The winter months normally bring a higher number of respiratory viruses as people spend more time indoors together and the cold, dry air allows viruses to survive, and infect people, more easily. The last two winters, however, have been very different. During both the 2020–21 and 2021–22 winter seasons, rates of COVID-19 were high and people were physical distancing, and wearing masks. This meant that the rates of influenza, RSV, rhinovirus, and other respiratory viral infections were incredibly low compared with previous winters. But as we have entered the warmer summer months in 2022, when rates of respiratory viral infections would normally be very low or absent, some countries have seen unusual seasonal changes in the prevalence of RSV, influenza, and parainfluenza.
Many public health restrictions related to the pandemic have been slowly lifted in recent months. Face masks are now optional in many places, people are no longer physical distancing, and large indoor public gatherings have resumed, so viruses are now more easily able to spread. But the surge of respiratory illnesses is likely due not only to the reduction in COVID-19 mitigation measures but also to the so-called immunity debt.
The long periods without infection have affected individuals' immune memory response. Paul Hunter, professor of medicine at the University of East Anglia (Norwich, UK) explains, “For endemic infections, the number of cases of infection are generally driven by the rate at which people lose immunity.” Therefore, the longer people are not exposed to these viruses, the weaker their immune systems are to prevent infection.
Countries are seeing not only increased rates of these respiratory infections but also an increase in the severity of infection. “If people are not exposed to pathogens for an extended period of time, their mucosal immunity to infection begins to wane. The longer this time period, the more likely it is that their systemic immunity to severe infection also diminishes, meaning they are more likely to become severely ill when infected”, Hunter suggests. Australia is seeing a surge in influenza cases with a high mortality rate, combined with higher numbers of COVID-19 cases than the country has seen in previous years of the pandemic. The threat of this combination of high rates of influenza and COVID-19 has been a concern for several countries during the pandemic, but thankfully did not become a reality due to the mismatch in the timings of influenza and COVID waves of infection.
How respiratory viruses will respond to the new immune landscape is unclear and different countries are seeing different virus patterns. Professor Louis Bont, paediatric infectiologist at the Wilhelmina Children's Hospital, Netherlands, says they are seeing a sustained increase in RSV cases and the prolonged season shows no sign of slowing down. The reasons for this are not known—careful recording and sharing of surveillance data for respiratory viruses will be key. It will also be of interest to see what effect the lower rate of respiratory illnesses has on children born during the pandemic who weren't exposed to the six to eight upper respiratory infections per year that are normal in young children. Following these children as they mature will yield important information on the links between viral illness, lung development, and respiratory diseases such as asthma.
It is unclear when a more predictable pattern of respiratory viruses will return, but what measures should be taken to reduce infection risks? Vaccination against SARS-CoV-2, influenza, and pneumonia is vital to reduce the risk of severe disease. Worryingly, there has been a decrease in the uptake of vaccines in some countries during the pandemic. In the USA, by early 2022, over 9 million fewer adults had received the flu vaccine than in 2021. Vaccination is especially important in at-risk groups, such as pregnant women and people older than 65 years, and prudent use of antivirals in those at risk of serious disease will also be important. Bont emphasises, “The biggest impact from all these viruses is the lack of health-care personnel”, and the poor staffing levels in many hospitals is a concern for patient safety. Providing adequate protective equipment and support for healthcare staff is key, especially when rates of burnout are high.
The new dynamics of respiratory virus infections will require an improved understanding of how circulatory patterns have altered in the context of the COVID-19 pandemic. Health-care systems will need to assess the implications of changing patterns of infection for managing staff and resources, as pressures might occur at different times, and countries should continue to record and share surveillance data so we can all learn and be prepared in these uncertain times.
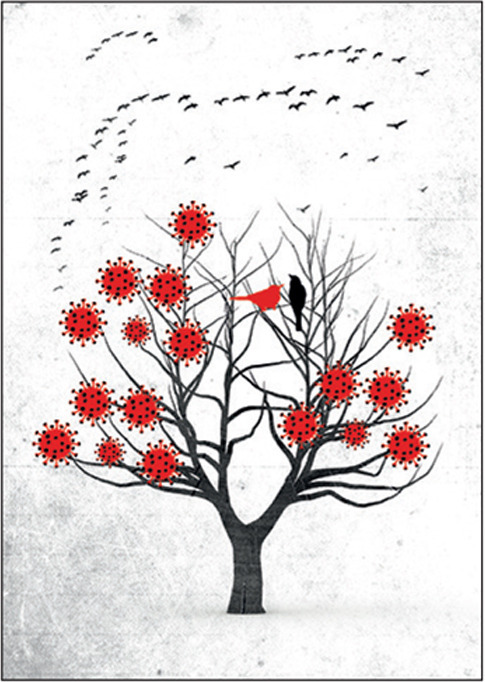
© 2022 Simone Golob/Science Photo Library


