1. BACKGROUND
Percutaneous coronary intervention (PCI) with Impella (Abiomed) support can be done using the same device's sheath to insert both the Impella pump and the PCI guiding catheter. This “single‐access” technique for protected PCI allows avoidance of multiple access sites and thereby has the potential to reduce the risk for access‐related complications. 1 Nevertheless, with the “classic” adoption of different access for PCI, postprocedural vessel integrity and hemostasis achievement can be checked at the time of Impella removal, 2 and this may prompt timely management of vascular complications to prevent major clinical consequences. 2 , 3 As a consequence, a possible drawback for single‐access protected PCI is that postprocedural hemostasis and arterial integrity cannot be angiographically checked. To overcome such possible limitations, we propose the following technical solution.
2. TECHNIQUE DESCRIPTION
We report a simple technique to be applied on top of the double preclosure technique that enables final angiographic examination of the access vessel following Impella pump removal in single‐access, Impella‐supported PCI.
A step‐by‐step description of this technique is as follows:
-
‐
Step 1: at the procedure start, two suture devices (ProGlide or ProStyle, Abbott Vascular) are implanted before the Impella sheath insertion according to the double preclosure technique.
-
‐
Step 2: at the procedure end, after Impella pump removal, a 0.35′ guidewire is inserted in the Impella sheath (Figure 1A).
-
‐
Step 3: the Impella sheath is removed and the two ProGlide's or ProStyle's node pushers are used to gently tighten the sutures to avoid bleeding (Figure 1B).
-
‐
Step 4: a diagnostic Judkins right (or pigtail) 4F catheter is advanced over the 0.35′ guidewire into the femoral artery, reaching the distal descending aorta (Figure 1C).
-
‐
Step 5: the 0.35′ guidewire is removed from the JR4 4F catheter and the catheter is connected to the injector (Figure 1D).
-
‐
Step 6: digital subtraction is performed to assess the integrity of the arterial axis and the absence of important blood leakage around the entry site (Figure 1E). At this stage, the recognition of vessel damages might be fixed using various endovascular techniques. In particular, iliac artery dissections might be fixed by reinserting a sheath (of appropriate size), allowing to deliver the selected devices (balloons/stents); significant residual entry site leaks might be fixed by reinserting the 0.35′ guidewire and adding an additional hemostatic device (either suture‐based or plug‐based). Of note, not all possible complications are expected to be fixed using the same single access: additional endovascular techniques may require other bail‐out arterial accesses (see Section 3).
-
‐
Step 7: if angiographic control confirms the achievement of acceptable hemostasis and the absence of arterial damages deserving intervention, the 0.35′ guidewire is inserted into the 4F catheter (to avoid its kinking), the 0.35′ guidewire/4F catheter system is removed, and the ProGlide's node pushers are used to tighten the sutures to complete hemostasis (Figure 1F).
Figure 1.
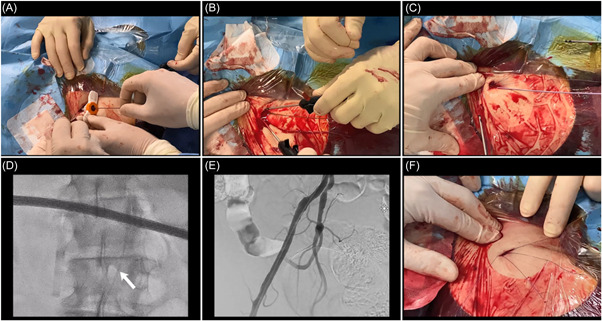
Procedural steps after Impella‐protected percutaneous coronary intervention with preimplantation of two suture devices (ProGlide or ProStyle). (A) After Impella pump removal, 0.35′ guidewire insertion into Impella sheath. (B) The Impella sheath is removed and the node pushers are used to gently tighten the two sutures. (C) A diagnostic JR4 4F is advanced over the 0.35′ guidewire into the femoral artery reaching the descending aorta. (D) The 0.35′ guidewire is removed from the JR4 4F catheter and the catheter is connected to the injector. (E) Digital subtraction is performed to assess arterial integrity. (F) The 0.35′ guidewire is inserted into the 4F catheter to avoid kinking. Then the 0.35′ guidewire/4F catheter system is removed, and the device's node pushers are used to tighten the sutures in order to complete hemostasis.
3. DISCUSSION
Impella‐protected PCI has an emerging role in the management of patients with complex coronary artery disease not amenable for surgical myocardial revascularization. 4 Such procedures require large‐bore sheath insertion, with which vascular damage risk is not negligible. 5 Since vascular complication risk is increased in the presence of multiple arterial accesses, the single‐access technique for protected PCI is gaining popularity. 1 When dealing with all percutaneous procedures needing large‐bore devices, prompt recognition of vascular complications at the end of the procedure might help implement a series of endovascular techniques that may prevent the occurrence of catastrophic clinical consequences. 6 Thus, angiographic confirmation of the entire iliac‐femoral axis integrity is advisable in the context of any Impella‐protected PCI. In the specific context of single‐access Impella‐protected PCI, angiography (either retrograde or antegrade with the help of a diagnostic catheter) can easily be done by the sheath before its removal, allowing prompt recognition and treatment of complications at the level of the iliac arteries. However, this technique is limited in that it is not feasible in the presence of impaired flow at the level of the sheath (in the case of small femoral artery size), or if the Impella sheath has been removed. Operators practicing Impella‐protected PCI are often using femoral hemostatic devices, and among these, suture‐based devices were adopted early. 3 , 7 Thus, we refined the herein reported simple technique allowing systematic antegrade angiography of the entire iliac‐femoral arterial axis to be applied on top of suture‐based hemostasis. The use of diagnostic 4F catheters as compared with other selections (like 4F sheaths) allows reduction of the residual hole at the femoral entry site, and the ability to perform, with single contrast injection, an antegrade check of the entire vessel. A different technique has been recently described by Summers et al. to achieve the same goal when a plug‐based hemostatic device is selected. 8 The recognition of vascular damage should prompt tailored management using various endovascular techniques that may be practiced via either the same or alternative access. 6 In particular, other access approaches like the contralateral femoral, the radial, or a different, recently described ipsilateral approach might be considered according to the complication type, location, and endovascular device availability. 9
4. CONCLUSIONS
In conclusion, this technique allows single‐access Impella‐protected PCI the potential to obtain postprocedural antegrade angiographic control. Furthermore, this technique can also be considered to check access‐site integrity anytime suture‐device‐based hemostasis is attempted in the presence of high‐risk features (imperfect entry site, adverse vascular anatomy, etc.).
AUTHOR CONTRIBUTIONS
Conceptualization: Francesco Burzotta, Enrico Romagnoli, Cristina Aurigemma, and Carlo Trani. Investigation: Piergiorgio Bruno, Stefano Cangemi, and Francesco Bianchini. Writing—review, and editing: Enrico Romagnoli, Cristina Aurigemma, and Carlo Trani. Writing—original draft: Francesco Burzotta. All authors have read and approved the final version of the manuscript. The corresponding author, Francesco Burzotta, had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICTS OF INTEREST
Dr. Burzotta, Dr. Trani, Dr. Romagnoli, and Dr. Aurigemma disclose to have received speaker's fees from Abbott, Abiomed, Medtronic, and Terumo. The authors declare that these companies had no role in the study design, collection, analysis, or interpretation of data and the decision to submit the report for publication. As reported in the acknowledgment section, Dana Bentley, MWC®, an employee of the device manufacturer (Abiomed), provided auxiliary medical writing services.
TRANSPARENCY STATEMENT
The corresponding author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
Dana Bentley, MWC®, an employee of the device manufacturer (Abiomed), provided auxiliary medical writing services.
Burzotta F, Romagnoli E, Aurigemma C, et al. A simple technique to obtain postprocedural antegrade angiographic control in single‐access Impella‐protected PCI. Health Sci. Rep. 2022;5:e709. 10.1002/hsr2.709
DATA AVAILABILITY STATEMENT
The authors are open to share, upon justified request to the corresponding author by qualified researchers trained in human subject confidentiality protocols, didactic video from a patient in whom this technique has been applied.
REFERENCES
- 1. Wollmuth J, Korngold E, Croce K, Pinto DS. The single‐access for hi‐risk PCI (SHiP) technique. Catheter Cardiovasc Interv. 2020;96:114‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burzotta F, Russo G, Previ L, Bruno P, Aurigemma C, Trani C. Impella: pumps overview and access site management. Minerva Cardioangiol. 2018;66:606‐611. [DOI] [PubMed] [Google Scholar]
- 3. Burzotta F, Trani C, Doshi SN, et al. Impella ventricular support in clinical practice: collaborative viewpoint from a European expert user group. Int J Cardiol. 2015;201:684‐691. [DOI] [PubMed] [Google Scholar]
- 4. Burzotta F, Crea F. “Protected” PCI: time to act. Minerva Cardioangiol. 2018;66:547‐550. [DOI] [PubMed] [Google Scholar]
- 5. Chieffo A, Ancona MB, Burzotta F, et al. Observational multicentre registry of patients treated with IMPella mechanical circulatory support device in Italy: the IMP‐IT registry. EuroIntervention. 2020;15:e1343‐e1350. [DOI] [PubMed] [Google Scholar]
- 6. Dato I, Burzotta F, Trani C, Crea F, Ussia GP. Percutaneous management of vascular access in transfemoral transcatheter aortic valve implantation. World J Cardiol. 2014;6:836‐846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Burzotta F, Paloscia L, Trani C, et al. Feasibility and long‐term safety of elective Impella‐assisted high‐risk percutaneous coronary intervention: a pilot two‐centre study. J Cardiovasc Med (Hagerstown). 2008;9:1004‐1010. [DOI] [PubMed] [Google Scholar]
- 8. Summers MR, Lavigne PM, Mahoney PD. Completion peripheral angiography in single‐access, Impella‐assisted, high‐risk PCI: using a buddy microcatheter sheath after MANTA closure for imaging and potential bailout. Catheter Cardiovasc Interv. 2022;99:1778‐1783. [DOI] [PubMed] [Google Scholar]
- 9. Shah A, Lodhi A, Bianco M, Kaluski E. Ipsilateral protection and bailout for large‐bore access. J Invasive Cardiol. 2021;33:E658‐E661. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are open to share, upon justified request to the corresponding author by qualified researchers trained in human subject confidentiality protocols, didactic video from a patient in whom this technique has been applied.


