
|---|---|
| Sex (male/female) | 14/25 |
| Body mass index (kg/㎡) | 24.7 ± 2.8(20.1–28.7) |
| Kellgren-Lawrence grade (1/2/3) | 5/32/2 |
Full-length standing plain radiography of the lower extremity was used to classify the severity of OA. The radiological severity according to the Kellgren-Lawrence classification system (KL classification)14 was as follows: Grade 1, 5 knees; Grade 2, 32 knees; Grade 3, 2 knees.
2.2. Surgical procedure and postoperative assessment
Prior to OWHTO, arthroscopic surgery was performed for medial meniscus injury and cartilage injury of the medial femoral condyle. For OWHTO, a 7 cm longitudinal skin incision was made in the anteromedial aspect of the tibia and the tibial tuberosity, and the superficial medial collateral ligament and a part of the pes anserinus were dissected. Preoperative planning for biplanar osteotomy was based on whole standing radiographs that aimed for an intraoperative correction angle defined as the angle at which the weight bearing line (Mikulicz line) passes through a point at 62.5% of the tibial plateau width. The intraoperative correction angle was determined by placing a metal rod from the center of the femoral head to the center of the ankle joint that passes through a point at 62.5% of the tibial plateau width while applying pressure on the sole of the feet. The mean intraoperative correction angle was 9.6 ± 1.6° (6-14). A locking plate (TomoFix® Osteotomy System, DePuy Synthes Inc., West Chester, Philadelphia, USA) was used for internal fixation, and the void created by the osteotomy was filled with a β-tricalcium phosphate block with 60% porosity (OSferion®, Olympus Terumo Biomaterials Corp., Tokyo, Japan).
The surgical indication of our study were patients with mild varus OA (femoral-tibial angle [FTA] of 180° or less, defined as the angle between the anatomical axis of the femur and the tibia in the anteroposterior [AP] view of the knee joint) with primary degenerative changes in the medial compartment and no degenerative changes in the lateral compartment and patellofemoral joint. Patients with inflammatory diseases such as rheumatoid arthritis, complications from spontaneous osteonecrosis of the knee, advanced OA of KL4, history of past knee ligament injury, and history of ipsilateral lower extremity fracture, past surgical history of meniscus or cartilage injury were excluded. For radiographic measurements, full-length anteroposterior standing plain radiography of the lower extremity were performed with the patella facing forward before surgery and at 1-year postoperatively. The FTA, hip-knee angle (HKA-negative value: varus, positive value: valgus), KJLO (negative value: varus, positive value: valgus), TPI (angle between the floor and tangential line; positive value: lateral inclination at the tibial plafond, negative value: medial inclination), talar tilt (TT, angle between the tibial plafond and talar dome), weight bearing line ratio (WBL ratio, the distance between the medial edge of the proximal tibia and the point at which the Mikulicz line intersects the proximal tibia, divided by the width of the tibial plateau) (Fig. 1), and the relationship between the pre-to postoperative changes in each measured value and intraoperative correction angle were examined. Radiological measurements were taken using OP-A (Fujifilm Corp., Tokyo, Japan). All radiological evaluations and measurements were conducted by three orthopaedic surgeons. Reliability of measurement were assessed by intra-class correlation coefficient (ICC). ICC were 0.83–0.96. Statistical analyses were performed using SPSS Statistics version 22.0 (IBM Japan, Ltd., Tokyo, Japan). Preoperative and 2-year postoperative clinical evaluations were conducted using the pain subscale of Knee Injury and Osteoarthritis Outcome Score (KOOS).
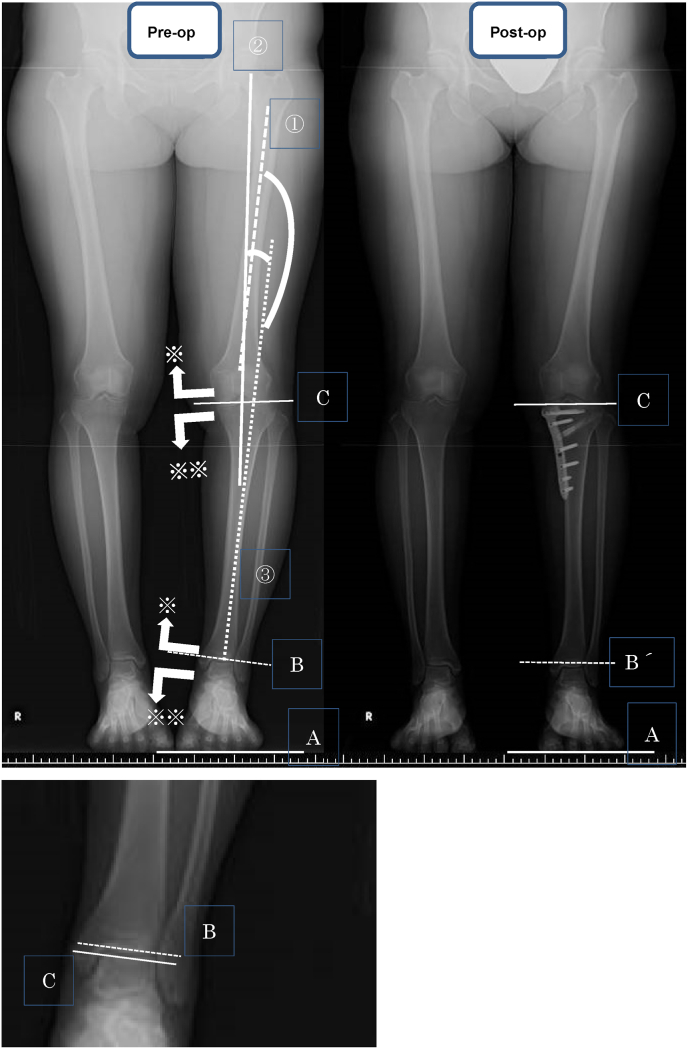
Fig. 1.
Measurement of FTA is defined as the angle between the femoral (①) and tibial (②) anatomical axis, and HKA is defined as the angle between the femoral (③) and tibial (②) mechanical axis. Measurement of KJLO. The angle between the floor (A) and the tangent of the medial/lateral tibial condyles (C) in the full-length standing anteroposterior view of the lower extremity is defined as KJLO. Valgus and varus alignment are defined as positive (※) and negative (※※), respectively. The angle between the floor and distal tibial articular surface (B, B′) is defined as the TPI, wherein the lateral inclination is positive (※) and medial inclination is negative (※※). In most cases, the postoperative TPI changes from a lateral inclination to a neutral alignment. The angle between the tibial plafond and talar dome (B,C) is defined as TT.
2.3. Statistical analysis
Statistical analyses were performed using SPSS Statistics version 22.0 (IBM Japan, Ltd., Tokyo, Japan). The paired t-test and Wilcoxon signed-rank test were used to compare the preoperative and mean values of the same item, and the unpaired t-test and Mann-Whitney U test were used to compare the TPI groups and the postoperative WBL ratio in Table 2. Both Pearson and Spearman's analyses were used for measuring correlations. The significance level was set to less than 0.01.
Table 2.
Comparison of pre- and post-operative WBL ratio between cases with small (less than 2°) and large (greater than 2°) pre-to post-operative changes in TPI. Although pre- and post-operative WBL ratio between cases with small and large pre-to post-operative changes in TPI were compared, there was no statistically significant difference in WBL ratio between the groups.
| WBL ratio | Pre- to post-op change in TPI (less than 2 deg; n=15) | Pre- to post-op change in TPI (greater than 2 deg; n=24) | P-value |
|---|---|---|---|
| Pre-op WBL ratio | 26.4 ± 12.8 | 25.7 ± 11.5 | 0.883 |
| Post-op WBL ratio | 59.3 ± 6.3 | 61.5 ± 5.1 | 0.288 |
3. Results
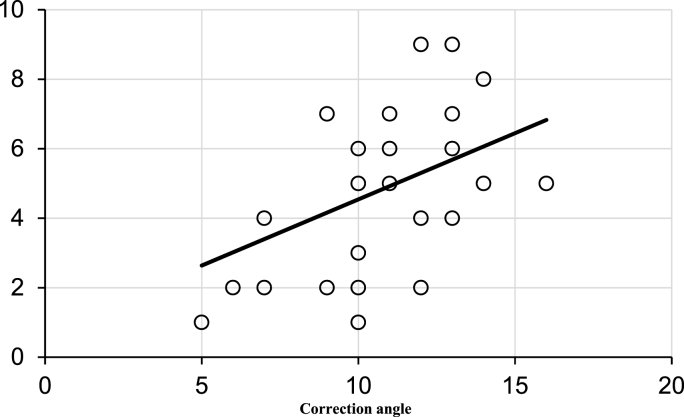
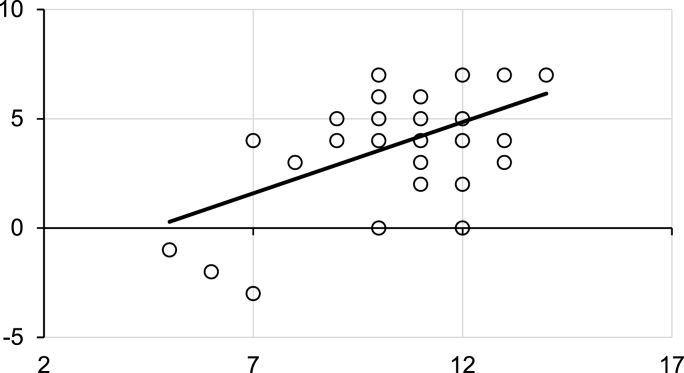
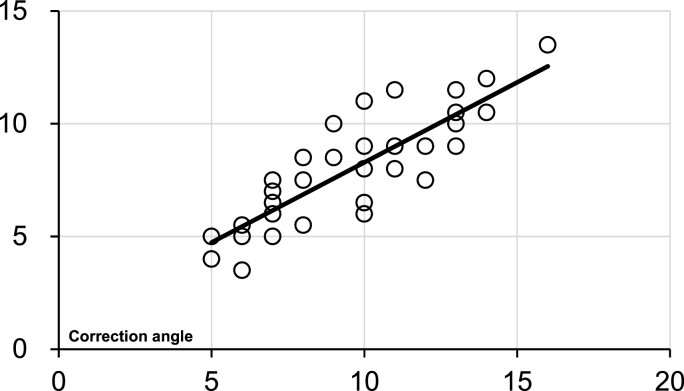
The mean pre- and postoperative values of each measurement were 179.8 ± 2.8 and 170.8 ± 2.4 for FTA, −4.8 ± 0.6 and 4.5 ± 1.3 for HKA, −0.5 ± 2.3 and 2.8 ± 2.8 for KJLO, and 4.0 ± 2.9 and 1.0 ± 2.2 for TPI, 0.6 ± 0.7 and 0.9 ± 0.8 for TT, 25.9 ± 8.2 and 60.8 ± 5.5 for WBL ratio, respectively. The mean pre-to post-operative changes were 9.0 ± 2.1 for FTA, 8.5 ± 3.2 for HKA, 3.2 ± 2.2 for KJLO, and 3.1 ± 2.5 for TPI, 0.2 ± 0.6 for TT, 35.1 ± 6.2 for WBL ratio, all of which showed significant postoperative differences except for TT. Although a mean difference of approximately 0.16° was observed between changes to the KJLO and TPI, no statistically significant difference was observed (Table 1). Both changes to the KJLO and TPI showed a significant correlation with the correction angle, and the knee joint demonstrated postoperative changes in the valgus direction with respect to the floor in all cases, and there were no cases that demonstrated changes in the varus direction (Fig. 2). In most cases, the ankle joint showed a tendency to improve horizontally from the preoperative lateral inclination (Fig. 1); however, the horizontal alignment changed from a preoperative neutral position to a medial inclination in 3 cases (Fig. 3, Fig. 4). In addition, the sum of changes to the KJLO and TPI showed a positive correlation that approximates the change in the correction angle (P = 0.006, Fig. 5). The mean pre- and postoperative KOOS subscales of pain were 50.2 ± 10.2 and 82.3 ± 9.1 (Table 3). Although the postoperative WBL ratio between patients with small (less than 2°) and large (greater than 2°) pre-to post-operative changes in TPI were compared, there was no statistically significant difference in the WBL ratio between the two groups (Table 2). There were no correlations between preoperative TPI, KJLO, pre-to post-operative change in TPI, KJLO, and postoperative KOOS subscale of pain (Table 4).
Fig. 2.
Correlation between pre-to postoperative changes in KJLO and correction angle. A positive correlation is confirmed between pre-to postoperative changes in KJLO and correction angle (P=0.06; correlation coefficient: 0.16).
Fig. 3.
Correlation between pre-to postoperative change in tibial plafond inclination and correction angle. The tibial plafond inclination changes from a lateral to medial alignment after surgery, and a correlation is observed with the correction angle (P<0.001; correlation coefficient: 0.519).Almost all cases shows improvement in the horizontal alignment with respect to the floor; however, 3 cases with preoperative neutral alignment with respect to the floor shows changes towards medial inclination after surgery.
Fig. 4.
A case shows a change from postoperative TPI to medial inclination. Surgery is performed with a correction angle of 6°. Although the preoperative TPI is 0° with a neutral alignment (A), a postoperative change is observed with a medial inclination of 2° (B).
Fig. 5.
Correlation between the sum of pre-to postoperative change (knee + tibial plafond inclination) and correction angle. The sum of changes to KJLO and the tibial plafond inclination shows a positive correlation with the correction angle. (P=0.006; correlation coefficient: 0.47).
Table 3.
Comparison of pre- and postoperative radiographic measurements and clinical evaluation. The FTA, HKA, and KLJO changed significantly in the valgus direction after surgery, and the tibial plafond inclination changed significantly in the medial direction (horizontal to the floor). Although the mean change in KJLO was approximately 0.16° greater than the tibial plafond inclination, no statistically significant difference was observed (∗; Wilcoxon signed rank test, P ≒ 0.88). There was no significant difference in pre-to postoperative changes in talar tilt. Postoperative KOOS was evaluated at 2 years after surgery. The pre-to post-operative KOOS was improved significantly.
| Parameter | Preoperative | Postoperative | Difference | P-value |
|---|---|---|---|---|
| FTA | 179.8 ± 2.8 | 170.6 ± 2.4 | 9.0 ± 2.1 | P<0.01 |
| HKA | −4.8 ± 0.6 | 4.5 ± 1.3 | 8.5 ± 3.2 | P<0.01 |
| KJLO | -0.5 ± 2.3 | 2.8 ± 2.8 | 3.2 ± 1.9 ※ |
P<0.01 |
| TPI | 4.0 ± 2.9 | 1.0 ± 2.2 | 3.1 ± 2.5 ※ |
P<0.01 |
| Talar tilt | 0.6 ± 0.7 | 0.9 ± 0.8 | 0.2 ± 0.6 | No significance |
| WBL ratio | 25.9 ± 11.7 | 60.8 ± 5.5 | 35.2 ± 6.2 | P<0.01 |
| KOOS | 51.3 ± 6.3 | 82.6± | 31.3 ± 8.4 | P<0.01 |
Abbreviations: FTA, femorotibial angle; HKA, hip-knee angle; KJLO, knee joint line obliquity.
Table 4.
Correlation between postoperative KOOS subscale of pain and preoperative KJLO, TPI, pre- and postoperative KJLO, and change in TPI.
| Parameters | Pre-op KJLO | Change in KJLO | Pre-op TPI | Change in TPI |
|---|---|---|---|---|
| P-value | 0.423 | 0.464 | 0.651 | 0.750 |
| Correlation Coefficient | −0.131 | −0.124 | -0.077 | −0.054 |
There was no correlation between preoperative TPI, KJLO, pre-to post-operative change in TPI, KJLO, and postoperative KOOS subscale of pain.
4. Discussion
From the results of this study, we confirmed that the alignment after OWHTO for varus OA with respect to the floor showed a tendency for the knee joint to shift from varus malalignment preoperatively to mild valgus postoperatively, and the ankle joint improved from a lateral inclination preoperatively to a neutral inclination postoperatively. However, in the TPI, there were neutral and well-aligned cases that shifted to a medial inclination. Subtalar compensation has been reported as a reason for the lateral inclination of the ankle joint to shift to a neutral alignment after surgery.2,8 Previous reports have described that the preoperative varus deformity of the ankle is compensated by the valgus alignment of the subtalar joint, and that the postoperative changes to the ankle in the valgus direction is compensated by the varus alignment of the subtalar joint.15 Changes in the deformity of the ankle joint due to varus knee OA is relatively mild and indicated for OWHTO, thereby enabling an easier subtalar compensation that results in many cases with good postoperative alignment of the ankle joint. However, the mobility of the subtalar joint can differ depending on the individual.16 Provided that the subtalar joint exhibits preoperative varus malalignment, subtalar compensation is less likely to occur. With less subtalar compensation, the knee and ankle joints are affected by the correction of OWHTO17; therefore, patients with normal preoperative alignment of the ankle joint may potentially worsen after surgery like the patient in Fig. 4, and we believe that caution should be exercised in performing the procedure.
Previous studies have reported on changes in foot and ankle alignment after OWHTO. Lee et al.3 reported that the amount of pre-to postoperative change in KJLO after correction was 4.1°, while the amount of change in distal TPI was approximately 6.8°. The authors suggested that the reason for the greater amount of change in TPI was due to the longer lever arm in the ankle joint that resulted from the osteotomy, making the moment of the force more likely to be applied. Choi et al.15 also reported similar findings in a separate study. Furthermore, the amount of pre-to post-operative change in the mechanical tibiofemoral angle has been reported to be close to the sum of the amount of change in KJLO and TPI.3 The present study also showed a positive correlation in which the correction angle was close to that of the sum of change in KJLO and TPI. The positive correlation that was observed in this study may have been due to patient inclusion that consisted of those with mild varus alignment and OA change in the knee joint before surgery. It is possible that these patients were less likely to be affected by soft tissues such as the medial collateral ligament during correction, in addition to the lack of OA change in the ankle joint with hindfoot compensation that may have enabled the amount of correction in the knee and ankle joints to directly affect changes in inclination. Moreover, no significant difference was observed between the amount of change in the TPI and KJLO, and no consistent trend was observed in the ratio between the correction angle and the amount of change in each measured value. The lack of significant difference in this study between the TPI and the amount of change in KJLO could be due to the preoperative TPI that was 4.0°, which was smaller than the 8.8° reported by Lee et al.3 and 7.4° reported by Choi et al.15 Because of the smaller inclination in the present study, we believe that change in TPI was unlikely to be affected. Miyazaki et al.2 reported that a larger deviation of the forefoot alignment (TPI + hindfoot alignment) results in an increased likelihood of under-correction in postoperative lower limb alignment. Although only the TPI was considered in this study, no effect on postoperative alignment correction was observed as a result of preoperative TPI and pre-to post-operative changes in TPI. A possible reason for this difference was that the preoperative mechanical axis of the study by Miyazaki et al. was 18.3% with a TPI of 6.2° and may be more prone to under-correction, considering that the surgical indication focused on preoperative varus alignment and ankle inclination. However, even in cases that exhibited a similar correction angle as with this study, there were cases with small changes in ankle joint inclination that resulted in substantial changes in KLJO. Although this did not affect short-term clinical results, we believe that cases should be observed with caution. Krause et al.17 reported in a cadaver study that the intra-articular pressure at the ankle increased when the tibia was put into varus after osteotomies around the knee. In cases with neutral preoperative TPI like the case in Fig. 4 of this study, the medial inclination of the ankle may have an adverse effect and should be carefully observed.
There were several notable limitations in this study. First, the TPI was evaluated on the distal tibial articular surface, which may have produced different results compared to an evaluation on the talar articular surface. Second, we did not evaluate the pre-to postoperative changes in alignment for the entire lower extremity, such as the hindfoot, ankle, and hip joint. Third, there were some variations in terms of the severity of OA and varus malalignment. Finally, the alignment was evaluated on the coronal plane alone.
From the results of this study, the alignment of OWHTO with respect to the floor in varus OA demonstrated that the knee joint changed from varus malalignment preoperatively to a mild valgus malalignment postoperatively, and the ankle joint showed a tendency to improve from a valgus malalignment preoperatively to neutral alignment postoperatively.
5. Conclusions
We examined the changes in KJLO and TPI after OWHTO for varus OA with a focus on their relationship to the correction angle. In terms of the postoperative alignment with respect to the floor, the knee joint changed from a preoperative varus malalignment to mild valgus malalignment, and the ankle joint showed a tendency to improve from a preoperative valgus malalignment to the postoperative neutral alignment. In addition, the sum of the two factors—changes to the KJLO and TPI—showed a positive correlation with the sum of changes in the correction angle.
Authorship
Conception and design of study: F.Kawashima, H.Takagi
Acquisition of data: F.Kawashima, H.Takagi
Analysis and/or interpretation of data:F.Kawashima,H.Takagi.
Drafting the manuscript: F.Kawashima,H.Takagi
Revising the manuscript critically for important intellectual content:F.Kawashima, H.Takagi.
Approval of the version of the manuscript to be published (the names of all authors must be listed):F.Kawashima,H.Takagi.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
All persons who have made substantial contributions to the work reported in the manuscript (e.g., technical help, writ-ing and editing assistance, general support), but who do not meet the criteria for authorship, are named in the Acknowledgements and have given us their written permission to be named. If we have not included an Acknowledgements in our manuscript, then that indicates that we have not received substantial contributions from non-authors.
References
- 1.Fujisawa Y., Masuhara K., Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 2.Miyazaki K., Maeyama A., Yoshimura I., Kobayashi T., Ishimatsu T., Yamamoto T. Influence of hindfoot alignment on postoperative lower limb alignment in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg. 2021 Jun 19 doi: 10.1007/s00402-021-04001-z. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 3.Lee K.M., Chang C.B., Park M.S., Kang S.B., Kim T.K., Chung C.Y. Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage. 2015;23:232–238. doi: 10.1016/j.joca.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Choi G.W., Yang J.H., Park J.H., et al. Changes in coronal alignment of the ankle joint after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:838–845. doi: 10.1007/s00167-015-3890-3. [DOI] [PubMed] [Google Scholar]
- 5.Gao F., Ma J., Sun W., Guo W., Li Z., Wang W. The influence of knee malalignment on the ankle alignment in varus and valgus gonarthrosis based on radiographic measurement. Eur J Radiol. 2016;85:228–232. doi: 10.1016/j.ejrad.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 6.Xie K., Jiang X., Han X., Ai S., Qu X., Yan M. Association between knee malalignment and ankle degeneration in patients with end-stage knee osteoarthritis. J Arthroplasty. 2018;33:3694–3698. doi: 10.1016/j.arth.2018.08.015. e1. [DOI] [PubMed] [Google Scholar]
- 7.Xie K., Han X., Jiang X., et al. The effect of varus knee deformities on the ankle alignment in patients with knee osteoarthritis. J Orthop Surg Res. 2019;134:14. doi: 10.1186/s13018-019-1191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takeuchi R., Saito T., Koshino T. Clinical results of a valgus high tibial osteotomy for the treatment of osteoarthritis of the knee and the ipsilateral ankle. Knee. 2008;15:196–200. doi: 10.1016/j.knee.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Michael E.H., Prodromos N., Antonios A.K., Ono Y., Nikolas D., Konstantinos N.M. Satisfactory functional and radiological outcomes can be expected in young patients under 45 years old after open wedge high tibial osteotomy in a long term follow up. Knee Surg Sports Traumatol Arthrosc. 2017;26:3199–3205. doi: 10.1007/s00167-017-4816-z. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence C.M., Jason C.H., Kwong Y.C., et al. Satisfactory long-term survival, functional and radiological outcomes of open wedge high tibial osteotomy for managing knee osteoarthritis: minimum 10 year follow up study. J Orthop Translat. 2020;26:60–66. doi: 10.1016/j.jot.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama H., Schröter S., Yamamoto C., et al. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc. 2018;26:1873–1878. doi: 10.1007/s00167-017-4680-x. [DOI] [PubMed] [Google Scholar]
- 12.Suero E.M., Sabbagh Y., Westphal R., et al. Effect of medial opening wedge high tibial osteotomy on intraarticular knee and ankle contact pressures. J Orthop Res. 2015;33:598–604. doi: 10.1002/jor.22793. [DOI] [PubMed] [Google Scholar]
- 13.Lee O.S., Lee S.H., Lee Y.S., Does Coronal Knee, Alignment Ankle. Affect recurrence of the varus deformity after high tibial osteotomy? Knee Surg Relat Res. 2018;30:311–318. doi: 10.5792/ksrr.18.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi J.Y., Song S.J., Kim S.J., Kim S.H., Park J.S., Suh J.S. Changes in hindfoot alignment after high or low tibial osteotomy. Foot Ankle Int. 2018;39:1097–1105. doi: 10.1177/1071100718773767. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka Y., Takakura Y., Hayashi K., Taniguchi A., Kumai T., Sugimoto K. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Br. 2006;88:909–913. doi: 10.1302/0301-620X.88B7.17325. [DOI] [PubMed] [Google Scholar]
- 17.Krause F., Barandun A., Klammer G., Zderic I., Gueorguiev B., Schmid T. Ankle joint pressure changes in high tibial and distal femoral osteotomies: a cadaver study. Bone Joint Lett J. 2017;99-B:59–65. doi: 10.1302/0301-620X.99B1.38054. [DOI] [PubMed] [Google Scholar]