Abstract
Introduction
People with mild cognitive impairment (MCI) are at increased risk of decreasing cognitive functioning. Computerised cognitive training (CCT) and nutrition have been shown to improve the cognitive capacities of people with MCI. For each variable, we developed two kinds of interventions specialised for people with MCI (CCT: ‘individualised’ CCT; nutrition: a whole-food, plant-based diet). Additionally, there are two kinds of active control measures (CCT: ‘basic’ CCT; nutrition: a healthy diet following the current guidelines of the German Nutrition Society). The aim of this study is to investigate the effects of the two interventions on cognition in people with MCI in a 2×2 randomised controlled trial with German participants.
Methods and analysis
Participants will be community-dwelling individuals with a psychometric diagnosis of MCI based on the Montreal Cognitive Assessment (MoCA) and Mini-Mental State Examination. With N=200, effects with an effect size of f≥0.24 (comparable to Cohen’s d≥0.48) can be detected. Screening, baseline, t6 and t12 testing will be conducted via a videoconferencing assessment, telephone, and online survey. Participants will be randomly allocated to one of four groups and will receive a combination of CCT and online nutritional counselling. The CCT can be carried out independently at home on a computer, laptop, or tablet. Nutrition counselling includes 12 online group sessions every fortnight for 1.5 hours. The treatment phase is 6 months with follow-ups after six and 12 months after baseline.
Ethics and dissemination
All procedures were approved by the Friedrich-Alexander-Universität Erlangen-Nürnberg Ethics Committee (Ref. 21-318-1-B). Written informed consent will be obtained from all participants. Results will be published in peer-reviewed scientific journals, conference presentations.
Trial registration number
ISRCTN10560738.
Keywords: GERIATRIC MEDICINE, Old age psychiatry, Delirium & cognitive disorders, NUTRITION & DIETETICS
Strengths and limitations of this study.
This study is being conducted completely remotely: videoconferencing assessments with valid telehealth assessments for cognitive function, telephone-based interviews, computerised cognitive test battery, computerised cognitive training (CCT) and online nutritional group counselling.
Randomised controlled trial with two interventions with an active control group for each component and longitudinal character of the study with an intervention period of 6 months, follow-ups after 6 and 12 months, and an open phase (planned) in which study participants might be assessed once a year.
Individualised CCT for the intervention group by means of a machine learning system that chooses computerised exercises that match the person’s level of difficulty by estimating the person’s likelihood of successfully solving the computerised exercises (‘individualised’ CCT).
Highly innovative curricular nutrition intervention based on current clinical evidence, tailored for people with mild cognitive impairment (MCI).
Methodological limitations might include a restriction to participants who feel comfortable with the use of technology; have internet access and own a computer, laptop or tablet; and have MCI as their only psychometric diagnosis without a clinical diagnosis.
Introduction
In the general population, the prevalence of mild cognitive impairment (MCI) defined by Petersen1 increases with age, at 6.7% for ages 60–64 and up to 25.2% for ages 80–84.2 People with MCI have a higher risk of progressing to dementia than cognitively normal individuals.1 3 For example, Inui et al4 found that 72% of patients with amnestic MCI progressed to Alzheimer’s disease (AD) over 5 years. Thus, MCI seems to be the optimal period for intervention before a conversion to dementia occurs.
There is currently no high-quality evidence to support pharmacological treatments for MCI.2 However, there is ample evidence showing that cognitive training is a significant modifiable risk factor for MCI or dementia.5–11 Only recently, a systematic review and meta-analysis concluded that evidence-based suggestions on AD prevention include cognitive activity.12 Computerised cognitive training (CCT) is an effective alternative to paper-and-pencil cognitive training with comparable or better effect sizes in cognitively healthy community-dwelling older adults.13 One important advantage is that the participants get instant feedback. Moreover, CCT can be custom-tailored for each participant while adapting task difficulty to individual performance.14 A considerable amount of research evaluating the effects of CCT for people with MCI has been done during the last decade.15 Various systematic reviews and meta-analyses of CCT intervention studies have already demonstrated positive (even though sometimes just moderate) effects on improving the cognitive capacity of people with MCI,15–20 for example, with Hedges’ g=from 0.23 to 0.52 for global cognitive functioning.15 16 20
Nutritional therapy is an essential part of medicine with clinical implications for a large number of disciplines. Hence, 70% of all chronic diseases are in some way associated with diet.21 Cohort studies and randomised controlled trials (RCTs) have demonstrated beneficial effects of nutrition on cognitive functioning, especially related to three types of diet: the Mediterranean Diet, the Dietary Approaches to Stop Hypertension (DASH Diet) and the Mediterranean-DASH Intervention for Neurodegenerative Delay Diet.22–25 All three above-mentioned diets are predominantly whole-food plant-based (WFPB) diets, primarily containing vegetables, whole grains, legumes, fruits, nuts and seeds, are rich in polyunsaturated and monounsaturated fatty acids, and contain hardly any processed foods.26 Furthermore, the diets are associated with reductions in various inflammatory markers.27–29 Since MCI seems to be accompanied by inflammatory processes,30 and exclusively plant-based foods contain bioactive substances, such as phytochemicals and fibre, which have anti-inflammatory properties,31 there is an obvious need to further investigate potential neuroprotective effects of plant-based nutrition in the context of clinical MCI studies. Since cardiometabolic diseases are associated with the occurrence of dementia,32 and weight loss is associated with improved attention and memory performance,25 it can be hypothesised that a well-planned anti-inflammatory, neuroprotective, plant-based diet has the potential to alleviate symptoms of MCI and the progression to dementia.
The aim of the proposed study is to examine the effects of CCT and online nutritional group counselling on the cognition of people with MCI in a completely digital RCT. We developed CCT and online nutritional group counselling, both specialised for people with MCI: individualised CCT (iCCT) targeting information processing speed, memory-span, short-term memory and decision making, and nutritional group counselling focusing on a WFPB diet. Additionally, there are two active control measures: basic CCT (bCCT) aiming on simple strategies and long-term memory, and nutritional group counselling focusing on a healthy diet recommended by the German Nutrition Society (Deutsche Gesellschaft für Ernährung, DGE diet). This manuscript describes the study protocol while following the evidence-based reporting guidelines of the SPIRIT statement.33
Methods and analyses
Aims and hypothesis
Research hypotheses
Primary hypothesis I: iCCT will lead to statistically significantly greater improvements in cognitive capacities during the intervention period of 6 months compared with bCCT.
Primary hypothesis II: Online nutritional group counselling focusing on a WFPB diet will lead to statistically significantly greater improvements in cognitive capacities during the intervention period of 6 months compared with online nutritional group counselling focusing on a healthy diet recommended by the German Nutrition Society.
Secondary hypothesis: iCCT in combination with online nutritional group counselling focusing on a WFPB diet will have a positive interaction effect. The group with iCCT in combination with online nutritional group counselling focusing on a WFPB diet will show more cognitive improvements than all other groups during the intervention period of 6 months in people with MCI.
Exploratory study question
Are there changes in the course of depression and activities of daily living (ADLs) during the 12-month observation period?
Study design and setting
A prospective 2×2 randomised controlled intervention study is being conducted to test the abovementioned hypotheses. The overall start date of the study was on 1 June 2021. Recruitment will begin on 3 January 2022 and will continue until 30 September 2022. Because the study is being conducted completely remotely, individuals from all over Germany can participate. At baseline, all study participants will be randomly assigned to one of four intervention arms (combination of iCCT or bCCT and group counselling on WFPB diet or DGE diet). The CCT intervention is double-blind, the online nutritional group counselling is single-blind. Since the principal usefulness of CCT is well known,15–20 it would be unethical to use a control group without any CCT. After baseline testing (t0), the participants will receive one of the two computerised training applications for their computer, laptop or tablet. It is recommended that they use the application at least 30 min per day 3 days a week during the 6-month intervention phase. Both computerised training applications contain the same computerised cognitive test battery (ccTB) that will be delivered and collected once a month (t0-t12). After the end of the 6-month intervention phase, all participants will be free to continue to use the application. The online nutritional group counselling sessions will focus on either a WFPB diet or a DGE diet. Both groups will receive curricular online nutritional group counselling at regular 14-day intervals for 1.5 hours (12 appointments total per participant over a period of 6 months, online group setting in a fixed group, max. 20 participants per group). The intervention phase is from t0 to t6. Follow-up is planned after six (t6) and 12 (t12) months. The open phase of the study will begin after t6 in order to test the hypotheses and exploratory study questions until t12. A follow-up study is planned to observe the participants after t12. Table 1 contains the trial registration data.
Table 1.
Trial registration data
| Data category | Information |
| 1. Primary registry and trial identification no | ISRCTN |
| 2. Date of registration in primary registry | 23 November 2021 |
| 3. Secondary identifying numbers | – |
| 4. Source(s) of monetary or material support | Karl and Veronica Carstens-Stiftung |
| 5. Primary sponsor | Karl and Veronica Carstens-Stiftung |
| 6. Secondary sponsor(s) | – |
| 7. Contact for public queries | see point 8 |
| 8. Contact for scientific queries | Prof. Dr. Elmar Graessel, elmar.graessel@uk-erlangen.de PD Dr. Christian Kessler, M.A., christian.kessler@charite.de |
| 9. Public title | BrainFit-Nutrition: Intervention study for people with mild cognitive impairment (MCI) using computerised cognitive training (CCT) tools and a nutrition intervention |
| 10.Scientific title | CCT tools and online nutritional group counselling for people with MCI: Study protocol of a completely digital, randomised, controlled trial |
| 11.Countries of recruitment | Germany |
| 12.Health condition(s) or problem(s) studied | MCI |
| 13.Intervention(s) | Participants will be randomly allocated to one of four groups with two intervention variables (BrainFit and Nutrition):
|
| 14.Key inclusion and exclusion criteria | Inclusion criteria:
|
Exclusion criteria:
| |
| 15.Study type | Prospective double-blind randomised controlled clinical intervention study |
| 16.Date of first enrolment | Starting on 03 January 2022 |
| 17.Target sample size | 200 |
| 18.Recruitment status | Not yet recruiting |
| 19.Primary outcome(s) | Cognition measured by the MoCA at baseline and after 6 months |
| 20.Key secondary outcome(s) | Cognitive Function measured by the MMSE at baseline and after 6 and 12 months Cognition measured by the computerised cognitive test battery integrated in the digital software at baseline and after 6 and 12 months Depression measured by the PHQ-9 at baseline and after 6 and 12 months Activities of daily living (ADL) measured by the Bayer ADLs Scale (B-ADL) at baseline and after 6 and 12 months |
WFPB, whole-food, plant-based.
Data will be collected by means of psychometric tests and structured interviews using videoconferencing, telephone and an online survey. The data will be collected by trained student assistants who have no knowledge of group allocation at any time. Two days before baseline testing (t0), the study participants will receive an email with a link to download the software for their version of the computerised application and instructions on how to download and instal the software.
Sample size estimation
A power analysis was computed with 200 participants distributed to the two groups of the 2×2×2 factorial variance-analytical experimental design with one repeated measure (factor 1: two CCTs; factor 2: two types of online training for dietary modification, factor 3: two time points). With 50 participants in each group, α=0.05, β=0.20 (corresponding to a power of 80%), a correlation between repeated measures of 0.5, and a nonsphericity correction of 1, we will have the power to detect effects with an effect size of f≥0.24 (comparable to Cohen’s d≥0.48).
Recruitment strategies
Participants will be recruited from the general population all over Germany. The project’s homepage was designed to provide information about the study. Also, an appointment for a screening can be made via the project homepage. We partnered with a health insurance company that is sending emails to their members aged 60 and above with information about the study and a link to the project homepage. About 25 000 members will receive an email with information about the study in 6 waves between December 2021 and May 2022.
Eligibility of participants
Individuals who are interested in the study can make an appointment for a screening via the project homepage. During the screening, we will offer an examination of basic cognitive functioning including a personal conversation about their screening results afterwards. Individuals who fulfil the criteria for inclusion will be informed about the study and asked to take part in the project.
Criteria for inclusion are: (1) MCI, psychometrically operationalised by a score on the MoCA ≤24 (cut-off for cognitive impairment) and at the same time a score on the Mini-Mental State Examination (MMSE) ≥24 (cut-off for no dementia), (2) possession of a computer (Windows/Linux/MacOS) with microphone and camera, laptop or Android tablet with access to the internet and basic skills in their use, (3) age ≥60 and (4) informed consent. Criteria for exclusion are (1) completely blind or deaf, (2) no personal computer, laptop, or tablet with access to the internet, (3) normal cognition, operationalised by a score on the MoCA >24, (4) dementia, operationalised by a score on the MMSE <24, (5) acute depression, operationalised by a score on the 9-Item Patient Health Questionnaire (PHQ-9)≥12 or (6) other psychiatric or neurologically diagnosed diseases (checklist): psychosis (schizophrenia, major depression, mania, bipolar psychosis), Parkinson’s disease, multiple sclerosis, several strokes, alcohol abuse/drug abuse (addiction), other serious brain disease (especially brain tumour, brain injury, hydrocephalus), or severe vitamin B deficiency.
The MMSE and the MoCA will be administered in combination to differentiate between normal cognition, MCI and dementia. The MoCA will be administered first to differentiate between normal cognition and MCI on the basis of the cut-off score of 24 points.34–36 The MMSE will be administered to differentiate between MCI and dementia on the basis of the cut-off score of 23 points.37 For these cut-offs, we will look for an optimised ratio of sensitivity and specificity. The criteria for a positive screening for MCI, normal cognition or dementia are shown in table 2.
Table 2.
Definition of MCI
| Normal cognition | MCI | Dementia | |
| Step 1: MoCA | 30–25 | 24 to 0 | 24–0 |
| Step 2: MMSE* | – | 30 to 24 | 23–0 |
| Decision | Exclusion | Inclusion | Exclusion |
*The MMSE will be applied only when the MoCA results are in the range of 24–0 points.
MCI, Mild cognitive impairment; MoCA, Montreal Cognitive Assessment; MMSE, Mini-Mental State Examination.
Randomisation
Our external biostatistics partner is creating computer-generated randomisation lists (Institute of Medical Informatics, Biometry and Epidemiology, Friedrich-Alexander Universität Erlangen-Nürnberg, Waldstraße 6, 91 054 Erlangen). All individuals meeting the inclusion criteria will be randomised into one of the four groups (combination of the CCT component: iCCT or bCCT and the online nutritional group counselling component: WFPB diet or DGE diet). Randomisation will be stratified by sex, age, MoCA score at screening. Residents of the same household will be assigned to the same group. Participants will not know which treatment condition they are in, and the student assistants who assess the outcomes of the study will be blind to participants’ allocation at all times.
Interventions
Computerised cognitive training
Both computerised applications (intervention and control) are available for Windows, MacOS and Linux PC/laptop and Android tablet.
iCCT for people with MCI
The exercises included in this training application have been selected to address the expected level of performance of people with MCI. All exercises are available with different levels of difficulty. The ten playful exercise tasks involve the basic parameters of information processing as well as short-term memory and require different types of decision making (see table 3). The initial difficulty levels of the exercises are determined by a machine-learning system, which uses (1) a (logistic regression) model that is based on data from people with MCI (individualised by considering each participant’s data) and (2) the cognitive status of the participant (ie, the results of the integrated ccTB) to estimate the likelihood of a participant’s success at a certain difficulty level for a task. The initial model is based on data collected prior to the study. The application chooses the highest level the participant is likely to solve as the entry level. With the machine learning system, individual (compensation) strategies are nullified, and the ideal level of difficulty for training is generated for each participant. Thus, the iCCT is aimed at improving the beneficial effects of CCT by providing exercises at the difficulty level that fits each participant best.
Table 3.
Computerised cognitive exercises
| CCT application | Group of tasks | Explanation | Key function | Cognitive domain (DSM-5) |
| Individualised CCT | Finding targets (‘Punkte sammeln’) |
For a set of pop-up pictures, participants must click on target pictures before they disappear | Sustained attention | Complex attention |
| Applying rules (‘Regel anwenden’) |
Select the winner or loser of a rock-paper-scissors game (either hand signs or in written form); if the game is presented with hand signs, the participant has to pick the winner; if presented with words, the loser has to be picked; this exercise has a time limit, depending on difficulty | Mental/cognitive flexibility | Executive function | |
| Layer sorting (‘Ebenen sortieren’) |
A target picture of a vase with flowers is presented; the participant has to reproduce the picture out of layers; easiest: background—foreground, up to five layers with distractors | Visuoconstructional reasoning | Perceptual-motor | |
| Jigsaw puzzle (‘Bild zusammensetzen’) |
Sorting of image sections | Visuoconstructional reasoning | Perceptual-motor | |
| Fill in the gaps (‘Felder füllen’) |
A grid has to be filled in according to rules; each symbol is used only once in every row, column and block; layout 4×4 to 9×9 fields | Working memory | Executive functions | |
| Remember cards (‘Karten merken’) |
Remember a row of (up to 5) cards; compare new card with fifth to last card | Working memory | Executive functions | |
| Find pairs (‘Paare finden’) |
Finding pairs of images in a pool; images covered; each turn two cards can be turned over | Visuo-spatial memory | Perceptual-motor | |
| Spot the difference (‘Unterschied erkennen’) |
A set of x identical pictures is presented, after a blank, the set and one extra picture are presented; the extra picture has to be selected | Visual perception | Perceptual-motor | |
| Pattern recognition (‘Schema erkennen’) |
A matrix of elements (combination of concentric geometrical figures) is presented; in one row or column, a figure is presented in the same position in all elements; the row/column has to be found; for small difficulties, hints are given | Decision making | Executive functions | |
| Word conversion (‘Wörter umwandeln’) |
Convert a source word to a target word in x steps; in each step, only one letter can be exchanged and each line must contain a word | Word finding | Language | |
| Basic CCT | Rotating picture puzzle (‘Drehpuzzle’) |
Picture is sectioned; sections are rotated; sections have to be turned in the right direction | Visuoconstructional reasoning | Perceptual-motor |
| Picture quiz (‘Bilder quiz’) |
Multiple-choice questions about images | Semantic and autobiographical long-term memory | Learning and memory | |
| Geography quiz (‘Länderspiel’) |
Knowledge quiz based on German federal states | Semantic and autobiographical long-term memory | Learning and memory | |
| Quiz-Show (‘Wissensquiz’) |
Quiz-show simulation with knowledge-based multiple-choice questions | Semantic and autobiographical long-term memory | Learning and memory |
CCT, computerised cognitive training; DSM-5, The Diagnostic and Statistical Manual of Mental Disorders.
bCCT (active control group)
This training application uses exercise tasks that are oriented towards quizzes and visual tasks (see table 3). The exercise tasks are playfully designed and require, among other things, simple strategies and long-term memory. Most of the exercises exist with only a single level of difficulty. The entry-level difficulties of the other exercises are determined solely by the participant’s prior successful results on this exercise. The exercises of the bCCT are aimed at providing enjoyable computerised leisure activities with a limited number of cognitive tasks for the active control group.
Online nutritional group counselling
These types of counselling are based on a structured curriculum including interactive methods and teaching materials, such as handouts, cooking instructions with recipes, and feedback and nutrition-related experience exchange rounds (see table 4). The use of different group work formats and alternating between a small-step introduction to the content and a person’s own elaboration, homework and reflection are aimed at maximising participants’ attention, participation and adherence. Furthermore, each participant receives a monthly delivery of a packet with selected food items. These deliveries are meant to be a useful complement regarding recommended products and are intended to invite the participants to get to know new and beneficial food items.
Table 4.
Overview of the 6-month online nutritional group counselling
| Session | Topic |
| 1 | Basics 1: Introduction, nutritional basics |
| 2 | Basics 2: Deepening knowledge about nutrition |
| 3 | Quantitative proportions and daily planning |
| 4 | Kitchen theory: Everything about storage, preparation, baking |
| 5 | Kitchen practice: Virtual buffet and virtual live show cooking |
| 6 | Scientific background - Impact of nutrition - Proteins |
| 7 | Carbohydrates, fibre |
| 8 | Oils, fats, nuts, seeds and drinks |
| 9 | Special nutrients, secondary plant substances, spices, age-specific nutrition |
| 10 | Circadian factors, periodic fasting |
| 11 | Mindful eating, stress and nutrition |
| 12 | Conclusion, evaluation, repetition |
Counselling focusing on a WFPB diet
In this group, a WFPB diet with anti-inflammatory, neuroprotective components is systematically taught and recommended as a regular diet. The WFPB diet essentially consists of vegetables, whole grains, legumes, fruits, nuts and seeds, without restricting energy intake (see table 5). In addition, the regular consumption of specific foods that have the potential to beneficially influence cognitive functions, based on current clinical evidence, is encouraged (eg, green leafy vegetables,38 mushrooms,39 citrus fruits,40 soy products,41 blueberries,42 nuts,43 turmeric,44 green tea45 and omega-3 fatty acids46). Participants are instructed to exclude animal products from their diets because of the proinflammatory potential of animal products and to refrain from consuming highly processed foods.47 Monthly delivery contains a selection of neuroprotective foods (eg, plant oil with polyunsaturated fatty acids, nuts, whole grains, green tea).
Table 5.
Recommendations of the nutrition interventions (per day, if not specified)
| Recommendations per day | WFPB | DGE |
| Vegetables | At least three portions (additionally 1 tbs of sea vegetables/algae) | three portions |
| Fruits | two portions | two portions |
| Cereals | Whole-grain, 3–4 portions | Whole-grain, 4 portions, incl. potatoes |
| Nuts and seeds | 1–2 portions | Not specified - mentioned as alternative for one fruit portion |
| Legumes | One portion | Not specified |
| Plant oil | 2–3 tbs (especially flax seed oil with DHA) | 1,5–2 tbs |
| Animal fats | Not recommended | 1,5–2 tbs (one tbs plant oil plus 15–30 g butter or margarine) |
| Milk products | Not recommended | three portions |
| Meat, poultry, fish, eggs | Not recommended | 300–600 g meat as well as 1–2 servings of fish (fatty, low-fat), 3 eggs per week plus 3 servings of sausage (à 30 g) |
| Milk alternatives | 1–3 portions | Not specified |
| Sweets, fried foods, fast foods | Not recommended | Max. 1 portion |
| Neuroprotective foods | Daily (eg, walnuts, flaxseed oil, berries, green leafy vegetables, herbs, etc) | Not specified |
DGE, Deutsche Gesellschaft für Ernährung; DHA, docosahexaenoic acid; WFPB, whole-food plant-based diet.
Counselling focusing on a diet recommended by the German Nutrition Society
Participants in this group will receive systematic recommendations according to the official guidelines of the DGE diet for healthy eating.48 This means they will be encouraged to establish an omnivorous diet based on vegetables, fruits and whole grains, including moderate intake of animal products, such as fish, poultry, red meat, eggs and milk products (see table 5). The DGE group will also be encouraged to prefer fresh, whole-food, non-processed foods and to reduce their consumption of saturated fatty acids, sweetened drinks or highly processed foods.48 49 Eating products coming from animals is also limited within the DGE context with a greater focus on vegetables, fruits and whole-grain cereals or bread. The delivery boxes will contain a selection of DGE-appropriate basic foods beneficial to health (eg, whole grain, plant-based oils or nuts/seeds, sugar alternatives, foods that are not very processed, vegetarian alternatives).
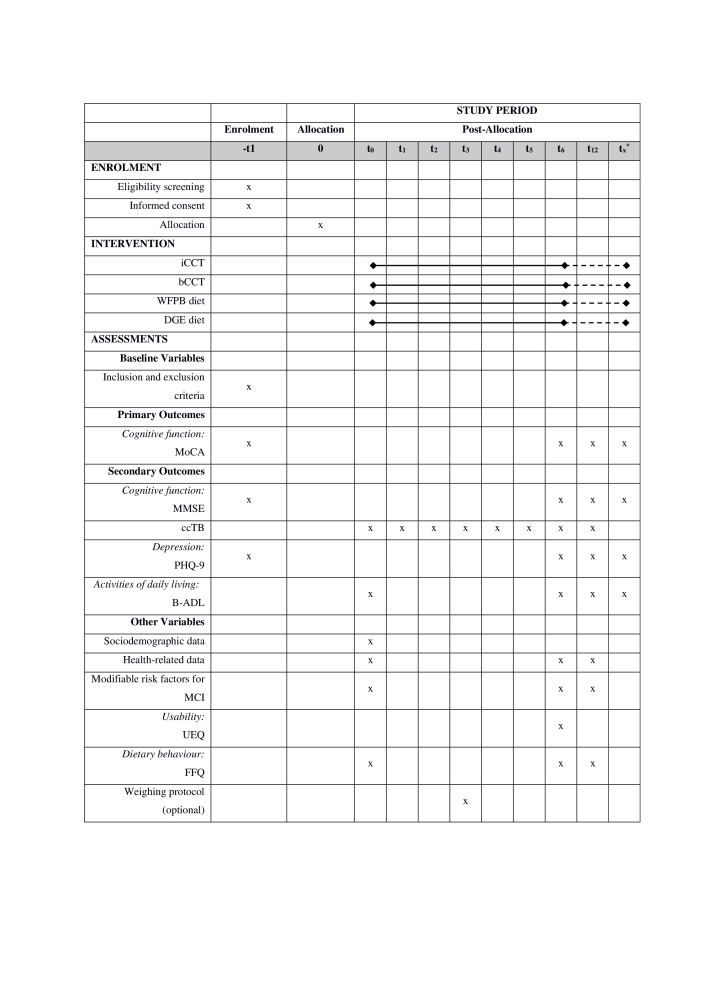
Measures
The data are being collected at baseline and follow-up by student assistants (psychology students) who are well trained to conduct performance tests and interviews via videoconferencing assessment or telephone and an online survey. The measures that are being used at the different measurement points are shown in figure 1.
Figure 1.
Timeline of measurements. *Intended for a follow-up study after t12. B-ADL, Bayer Activities of Daily Living Scale; bCCT, basic computerised cognitive training; ccTB, computerised cognitive test battery; DGE diet, diet recommended by the German nutrition Society (Deutsche Gesellschaft für Ernährung, DGE); FFQ, Food Frequency Questionnaire; iCCT, individualised computerised cognitive training; MCI, mild cognitive impairment; MoCA, Montreal cognitive assessment; MMSE, Mini-Mental state examination; PHQ-9, Patient health questionnaire; UEQ, User Experience Questionnaire; WFPB diet, whole-food plant-based diet.
Primary outcome measures
MoCA50: The MoCA is a performance test that is used to screen for MCI. It consists of more difficult items than the MMSE and is thus able to better detect MCI.50–53 The score ranges from 0 to 30 points, with higher scores indicating better cognitive performance. A score ≤24 indicates cognitive impairment.34–36 There are three parallel versions of the German translation of MoCA for videoconferencing being used. V.8.1 is conducted at t1 (screening), V.8.2 at t6 and V.8.3 at t12. The MoCA has been found to be an appropriate measure for cognitive screening and has good reliability and validity values.54
Secondary outcome measures
MMSE55: The MMSE is the most frequently employed screening test for dementia.56 It measures five areas of cognitive functioning: orientation, registration, attention and calculation, recall, and language. The score ranges from 0 to 30 points, with higher scores representing better cognitive performance. Values above 23 points are interpreted as ‘not demented’, whereas scores between 0 and 23 indicate a dementia syndrome.37 The reliability and validity of the MMSE has been established in numerous studies.37 57 58 For this study, the MMSE was adapted to an audiovisual setting based on Timpano et al.59 60
ccTB: Both versions of the computerised training application contain a set of exercises for measuring different cognitive abilities monthly, beginning at baseline. Eight tests are used to measure various cognitive abilities (see table 6).
Table 6.
Computerised cognitive test battery
| Test | Description | Adaptation of |
| Memory span I: Digit span, unsorted (‘Zahlen merken – unsortiert’) |
Rows of single digit numbers are presented (each for 1 s); the numbers must be reproduced immediately afterwards | WAIS-IV80, task Digit Span |
| Memory span II: Digit span, ascending (‘Zahlen merken – aufsteigend’) |
Like Memory span I; numbers must be reproduced in ascending order | WAIS-IV80, task Digit Span |
| Processing speed I: No Comparison (‘Zahlen vergleichen’) |
Comparison of two single-digit numbers separated by a horizontal line (participants should react if same no) | Pattern Comparison\Letter Comparison81 |
| Processing speed II: Symbol count (‘Symbole zählen’) |
Counting a target symbol in a pool as fast as possible | SKT82, task ‘counting symbols’ |
| Processing speed III: Numerical Stroop task (‘numerischer Stroop-Test’) |
Two single-digit numbers are presented in different sizes (congruent/incongruent mixed); no with higher value must be clicked as quickly as possible | Numerical stroop task83 84 |
| Short term memory I: Free recall (‘Wortliste – Erinnern’) |
12 objects have to be named; afterwards shown for 1 min; some tests later, the objects must be remembered | SKT82, task ‘delayed recall’ |
| Short term memory II: Cued recall (‘Wortliste – erkennen’) |
The objects from Short term memory I must be selected from a selection of 48 objects | SKT82, task ‘recognition recall’ |
| Logical reasoning: Matrices Test (‘Matrizentest’) |
In a (2×2 or 3×3) matrix of symbols, the bottom right symbol is missing; the composition rule has to be understood and the correct symbol must be selected | Raven’s Standard Progressive Matrices85 |
SKT, Syndrom-Kurz-Test (engl Short Cognitive Performance Test); WAIS-IV, Wechsler Adult Intelligence Scale-Fourth Edition.
The PHQ-961 62: The PHQ-9 is a short self-assessment tool often used in primary care settings to screen for depression.63 Its nine items cover the nine DSM-IV criteria by asking patients about their experiences during the last 2 weeks and are rated on a four-point scale ranging from 0 (‘not at all’) to 3 (‘nearly every day’). The total sum score suggests varying levels of depression. A cut-off ≥12 was found to show a good balance between sensitivity and specificity.64 The PHQ-9 was found to be a reliable and valid instrument for screening for depression.61
The Bayer ADL Scale (B-ADL)65: The B-ADL assesses difficulties in the performance of everyday activities. It comprises 25 items, which evaluate general ADL competencies and specific tasks important for management in everyday life. The frequency of difficulties the patient experiences in performing everyday activities is rated on a 10-point scale ranging from 1 (‘never’) to 10 (‘always’). A global score is computed by summing across all items and dividing by the number of items rated. The resulting score ranges from 1 to 10 with higher scores corresponding to more severe deficits.
Other variables
Questionnaire on sociodemographic and health-related data: sociodemographic data (age, sex, marital status, highest educational level, employment status, monthly income, household size) from a standardised questionnaire will be recorded by the student assistants at baseline. Modifiable risk factors for MCI (status of general mental activities, physical activities, social participation, sleeping habits, average liquid intake, eating habits, alcohol consumption, nicotine consumption, visual/hearing capacity) and health-related data (diseases, medications, body weight, body height, dementia cases in the family) will be recorded at baseline, t6 and t12.
User Experience Questionnaire (UEQ)66: The UEQ measures attractiveness, perspicuity, efficiency, dependability, stimulation and novelty of software with 26 bipolar items. The questionnaire consists of pairs of contrasting attributes (eg, ‘understandable’ vs ‘not understandable’) that can be rated on a 7-point Likert scale. The UEQ was found to show a satisfactory level of reliability and construct validity.66
Additional digital data: both CCTs track usage data. The usage data include the duration of use, difficulty, success and other parameters for each training task run.
Online Food Frequency Questionnaire (FFQ)67: A modified FFQ of the DEGS1-Survey from the Robert Koch Institute will be assessed as an online survey at baseline, t6 and t12 . It consists of questions about dietary behaviour from the past 4 weeks (on average), containing all relevant plant-based and animal-based foods as well as neuroprotective ingredients, to estimate the frequency of the consumption of different food groups.
Weighing protocol: After 3 months of intervention (t3) a non-obligatory weighing protocol (3 days: 2 working days/1 weekend day) will be emailed and is to be completed and scanned back or completed online.
Data collection
The data will be collected at baseline (t0) and at follow-up after 6 (t6) and 12 months (t12) (see figure 1). Annual follow-up studies will test for conversions to dementia. The trial will be conducted remotely. All data will be generated via videoconferencing, telephone, online survey or the ccTB that is integrated into the CCTs.
Testing with the MoCA and MMSE will be conducted via videoconferencing with the student assistants. Videoconferencing assessments with the MoCA and MMSE have very high reliability scores compared with face-to-face testing. The intraclass correlation coefficients (ICCs) for the MoCA and the MMSE have been demonstrated in several studies and go up to ICC=0.99 for the MoCA68 and up to ICC=0.92 for the MMSE.69 In a recent systematic review,70 the MoCA and the MMSE were described as valid telehealth measures for screening cognitive status. Telemedicine is an emerging new field, and there is evidence that it is a valuable tool for assessing neurodegenerative diseases.70–72
The questionnaire on sociodemographic and health-related data will be sent to the study participants to prepare them for the interview. The FFQ online survey and the non-obligatory weighing protocol will be emailed to participants and are to be completed and scanned back or completed online. The evaluation will be done pseudonymously via nutrition software with a food database (NutriGuide) to support the accuracy of the FFQ survey. During the 6 month intervention period, the usage data collected by the CCT, including the ccTB data, will be obtained from the participants. After the monthly ccTB assessment, consent to upload the CCT data will be requested. When consent is given, the data will be uploaded to the Erlangen study centre’s server. The server configuration prohibits downloads of the data by people who are not study team members. The data will be pseudonymised.
Data quality management and data protection
The student assistants involved in the study have been thoroughly trained for their tasks by the study centre’s staff. When the participants have questions concerning the computerised interventions or the online nutrition groups, they can email the study centre. The quality of the data will be guaranteed by strict data monitoring at the study centre for the total study period. Plausibility checks and logical considerations of the relationships between associated variables will be performed. A data protection concept was developed, reviewed and approved by the data protection officer of the Universitätsklinikum Erlangen.
Patient and public involvement
Study participants or the public will not be involved in developing, designing, or conducting the study. To recruit participants from the general population, our recruitment partner, a health insurance company, will send emails to their customers with information about our study. Additional information about the study can be found on the project homepage.
Data analysis
All relevant data, sociodemographic, health-related, primary and secondary outcome variables will be reported descriptively. In order to be able to assess the quality of the randomisation, the baseline data from the intervention and control groups will be tested for statistically significant differences. For the multivariate analyses, we will impute missing values using the expectation maximisation algorithm. The primary hypothesis will be tested via analysis of variance, which makes it possible to detect interaction effects in the chosen 2×2×2 factorial design. To ensure the robustness of the results, we will perform both intention to treat and per protocol analyses. Intention-to-treat evaluations are carried out with all cases still alive at the end of the intervention or observation period. The significance level is defined as α=0.05. The data analyses will be performed using the IBM SPSS Statistics V.28 software.
Ethics and dissemination
Ethical considerations
All procedures were approved by the Friedrich-Alexander-Universität Erlangen-Nürnberg Ethics Committee (Ref. 21-318-1-B). Participation will be voluntary, and participants will be free to leave the study at any time. All legal matters, such as voluntariness, right of revocation and General Data Protection Regulation (EU) are considered. People with MCI are independent and fully capable of conducting business and giving consent. On agreement, consent to participate (written informed consent) will be obtained from all participants by the student assistants who are members of the study centre. All participants will be informed about the study in a personal videoconference after they are screened for eligibility. A participant information sheet including important information about participation (eg, randomisation, data protection, data storage) will be given to every participant (sent by post). The opportunity to ask questions will be granted by videoconference, telephone and email afterwards at any time. Participants will not be offered any financial inducement to participate. The external funder, the Karl and Veronica Carstens-Stiftung, is continuously being informed about the progress of the study. In the case of important protocol modifications, we will inform the Ethics Committee, the funder and the trial registry platform.
Data handling
Informed consent will be stored in a locked steel cabinet. A customised digital participant management system webMODYS (Web-based modular control and documentation system; Leibniz Institute for Prevention Research and Epidemiology—BIPS, Bremen, Germany) will be used for the administration of the study and will be the only location for personal data. webMODYS is hosted in the IT infrastructure of the Universitätsklinikum Erlangen. Only members of the study team will have access to the lists of participants’ names and codes in webMODYS. All data will be stored in only a pseudonymised form digitally in the data collection system REDCap73 74 hosted at the Universitätsklinikum Erlangen and Charité Berlin. REDCap is a secure, web-based software platform designed to support data capturing for research studies. The IT architecture including the digital study administration and data collection was ‘inspired’ by the digiDem Bayern Registry.75 Results of the study for scientific or other publications will be published only in aggregate form (mean values, etc). No published material will contain patient-identifying information.
Safety considerations
The CCT applications might have an impact on existing excessive computer use. However, both CCT applications that we developed are not based on motivational or emotional components. The CCT applications require cognitive performance, which could instead lead to exhaustion.
Adverse effects are rare and minor in the context of dietary regimens. The following adverse effects might occur: feeling of heat, changes in mouth and/or body odour, constipation, diarrhoea, meteorism, stomach cramps, nausea or vomiting. The two dietary recommendations are based either on the recommendations of the German Nutrition Society for a wholesome omnivorous diet or on plant-based dietary recommendations.76 The plant-based diet is recognised as a safe, sustainable diet for all lifestyles by various nutrition institutes.77–79
Dissemination plan
The research group intends to publish the data generated from this study in peer-reviewed journals. In addition, results will be communicated at international conferences, national conventions with the funders and the press.
Trial status
Protocol V.1.0, 22 December 2021. The overall start date of the study was 1 June 2020. Recruitment will begin on 3 January 2022 and will continue until 30 September 2022.
Supplementary Material
Acknowledgments
We would like to extend thanks to our student assistants Özlem Bülbül-Gümüs, Paula Hinkl, Tina Kopp, Johanna Lefringhausen, Paulina Lohmüller, Selina Muhehe, Martin Schmitt, Kerstin Schwenkschuster, Isabel Steger, and Nora Straschewski for their support and commitment. Many thanks to the team at Centrum für interdisziplinäre Gesundheitsförderung e.V., Technische Hochschule Nürnberg Georg-Simon-Ohm, Prof. Dr.-Ing. Helmut Herold, Dipl.-Ing. (FH) Wolfgang Bergmann and to genesis systems, Prof. Ethelbert Hörmann, for their support in developing individualised and basic CCT. We would like to thank the SBK Siemens-Betriebskrankenkasse for sending the recruitment emails and the Karl and Veronica Carstens foundation for funding the study. Many thanks also to our professional English-language editor, Dr. Jane Zagorski.
Footnotes
Contributors: PS contributed to the design of the study, is supervising the study, is contributing to the implementation of the study, and drafted the manuscript. StB contributed to the design of the study, is supervising the study, is contributing to the implementation of the study, and drafted the manuscript. MJa designed the CCT applications, is contributing to the implementation of the study, and drafted parts of the manuscript. EH is contributing to the implementation of the study and drafted parts of the manuscript. MD designed the nutrition intervention and is contributing to the implementation of the study. JS designed the nutrition intervention and is contributing to the implementation of the study. MJe contributed to the design of the study and is supervising the study. J-SS is supervising the study and contributing to the implementation of the study. SoB is contributing to the psychometric examinations and supervising the student assistants. CK initiated the study, contributed to the design of the study, and is supervising the study. EG initiated the study, contributed to the design of the study, is supervising the study, and drafted parts of the manuscript. All authors read and approved the final version of the manuscript. CK and EG are shared last authors.
Funding: This work is supported by the Karl and Veronica Carstens-Stiftung (Am Deimelsberg 36, 45 276 Essen).
Disclaimer: The funding body has no role in the study design, the collection, analysis, or interpretation of the data, or in writing the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med 2004;256:183–94. 10.1111/j.1365-2796.2004.01388.x [DOI] [PubMed] [Google Scholar]
- 2.Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: mild cognitive impairment: report of the Guideline development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018;90:126–35. 10.1212/WNL.0000000000004826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberts RO, Knopman DS, Mielke MM, et al. Higher risk of progression to dementia in mild cognitive impairment cases who revert to normal. Neurology 2014;82:317–25. 10.1212/WNL.0000000000000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inui Y, Ito K, Kato T, et al. Longer-term investigation of the value of 18F-FDG-PET and magnetic resonance imaging for predicting the conversion of mild cognitive impairment to Alzheimer's disease: a multicenter study. J Alzheimers Dis 2017;60:877–87. 10.3233/JAD-170395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guure CB, Ibrahim NA, Adam MB, et al. Impact of physical activity on cognitive decline, dementia, and its subtypes: meta-analysis of prospective studies. Biomed Res Int 2017;2017:13 10.1155/2017/9016924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonçalves A-C, Cruz J, Marques A, et al. Evaluating physical activity in dementia: a systematic review of outcomes to inform the development of a core outcome set. Age Ageing 2018;47:34–41. 10.1093/ageing/afx135 [DOI] [PubMed] [Google Scholar]
- 7.Huang X, Zhao X, Li B, et al. Comparative efficacy of various exercise interventions on cognitive function in patients with mild cognitive impairment or dementia: a systematic review and network meta-analysis. Jshs 2021;12:2095–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuzum H, Stickel A, Corona M, et al. Potential benefits of physical activity in MCI and dementia. Behav Neurol 2020;2020:7807856 10.1155/2020/7807856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beishon L, Intharakham K, Swienton D, et al. Neuroimaging outcomes in studies of cognitive training in mild cognitive impairment and early Alzheimer's disease: a systematic review. Curr Alzheimer Res 2020;17:472–86. 10.2174/1567205017666200624202425 [DOI] [PubMed] [Google Scholar]
- 10.Gómez-Soria I, Peralta-Marrupe P, Calatayud-Sanz E, et al. Efficacy of cognitive intervention programs in amnesic mild cognitive impairment: a systematic review. Arch Gerontol Geriatr 2021;94:104332. 10.1016/j.archger.2020.104332 [DOI] [PubMed] [Google Scholar]
- 11.Xu W, Wang HF, Wan Y, et al. Leisure time physical activity and dementia risk: a dose-response meta-analysis of prospective studies. BMJ Open 2017;7:e014706. 10.1136/bmjopen-2016-014706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu J-T, Xu W, Tan C-C, et al. Evidence-based prevention of Alzheimer's disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry 2020;91:1201–9. 10.1136/jnnp-2019-321913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kueider AM, Parisi JM, Gross AL, et al. Computerized cognitive training with older adults: a systematic review. PLoS One 2012;7:e40588. 10.1371/journal.pone.0040588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faucounau V, Wu YH, Boulay M, et al. Cognitive intervention programmes on patients affected by mild cognitive impairment: a promising intervention tool for MCI? J Nutr Health Aging 2010;14:31–5. 10.1007/s12603-010-0006-0 [DOI] [PubMed] [Google Scholar]
- 15.Zhang H, Huntley J, Bhome R, et al. Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: a systematic review and meta-analysis. BMJ Open 2019;9:e027062. 10.1136/bmjopen-2018-027062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hill NTM, Mowszowski L, Naismith SL, et al. Computerized cognitive training in older adults with mild cognitive impairment or dementia: a systematic review and meta-analysis. Am J Psychiatry 2017;174:329–40. 10.1176/appi.ajp.2016.16030360 [DOI] [PubMed] [Google Scholar]
- 17.Ge S, Zhu Z, Wu B, et al. Technology-based cognitive training and rehabilitation interventions for individuals with mild cognitive impairment: a systematic review. BMC Geriatr 2018;18:213. 10.1186/s12877-018-0893-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coyle H, Traynor V, Solowij N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: systematic review of the literature. Am J Geriatr Psychiatry 2015;23:335–59. 10.1016/j.jagp.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 19.Chandler MJ, Parks AC, Marsiske M, et al. Everyday impact of cognitive interventions in mild cognitive impairment: a systematic review and meta-analysis. Neuropsychol Rev 2016;26:225–51. 10.1007/s11065-016-9330-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu M, Wu X, Shu X, et al. Effects of computerised cognitive training on cognitive impairment: a meta-analysis. J Neurol 2021;268:1680–8. 10.1007/s00415-019-09522-7 [DOI] [PubMed] [Google Scholar]
- 21.Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019;393:447–92. 10.1016/S0140-6736(18)31788-4 [DOI] [PubMed] [Google Scholar]
- 22.Ballarini T, Melo van Lent D, Brunner J, et al. Mediterranean diet, Alzheimer disease biomarkers and brain atrophy in old age. Neurology 2021;96:e2920–32. 10.1212/WNL.0000000000012067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scarmeas N, Anastasiou CA, Yannakoulia M. Nutrition and prevention of cognitive impairment. Lancet Neurol 2018;17:1006–15. 10.1016/S1474-4422(18)30338-7 [DOI] [PubMed] [Google Scholar]
- 24.van den Brink AC, Brouwer-Brolsma EM, Berendsen AAM, et al. The mediterranean, dietary approaches to stop hypertension (DASH), and mediterranean-DASH intervention for neurodegenerative delay (mind) diets are associated with less cognitive decline and a lower risk of Alzheimer's Disease-A review. Adv Nutr 2019;10:1040–65. 10.1093/advances/nmz054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020;396:413–46. 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen X, Maguire B, Brodaty H, et al. Dietary patterns and cognitive health in older adults: a systematic review. J Alzheimers Dis 2019;67:583–619. 10.3233/JAD-180468 [DOI] [PubMed] [Google Scholar]
- 27.Bonaccio M, Pounis G, Cerletti C, et al. Mediterranean diet, dietary polyphenols and low grade inflammation: results from the MOLI-SANI study. Br J Clin Pharmacol 2017;83:107–13. 10.1111/bcp.12924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smidowicz A, Regula J. Effect of nutritional status and dietary patterns on human serum C-reactive protein and interleukin-6 concentrations. Adv Nutr 2015;6:738–47. 10.3945/an.115.009415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soltani S, Chitsazi MJ, Salehi-Abargouei A. The effect of dietary approaches to stop hypertension (DASH) on serum inflammatory markers: a systematic review and meta-analysis of randomized trials. Clin Nutr 2018;37:542–50. 10.1016/j.clnu.2017.02.018 [DOI] [PubMed] [Google Scholar]
- 30.Shen X-N, Niu L-D, Wang Y-J, et al. Inflammatory markers in Alzheimer's disease and mild cognitive impairment: a meta-analysis and systematic review of 170 studies. J Neurol Neurosurg Psychiatry 2019;90:590–8. 10.1136/jnnp-2018-319148 [DOI] [PubMed] [Google Scholar]
- 31.Poulsen NB, Lambert MNT, Jeppesen PB. The effect of plant derived bioactive compounds on inflammation: a systematic review and meta-analysis. Mol Nutr Food Res 2020;64:e2000473:2000473. 10.1002/mnfr.202000473 [DOI] [PubMed] [Google Scholar]
- 32.Fayosse A, Nguyen D-P, Dugravot A, et al. Risk prediction models for dementia: role of age and cardiometabolic risk factors. BMC Med 2020;18:107. 10.1186/s12916-020-01578-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Caoimh R, Timmons S, Molloy DW. Screening for mild cognitive impairment: comparison of "MCI specific" screening instruments. J Alzheimers Dis 2016;51:619–29. 10.3233/JAD-150881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ciesielska N, Sokołowski R, Mazur E, et al. Is the Montreal cognitive assessment (MoCA) test better suited than the Mini-Mental state examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? meta-analysis. Psychiatr Pol 2016;50:1039–52. 10.12740/PP/45368 [DOI] [PubMed] [Google Scholar]
- 36.Thomann AE, Berres M, Goettel N, et al. Enhanced diagnostic accuracy for neurocognitive disorders: a revised cut-off approach for the Montreal cognitive assessment. Alzheimers Res Ther 2020;12:39. 10.1186/s13195-020-00603-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 1992;40:922–35. 10.1111/j.1532-5415.1992.tb01992.x [DOI] [PubMed] [Google Scholar]
- 38.Morris MC, Wang Y, Barnes LL, et al. Nutrients and bioactives in green leafy vegetables and cognitive decline: prospective study. Neurology 2018;90:e214–22. 10.1212/WNL.0000000000004815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Feng L, Cheah IK-M, Ng MM-X, et al. The association between mushroom consumption and mild cognitive impairment: a community-based cross-sectional study in Singapore. J Alzheimers Dis 2019;68:197–203. 10.3233/JAD-180959 [DOI] [PubMed] [Google Scholar]
- 40.Zhang S, Tomata Y, Sugiyama K, et al. Citrus consumption and incident dementia in elderly Japanese: the Ohsaki cohort 2006 study. Br J Nutr 2017;117:1174–80. 10.1017/S000711451700109X [DOI] [PubMed] [Google Scholar]
- 41.Cui C, Birru RL, Snitz BE, et al. Effects of soy isoflavones on cognitive function: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev 2020;78:134–44. 10.1093/nutrit/nuz050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Travica N, D'Cunha NM, Naumovski N, et al. The effect of blueberry interventions on cognitive performance and mood: a systematic review of randomized controlled trials. Brain Behav Immun 2020;85:96–105. 10.1016/j.bbi.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 43.Chauhan A, Chauhan V. Beneficial effects of walnuts on cognition and brain health. Nutrients 2020;12. doi: 10.3390/nu12020550. [Epub ahead of print: 20 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhu L-N, Mei X, Zhang Z-G, et al. Curcumin intervention for cognitive function in different types of people: a systematic review and meta-analysis. Phytother Res 2019;33:524–33. 10.1002/ptr.6257 [DOI] [PubMed] [Google Scholar]
- 45.Kakutani S, Watanabe H, Murayama N. Green tea intake and risks for dementia, Alzheimer's disease, mild cognitive impairment, and cognitive impairment: a systematic review. Nutrients 2019;11. doi: 10.3390/nu11051165. [Epub ahead of print: 24 May 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vasefi M, Hudson M, Ghaboolian-Zare E. Diet associated with inflammation and Alzheimer's disease. J Alzheimers Dis Rep 2019;3:299–309. 10.3233/ADR-190152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beilharz JE, Maniam J, Morris MJ. Diet-induced cognitive deficits: the role of fat and sugar, potential mechanisms and nutritional interventions. Nutrients 2015;7:6719–38. 10.3390/nu7085307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hauner H, Beyer-Reiners E, Bischoff G, et al. Leitfaden Ernährungstherapie in Klinik und praxis (LEKuP). Aktuelle Ernährungsmedizin 2019;44:384–419. [Google Scholar]
- 49.Francis HM, Stevenson RJ. Higher reported saturated fat and refined sugar intake is associated with reduced hippocampal-dependent memory and sensitivity to interoceptive signals. Behav Neurosci 2011;125:943–55. 10.1037/a0025998 [DOI] [PubMed] [Google Scholar]
- 50.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695–9. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 51.Freitas S, Simões MR, Alves L, et al. Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord 2013;27:37–43. 10.1097/WAD.0b013e3182420bfe [DOI] [PubMed] [Google Scholar]
- 52.Larner AJ. Screening utility of the Montreal Cognitive Assessment (MoCA): in place of--or as well as--the MMSE? Int Psychogeriatr 2012;24:391–6. 10.1017/S1041610211001839 [DOI] [PubMed] [Google Scholar]
- 53.Dong Y, Lee WY, Basri NA, et al. The Montreal cognitive assessment is superior to the Mini-Mental state examination in detecting patients at higher risk of dementia. Int Psychogeriatr 2012;24:1749–55. 10.1017/S1041610212001068 [DOI] [PubMed] [Google Scholar]
- 54.Freitas S, Simões MR, Marôco J, et al. Construct validity of the Montreal cognitive assessment (MoCA). J Int Neuropsychol Soc 2012;18:242–50. 10.1017/S1355617711001573 [DOI] [PubMed] [Google Scholar]
- 55.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 56.Arevalo-Rodriguez I, Smailagic N, Roque IFM. Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev 2015;3:CD010783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Creavin ST, Wisniewski S, Noel-Storr AH, et al. Mini-Mental state examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev 2016;1:CD011145. 10.1002/14651858.CD011145.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tsoi KKF, Chan JYC, Hirai HW, et al. Cognitive tests to detect dementia: a systematic review and meta-analysis. JAMA Intern Med 2015;175:1450–8. 10.1001/jamainternmed.2015.2152 [DOI] [PubMed] [Google Scholar]
- 59.Munro Cullum C, Hynan LS, Grosch M, et al. Teleneuropsychology: evidence for video teleconference-based neuropsychological assessment. J Int Neuropsychol Soc 2014;20:1028–33. 10.1017/S1355617714000873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Timpano F, Pirrotta F, Bonanno L, et al. Videoconference-based mini mental state examination: a validation study. Telemed J E Health 2013;19:931–7. 10.1089/tmj.2013.0035 [DOI] [PubMed] [Google Scholar]
- 61.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Löwe B, Spitzer RL, Zipfel S. PHQ-D. Gesundheitsfragebogen für Patienten. Manual. 2 edn. Pfizer, 2002. [Google Scholar]
- 63.Kroenke K, Spitzer RL, Williams JBW, et al. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–59. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 64.Gilbody S, Richards D, Barkham M. Diagnosing depression in primary care using self-completed instruments: UK validation of PHQ-9 and CORE-OM. Br J Gen Pract 2007;57:650–2. [PMC free article] [PubMed] [Google Scholar]
- 65.Hindmarch I, Lehfeld H, de Jongh P, et al. The Bayer activities of daily living scale (B-ADL). Dement Geriatr Cogn Disord 1998;9 Suppl 2:20–6. 10.1159/000051195 [DOI] [PubMed] [Google Scholar]
- 66.Laugwitz B, Held T, Schrepp M. Construction and evaluation of a user experience questionnaire. Berlin, Heidelberg: Springer Berlin Heidelberg, 2008: 63–76. [Google Scholar]
- 67.Haftenberger M, Heuer T, Heidemann C, et al. Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr J 2010;9:36. 10.1186/1475-2891-9-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.DeYoung N, Shenal BV. The reliability of the Montreal cognitive assessment using telehealth in a rural setting with veterans. J Telemed Telecare 2019;25:197–203. 10.1177/1357633X17752030 [DOI] [PubMed] [Google Scholar]
- 69.Wadsworth HE, Galusha-Glasscock JM, Womack KB, et al. Remote neuropsychological assessment in rural American Indians with and without cognitive impairment. Arch Clin Neuropsychol 2016;31:420–5. 10.1093/arclin/acw030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marra DE, Hamlet KM, Bauer RM, et al. Validity of teleneuropsychology for older adults in response to COVID-19: a systematic and critical review. Clin Neuropsychol 2020;34:1411–52. 10.1080/13854046.2020.1769192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adams JL, Myers TL, Waddell EM, et al. Telemedicine: a valuable tool in neurodegenerative diseases. Curr Geriatr Rep 2020;9:72–81. 10.1007/s13670-020-00311-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Costanzo MC, Arcidiacono C, Rodolico A, et al. Diagnostic and interventional implications of telemedicine in Alzheimer's disease and mild cognitive impairment: a literature review. Int J Geriatr Psychiatry 2020;35:12–28. 10.1002/gps.5219 [DOI] [PubMed] [Google Scholar]
- 73.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Reichold M, Dietzel N, Chmelirsch C, et al. Designing and implementing an IT architecture for a digital multicenter dementia registry: digiDEM Bayern. Appl Clin Inform 2021;12:551–63. 10.1055/s-0041-1731286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.M: R. Position der Deutschen Gesellschaft für Ernährung eV (DGE)–Vegane Ernährung. Ernährungsumschau 2016;63:92–102. [Google Scholar]
- 77.Agnoli C, Baroni L, Bertini I, et al. Position paper on vegetarian diets from the Working group of the Italian Society of human nutrition. Nutr Metab Cardiovasc Dis 2017;27:1037–52. 10.1016/j.numecd.2017.10.020 [DOI] [PubMed] [Google Scholar]
- 78.Melina V, Craig W, Levin S. Position of the Academy of nutrition and dietetics: vegetarian diets. J Acad Nutr Diet 2016;116:1970–80. 10.1016/j.jand.2016.09.025 [DOI] [PubMed] [Google Scholar]
- 79.Phillips F. Vegetarian nutrition. Nutr Bull 2005;30:132–67. 10.1111/j.1467-3010.2005.00467.x [DOI] [Google Scholar]
- 80.Wechsler D. Wechsler adult intelligence scale–fourth edition (WAIS-IV)–Deutsche Version. Frankfurt/Main: Pearson Assessment, 2012. [Google Scholar]
- 81.Salthouse TA. The processing-speed theory of adult age differences in cognition. Psychol Rev 1996;103:403–28. 10.1037/0033-295X.103.3.403 [DOI] [PubMed] [Google Scholar]
- 82.Lehfeld H, Schläfke S, Hoerr R, et al. SKT short cognitive performance test and activities of daily living in dementia. GeroPsych 2014;27:75–80. 10.1024/1662-9647/a000104 [DOI] [Google Scholar]
- 83.Henik A, Tzelgov J. Is three greater than five: the relation between physical and semantic size in comparison tasks. Mem Cognit 1982;10:389–95. 10.3758/BF03202431 [DOI] [PubMed] [Google Scholar]
- 84.Kaufmann L, Ischebeck A, Weiss E, et al. An fMRI study of the numerical Stroop task in individuals with and without minimal cognitive impairment. Cortex 2008;44:1248–55. 10.1016/j.cortex.2007.11.009 [DOI] [PubMed] [Google Scholar]
- 85.Raven JC, Court JH. Manual for Raven’s Progressive matrices and vocabulary scales. London: H.K. Lewis, 1986. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.