Abstract
Purpose
Although childhood asthma is a risk factor for adult lung function disorders, the correlation between childhood asthma control level and lung function growth remains unclear in Japan. The correlation between childhood asthma control and early adulthood lung function growth was investigated in this study.
Patients and Methods
We included 505 children with asthma from the Omuta City Air Pollution-Related Health Damage Cohort Program. The characteristics and lung function of girls and boys aged 6–11 years and 12–17 years were compared between poor and good asthma control groups.
Results
Among the 505 children, 214 (42.4%) showed poor asthma control. The mean percentage forced expiratory volume in 1 second predicted for girls and boys aged 6–11 years (80.2% and 79.2%, respectively) and 12–17 years (80.0% and 81.1%, respectively) in the poor control group was significantly lower than those of girls and boys aged 6–11 years (87.9% and 87.3%, respectively) and 12–17 years (88.1% and 87.8%, respectively) in the good control group. However, a linear regression model did not reveal between-group differences in the slopes of lung function growth for both sexes. Girls (24.6%, P < 0.0001) and boys (24.4%, P = 0.0026) in the poor control group had a significantly higher proportion of young adults with obstructive ventilatory patterns than girls (1.4%) and boys (8.1%) in the good control group.
Conclusion
Our findings revealed that poor childhood asthma control leaded to lung function disorders, which suggest the importance of early asthma control in school children.
Keywords: childhood asthma, airflow limitation, Japanese, transition, school-age children
Plain Language Summary
We Japanese investigators group found that poor control of asthmatic symptoms at childhood may affect poor lung functions in adulthood by using data from the Japanese long-term observational cohort program. Then, we believe that getting the solid asthma treatments at the childhood helps maintain normal lung functions when they grow up to adults.
Introduction
From 2001 to 2010, the global age-standardized asthma mortality rate was 9.34 per million.1,2 An analysis of the World Health Organization database found that the reduction trend in global asthma mortality might have stalled between 2006 and 2012.3 An updated Japanese survey report revealed that the reduction trend in asthma mortality in Japan appeared to be stalling in the recent years; however, the number of asthma-related deaths in Japan decreased from 5926 in 1996 to 1511 in 2015.4,5
Asthma-related mortality is associated with severe diseases and their poor control.6,7 Poor control of airway inflammation may cause longitudinal lung function decline.8,9 Furthermore, airway obstruction leads to poor long-term mortality in patients with asthma.10–13 Asthma attacks and hospital admissions are frequent and mortality is still unacceptably high. Although nearly 5% of children with asthma present with a severe uncontrolled disease, these patients and their caregivers face a significant burden, including troublesome persistent symptoms, life-threatening acute attacks, medication side effects, impaired school performance, neuropsychological problems, and a lower quality of life.14,15 Childhood uncontrolled asthma is a complex and heterogeneous disease. Positive family history of asthma and atopy, genetic polymorphisms, epigenetic markers, respiratory tract infections early in life, allergic comorbidities such as eczema and allergic rhinitis, active smoking in adolescence, and lung function deficits have all been identified as important determinants of persisting asthma symptoms from childhood through to adulthood.16–18 The incidence of childhood asthma may affect lung function growth, including airway hyperresponsiveness, atopic conditions, and peripheral eosinophilia,19–21 which may cause persistent asthma and chronic obstructive pulmonary disease (COPD) with early smoke exposure in adolescents.22–24 However, the relationship between childhood asthma control level and lung function growth remains unclear in Japan.25–27
In accordance with the Pollution-related Health Damage Compensation Act since 1973, the Omuta City Air Pollution-Related Health Damage Cohort Program prospectively monitors residents with confirmed air pollution-related chronic respiratory diseases, including asthma, chronic bronchitis, and pulmonary emphysema.4 However, the cohort program could not investigate the relationship between childhood asthma control and longitudinal lung function growth until early adulthood. Nonetheless, a previous study reported that airflow obstruction was an independent risk factor for long-term mortality in adulthood asthma using data from the cohort program.10 This study aimed to investigate the relationship between childhood asthma control level and lung function growth in young adults using data from the long-term cohort program in Japanese.
Patients and Methods
Study Protocol
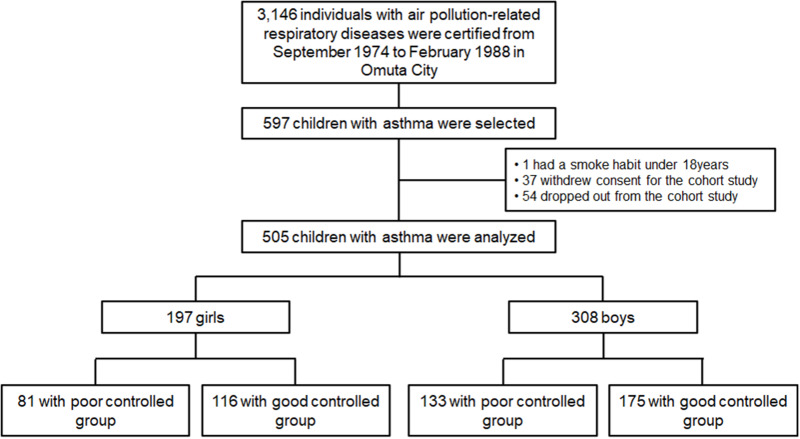
The Omuta City Air Pollution-Related Health Damage Cohort Program (Omuta, Fukuoka, Japan) was established by the Pollution-related Health Damage Compensation Act.10 Between 1974 and 1988, 3146 patients with air pollution-related respiratory diseases were registered (Figure 1) in the program, which required annual measurements of height, weight, asthma control level, and spirometry. All cohort data were managed in the Department of Health and Welfare, Omuta City, Fukuoka, Japan, from the time of registration (enrollment) until the present. In the study, we included all data of children (aged <18 years at enrollment) with asthma.
Figure 1.
Study design.
Patients
Among all registered patients, 597 children were diagnosed with asthma. Four participants were excluded due to smoke exposure, 37 withdrew consent, and 54 dropped out from the cohort program aged < 18 years. Finally, 505 children were selected (intention to treat) (Figure 1). Asthma was diagnosed based on the criteria stipulated in the Pollution-related Health Damage Compensation Act, which included symptoms such as occasional spasmodic, repeated, and fluctuating wheezing and dyspnea at enrollment. However, a diagnosis of asthmatic bronchitis and pollution-unrelated and allergic asthma may be included in the diagnosis of asthma. The Act defined a four-step scoring system for the annual asthma control level based on patient- or guardian-reported asthmatic symptoms and the monthly exacerbation rates once a year. The annual asthma control level was scored (1=very poor; 2=poor; 3=partly poor; 4=good) based on the Act (Supplementary Table 1).10 The children were classified into the poor and good asthma control groups. Specifically, children with mean scores of < 4.0 and 4.0 points for asthma control levels throughout the period from the ages of 6 to 17 years were classified into the poor and good control groups, respectively.
Data Collection
We collected the data obtained at enrollment and annually after enrollment until the age of 20 years, including age, sex, height, weight, smoking status, asthma control level, and spirometry data, from 505 children with asthma. The children were required to undergo an annual lung function test after reaching an age at which they could understand and undergo spirometry. The forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), predicted FVC value (%FVC predicted), percentage of predicted FEV1 value (%FEV1 predicted), and FEV1/FVC ratio were determined through spirometry. The %FEV1 predicted and %FVC predicted were calculated based on the formula for Japanese children aged 6–17 years.28 Spirometric-restrictive and obstructive ventilatory patterns were defined as %FVC predicted < 80% with FEV1/FVC ratio ≥ 0.7 and FEV1/FVC ratio < 0.7, respectively.29 Mixed ventilatory pattern was defined as the presence of both restrictive and obstructive ventilatory patterns. However, the Act did not require measurement of the reversibility of FEV1 through pre- and post-bronchodilations.10
Ethical Approval
The investigators signed a contract with Omuta City for permission to use the data on August 27, 2015 (updated on August 19, 2020). The study was conducted following the Good Clinical Practice guidelines and was approved by the local ethics board of Kurume University (No. 20–225, January 19, 2021). The study protocol was registered with the University Hospital Medical Information Network (UMIN) Center (UMIN No. 000043876) on April 9, 2021. Participants were allowed an opt-out option between April 9 and October 9, 2021 (for 6 months).
Statistical Analyses
Characteristics of the study cohort at the age of 6 years were expressed as mean ± standard deviation (SD) and the number (%) of patients. Between-group comparisons of characteristics were performed using Student’s t-tests and chi-squared tests. The measurements of %FVC predicted, %FEV1 predicted, and FEV1/FVC ratio were plotted over the age range between 6 and 17 years in children by sex and the asthma control level (poor or good control), as previous studies demonstrated that sex difference affected lung function growth difference in children with asthma.24,30 To investigate the correlation of asthma control level with lung function growth, we performed between-group comparisons of the proportion of girls and boys with restrictive, obstructive, and mixed ventilatory patterns within each age group. Welch’s t-test was used for between-group comparisons of the means (± SD) of % FVC predicted, % FEV1 predicted, and FEV1/FVC ratio measured from children aged 6–11 years (with primary sexual characteristics) and 12–17 years (with secondary sexual characteristics) for each sex separately.30–32 A linear mixed effect model was used to describe the individual growth of longitudinal physique and lung function. The model included a normally distributed random intercept to model between-individual variations in addition to fixed intercept and age effect, both of which were allowed to vary by the asthma control level. This model was separately fitted for the age ranges of 6–11 years and 12–17 years as well as for girls and boys.
To investigate whether the childhood asthma control level was associated with early-adulthood lung function, the odds ratio (95% confidential interval [CI]) for poorly controlled early-adulthood ventilatory patterns at the ages of 18 to 20 years compared with the good control group was calculated using Fisher’s exact tests. However, among all children tested between the ages of 18 and 20, the children were divided into each group of restrictive, obstructive, and mixed ventilatory patterns, when at least one positive result from the three tests was obtained in each pattern. Moreover, the relative risk was adjusted for potential confounders, including age at enrollment, sex, and lung function levels. In addition, to investigate the associations between the effects of control levels under 6 years and the lung function levels at 6 and/or 7 years as sub-analysis. Statistical significance was set at P < 0.05. Statistical analyses were performed using JMP version 14.2.0 software package (SAS Institute Japan Inc., Tokyo, Japan) and R (version 3.6.1, R Foundation, https://www.r-project.org/).
Results
Study Population
Among 505 children [girls, n = 197 (39.0%) and boys, n = 308 (61.0%)] with asthma, 81 girls and 133 boys (214 [42.4% of total population]) were classified into the poor control group, while 116 girls and 175 boys (291 [57.6%]) were classified into the good control group (Figure 1). The median observation period (25 and 75 percentiles [range]) was 10 (5 and 13 [1–14]) years between the ages of 6 and 20 years. None of the participants died during the period. Table 1 shows the between-group comparison of characteristics in girls and boys aged 6 years. Boys in the poor control group had significantly lower weight, body mass index (BMI), %FEV1 predicted, and FEV1/FVC ratio than those in the good control group; however, there was no between-group difference for girls. Poor control group had significantly higher proportion (odds ratio [95% CI]) of girls and boys with obstructive (1.95 [1.34 to 2.84], P = 0.0002 and 2.78 [1.98 to 3.90], P <0.0001, respectively) and mixed (4.60 [1.99 to 10.64], P <0.0001 and 1.93 [1.01 to 3.67], P = 0.0492, respectively), but not restrictive (1.18 [0.83 to 1.69], P = 0.4135 and 1.24 [0.91 to 1.68], P = 0.1914, respectively), when compared with good control group (complete analysis of each age group is shown in Supplementary Table 2A and B).
Table 1.
Between-Group Comparisons of Characteristics in Girls and Boys at the Age of 6 Years
| Characteristics | Girls, n = 197 | Boys, n = 308 | ||||
|---|---|---|---|---|---|---|
| Poor Control Group, n = 81 | Good Control Group, n = 116 | P value | Poor Control Group, n = 133 | Good Control Group, n =175 | P value | |
| Height, cm | 112.4 ± 5.4, n = 37 | 114.1 ± 5.4, n = 28 | 0.2 | 114.3 ± 5.9, n = 61 | 114.6 ± 4.9, n = 41 | 0.8 |
| Weight, kg | 19.1 ± 3.0, n = 36 | 20.1 ± 2.8, n = 28 | 0.2 | 19.4 ± 2.8, n = 60 | 20.8 ± 3.4, n = 40 | 0.0246* |
| Body mass index, kg/m2 | 15.1 ± 1.6, n = 36 | 15.6 ± 1.4, n = 27 | 0.3 | 14.9 ± 1.4, n = 60 | 15.8 ± 2.0, n = 40 | 0.0057* |
| Lung function tests | ||||||
| FVC, L | 1.15 ± 0.24, n = 21 | 1.20 ± 0.33, n = 13 | 0.6 | 1.32 ± 0.31, n = 34 | 1.28 ± 0.24, n = 26 | 0.6 |
| %FVC predicted, % | 92.4 ± 19.2, n = 21 | 100.0 ± 23.8, n = 13 | 0.3 | 90.3 ± 15.7, n = 34 | 90.4 ± 14.1, n = 26 | 1.0 |
| FEV1, L | 0.90 ± 0.27, n = 21 | 0.93 ± 0.26, n = 13 | 0.6 | 0.94 ± 0.25, n = 35 | 1.09 ± 0.17, n = 26 | 0.1 |
| %FEV1 predicted, % | 78.0 ± 22.6, n = 21 | 84.1 ± 20.7, n = 13 | 0.4 | 74.0 ± 15.1, n = 35 | 84.3 ± 11.6, n = 26 | 0.0048* |
| FEV1/FVC ratio | 0.77 ± 0.13, n = 21 | 0.78 ± 0.12, n = 13 | 0.7 | 0.77 ± 0.14, n = 34 | 0.87 ± 0.11, n = 26 | 0.0047* |
| No. of children with ventilatory patterns, n (%) | ||||||
| Restrictive | 2 (9.5), n = 21 | 2 (15.4), n = 13 | 0.6 | 7 (20.6), n = 34 | 6 (23.1), n = 26 | 1.0 |
| Obstructive | 7 (33.3), n = 21 | 4 (30.8), n = 13 | 1.0 | 13 (38.2), n = 34 | 2 (7.7), n = 26 | 0.0076* |
| Mixed | 4 (19.1), n = 21 | 1 (7.7), n = 13 | 0.6 | 1 (2.9), n = 34 | 0 (0), n = 26 | 1.0 |
Notes: Data were expressed as mean ± SD and number (%) of children. The poor control group had significantly lower mean scores (± SD, points) of the asthma control level in girls (2.95 ± 0.46, n = 39) (P < 0.0001) and boys (3.16 ± 0.37, n = 67) (P < 0.0001) compared with the good control group (4.0, n = 30 and 4.0, n = 46, respectively) at the age of 6 years. n = number of children tested. *P < 0.05 for between-group comparisons.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; SD, standard deviation.
Between-Group Comparisons of Lung Function in Girls and Boys Aged 6 to 17 Years
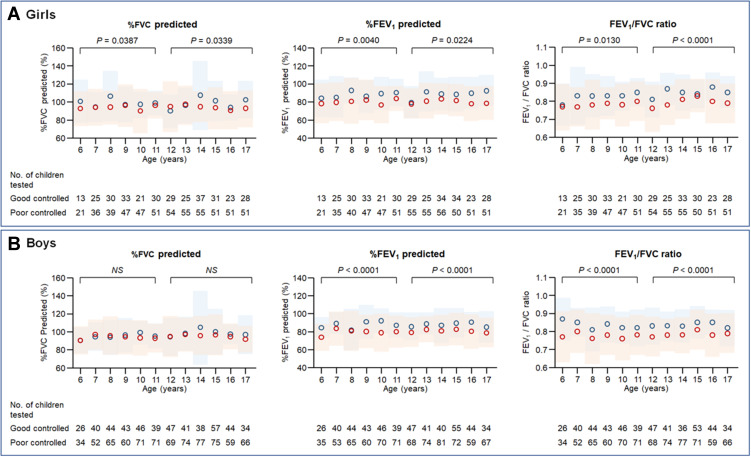
Figure 2 depicts the mean (± SD) of the % FVC predicted, % FEV1 predicted, and FEV1/FVC ratio in girls and boys based on asthma control level (poor vs good) for each year from 6 to 17 years of ages. Among girls, the poor control group had significantly lower mean values [SD] of %FVC and %FEV1 predicted and FEV1/FVC ratio than the good control group from the ages of 6 to 11 years (93.2% [14.3] vs 98.4% [18.5], P = 0.0387 and 80.2% [16.1] vs 87.9% [16.0], P = 0.0040, and 0.79 [0.09] vs 0.83 [0.10], P = 0.0130, respectively) and from the ages of 12 to 17 years (93.5% [22.4] vs 98.4% [25.2], P = 0.0339 and 80.0% [19.4] vs 88.1% [19.0], P = 0.0224, and 0.79 [0.11] vs 0.85 [0.09], P < 0.0001, respectively). In contrast, among boys, there was no significant between-group difference in %FVC predicted from the ages of 6 to 11 years (93.2% [13.2] vs 95.1% [15.9], P = 0.2994) and 12 to 17 years (95.1% [19.7] vs 98.6% [24.4], P = 0.0558). The poor control group had significantly lower mean values [SD] of %FEV1 predicted, and FEV1/FVC ratio than the good control group from the ages of 6 to 11 years (79.2% [15.4] vs 87.3% [16.4], P < 0.0001, 0.77 [0.10] vs 0.83 [0.09], P < 0.0001, respectively) and from the ages of 12 to 17 years (81.1% [16.9] vs 87.8% [15.3], P < 0.0001, and 0.79 [0.11] vs 0.83 [0.09], P < 0.0001, respectively).
Figure 2.
Between-group comparisons of lung functions in girls and boys from the ages of 6 years to 17 years.
Notes: %FVC predicted, %FEV1 predicted, and FEV1/FVC ratio in Girls (A) and Boys (B). The poor and good control groups are shown in red and blue, respectively. The mean and SD are shown in open circles and pale-colored squares, respectively. We performed between-group comparisons of the mean values of %FVC predicted, %FEV1 predicted, and FEV1/FVC ratio in the two age groups (ages: 6–11 years and 12–17 years).
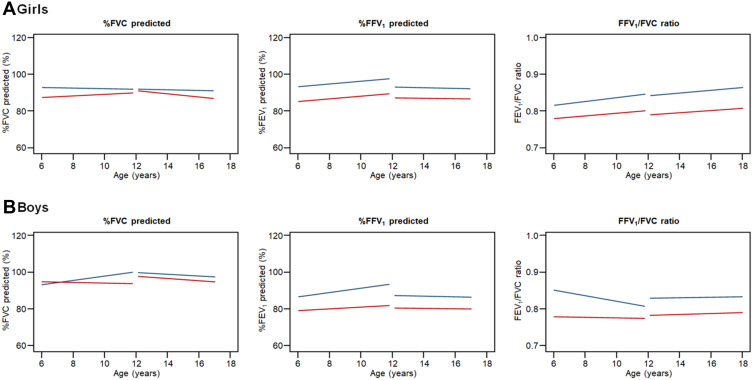
Between-Group Comparison of the Slopes for Lung Function Growth in Girls and Boys from the Ages of 6 Years to 17 Years
Figure 3 shows that there were no significant between-group differences in the slopes of %FVC and %FEV1 predicted. The FEV1/FVC ratio growth for girls from the ages of 6 to 11 years was 0.92% [1.20] and 0.06% [1.11], and 0.00 [0.01], respectively, and from 12 to 17 years was 0.87 [0.91] % and 0.10 [0.62] %, and 0.00 [0.00], respectively; for boys from the ages of 6 to 11 years it was 1.26% [0.80] and 0.64% [0.81] and, 0.01 [0.00], respectively, and from 12 to 17 years (0.09% [0.64] and 0.08 [0.44], and 0.00 [0.00], respectively. However, there was a difference in the slopes between the age-groups in both sexes (other results are shown in Supplementary Figure 1). The slopes of height (0.26 cm per year, P <0.0001) and weight (0.32 kg per year, P <0.0001) growth lines was significant difference between the ages of 6 to 11 and 12 to 17 in boys, whereas the slope of weight (0.33kg per year, P <0.0001), but not height (0.02cm per year, P >0.05), was significant difference between the age groups in girls (Supplementary Figure 2).
Figure 3.
Between-group comparison of the slopes for lung function growth in girls and boys from the ages of 6 years to 17 years.
Notes: %FVC predicted, %FEV1 predicted, and FEV1/FVC ratio in Girls (A) and Boys (B). The slopes with poor and good control groups are shown in red and blue lines, respectively. We performed between-group comparisons of the slopes of %FVC predicted, %FEV1 predicted, and FEV1/FVC ratio growth in the two age groups (ages: 6–11 years and 12–17 years).
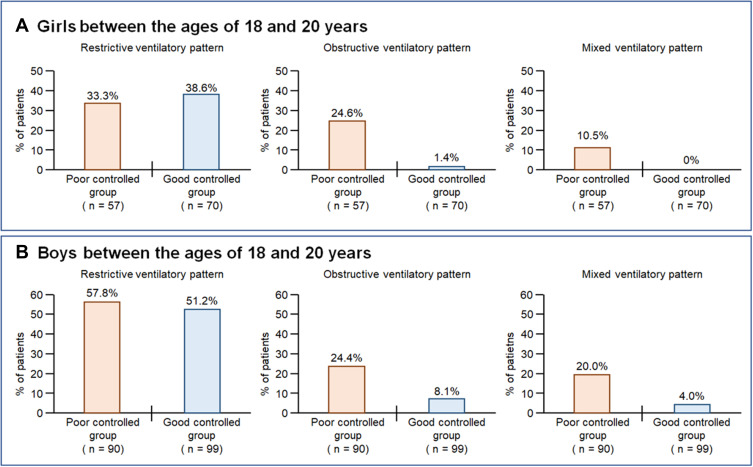
Between-Group Comparisons in the Proportion of Girls and Boys with Ventilatory Patterns in Children Between the Ages of 18 and 20 Years
Figure 4 shows the between-group comparison of the proportion of girls and boys between the ages of 18 and 20 years with obstructive, restrictive, and mixed ventilatory patterns (complete analysis is shown in Supplementary Table 3). Figure 4A and B showed that the poor control group had significantly higher proportions of girls and boys with obstructive (Odds ratio [OR] 17.19 [95% CI 2.33 to 129.90], P < 0.0001 and 3.03 [1.42 to 6.45], P = 0.0026, respectively) and mixed (OR and 95% CI not available, P = 0.0007 and 4.50 [1.56 to 12.96], P = 0.0019, respectively) ventilatory patterns than the good control group, although the between-group difference in the proportion of girls and boys with restrictive ventilatory patterns (0.88 [95% CI 0.54 to 1.39], P = 0.5814 and 1.12 [0.86 to 1.46], P = 0.4548, respectively) was not statistically significant.
Figure 4.
Between-group comparisons of lung functions in girls and boys in early adulthood.
Notes: Data were expressed as a percentage of the patients with restrictive, obstructive, and mixed ventilatory pattern among girls (A) and boys (B) between the ages of 18 and 20 years, respectively.
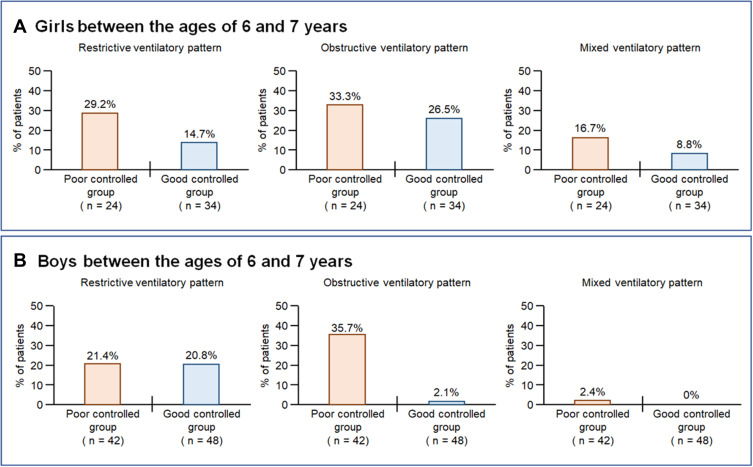
The Effect of Asthma Control Levels Under 6 Years on Lung Function in Girls and Boys at 6 or 7 Years
Among 505 children, 148 (girls = 58 and boys = 90) were assessed for asthma control levels under 6 years based on the scoring system of the Act10 and underwent spirometry at either 6 or 7 year. The number (%) of girls and boys with poor asthma control under 6 years was 34 (58.6%) and 42 (46.7%), respectively. Boys with poor control levels under 6 years had a significantly higher proportion of obstructive pattern, but not restrictive and mixed ventilatory patterns (Figure 5A), whereas there was no difference in the proportion of ventilatory patterns between girls’ groups at either 6 or 7 year (Figure 5B) (Supplementary Table 4A and B).
Figure 5.
Between-group comparisons of lung functions at either 6 or 7 years in girls and boys.
Notes: Data were expressed as a percentage of the patients with restrictive, obstructive, and mixed ventilatory pattern among girls (A) and boys (B) at either 6 or 7 year, respectively. On an average, poor and good asthma control levels were scored <4.0 and 4.0 of the scoring system under 6years by the Act, respectively.
Discussion
A history of childhood asthma is among the risk factors for early-adulthood COPD and lung function impairments.20,33–35 To our best knowledge, the correlation between childhood asthma severity and lung function growth remains unclear in Japanese.25,27,36,37 However, poor asthma control in adults and frequent exacerbations are known to cause lung function decline, which facilitates the development of COPD.26,27,38–41
The present study showed that poor control of childhood asthma was associated with lung function impairment during early adulthood. First, the children with asthma were classified according to sex to account for sex differences in the growth curve of the body physique and lung function.24,30 Second, the girls and boys were divided into two age groups; namely, 6–11 years old and 12–17 years old (showing primary and secondary sexual characteristics, respectively) based on the Japanese children’s growth curve.31,32 For both sexes, the poor control group had significantly lower mean values of %FEV1 predicted and FEV1/FVC ratio than the good control group from 6 years of age to 17 years of age. The results supported the previous reports.20–25 Contrastingly, compared with the good control group, the poor control group had significantly lower values of %FVC predicted only for girls aged 6–11 and 12–17 years. Additionally, the poor control group showed a significantly higher number of girls and boys at the ages of 18 to 20 years (early-adulthood) with obstructive and mixed, but not restrictive, ventilatory patterns than the good control group. This suggests that school children with poor asthma control showed greater impairment of obstructive, rather than restrictive, ventilation in the lung function growths. A child’s sex and the timing appearance of secondary sexual characteristics may influence the occurrence of obstructive ventilatory patterns related to poor asthma control. Contrastingly, poor asthma control may not affect the growth of body physiques since we observed no significant between-group differences in the height, weight, and BMI in each age group.
We used linear regression models to assess the growth curve based on the slopes at the ages of 6–11 years and 12–17 years. We observed a significant between-group difference in the slopes of weight (BMI) growth in only girls aged 12–17 years (Supplementary Figure 2). However, there were no significant between-group differences in the slopes of lung function growth in girls and boys (Figure 3). However, the poor control group showed significantly lower values of %FEV1 predicted and FEV1/FVC ratio, but not %FVC predicted, than the good control group for both sexes in both age groups. Our findings suggest that asthma control levels during preschool age (< 6 years) in boys but not in girls affect the subsequent between-group differences in the occurrence of obstructive ventilatory patterns after early school ages (6 and/or 7 years) (Supplementary Figure 3 and Supplementary Table 4). During preschool age, asthma control levels may influence the development of obstructive ventilatory patterns and vice versa.20,24–27,30,35
The cut-off values of the lower limit of normal (LLN) is often used to detect abnormalities in lung function.42–44 We found 0.605 for FEV1/FVC ratio and 64.06% for %FVC predicted as the LLN cut-off values for obstructive and restrictive patterns, respectively. The proportions of children with each ventilatory pattern using the LLN cut-off values was lower than those using the fixed cut-off values, and it was seemed to be no difference in the population between poor and good control groups in both sexes (Supplementary Table 5A and B). The LLN cut-off values may underestimate the number of children with abnormal lung functions, because both the cut-off values were lower than 0.7 for FEV1/FVC ratio and 80% for %FVC predicted as the fixed cut-off values in our cohort.42–44 Therefore, we did not use the LLN cut-off values were not used in our study.
Our findings suggest the need for an intervention strategy for preschool children with asthma to maintain normal lung function during school ages and young adulthood as previously reported.23 However, it is difficult to perform spirometry in preschool children.26,27,45,46 Body plethysmography and the impulse oscillometry system are necessary for evaluating lung function in infants and preschool children.26,27 Our cohort study found that the number (%) of children who underwent spirometry at the ages < 4 years, 4 years, and 5 years were 0 (0%), 6 (1.2%), and 28 (5.4%), respectively. Contrastingly, the number (%) of children who underwent evaluations for asthma control levels based on symptoms and exacerbations at the ages < 4 years, 4 years, and 5 years were 150 (29.1%), 121 (23.4%), and 160 (31.0%), respectively. Evaluation of asthmatic symptoms and exacerbations in infants and preschool-aged children could facilitate the prediction of asthma-related outcomes and lung function during adolescence.47,48 Wheezing is both an auscultatory finding and a respiratory symptom. Childhood wheezing is associated with decreased lung function levels during adolescence.20,26,27,35 To estimate impaired lung function growth in young adults, wheezing may be an important finding that should not be overlooked even in cases where lung function tests cannot be performed.
Our study had some study limitations. First, we missed some data due to drop out from the study as well as intermittent blanks. Then, our study had a bias that the poor control group had more than twice the population of both girls and boys requiring lung function tests compared with the good control group. Among the 505 included children, 432 (86%) were registered at ages ≤ 11 years; among them, 73 (14%) and 114 (23%) children lacked measurements at ages ≥ 12 years and ≥ 15 years, respectively. Our main analyses involved modeling of age-specific changes in each outcome variable using a linear mixed-effect regression model, which is relatively robust for missing data. Generally, the validity of analysis ignoring missing information depends on whether the missingness of the outcome measurement depends on the measurement itself. This study cannot rule out such a missing pattern; however, examining this is difficult. Second, we observed that between-group differences in lung function levels and the occurrence of lung function impairment differed according to sex. The sex differences may be attributed to differences in the defense thresholds against asthma or sample bias. In their early school years, boys may have more severe symptoms and lower lung function levels compared with girls.26,27,49,50 Our study sample included fewer girls than boys. Our results could not reflect the results of all children, as the frequency of children who underwent lung function tests was about 20% for poor control and 50% for good control group in each age group (Supplementary Figure 1). Third, our study might have included an excessive number of children with spirometric-restrictive ventilatory patterns. The gap between the predicted and measured FVC values may influence the findings. The standard regression equation for predicted FVC values was developed for Japanese children in 2008. In this study, children were enrolled from 1974 to 1988 and observed from 1994 to 2008. As both lung function and height are increasing with the times in the world,51 in Japanese school children the average height also increased by 5 cm (2 inches) between 1974 and 2004.52 Our cohort program did not assess total lung capacity and functional residual capacity. The spirometric-restrictive patterns may include physical disorders such as obesity, scoliosis, and thoracic cage abnormalities, but not true lung function disorders. Fourth, the effects of medicine and quality of air pollution at the time could not be assessed for the lung function growth and disease control levels because the cohort program did not collect data regarding medicine used for asthma and the quality of air pollution at the time. In a 2001 survey of Japanese children under the age of 15, inhaled corticosteroid (ICS) was used in 7.3% of patients with asthma.53 Most of our cohort patients enrolled before 2000 may not benefit from ICS. There is a need for further studies on important risk factors affecting the severity and prognosis of airflow obstruction in pediatric asthma.
Conclusion
We found that poor asthma control during school ages was associated with low FEV1 values during childhood and early-adulthood airflow obstruction, which may lead to adult COPD. Our findings suggest the importance of early and sustainable asthma management and better care transition plan in preschool and school children. These findings could facilitate improvement in asthma control in children and reduce of the proportion of adult Japanese patients with COPD in the future.
Acknowledgments
The authors thank all members of the Review Board Committee of the Omuta City Air Pollution-Related Health Damage Cohort Program. Special thanks are extended to Dr. Masayuki Kawasaki, Chairman of the Review Board Committee, President of the National Hospital Organization Omuta Hospital, and Adviser for the Review Board Committee, as well as Mrs. Masami Kanamaru and Mrs. Naomi Shimomura for data management and Mr. Keiji Hirayama, Chief Manager, Department of Health and Welfare, Omuta City.
Funding Statement
This work was supported by JSPS KAKENHI Grant Number JP 21K16152, Japan (J. S.).
Abbreviations
ANOVA, analysis of variance; BMI, body mass index; CI, confidence interval; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ICD-10 Version, International Statistical Classification of Diseases and Related Health Problems 10th Revision; SD, standard deviation; UMIN, University Hospital Medical Information Network.
Disclosure
Prof. Tomotaka Kawayama reports grants from Novartis and lecture fees from AstraZeneca, GlaxoSmithKline (GSK), Boehringer Ingelheim, Novartis, Teijin Home Healthcare, Sanofi, Kyorin, and MeijiSaika Pharma. Dr. Takashi Kinoshita reports grants from GSK, AstraZeneca, and a lecture fee from AstraZeneca. Prof. Tomoaki Hoshino reports a grant from GSK, Novartis, and Chugai Pharmaceutical. The other authors have no potential conflicts of interest for this study.
References
- 1.GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. doi: 10.1016/S2213-2600(17)30293-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Asthma Network. The global asthma report; 2018. Available from: http://www.globalasthmanetwork.org/. Accessed April 1, 2021.
- 3.Ebmeier S, Thayabaran D, Braithwaite I, Bénamara C, Weatherall M, Beasley R. Trends in international asthma mortality: analysis of data from the WHO mortality database from 46 countries (1993–2012). Lancet. 2017;390(10098):935–945. doi: 10.1016/S0140-6736(17)31448-4 [DOI] [PubMed] [Google Scholar]
- 4.Ministry of health, labour and welfare, Japan. Available from: http://www.mhlw.go.jp/. Accessed April 1, 2021. Japanese.
- 5.Ichinose M, Sugiura H, Nagase H, et al. Japanese guidelines for adult asthma 2017. Allergol Int. 2017;66(2):163–189. doi: 10.1016/j.alit.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 6.Bourdin A, Fabry-Vendrand C, Ostinelli J, et al. The burden of severe asthma in France: a case-control study using a medical claims database. J Allergy Clin Immunol Pract. 2019;7(5):1477–1487. doi: 10.1016/j.jaip.2018.12.029 [DOI] [PubMed] [Google Scholar]
- 7.Omachi TA, Iribarren C, Sarkar U, et al. Risk factors for death in adults with severe asthma. Ann Allergy Asthma Immunol. 2008;101(2):130–136. doi: 10.1016/S1081-1206(10)60200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sears MR. Consequences of long-term inflammation. The natural history of asthma. Clin Chest Med. 2000;21(2):315–329. doi: 10.1016/s0272-5231(05)70269-0 [DOI] [PubMed] [Google Scholar]
- 9.Ulrik CS. Outcome of asthma: longitudinal changes in lung function. Eur Respir J. 1999;13(4):904–918. doi: 10.1034/j.1399-3003.1999.13d35.x [DOI] [PubMed] [Google Scholar]
- 10.Okayama Y, Kawayama T, Kinoshita T, et al. Impact of airflow obstruction on long-term mortality in patients with asthma in Japan. Allergol Int. 2019;68(4):462–469. doi: 10.1016/j.alit.2019.04.009 [DOI] [PubMed] [Google Scholar]
- 11.Lange P, Çolak Y, Ingebrigtsen TS, Vestbo J, Marott JL. Long-term prognosis of asthma, chronic obstructive pulmonary disease, and asthma-chronic obstructive pulmonary disease overlap in the Copenhagen City Heart study: a prospective population-based analysis. Lancet Respir Med. 2016;4(6):454–462. doi: 10.1016/S2213-2600(16)00098-9 [DOI] [PubMed] [Google Scholar]
- 12.Siroux V, Boudier A, Dolgopoloff M, et al. Forced midexpiratory flow between 25% and 75% of forced vital capacity is associated with long-term persistence of asthma and poor asthma outcomes. J Allergy Clin Immunol. 2016;137(6):1709–1716.e6. doi: 10.1016/j.jaci.2015.10.029 [DOI] [PubMed] [Google Scholar]
- 13.Huang S, Vasquez MM, Halonen M, Martinez FD, Guerra S. Asthma, airflow limitation and mortality risk in the general population. Eur Respir J. 2015;45(2):338–346. doi: 10.1183/09031936.00108514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pijnenburg MW, Fleming L. Advances in understanding and reducing the burden of severe asthma in children. Lancet Respir Med. 2020;8(10):1032–1044. doi: 10.1016/S2213-2600(20)30399-4 [DOI] [PubMed] [Google Scholar]
- 15.Castagnoli R, Marseglia A, Brambilla I, et al. Severe uncontrolled asthma in children: practical approach on diagnosis and management. Minerva Pediatr. 2020;72(3):196–205. doi: 10.23736/S0026-4946.20.05818-1 [DOI] [PubMed] [Google Scholar]
- 16.Licari A, Brambilla I, Filippo MD, Poddighe D, Castagnoli R, Marseglia GL. The role of upper airway pathology as a co-morbidity in severe asthma. Expert Rev Respir Med. 2017;11(11):855–865. doi: 10.1080/17476348.2017.1381564 [DOI] [PubMed] [Google Scholar]
- 17.Fuchs O, Bahmer T, Rabe KF, et al. Asthma transition from childhood into adulthood. Lancet Respir Med. 2017;5:224–234. doi: 10.1016/S2213-2600(16)30187-4 [DOI] [PubMed] [Google Scholar]
- 18.Trivedi M, Denton E. Asthma in children and adults–what are the differences and what can they tell us about asthma? Front Pediatr. 2019;7:256. doi: 10.3389/fped.2019.00256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rennard SI, Drummond MB. Early chronic obstructive pulmonary disease: definition, assessment, and prevention. Lancet. 2015;385(9979):1778–1788. doi: 10.1016/S0140-6736(15)60647-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koefoed HJL, Zwitserloot AM, Vonk JM, Koppelman GH. Asthma, bronchial hyperresponsiveness, allergy and lung function development until early adulthood: a systematic literature review. Pediatr Allergy Immunol. 2021;32(6):1238–1254. doi: 10.1111/pai.13516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koefoed HJL, Gehring U, Vonk JM, Koppelman GH. Blood eosinophils associate with reduced lung function growth in adolescent asthmatics. Clin Exp Allergy. 2021;51(4):556–563. doi: 10.1111/cea.13818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bui DS, Lodge CJ, Burgess JA, et al. Childhood predictors of lung function trajectories and future COPD risk: a prospective cohort study from the first to the sixth decade of life. Lancet Respir Med. 2018;6(7):535–544. doi: 10.1016/S2213-2600(18)30100-0 [DOI] [PubMed] [Google Scholar]
- 23.Belgrave DCM, Granell R, Turner SW, et al. Lung function trajectories from pre-school age to adulthood and their associations with early life factors: a retrospective analysis of three population-based birth cohort studies. Lancet Respir Med. 2018;6(7):526–534. doi: 10.1016/S2213-2600(18)30099-7 [DOI] [PubMed] [Google Scholar]
- 24.McGeachie MJ, Yates KP, Zhou X, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med. 2016;374(19):1842–1852. doi: 10.1056/NEJMoa1513737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lo DK, Beardsmore CB, Roland D, et al. Lung function and asthma control in school-age children managed in UK primary care: a cohort study. Thorax. 2020;75(2):101–107. doi: 10.1136/thoraxjnl-2019-213068 [DOI] [PubMed] [Google Scholar]
- 26.Pijnenburg MW, Baraldi E, Brand PLP, et al. Monitoring asthma in children. Eur Respir J. 2015;45(4):906–925. doi: 10.1183/09031936.00088814 [DOI] [PubMed] [Google Scholar]
- 27.Spahn JD, Covar R. Clinical assessment of asthma progression in children and adults. J Allergy Clin Immunol. 2008;121(3):548–557. doi: 10.1016/j.jaci.2008.01.012 [DOI] [PubMed] [Google Scholar]
- 28.Takase M, Sakata H, Shikada M, et al. Standardization of predicted values of spirogram for Japanese Children (Final Report). Jpn J Pediatr Pulmonol. 2008;9:164–176. Japanese. [Google Scholar]
- 29.Soriano JB, Miravitlles M, García-Río F, et al. Spirometrically-defined restrictive ventilatory defect: population variability and individual determinants. Prim Care Respir J. 2012;21(2):187–193. doi: 10.4104/pcrj.2012.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sekerel BE, Civelek E, Karabulut E, et al. Are risk factors of childhood asthma predicting disease persistence in early adulthood different in the developing world? Allergy. 2006;61(7):869–877. doi: 10.1111/j.1398-9995.2006.01082.x [DOI] [PubMed] [Google Scholar]
- 31.The Japanese Society for Pediatric Endocrinology. Clinical growth charts. Available from: http://jspe.umin.jp/index.html. Accessed October 6, 2019. Japanese.
- 32.Suwa S, Tachibana K, Maesaka H, et al. Longitudinal standards for height and height velocity for Japanese children from birth to maturity. Clin Pediatr Endocrinol. 1992;1(1):5–13. doi: 10.1297/cpe.1.5 [DOI] [Google Scholar]
- 33.Duan P, Wang Y, Lin R, et al. Impact of early life exposures on COPD in adulthood: a systematic review and meta-analysis. Respirology. 2021;26(12):1131–1151. doi: 10.1111/resp.14144 [DOI] [PubMed] [Google Scholar]
- 34.Okyere DO, Bui DS, Washko GR, et al. Predictors of lung function trajectories in population-based studies: a systematic review. Respirology. 2021;26(10):938–959. doi: 10.1111/resp.14142 [DOI] [PubMed] [Google Scholar]
- 35.Ali KM. Childhood asthma as a risk factor for adult chronic obstructive pulmonary disease: a systematic review and meta-analysis. Expert Rev Respir Med. 2020;29:1–7. doi: 10.1080/17476348.2021.1864328 [DOI] [PubMed] [Google Scholar]
- 36.Leung TF, Tang MF, Leung ASY, Tam WWS, Sy HY, Wong GWK. Trajectory of spirometric and exhaled nitric oxide measurements in Chinese schoolchildren with asthma. Pediatr Allergy Immunol. 2018;29(2):166–173. doi: 10.1111/pai.12836 [DOI] [PubMed] [Google Scholar]
- 37.Kelly WJ, Hudson I, Raven J, Phelan PD, Pain MC, Olinsky A. Childhood asthma and adult lung function. Am Rev Respir Dis. 1988;138(1):26–30. doi: 10.1164/ajrccm/138.1.26 [DOI] [PubMed] [Google Scholar]
- 38.Ortega H, Yancey SW, Keene ON, Gunsoy NB, Albers FC, Howarth PH. Asthma exacerbations associated with lung function decline in patients with severe eosinophilic asthma. J Allergy Clin Immunol Pract. 2018;6(3):980–986.e1. doi: 10.1016/j.jaip.2017.12.019 [DOI] [PubMed] [Google Scholar]
- 39.Silkoff PE, Laviolette M, Singh D, et al. Longitudinal stability of asthma characteristics and biomarkers from the Airways Disease Endotyping for Personalized Therapeutics (ADEPT) study. Respir Res. 2016;17:43. doi: 10.1186/s12931-016-0360-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matsunaga K, Hirano T, Oka A, et al. Progression of irreversible airflow limitation in asthma: correlation with severe exacerbations. J Allergy Clin Immunol Pract. 2015;3(5):759–64.e1. doi: 10.1016/j.jaip.2015.05.005 [DOI] [PubMed] [Google Scholar]
- 41.O’Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW; START Investigators Group. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009;179(1):19–24. doi: 10.1164/rccm.200807-1126OC [DOI] [PubMed] [Google Scholar]
- 42.Çolak Y, Afzal S, Nordestgaard BG, et al. Young and middle-aged adults with airflow limitation according to lower limit of normal but not fixed ratio have high morbidity and poor survival: a population-based prospective cohort study. Eur Respir J. 2018;51(3):1702681. doi: 10.1183/13993003.02681-2017 [DOI] [PubMed] [Google Scholar]
- 43.Swanney MP, Ruppel G, Enright PL, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63(12):1046–1051. doi: 10.1136/thx.2008.098483 [DOI] [PubMed] [Google Scholar]
- 44.Smith LJ. The lower limit of normal versus a fixed ratio to assess airflow limitation: will the debate ever end? Eur Respir J. 2018;51(3):1800403. doi: 10.1183/13993003.00403-2018 [DOI] [PubMed] [Google Scholar]
- 45.Hopp RJ, Wilson MC, Pasha MA. Small airway disease in pediatric asthma: the who, what, when, where, why, and how to remediate. A review and commentary. Clin Rev Allergy Immunol. 2020;62(1):145–159. doi: 10.1007/s12016-020-08818-1 [DOI] [PubMed] [Google Scholar]
- 46.Beydon N, Davis SD, Lombardi E, et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med. 2007;175(12):1304–1345. doi: 10.1164/rccm.200605-642ST [DOI] [PubMed] [Google Scholar]
- 47.Deliu M, Fontanella S, Haider S, et al. Longitudinal trajectories of severe wheeze exacerbations from infancy to school age and their association with early-life risk factors and late asthma outcomes. Clin Exp Allergy. 2020;50(3):315–324. doi: 10.1111/cea.13553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeiger RS, Dawson C, Weiss S. Relationships between duration of asthma and asthma severity among children in the Childhood Asthma Management Program (CAMP). J Allergy Clin Immunol. 1999;103(3 Pt 1):376–387. doi: 10.1016/s0091-6749(99)70460-4 [DOI] [PubMed] [Google Scholar]
- 49.Tse SM, Coull BA, Sordillo JE, Datta S, Gold DR. Gender- and age-specific risk factors for wheeze from birth through adolescence. Pediatr Pulmonol. 2015;50(10):955–962. doi: 10.1002/ppul.23113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mohammad HR, Belgrave D, Harding KK, et al. Age, sex and the association between skin test responses and IgE titres with asthma. Pediatr Allergy Immunol. 2016;27(3):313–319. doi: 10.1111/pai.12534 [DOI] [PubMed] [Google Scholar]
- 51.Allinson JP, Afzal S, Çolak Y, et al. Changes in lung function in European adults born between 1884 and 1996 and implications for the diagnosis of lung disease: a cross-sectional analysis of ten population-based studies. Lancet Respir Med. 2022;10(1):83–94. doi: 10.1016/S2213-2600(21)00313-1 [DOI] [PubMed] [Google Scholar]
- 52.Ministry of education, culture, sports, science and technology in Japan. Available from: https://www.mext.go.jp/index.htm. Accessed November 10, 2021. Japanese.
- 53.Yoshihara S, Yoshida T, Kurosaka F, et al. Internet survey of childhood asthma and use of inhaled therapy in the home in Japan. Pediatr Int. 2008;50(4):495–499. doi: 10.1111/j.1442-200X.2008.02704.x [DOI] [PubMed] [Google Scholar]