Abstract
State-level all-payer claims databases (APCDs) are a possible new public health surveillance tool, but their reliability is unclear. We compared Colorado’s APCD with other state-level databases for use in monitoring the opioid epidemic (Colorado Hospital Association and Colorado’s Prescription Drug Monitoring Program database for 2010–2017), using descriptive analyses comparing quarterly counts/rates of opioid-involved inpatient and emergency department visits and counts/rates of 30-day opioid fills between databases. Utilization is lower in the Colorado APCD than the other databases for all outcomes but trends are parallel and consistent between databases. State APCDs hold promise for researchers, but they may be better suited to individual-level analyses or comparisons of providers than for surveillance of public health trends related to addiction.
Keywords: All-Payer Claims Database, opioid utilization, opioid-related harms, Colorado Hospital Association, Prescription Drug Monitoring Program, claims data analysis
Introduction
As the opioid epidemic continues to evolve and plague the United States, high-quality data systems that can be used to monitor and evaluate the impact of policies being adopted to tackle the epidemic at more localized levels is becoming increasingly more important. As is true for many health conditions, public health officials, researchers, and others have relied on a variety of databases to monitor the opioid epidemic over the past decade (Smart et al., 2018), including hospital discharge data (Liu et al., 2020), claims data (Bradford & Bradford, 2016; Bradford et al., 2018; Brummett et al., 2019; Burke et al., 2020; Heins et al., 2018), pharmacy dispensing (Guy et al., 2019), worker’s compensation data (Buttorff et al., 2017; Heins et al., 2016; Tenney et al., 2019), and of course mortality data (Bachhuber et al., 2014; Centers for Disease Control and Prevention [CDC], 2014; Mattson et al., 2021). Administrative data sources like these have a key advantage in allowing researchers to track behaviors at different parts of the use cycle, from the initiation of opioid use, to the escalation to problematic use (through measures of doctor, pharmacy shopping, or high dose fills) to harms from misuse (accidents, poisonings, and cardiac events). A key drawback for most administrative data is that the same individual cannot always be viewed across all payers due to nonunique identifiers or changes in health insurance.
State-level, all-payer claims databases (APCDs) are a newer, additional public health surveillance tool for monitoring substance abuse. They can include medical, dental, and pharmacy claims for the same individual across multiple payers (Agency for Healthcare Research and Quality [AHRQ], 2017, 2018; Carman et al., 2021; McCarthy, 2020). APCDs typically include private and public payers and health care received at multiple care sites (inpatient, outpatient, etc.), making them more comprehensive than some national databases. However, they may be missing some large employers or other payers within the state due to court cases that exempted large, self-insured employers from submitting.1 In the case of studying opioid prescribing or misuse, APCDs may be additionally limited because of a change in the interpretation of federal guidelines related to redaction of addiction-related claims prior to sharing claims data externally that were in place from 2013 through 2017 (Frakt & Bagley, 2015). As noted by various authors (Austin et al., 2018; Frakt & Bagley, 2015), the implication of these redacted claims has important long-term implications, particularly for studies examining health conditions influenced by addiction to substances like opioids and alcohol.
This study investigates how well the information on opioid-specific outcomes in Colorado’s APCD compare with those from two other statewide data sources, which in theory should contain comparable health outcome data for the entire state without redaction: (a) Colorado Hospital Association’s (CHA) hospital claims data and (b) the Colorado Prescription Drug Monitoring Program (PDMP). The objective of this study was to compare opioid-related inpatient, emergency department (ED), and prescription fill data within the APCD with other statewide systems to assess how well the APCD tracked levels and trends in opioid-related outcomes. Whereas national payer databases have been used to examine the opioid epidemic (Brummett et al., 2019; Dilonardo et al., 2000; Kirson et al., 2012; Saloner et al., 2017), very few studies have been published using state-level APCDs (Bartels et al., 2018; Burke et al., 2020; LeBaron et al., 2019; Malon et al., 2018) and the implications of doing so are relatively unknown.
Colorado represents an important market for conducting this study in that it was among the first states to implement an APCD (beginning in 2010), it has ongoing evidence of an opioid problem (National Institute on Drug Abuse, 2020), and multiple researchers are examining how Colorado’s harm reduction strategies, particularly cannabis legalization, have influenced opioid-related harm (Bradford & Bradford, 2016; Davis et al., 2016; Livingston et al., 2017; Shi et al., 2019; Wen & Hockenberry, 2018).
New Contribution
APCDs are a promising new source of data for understanding changing patterns of medical care and surveillance. As of 2020, 18 states have mandated the creation of an APCD, and an additional 30 are developing or exploring the concept (APCD Council, 2020). We assessed Colorado’s APCD for examining the opioid epidemic and found that it is better suited to more focused research questions on individuals or providers than surveillance of trends in substance abuse diagnoses. Few peer-reviewed studies have used the Colorado APCD, and we also contribute to the knowledge base of using this data source (Bartels et al., 2018; Panhans, 2019).
Methods
We use an observational study design to examine differences in cases, rates, and trends in opioid-related measures constructed similarly in each of three data sets. Our primary data set is the 2010–2017 Colorado APCD. Launched in 2010 (although began data collection in 2012, retrospective to 2010), Colorado’s APCD today contains claims for the majority of insured Coloradans (4.3 million unique individuals) from more than 33 commercial payers, as well as Medicare and Medicaid (Center for Improving Value in Health Care [CIVHC], 2020a). Self-insured plans do not have to report claims under current law, so some commercially insured adults in Colorado are not included, although a few large self-insured firms voluntarily participate. Our APCD data were limited by the APCD’s data release committee to adults aged 21 to 64 with either an opioid-involved diagnosis or a diagnosis code where opioids could plausibly be used in treatment.
The APCD is limited in the number of abuse and dependence codes it contains for any drug, due to the Colorado APCD’s interpretation of federal privacy laws (Substance Abuse and Mental Health Services Administration, 2017). The database requested payers redact medical claims with certain substance abuse diagnosis codes from their data prior to submitting until 2017, and now leaves it up to non–federally funded payers whether to submit these claims (CIVHC, 2020b). This results in variation across payers in which claims are submitted. This policy does not affect claims with poisoning codes or prescription drug claims (which do not contain diagnosis codes).
The second data set comes from CHA for 2010–2017 and includes opioid-involved inpatient and ED visits (the ED data are only available starting in 2013). The CHA data include information from the majority of the 108 hospitals in Colorado, depending on the year (CHA, 2014). The CHA includes all ED and inpatient visits, regardless of payer or ability to pay.
The third data set is the Colorado PDMP from 2013 to 2017, which captures all pharmacy claims filled, regardless of source of payment, for any Scheduled II to V drug on the Colorado Uniformed Controlled Substance Act (Colorado Revised Statutes Title 18—Criminal Code Article 18—Uniform Controlled Substances Act of 2013, 2017). Although the PDMP is available before 2013, the data appear underreported prior to the organization switching data vendors in late 2012.
We chose three primary opioid-involved outcomes to consider across these data sets. First, to capture opioid-related harm, we constructed in the CHA inpatient data and APCD data measures of an opioid-involved inpatient and ED visits. Opioid-involved inpatient and ED visits were defined using the International Classification of Disease (ICD) Version 10 codes and their corresponding Version 9 codes (the switch occurred in October 2015). For brevity, we report just the Version 10 codes, which include F11* (opioid use, misuse or dependence), T40* and T507* (opioid poisonings), and Z798* (the long-term use of opioids). The actual number of opioid-involved inpatient stays as well as the rates are included, using the number of enrolled persons as the denominator for the APCD and the county population estimate from the American Community Survey as the denominator for CHA and the PDMP. The second opioid-involved outcome was the number and rate of opioid-involved ED visits using both the CHA and APCD. We used the same ICD-9 and ICD-10 codes to construct the ED measures.
Our third was the number and rate (per 10,000 patients or population) of 30-day opioid prescriptions filled per quarter. Unique prescription claims are identified using National Drug Codes (NDCs), which contain information on the manufacturer and active ingredient. Each prescription may be filled for a specific number of days, such as 7 or 30. We standardized each prescription to the number of 30-day fills, so a 7-day fill counts as 0.23 of a fill. We identified opioids using the CDC’s (2020) list of outpatient opioids in conjunction with a therapeutic classification scheme that classifies individual drugs into classes, such as opioids.
We used descriptive methods to compare the opioid-related ED and inpatient visits between the APCD and CHA, and the number of 30-day fills between the APCD and PDMP. We used Stata, Version 16, for all analyses. The RAND Human Subjects Protection Committee deemed this study to be exempt from human subjects protections.
Findings
Overall, the number of opioid-related inpatient hospital and ED (after 2013) visits are much lower in the APCD than CHA (Figure 1). There were 1,986 inpatient visits for opioid-related harms in the CHA data in Q4 2010 (quarter 4), which increased to 3,199 in Q4 2017. Inpatient visits reached a maximum of 3,493 visits in Q3 2016. Inpatient hospital visits reported to the APCD also increased from 192 to 1,043, in the same quarters. Starting in Q1 2013, CHA ED visits increased from 2,075 to 3,000 in Q4 2017, while ED visits for opioid-related harms in the APCD increased from 651 to 1,181, respectively. Both APCD ED and CHA ED visits peaked in Q3 2016. The solid vertical line in Figure 1 during 2015 indicates the point at which ICD-9 codes were transitioned to ICD-10 codes, and it is clear that this affected the number of opioid-involved inpatient and ED visits in both data systems.
Figure 1.
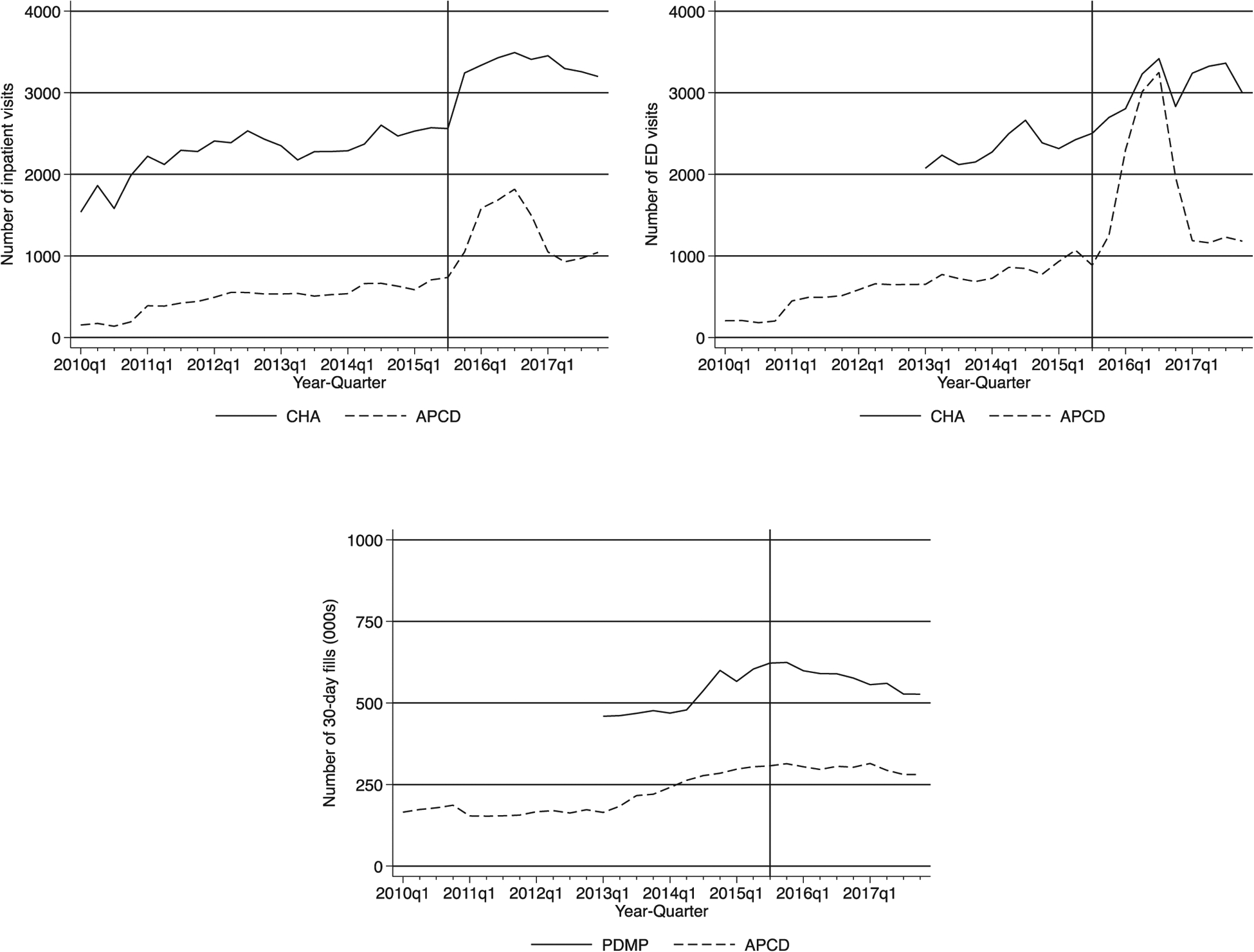
Number of Opioid-Related Inpatient and ED Visits and Opioid Prescription Fills, Statewide per Quarter, 2010–2017.
Note. The trendlines show the statewide per capita counts of inpatient, ED visits for opioid-related harms, and 30-day prescription fills by quarter. CHA’s ED data and data from PDMP are only available from 2013 onward. CHA = Colorado Hospital Association; APCD = Colorado’s All-Payer Claims Database; PDMP = Prescription Drug Monitoring Database; ED = emergency department.
Both the APCD and the PDMP show the number of 30-day fills for opioid prescriptions continued to increase through the end of 2015, and began declining thereafter. The PDMP had 459,346 thirty-day prescription opioid fills in Q1 2013 and 623,956 in Q4 2015 (a 40% increase). Even after the peak, Coloradans still filled more than 500,000 thirty-day fills of opioids in 2017 (526,789 in Q4 2017). The number of 30-day fills in the APCD show a similar pattern to PDMP at a lower level, increasing from 186,557 in Q4 2010 to 280,547 in Q4 2017.
While we expect that the APCD would have fewer counts of both visits and prescription drugs, we may expect the rates to be similar for the outcomes between the three databases, as the rates adjust for population size captured in each dataset. Figure 2 presents each outcome in each database per 10,000 people. The trends are similar, but the rates are still higher in CHA than in the APCD.
Figure 2.
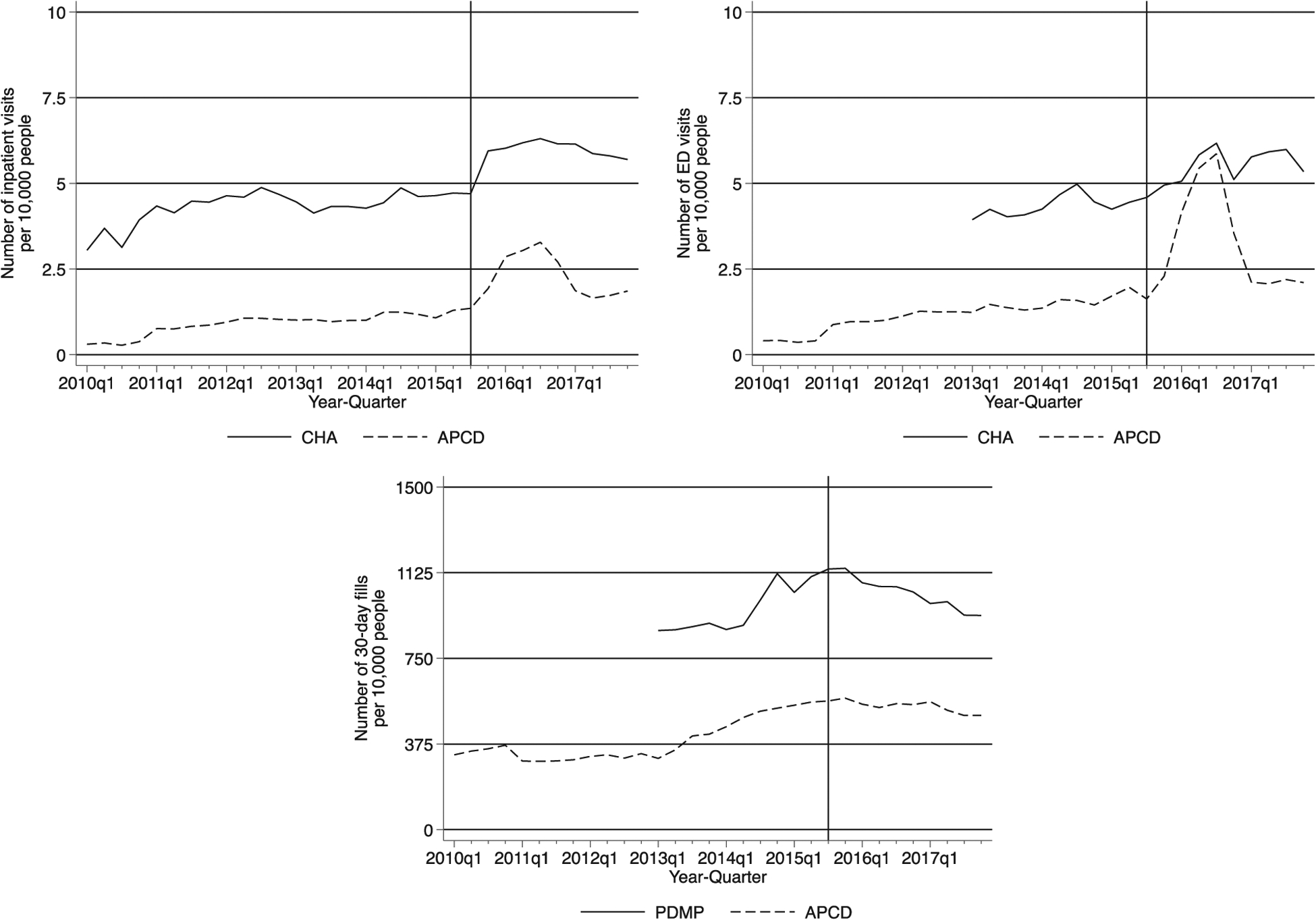
Statewide per Capita Figures.
Note. The trendlines show the statewide per capita counts of inpatient, ED visits for opioid-related harms, and 30-day prescription fills by quarter. CHA’s ED data and data from PDMP are only available from 2013 onward. CHA = Colorado Hospital Association; APCD = Colorado’s All-Payer Claims Database; PDMP = Prescription Drug Monitoring Database; ED = emergency department.
In addition to the main findings, both figures show a large spike in opioid-related claims for the APCD in 2016. We found that this spike was due to one large insurer who was inadvertently including claims for three of the four quarters within the year with substance abuse codes that others were redacting, and the insurer changed its behavior in subsequent periods.
Discussion
As the opioid epidemic continues to evolve in response to various strategies being tried in local jurisdictions, the need for comprehensive data to help monitor how use patterns and public health harms change in those jurisdictions becomes increasingly important. State-level APCDs are a burgeoning resource for studying many health conditions, although they have limitations for studies evaluating opioid use disorder and opioid treatment that researchers and public health officials need to understand. In our comparison of Colorado’s relatively mature APCD with two other state-level data sources capturing similar health outcomes for the full state population, we found generally consistent trends between the CHA ED visits and inpatient visits and the APCD ED and inpatient visits, with both databases showing a general rise in each from 2010 through 2017. The level estimates across these two data sources, whether measured in terms of absolute numbers or rates per 10,000 patients, are considerably different, however. This is due to the differing populations captured in each. Trends in opioid prescriptions were also consistent between the APCD and PDMP, with both systems showing a peak in opioid prescribing in 2015, much later than the peak observed in national data (IQVIA, 2018). Despite a decline in overall opioid prescribing starting in 2015, there continues to be an increase in opioid-related overdoses in Colorado, which may be due to lasting effects of opioid use or substitution toward illegal drug markets (Rudd et al., 2016; Schieber et al., 2019; Scholl et al., 2018).
Affecting all claims databases is the switch from ICD-9 to ICD-10 diagnosis codes that occurred in October 2015, partway through our study period of 2010–2017, which may contribute to the increase in ED and inpatient visits we observe in late 2015. There are many more diagnosis codes in Version 10 than Version 9, which may have increased the number of claims coded with specific diagnoses as providers became more familiar with the ICD-10 codes in the initial period after the switch. This makes it difficult to be sure whether the number of opioid-related hospital visits is truly increasing in comparison with the pre–October 2015 period versus an artifact of coding differences. The conversion in diagnosis code schemes would not affect the number of prescription opioids filled as diagnosis codes are not associated with prescription drug claims. We observe an increase in opioid prescription fills through the end of 2015, which may indicate that problems associated with opioid use that lead to hospital visits could still be increasing, and thus the bump observed is not strictly an artifact of the change in coding schemes.
APCDs are more aptly termed “multi-payer” rather than “all payer” databases as they exclude important populations. They generally cannot capture the utilization for the uninsured or those paying cash for services, which is particularly important for opioid research. Many opioids are cheaply available as generics, and paying cash is a way to circumvent payer policies attempting to restrict opioid utilization. In addition, APCDs also exclude some privately insured residents who receive their insurance through a self-insured firm that is not required to submit data. This can result in large omissions for some states, depending on the number of residents employed by self-insured employers. There may also be issues with integrating encounters from capitated plans within the state (such as Kaiser Permanente or Medicaid behavioral health organizations).
As we noted in the introduction, APCDs may not have all data processing steps in perfect order, particularly in early stages of development, and data quality for APCDs has been a challenge to using the data (Carman et al., 2021). Issues with harmonizing or cleaning claims from multiple payers can give rise to variation in fields reported. We identified that the Colorado’s APCD’s redaction request was not followed uniformly by all payers or even within payers over time. The temporary inclusion of these data by one payer could have a profound impact on conclusions drawn from these data if one was not careful in identifying the cause for the increase. As a result, the Colorado APCD is less useful for studying research questions related to the utilization of treatment services or costs of care for individuals with substance abuse diagnoses, although it is still useful for looking at patterns of care for individuals filling large numbers of opioid prescriptions, for example. Users of other APCD data should pay close attention to whether such inconsistencies in data submission may be affecting trends in their data. Efforts across the county to improve interoperability between insurers and providers should improve the data quality for APCDs, and in fact, the APCD council (2021) has been working on a set of submission guidelines to improve the quality of submitted data.
Despite the identified drawbacks for substance abuse research, APCDs like Colorado’s are still useful for research, primarily for studying care patterns, cost, or quality of care at the individual patient or provider level. Additional benefits of APCDs include granular geographic data, details on longitudinal patient care, particularly if a patient switches insurance carriers, and more complete estimates of total health care costs (AHRQ, 2018; Diaz-Perez et al., 2019; Peters et al., 2014; Rocco et al., 2017). APCDs may also be useful in assisting state and federal policy makers with quality improvement initiatives, such as in the reporting of opioid quality measures to state or federal agencies (Centers for Medicare & Medicaid Services, 2021). In fact, Colorado’s APCD has served that role in developing and reporting quality measures for the state’s evaluation of a payment innovation model for Medicaid providers (CIVHC, 2021).
Although the CHA and PDMP databases do supposedly represent the population of the state, we know not all hospitals report data to CHA, and the PDMP also had variable reporting from pharmacies prior to a vendor switch in 2012. Both databases also focus on more narrow care settings and care utilization than the APCD. CHA is solely focused on hospital utilization, while the PDMP is focused on Drug Enforcement Agency-scheduled prescription drug utilization filled through retail pharmacies.
The findings in this article show that while APCDs hold wonderful promise for researchers interested in substance abuse–related research, they may not be well suited for analyzing opioid-related outcomes on a population level due to the particular relevance of some of the excluded populations for this condition (e.g., the uninsured) or the inconsistent behavior of payers in redacting the addiction claims. State APCDs may be better suited to studies of individual patient groups or providers (Table 1)
Table 1.
Approximate Sample Sizes for the Three Databases Used in the Analysis.
| Database and Claim Type | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| Number of covered lives | ||||||||
| APCD—Enrollment (distinct members) | 843,394 | 891,647 | 1,049,479 | 1,213,556 | 1,549,301 | 1,775,887 | 1,840,571 | 1,882,852 |
| Number of claims in sample used in analysis | ||||||||
| APCD—Medical | 9,862,742 | 10,943,442 | 15,230,809 | 16,928,083 | 21,029,142 | 25,466,675 | 26,719,573 | 27,902,642 |
| APCD—Prescription | 12,152,028 | 13,042,661 | 12,608,940 | 13,844,431 | 20,091,790 | 22,376,246 | 23,464,471 | 21,342,530 |
| CHA—Inpatient | 150,002 | 181,708 | 183,073 | 186,780 | 194,867 | 216,959 | 194,084 | 203,171 |
| CHA—ED | 262 | 533,818 | 565,241 | 637,633 | 675,668 | 641,963 | ||
| PDMP | 8,403,914 | 8,780,577 | 9,037,620 | 8,842,955 | 8,434,774 | |||
Note. The APCD enrollment numbers in this table do not represent the full APCD. Our data consist of adults aged 21 to 64 with certain conditions that might be treated with opioids. We also drop a small number of members with inconsistent scrambled patient identifiers where the APCD could not uniquely identify these individuals across payers. CHA and the PDMP effectively represent the entire population of Colorado, which is currently about 5.7 million people. The CHA counts presented here are a subset of their entire database for claims with opioid-related ED or inpatient visits. The PDMP contains information on prescriptions for scheduled drugs, a subset of all prescription drugs. CHA ED and PDMP are only available from 2013 to 2017. APCD = Colorado’s All-Payer Claims Database; CHA = Colorado Hospital Association; ED = emergency department; PDMP = Prescription Drug Monitoring Database.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The National Institute on Drug Abuse funded this study (Grant No. 1R01DA045051).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Code Availability
As we cannot share the data, we do not feel it makes sense to share analytic code either, although we are happy to by request.
Availability of Data and Material
The data are proprietary and thus cannot be shared.
References
- Agency for Healthcare Research and Quality. (2017). Data evaluation of All-Payer Claims Databases: Inventory and prioritization of measures to support the growing effort in transparency using All-Payer Claims Databases. https://www.ahrq.gov/data/apcd/backgroundrpt/data.html
- Agency for Healthcare Research and Quality. (2018). All Payer’s Claim Databases. https://www.ahrq.gov/data/apcd/index.html#i
- All-Payer Claims Database Council. (2020). Interactive State Report Map. https://www.apcdcouncil.org/state/map
- All-Payer Claims Database Council. (2021). Common data layout. https://www.apcdcouncil.org/common-data-layout
- Austin AM, Bynum JPW, Maust DT, Gottlieb DJ, & Meara E (2018). Long-term implications of a short-term policy: Redacting substance abuse data. Health Affairs, 37(6), 975–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, & Barry CL (2014). Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Internal Medicine, 174(10), 1668–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels K, Fernandez-Bustamante A, McWilliams SK, Hopfer CJ, & Mikulich-Gilbertson SK (2018). Long-term opioid use after inpatient surgery—A retrospective cohort study. Drug and Alcohol Dependence, 187, 61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford AC, & Bradford WD (2016). Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Affairs, 35(7), 1230–1236. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, Abraham A, & Bagwell Adams G (2018). Association between US state medical cannabis laws and opioid prescribing in the Medicare Part D population. JAMA Internal Medicine, 178(5), 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brummett CM, England C, Evans-Shields J, Kong AM, Lew CR, Henriques C, Zimmerman NM, Pawasauskas J, & Oderda G (2019). Health care burden associated with outpatient opioid use following inpatient or outpatient surgery. Journal of Managed Care & Specialty Pharmacy, 25(9), 973–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LG, Zhou X, Boyle KL, Orav EJ, Bernson D, Hood ME, Land T, Bharel M, & Frakt AB (2020). Trends in opioid use disorder and overdose among opioid-naive individuals receiving an opioid prescription in Massachusetts from 2011 to 2014. Addiction, 115(3), 493–504. [DOI] [PubMed] [Google Scholar]
- Buttorff C, Trujillo AJ, Castillo R, Vecino-Ortiz AI, & Anderson GF (2017). The impact of practice guidelines on opioid utilization for injured workers. American Journal of Industrial Medicine, 60(12), 1023–1030. [DOI] [PubMed] [Google Scholar]
- Carman KG, Dworsky M, Heins SE, Schwam D, Shelton S, & Whaley C (2021). The history, promise and challenges of State All Payer Claims Databases: Background memo for the State All Payer Claims Database Advisory Committee to the Department of Labor. U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. [Google Scholar]
- Center for Improving Value in Health Care. (2020a). CO APCD overview. https://www.civhc.org/get-data/co-apcd-info/
- Center for Improving Value in Health Care. (2020b). Plaintalk blog: Why the CO APCD does not have substance use disorder claims. https://www.civhc.org/2019/03/21/plaintalk-blog-why-the-co-apcd-does-not-have-substance-use-disorder-claims/
- Center for Improving Value in Health Care. (2021). Colorado State Innovation Model. http://www.civhc.org/change-agent-gal-lery/colorado-state-innovation-model/
- Centers for Disease Control and Prevention. (2014). Drugpoisoning deaths involving opioid analgesics: United States, 1999–2011. https://pubmed.ncbi.nlm.nih.gov/25228059/
- Centers for Disease Control and Prevention. (2020). Data resources: Analyzing prescription data and morphine milligram equivalents (MME). https://www.cdc.gov/drugoverdose/resources/data.html
- Centers for Medicare & Medicaid Services. (2021). Meaningful measures hub. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page#Measurement_Areas
- Colorado Hospital Association. (2014). CHA Databank. http://www.cha.com/Member-Services/CHA-DATABANK.aspx
- Colorado Revised Statutes Title 18—Criminal Code Article 18—Uniform Controlled Substances Act of 2013. (2017).
- Davis JM, Mendelson B, Berkes JJ, Suleta K, Corsi KF, & Booth RE (2016). Public health effects of medical marijuana legalization in Colorado. American Journal of Preventive Medicine, 50(3), 373–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Perez MJ, Hanover R, Sites E, Rupp D, Courtemanche J, & Levi E (2019). Producing comparable cost and quality results from All-Payer Claims Databases. The American Journal of Managed Care, 25(5), e138–e144. [PMC free article] [PubMed] [Google Scholar]
- Dilonardo J, Chalk M, Mark TL, Coffey RM, & CSAT/CMHS Spending Estimates Team. (2000). Recent trends in the financing of substance abuse treatment: Implications for the future. Health Services Research, 35(5, Pt 3), 60–71. [PMC free article] [PubMed] [Google Scholar]
- Frakt AB, & Bagley N (2015). Protection or harm? Suppressing substance-use data. The New England Journal of Medicine, 372(20), 1879–1881. [DOI] [PubMed] [Google Scholar]
- Guy G, Haegerich TM, Evans ME, Losby JL, Young R, & Jones CM (2019). Vital signs: Pharmacy-based naloxone dispensing—United States, 2012–2018. Morbidity and Mortality Weekly Report, 68(31), 679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heins SE, Feldman DR, Bodycombe D, Wegener ST, & Castillo RC (2016). Early opioid prescription and risk of long-term opioid use among US workers with back and shoulder injuries: A retrospective cohort study. Injury Prevention, 22(3), 211–215. [DOI] [PubMed] [Google Scholar]
- Heins SE, Sorbero MJ, Jones CM, Dick AW, & Stein BD (2018). High-risk prescribing to Medicaid enrollees receiving opioid analgesics: Individual- and county-level factors. Substance Use & Misuse, 53(10), 1591–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IQVIA. (2018). Medicine use and spending in the U.S.: A review of 2017 and Outlook to 2022 IQVIA Institute for Human Data Science. [Google Scholar]
- Kirson NY, White AG, Birnbaum HG, Schiller M, Waldman T, Peterson K, Ben-Joseph RH, Berner T, & Summers KH (2012). Direct and indirect costs of patients treated with extended-release oxymorphone HCl or controlledrelease oxycodone HCl. Journal of Medical Economics, 15(1), 87–95. [DOI] [PubMed] [Google Scholar]
- LeBaron VT, Camacho F, Balkrishnan R, Yao NA, & Gilson AM (2019). Opioid epidemic or pain crisis? Using the Virginia All Payer Claims Database to describe opioid medication prescribing patterns and potential harms for patients with cancer. Journal of Oncology Practice, 15(12), e997–e1009. [DOI] [PubMed] [Google Scholar]
- Liu S, Scholl L, Hoots B, & Seth P (2020). Nonfatal drug and polydrug overdoses treated in emergency departments—29 states, 2018–2019. Morbidity and Mortality Weekly Report, 69(34), 1149–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston MD, Barnett TE, Delcher C, & Wagenaar AC (2017). Recreational cannabis legalization and opioid-related deaths in Colorado, 2000–2015. American Journal of Public Health, 107(11), 1827–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malon J, Shah P, Koh WY, Cattabriga G, Li E, & Cao L (2018). Characterizing the demographics of chronic pain patients in the state of Maine using the Maine all payer claims database. BMC Public Health, 18(1), Article 810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, & Davis NL (2021). Trends and geographic patterns in drug and synthetic opioid overdose deaths — United States, 2013–2019. MMWR Morbidity and Mortality Weekly Report, 70(6), 202–207. 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy D (2020, December 10). State All-Payer Claims Databases: Tools for improving health care value, part 2 [Report]. The Commonwealth Fund. [Google Scholar]
- National Institute on Drug Abuse. (2020). Colorado: Opioid-involved deaths and related harms. https://www.drugabuse.gov/drug-topics/opioids/opioid-summaries-by-state/Colorado-opioid-involved-deaths-related-harms
- Panhans M (2019). Adverse selection in ACA exchange markets: Evidence from Colorado. American Economic Journal: Applied Economics, 11(2), 1–36. [Google Scholar]
- Peters A, Sachs J, Porter J, Love D, & Costello A (2014). The value of All-Payer Claims Databases to states. North Carolina Medical Journal, 75(3), 211–213. [DOI] [PubMed] [Google Scholar]
- Rocco P, Kelly AS, Beland D, & Kinane M (2017). The new politics of US health care prices: Institutional reconfiguration and the emergence of All-Payer Claims Databases. Journal of Health Politics, Policy and Law, 42(1), 5–52. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, & Scholl L (2016). Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morbidity and Mortality Weekly Report, 65(50–51), 1445–1452. [DOI] [PubMed] [Google Scholar]
- Saloner B, Daubresse M, & Caleb Alexander G (2017). Patterns of buprenorphine-naloxone treatment for opioid use disorder in a multistate population. Medical Care, 55(7), 669–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieber LZ, Guy G, Seth P, Young R, Mattson CL, Mikosz CA, & Schieber RA (2019). Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006–2017. JAMA Network Open, 2(3), Article e190665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, & Baldwin G (2018). Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity and Mortality Weekly Report, 67(5152), 1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Liang D, Bao Y, An R, Wallace MS, & Grant I (2019). Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug and Alcohol Dependence, 194, 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, Kase CAM, & Stein B (2018). Data sources and data-linking strategies to support research to address the opioid crisis. U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation, Office of Health Policy. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Federal Register: 42 CFR part 2: Confidentiality of substance use disorder patient records: Final rule—Rules and regulations (pp. 6052–6127). Department of Health and Human Services. [PubMed] [Google Scholar]
- Tenney L, McKenzie LM, Matus B, Mueller K, & Newman LS (2019). Effect of an opioid management program for Colorado workers’ compensation providers on adherence to treatment guidelines for chronic pain. American Journal of Industrial Medicine, 62(1), 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, & Hockenberry JM (2018). Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Internal Medicine, 178(5), 673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are proprietary and thus cannot be shared.


