Abstract
This study was conducted experimentally to evaluate the effect of neuro-linguistic programming (NLP) on fear of COVID-19 in kidney transplant patients. The study was carried out between June 2021 and October 2021. The Personal Information Form and COVID-19 Fear Scale (FCV–19S) were used to collect data. The obtained data obtained were evaluated using the SPSS 25 software. NLP was found to reduce the fear of COVID-19 in kidney transplant patients. Clinical nurses can use NLP techniques to support patients with fear in similar patient groups. Patients can be provided with access to training programs where they can learn NLP techniques.
Clinicaltrials.gov
Keywords: COVID-19, Fear, Kidney transplant, Neuro-linguistic programming, Nursing
1. Introduction
COVID-19 can increase death and morbidity, especially in certain high-risk groups. It has been reported that the mortality rate in groups at risk can reach up to 49%. Among these groups, older adults, diabetes and hypertension patients, chronic kidney disease patients, obese individuals, coronary heart and lung disease patients, those receiving chronic immunosuppression therapy, and organ transplant patients are at highest risk [[1], [2], [3]]. After organ transplants, patients require lifelong immunosuppressive therapy. It has been reported that mortality was higher in kidney transplant recipients than in other transplants recipients during the COVID-19 pandemic [4,5]. This may lead to an increased fear of COVID-19 in patients.
In addition to the physiological effect of COVID-19, serious psychological issues can arise from virus contamination, incubation period, geographical coverage, number of infected people, quarantine procedures, and suspicious information about the real death rate. “Fear” is among the emerging psychological problems [6,7]. Studies conducted in high risk groups show that patients have a high level of fear of COVID-19 [[7], [8], [9]]. Although moderate level of fear can increase compliance to public health measures (for example, handwashing and social distancing) and decrease participation in unsafe behaviors, experiencing high levels of fear may be associated with important psychological problems [1,6,10]. Fear, which is a psychological symptom, is also a nursing diagnosis and needs intervention due to the problems it creates. Identifying and managing fear in patients has an important place in the nursing profession. Nurses should monitor whether patients are experiencing fear, and if they detect fear, they should develop and implement strategies to solve it [11,12].
Although there are several treatments for psychological problems, non-drug methods such neuro-linguistic programming (NLP) have started to attract attention in recent years [[13], [14], [15]]. People want to have control over their own lives [16]. With NLP, the individual realizes their existing power. NLP is easy to learn, easy to apply, and an effective method for various problems [[13], [14], [15],17]. NLP is a method that allows people to change the neural programming of any situation or emotional perception with various techniques and is similar to body-mind therapies in this respect. The meaning of the word “neurological” can be described as the processing of information obtained through the five senses by neurons. The linguistic aspect of the technique refers to the fact that language is the basis for the organization of ideas and communication. The term programming recognizes that ideas and behaviors can be changed and manipulated to create desired results. NLP allows one to decipher the origin of individual words and speech. In this way, people feel, think, speak, and can therefore manage their own emotions [13,18].
There are studies that show that NLP is useful in coping with many psychological problems, including fear [[13], [14], [15]]. It is known that kidney transplant recipients are among the patient groups who are most vulnerable to COVID-19 and have high risk of infection [19] and may therefore experience fear. It is important to keep fear at tolerable levels as how the life of an infected individual will be affected by this virus cannot be predicted, and it is not known when the pandemic will end or whether a definite cure will be found [1,20,21]. When the literature was examined, no study was found on the effect of NLP on fear of COVID-19 in kidney transplant patients. Nurses are the first to notice patients' fear and refer patients for support with psychiatrists and psychologists. In addition, nurses can support patients by teaching non-invasive, inexpensive methods such as NLP that patients can use on their own. In this context, this study was performed to determine the effect of NLP on the fear of COVİD-19 in kidney transplant patients who have a high level of fear of COVID-19.
1.1. Study hypotheses
H0
The application of NLP in kidney transplant recipients has no effect on reducing the fear of COVID-19.
H1
: NLP application in kidney transplant recipients is effective in reducing the fear of COVID-19.
2. Materials and methods
2.1. Objective and type of study
This study was conducted experimentally (prospective randomized single-blind clinical trial model) to evaluate the effect of NLP on fear of COVID-19 in kidney transplant patients.
2.2. Place and time
This study was conducted at a university research hospital between June 2021 and October 2021.
2.3. Population and sample
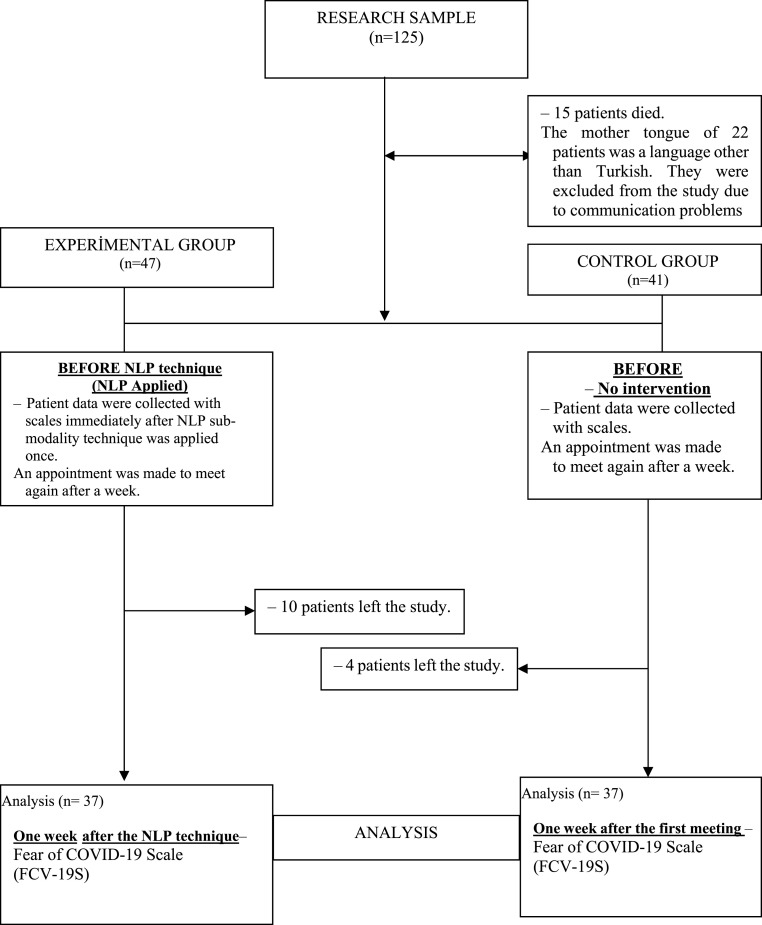
The population of the study consisted of patients who received kidney transplants in the hospital where the study was conducted. The sample of the study was determined by using the power analysis method. Using G*power 3.1 software, the sample size was calculated to be 74 (37 in each group) with an effect size of 0.80, a margin of error of 0.05, a confidence level of 0.95, and a population representation of 0.95. [22,23] Simple random sampling method, a probability sampling method, was used to determine the participants. Single-group columns between 1 and 300 were created using the Random Integer Generator method, which can be found in the Numbers sub-heading of the random.org website, for the participants who met the sample selection criteria. Participants were randomly assigned to numbers 1 and 2, considering the numbers 1 and 2 in the column. [22,23] Sample selection and assignment to groups were made by a researcher other than the principal researcher who did not practice NLP. The size of experimental (NLP sub-modality technique will be applied) or control groups was determined by drawing lots at the beginning of the study. Participants were individuals who were discharged from the hospital. There was no interaction between the groups since the data were obtained by interviewing them over phone, and the patients did not know which group they were in. A total of 125 participants in the randomization list were called by phone, [22] participants were excluded from the study due to communication problems, and 15 participants were excluded due to death after kidney transplant. Ten participants from the experimental group and 4 participants from the control group left the study. The study was completed with 74 participants. Details are given in Fig. 1 .
Fig. 1.
Study design.
2.4. Inclusion criteria and exclusion criteria
Patients who could communicate verbally, had no hearing problems, had a high or moderate fear of COVID-19 (20 or more), and had not applied NLP previously were included in the study. Patients who wanted to leave voluntarily at any stage after being included in the study, and who had to be hospitalized again for organ rejection or any other reason while the study was ongoing, were not included in the study.
2.5. Data Collection instruments: the personal information form and fear of COVID-19 scale (FCV–19S) were used to collect data
Personal Information Form: The personal information form created by the researchers in line with the literature [1,6,8] consisted of 16 questions related to personal information of the patients (age, sex, educational status, marital status, economic status, occupation, reason for transplant, time elapsed after transplant, degree of donor affinity, place of residence, family structure, previous diagnosis of psychiatric illness, years of kidney disease prior to transplant, history of other chronic diseases, history of past surgery, and methods used to cope with fears in daily life).
Fear of COVID-19 Scale (FCV–19S): The Turkish validity and reliability study of the scale created by Ahorsu et al. (2020) was conducted by Satıcı et al. This Likert-type scale consists of 7 items coded as “1: Strongly Disagree, 2: Disagree, 3: Neutral, 4: Agree, 5: Strongly Agree”. It was determined that there was no reverse item in the scale. The total score of the scale reflects the level of fear of COVID-19 experienced by the individual. The scores can range from 7 to 35. A high score on the scale means a high level of fear of COVID-19. The Cronbach's alpha value of the scale was found to be 0.84 [24,25]. Pearson correlation coefficient was used because the variables included in the study showed normal distribution. In the validity analysis, two values were calculated as composite reliability (CR) and average variance extracted (AVE). The results obtained from the CR value analysis, which shows the extent a latent variable is represented by the observed variables, were generally in line with the calculated Cronbach α values. CR results should be 0.70 and above. The AVE value, which indicates the average variance that can be explained in the observed variables to which a theoretically unobservable structure is associated, must be greater than the unexplained variance and 0.50 [26]. The AVE value of the participants in the experimental group was 0.59 and the CR value was 0.86 for the COVID-19 initial scores, and the AVE value was 0.55 and the CR value was 0.85 for the control group. The scale used was determined to be valid and reliable. For the fear of COVID-19 final scores, the AVE and CR values of the experimental group participants were 0.58 and 0.86, respectively. For the control group, the AVE and CR values were 0.53 and 0.84, respectively. The scale used was determined to be valid and reliable.
2.6. Data Collection
Data were collected from July 1, 2021 to August 1, 2021. The author, who is also a certified NLP practitioner, spoke to the patients by phone. Patients who had undergone kidney transplantation were called by phone, given information about the study, and their verbal consent was obtained.
2.7.1. Patients in the experimental group: After administering the personal information form and Fear of COVID-19 Scale (FCV–19S) to the patients in the experimental group, the sub-modality technique of NLP was applied once, and then FCV-19S was administered again one week later. Before the first interview ended, the participants were informed that they would be called one week later, on the same day, at the same time. One week later, the patients were called on the same day and time by phone, and the FCV-19S was applied.
*Sub modality Technique: People experience the world with their five senses, and the thoughts that an individual creates in his brain about a situation are coded with these five senses. When these encodings change, the individual's perception of the situation also changes. Individual emotion is encode in the brain as weight, size, sound, shape and color. When these encodings are changed, the feeling that disturbs the individual also changes. For this, programs in which people encode emotions can be learned, and emotion exchange is done by enabling the person to use their imagination [27].
For the fear of COVID-19, the following procedure was followed in this study. Each patient was asked questions about these codes in the same way and in the same order. They were then asked if they would like to keep this fear at a reasonable level. Patient consent was obtained (each patient reported that he wanted to keep it at a reasonable level). To reduce fear, the patient was asked to imagine what he was about to say as if it was happening even if he knew it was not really. Patient consent was awaited (each patient agreed). From the answers given by the patient, it was understood which representation system was the most effective in the patient. While some patients emphasized size specifically, some gave more detailed information about temperature, color, or shape. Emotion change was achieved by changing these codes using the imagination process.
2.7.2. Patients in the control group: The personal information form and the COVID-19 fear scale were applied once and no intervention was carried out. Before the first interview ended, the participants were informed that they would be called one week later, on the same day, at the same time. One week later, the patients were called on the same day and time by phone, and the FCV-19S was applied. The administration of the personal information form and the scale took an average of 10–15 min for each patient.
When the characteristics of the participants included in the study were examined, it was seen that the majority of patients were male, unemployed, and married (Table 1 ); the mean age of both groups (experimental and control) was 41.73 years (Table 2 ). The experimental and control groups were similar in terms of demographics (Table 1).
Table 1.
Demographic information of participants.
| Variable | Group | Experimental (NLP) |
Control |
||
|---|---|---|---|---|---|
| Number (n = 37) | Percent | Number (n = 37) | Percent | ||
| Gender | Female | 14 | 37,8 | 9 | 24,3 |
| Male | 23 | 62,2 | 28 | 75,7 | |
| Education Level | Primary-Secondary School | 13 | 35,1 | 23 | 62,2 |
| High School | 16 | 43,2 | 7 | 18,9 | |
| University and above | 8 | 21,6 | 7 | 18,9 | |
| Marital Status | Married | 24 | 64,9 | 26 | 70,3 |
| Single | 13 | 35,1 | 11 | 29,7 | |
| Occupation | Housewife | 7 | 18,9 | 9 | 24,3 |
| Employee | 2 | 5,4 | 1 | 2,7 | |
| Civil servant | 8 | 21,6 | 6 | 16,2 | |
| Self-employment | 6 | 16,2 | 3 | 8,1 | |
| Retired | 4 | 10,8 | 9 | 24,3 | |
| Unemployed | 10 | 27,0 | 9 | 24,3 | |
| Transplant Reason | Acute Kidney Failure | 16 | 43,2 | 11 | 29,7 |
| Chronic Kidney Failure | 21 | 56,8 | 26 | 70,3 | |
| Donor Type | 1st Degree Relative | 15 | 40,5 | 8 | 21,6 |
| 2nd Degree Relative | 12 | 32,4 | 6 | 16,2 | |
| Spouse | 4 | 10,8 | 2 | 5,4 | |
| Friend | 1 | 2,7 | 12 | 32,4 | |
| Cadaver | 5 | 13,5 | 9 | 24,3 | |
| Past Surgery | Yes | 17 | 45,9 | 16 | 43,2 |
| No | 20 | 54,1 | 21 | 56,8 | |
| The Method of Coping with Fear in Daily Life | Nothing | 26 | 70,3 | 24 | 64,9 |
| Finding a Hobby | 1 | 2,7 | 3 | 8,1 | |
| Praying | 10 | 27,0 | 10 | 27,0 | |
| Income Level | High | 1 | 2,7 | ||
| Middle | 21 | 56,8 | 22 | 59,5 | |
| Low | 15 | 40,5 | 15 | 40,5 | |
Descriptive statistics (mean, standard deviation, minimum and maximum value) of the demographic information of the patients included in the study were calculated, and the results are given in Table 2 below.
Table 2.
Descriptive statistics of participants' demographic information.
| Variable | Mn ± SD | Min | Max |
|---|---|---|---|
| Years Passed After Transplant | 4,07 ± 2,38 | 1,00 | 10,00 |
| Duration of Kidney Disease | 7,57 ± 5,02 | 1,00 | 21,00 |
| Age | 41,73 ± 12,26 | 21,00 | 64,00 |
Mn; mean, SD; Standard Deviation, Min; Minimum value obtained, Max; Maximum value obtained.
2.7. Data Analysis
The analysis of the data obtained from the research was carried out using SPSS 25 software. Whether the data conformed to the normal distribution was checked with the Kolmogorov–Smirnov Test. The significance level (p) for the comparison tests was set at 0.05. Since the normal distribution was achieved in the variables (p > 0.05), the analysis was continued with parametric test methods. In the comparisons of independent paired groups, the significance test of the difference between the two pairs (two paired samples t-test) was used since the assumption of normality was ensured, and repeated measures analysis of variance was used to test whether there was a difference between the groups in repeated measurements. Multiple normal distribution and homogeneity of variance were controlled in the analyses.
2.8. Ethical aspects of the study
The ethics committee of the faculty gave approval for this study, and this study was conducted in compliance with the Declaration of Helsinki. The institution where the study was conducted also gave written permission (Approval Number: EE93629378-60.,01–30510). Moreover, verbal consent from the individuals participating in the study was obtained. After the completion of the study, NLP was applied to the control group patients.
3. Results
The demographic information of the patients included in the study was calculated as numbers and percentages, and the results are given in Table 1; p > 0.05 shows that the two groups were similar.
Whether the mean values of the Fear of COVID-19 Scale (FCV–19S) Scores varied according to time both within and between groups (experimental and control) was tested, and the results are given in Table 3 .
Table 3.
Intra-group and inter-group comparison of fear of COVID-19 scale scores.
| Variable | Fear of COVID-19 | Mn ± SD | Intra-Group |
Inter-Group |
|||
|---|---|---|---|---|---|---|---|
| F value | p1 value | F value | p2 value | Ƞ | |||
| Experiment (NLP) | First | 22,92 ± 3,30 | 206,481 | 0,001* | 120,11 | 0,001** | 0,625 |
| Last | 14,32 ± 3,12 | ||||||
| Control | First | 22,14 ± 2,25 | 1276 | 0,262 | |||
| Last | 21,46 ± 4,41 | ||||||
Mn; Mean, SD; Standard Deviation, p1 value; the result of the intra-group comparison significance test, p2 value; ANOVA significance test result in repeated measures between groups, Ƞ; Eta value *p < 0,05 There is a statistically significant difference between intra-group measurements. **p < 0,05 There is a statistically significant difference between the groups.
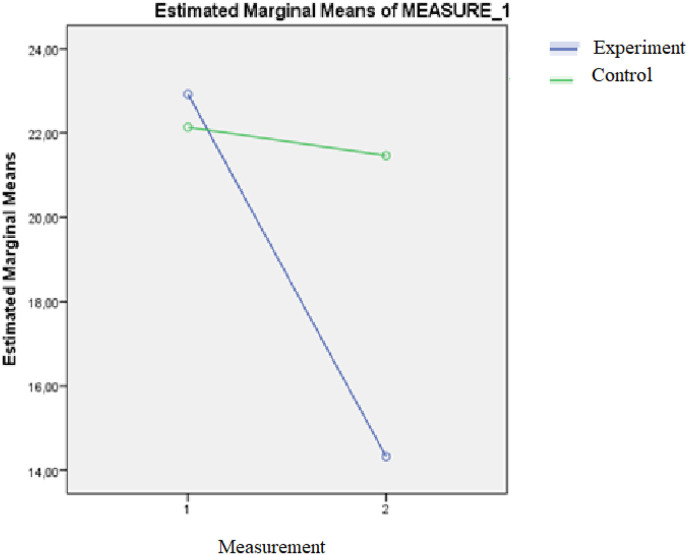
In the experimental group, the mean of the first measurement of the fear of the COVID-19 scale was 22.92 ± 3.30, and the last measurement was 14.32 ± 3.12. The value obtained in the second measurement was significantly lower than the value obtained in the first measurement (p < 0.05, Table 3). In the control group, the mean of the first measurement of the COVID-19 fear scale was 22.14 ± 2.25, and the final measurement was 21.46 ± 4.41. The value obtained in the second measurement was not significantly lower than the value obtained in the first measurement (p > 0.05, Table 3). In the patients included in the study, there was a significant difference in the changes in the COVID-19 fear scale between the first measurement and the second measurement according to time between the experimental and control groups (p < 0.05, Table 2), and 62.5% (Ƞ = 0.625) of the variation between the measurements in time difference was explained by the groups. The interaction graph of the measurements is given in Fig. 2 .
Fig. 2.
Interaction graph of the measurements of the experimental (NLP) and control groups.
4. Discussion
Patients who have end-stage renal disease need renal replacement therapy for maintaining their kidney function. However, each medical and surgical treatment methods has advantages, disadvantages, and different effects on the physical, psychological and social health of patients. One of the focuses of care in the perioperative period is to control psychological factors along with the patient's physical recovery and prevention of rejection [[28], [29], [30]].
As a result of this study, it was found that the majority of the patients did not do anything to cope with fear in daily life. According to previous studies, the majority of individuals do not use any method to cope with fear [20,31]. Fear is an emotion caused by one's own thoughts. A fear reaction arises because there is “danger” in the content of these thoughts. Most of the time, people who experience fear do not find an effective solution because they do not know that fear can be caused by their own thoughts, and they may experience desperation and bring their fear to a level of crisis. These crises also increase avoidance behaviors and decrease the potential to enjoy life [20,21,31]. Experiencing high levels of fear brings along physiological problems along with symptoms such as anxiety, depression, and insomnia [1,6,10]. For all these reasons, it is of great importance to develop strategies to eliminate fear [6,10,20,21].
In this study, kidney transplant patients who had a high level of fear of COVID-19 were included in the experimental and control groups, and in several studies, it is seen that the fear of COVID-19 is high in transplant patients [7,32,33]. It is thought that the high level of fear in transplant patients is related to the easy contagiousness of COVID-19, its prevalence, relationship with level of immunity, and the continued increase in mortality rates [7,32,33]. Cellular immunity plays an important role in COVID-19. Transplant patients whose immune system is suppressed as a result of long-term use of immunosuppression become a potential risk group for COVID-19. Due to its rapid spread and serious morbidity and mortality, COVID-19 generates a significant fear in society [1,3,7,19,32].
The mean of the first measurement of the Fear of COVID-19 Scale (FCV–19S) in the experimental group was 22.92 ± 3.30, and the last measurement was 14.32 ± 3.12. The value obtained in the second measurement was significantly lower than the value obtained in the first measurement. In the control group, the mean of FCV-19S first measurement was 22.14 ± 2.25, and the last measurement was 21.46 ± 4.41. The value obtained in the second measurement was not significantly lower than the value obtained in the first measurement. The changes in FCV-19S between the first measurement and the second measurement according to time in the patients included in the study significantly differed between the experimental and control groups. The variation of 62.5% (Ƞ = 0.625) between the measurements in the time difference is explained by the groups. While there was a serious decrease in FCV-19S score in the experimental group, less decrease was observed in the control group. As a result, the hypothesis of “H1: NLP application in kidney transplant recipients is effective in reducing the fear of COVID-19.” was confirmed.
When the literature was examined, no study was found in which the fear of COVID-19 was addressed using the NLP in kidney transplant patients. However, there are studies indicating that NLP application reduces fear in individuals [[34], [35], [36], [37]]. In this study, positive attitude and goal setting were promoted to overcome the fear of COVID-19 using NLP techniques in the interviews, and the sub-modality technique was used. According to NLP assumptions, people have the resources they need. In goal setting studies with NLP, the resources to be used while moving from the current situation to the desired situation were focused on, and awareness of their resources was created in patients [[36], [37], [38]]. With the help of NLP studies, patients found the courage and ability to cope with negative emotions, felt able to reach the goals they set, and the fear of COVID-19 decreased. According to NLP assumptions, mind and body are part of a system, and the unconscious mind balances consciousness. With NLP techniques, patients are prepared both physically and mentally. Since every behavior has a structure, it has been emphasized that if change can be created in mental programs, change can be achieved in feelings, thoughts, and attitudes toward COVID-19 [[37], [38], [39], [40]]. It is thought that this change may be the reason for the decrease in the COVID-19 fear scores in the NLP group. The effectiveness of NLP studies on the patient's fear of COVID-19 may be due to the fact that calibration and a safe communication environment were provided in the interviews, and relief was obtained with breathing exercises. It may also depend on the fact that target setting and decision-making studies have been carried out for COVID-19. Finally, the constant emphasis on the assumptions of “A person has all the resources he needs” and “every behavior has a positive intention at its core” can have an impact on the effectiveness of NLP. According to NLP, “mind and body form a magnificent system working together” [[38], [39], [40]]. In this study, both mental and physical preparation suggestions were given to cope with the fear of COVID-19, and the implementation of the relevant practices may have been effective in reducing the fear. The use of NLP techniques may have increased patients' belief that they can cope with the difficulties they encounter more effectively.
4.1. Conclusion and recommendations
In this study, NLP intervention was found to reduce the fear of COVID-19 in kidney transplant patients. An individualized care plan should be created for patients and support should be provided with a multidisciplinary approach. Every application will enable patients to enjoy life a little more and reduce the fear of COVID-19. Clinical nurses can use NLP in their application preferences for fear in similar patient groups. Patients can be provided with access to training programs where they can learn NLP practice. In this study, which was carried out with an experimental design, there were two groups, the experimental group and the control group. In future studies, a third group in which a different approach is used may be included in the study. Thus, it will be possible to compare the effect of NLP on fear of COVID-19 with a different approach.
4.2. Limitations and strengths of the study
There are a limited number of randomized controlled studies using NLP techniques in the field of nursing care. This study is the first randomized controlled trial to examine the effect of NLP on fear of COVID-19 in kidney transplant patients. In this study, important results were found on the effectiveness of NLP techniques to reduce the fear of COVID-19 in kidney transplant patients. Although the study has its strengths, it also has limitations. Due to the COVID-19 pandemic, interviews could not be conducted face-to-face and therefore a single NLP technique was applied. Another limitation of this study is that because there is no active comparator condition, it is difficult to know if the decrease in fear is related to the validation participants in the intervention group received or/and the attention they got from the researcher as being part of the intervention group.
Funding
During the present study, no financial support was received from institutions or organizations.
Author contributions
Study design: AD, RD, TM, HBB; Manuscript writing: AD, RD, TM, HBB; Data Collection: AD, RD; Data Analysis: FK; Study Supervision: AD, RD, TM, HBB; Critical revisions for important intellectual content: AD, RD, TM, HBB.
Declaration of competing interest
There is no conflict of interest between the authors and/or family members regarding this study.
Acknowledgment
We are grateful to all the individuals who participated in the study.
References
- 1.Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2020:1–14. doi: 10.1007/s11469-020-00281-5. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng Z., Peng F., Xu B., et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J. Infect. 2020;81(2):e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pereira M.R., Mohan S., Cohen D.J., et al. COVID-19 in solid organ transplant recipients: initial report from the US epicenter. Am. J. Transplant. 2020;20(7):1800–1808. doi: 10.1111/ajt.15941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Godara S., Saraf K., Sadasukhi T.C., et al. COVID-19 infection in kidney transplant recipients: a single centre study from Northern India. Indian J. Nephrol. 2021;31(6):535. doi: 10.4103/IJN.IJN_571_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raja M.A., Mendoza M.A., Villavicencio A., et al. COVID-19 in solid organ transplant recipients: a systematic review and meta-analysis of current literature. Transplant. Rev. 2021;35(1) doi: 10.1016/J.TRRE.2020.100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gritsenko V., Skugarevsky O., Konstantinov V., et al. COVID 19 fear, stress, anxiety, and substance use among Russian and Belarusian university students. Int. J. Ment. Health Addiction. 2020:1–7. doi: 10.1007/s11469-020-00330-z. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reuken P.A., Rauchfuss F., Albers S., et al. Between fear and courage: attitudes, beliefs, and behavior of liver transplantation recipients and waiting list candidates during the COVID‐19 pandemic. Am. J. Transplant. 2020;20(11):3042–3050. doi: 10.1111/ajt.16118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guven D.C., Sahin T.K., Aktepe O.H., Yildirim H.C., Aksoy S., Kilickap S. Perspectives, knowledge, and fears of cancer patients about COVID-19. Front. Oncol. 2020;10:1553. doi: 10.3389/fonc.2020.01553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stankovska G., Memedi I., Dimitrovski D. Coronavirus COVID-19 disease, mental health and psychosocial support. Society Register. 2020;4(2):33–48. doi: 10.14746/sr.2020.4.2.03. [DOI] [Google Scholar]
- 10.Çobaner A.A. Vol. 37. İletişim Kuram ve Araştırma Dergisi; 2013. (Sağlık İletişiminde Korku Öğesinin Kullanımı: Sigara Paketlerinde Kullanılan Sigara Karşıtı Görsellerin Göstergebilimsel Analizi). [Google Scholar]
- 11.Jomar R.T., Bispo VR. de S. The most common nursing diagnosis among adults/seniors hospitalised with cancer: integrative review. Ecancer Med. Sci. 2014;8:462. doi: 10.3332/ECANCER.2014.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doğan R., Kaplan Serin E., Bağcı N. Fear of COVID 19 and social effects in liver transplant patients. Transpl. Immunol. 2021;69 doi: 10.1016/J.TRIM.2021.101479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HemmatiMaslakpak M., Farhadi M., Fereidoni J. The effect of neuro-linguistic programming on occupational stress in critical care nurses. Iran. J. Nurs. Midwifery Res. 2016;21(1):44. doi: 10.4103/1735-9066.174754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotera Y., Sheffield D., Van Gordon W. The applications of neuro-linguistic programming in organizational settings: a systematic review of psychological outcomes. Hum. Resour. Dev. Q. 2019;30(1):101–116. doi: 10.1002/HRDQ.21334. [DOI] [Google Scholar]
- 15.Kotera Y., Van Gordon W. Japanese managers' experiences of neuro-linguistic programming: a qualitative investigation. J. Ment. Health Train Educ. Pract. 2019;14(3):174–185. doi: 10.1108/JMHTEP-06-2018-0033/FULL/PDF. [DOI] [Google Scholar]
- 16.Doğan R., Doğan A., Bağci N. The effect of neuro-linguistic programming on depression, anxiety and stress in liver transplant patients. Med Records. 2022;4(1):102–110. doi: 10.37990/medr.1031528. [DOI] [Google Scholar]
- 17.Doğan A., Saritaş S. The effects of neuro-linguistic programming and guided imagery on the pain and comfort after open-heart surgery. J. Card. Surg. 2021;36(7):2389–2397. doi: 10.1111/JOCS.15505. [DOI] [PubMed] [Google Scholar]
- 18.Bandler R., Grinder J. In: NLP Değişim İçin Beyninizi Kullanın: Nöro-Linguistik Programlama. 5. Baskı. Çeviri, Akınhay O., editors. Alfa Yayınları; 2016. [Google Scholar]
- 19.Soylu D., Ceyhan Ö., Tekinsoy Kartın P. Nursing care in managing risk factors of metabolic syndrome after kidney transplant. Arch. Med. Rev. J. 2019;28(1):60–65. doi: 10.17827/aktd.381352. [DOI] [Google Scholar]
- 20.Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Chin. J. Ind. Hyg. Occup. Dis. 2020;38(3):192–195. doi: 10.3760/CMA.J.CN121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 21.Yıldırım M., Geçer E., Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2021;26(1):35–43. doi: 10.1080/13548506.2020.1776891. [DOI] [PubMed] [Google Scholar]
- 22.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. 2009;41(4) [DOI] [PubMed] [Google Scholar]
- 23.Cohen J. Vol. 2. Taylor & Francis INC; Edition: 1988. (Statistical Power Analysis for the Behavioral Sciences). [Google Scholar]
- 24.Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Satici B., Tekin E.G., Deniz M.E., Satici S.A. Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00294-0. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kılınc E., İnceoğlu F., Aktas K. İş Yükü Fazlalığının Psikolojik Sermayeye Etkisi: Ulaşım Sektöründe Bir Araştırma. Social Sci. Studies J. 2019;5(35):2586–2596. doi: 10.26449/SSSJ.1500. [DOI] [Google Scholar]
- 27.Karunaratne M. Neuro-linguistic programming and application in treatment of phobias. Compl. Ther. Clin. Pract. 2010;16(4):203–207. doi: 10.1016/J.CTCP.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Clayton P.A., McDonald S.P., Russ G.R., Chadban S.J. Long-term outcomes after acute rejection in kidney transplant recipients: an ANZDATA analysis. J. Am. Soc. Nephrol. 2019;30(9):1697–1707. doi: 10.1681/ASN.2018111101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dąbrowska-Bender M., Dykowska G., Żuk W., Milewska M., Staniszewska A. The impact on quality of life of dialysis patients with renal insufficiency. Patient Prefer. Adherence. 2018;12:577. doi: 10.2147/PPA.S156356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamran F., Ogden J. Transitions in psychological well-being and life orientation: the phenomenon of post traumatic growth after renal transplantation. Pakistan J. Psychol. Res. 2016;31:419–440. [Google Scholar]
- 31.Cao W., Fang Z., Hou G., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr. Res. 2020 doi: 10.1016/J.PSYCHRES.2020.112934. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Klaveren C.W., De Jong P.G.M., Hendriks R.A., et al. Topics, delivery modes, and social-Epistemological dimensions of web-based information for patients undergoing renal transplant and living donors during the COVID-19 pandemic: content analysis. J. Med. Internet Res. 2020;22(10) doi: 10.2196/22068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kute V., Varugese S., Prasad N., Shroff S., Agarwal S. Renal transplant guidelines with reference to COVID-19 infection. Indian J. Nephrol. 2020;30(3):176–178. doi: 10.4103/IJN.IJN_221_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hafid A., Pruitt K.D. Neurolinguistic programming in practice: more Empirical than magical. EC Psychol. Psychiatry. 2021;10(3):93–104. doi: 10.31080/ecpp.2021.10.00841. [DOI] [Google Scholar]
- 35.Arroll B., Henwood S. Rapport The Magazine for NLP Professionals Special NLP Conference. Vol. 54. 2017. NLP research, equipoise and reviewer prejudice; pp. 24–26. 2017. [Google Scholar]
- 36.Passmore J., Rowson T.S. Neuro-linguistic-programming: a critical review of NLP research and the application of NLP in coaching. Int. Coach. Psychol. Rev. 2019;14(1):57–69. [Google Scholar]
- 37.Silverman G.M., Sahoo H.S., Ingraham N.E., et al. NLP methods for extraction of symptoms from unstructured data for use in prognostic COVID-19 analytic models. J. Artif. Intell. Res. 2021;72:429–474. doi: 10.1613/JAIR.1.12631. [DOI] [Google Scholar]
- 38.Carriere J., Shafi H., Brehon K., et al. Case report: utilizing AI and NLP to assist with healthcare and rehabilitation during the COVID-19 pandemic. Frontiers Artificial Intelligence. 2021;4 doi: 10.3389/FRAI.2021.613637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bose P., Roy S., Ghosh P. A comparative NLP-based study on the current trends and future directions in COVID-19 research. IEEE Access. 2021;9:78341–78355. doi: 10.1109/ACCESS.2021.3082108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Das R., Pal A., Paul M., Mandal A. In: Intelligent Modeling, Prediction, and Diagnosis from Epidemiological Data: COVID-19 and beyond. Bhattacharyya S., editor. CRC Press; 2021. Exploring twitter data to understand the impact of COVID-19 pandemic in India using NLP and deep learning; p. 137. [Google Scholar]