Abstract
Background
Epithelial tubo-ovarian cancer (EOC) has high mortality partly due to late diagnosis. Prevention is available but may be associated with adverse effects. A multifactorial risk model based on known genetic and epidemiological risk factors (RFs) for EOC can help identify women at higher risk who could benefit from targeted screening and prevention.
Methods
We developed a multifactorial EOC risk model for women of European ancestry incorporating the effects of pathogenic variants (PVs) in BRCA1, BRCA2, RAD51C, RAD51D and BRIP1, a Polygenic Risk Score (PRS) of arbitrary size, the effects of RFs and explicit family history (FH) using a synthetic model approach. The PRS, PV and RFs were assumed to act multiplicatively.
Results
Based on a currently available PRS for EOC that explains 5% of the EOC polygenic variance, the estimated lifetime risks under the multifactorial model in the general population vary from 0.5% to 4.6% for the first to 99th percentiles of the EOC risk distribution. The corresponding range for women with an affected first-degree relative is 1.9%–10.3%. Based on the combined risk distribution, 33% of RAD51D PV carriers are expected to have a lifetime EOC risk of less than 10%. RFs provided the widest distribution, followed by the PRS. In an independent partial model validation, absolute and relative 5-year risks were well calibrated in quintiles of predicted risk.
Conclusion
This multifactorial risk model can facilitate stratification, in particular among women with FH of cancer and/or moderate-risk and high-risk PVs. The model is available via the CanRisk Tool (www.canrisk.org).
Keywords: genetics, public health, early diagnosis, clinical decision-making, genetic counseling
Introduction
Epithelial tubo-ovarian cancer (EOC), the seventh most common cancer in women globally, is often diagnosed at late stage and is associated with high mortality. There were 7443 new cases of EOC and 4116 deaths from EOC annually in the UK in 2015–2017.1 Early detection could lead to an early-stage diagnosis, enabling curative treatment and reducing mortality. Annual multimodal screening using a longitudinal serum CA125 algorithm in women from the general population resulted in significantly more women diagnosed with early-stage disease but without a significant reduction in mortality.2 Four-monthly screening using the same multimodal approach also resulted in a stage shift in women at high risk (>10% lifetime risk of EOC).3 Currently, risk-reducing bilateral salpingo-oophorectomy (RRSO), on completion of their families, remains the most effective prevention option,4 and it has been recently suggested that RRSO would be cost-effective in postmenopausal women at >4% lifetime EOC risk.5 6 Beyond surgical risk, bilateral oophorectomy may be associated with increased cardiovascular mortality7 and a potential increased risk of other morbidities such as parkinsonism, dementia, cardiovascular disease and osteoporosis,8 9 particularly in those who do not take menopausal hormone therapy (MHT).10 Therefore, it is important to target such prevention approaches to those at increased risk who are most likely to benefit.
Over the last decade, there have been significant advances in our understanding of susceptibility to EOC. After age, family history (FH) is the most important risk factor (RF) for the disease. Approximately 35% of the observed familial relative risk (FRR) can be explained by rare pathogenic variants (PVs) in the BRCA1, BRCA2, RAD51C, RAD51D and BRIP1 genes.11–14 Recent evidence suggests that PALB2, ATM, MLH1, MSH2 and MSH6 are also involved in the EOC genetic susceptibility.14–18 Common variants, each of small effect, identified through genome-wide association studies,19 20 explain a further 4%. Several epidemiological RFs are also known to be associated with EOC risk, including use of MHT, Body Mass Index (BMI), history of endometriosis, use of oral contraception, tubal ligation and parity.21–26 Despite these advances, those at high risk of developing EOC are currently identified mainly through FH of the disease or on the basis of having PVs in BRCA1 and BRCA2. However, more personalised risk prediction could be achieved by combining data on all known epidemiological and genetic RFs. The published EOC prediction models consider either RFs24 25 27 or common variants.24 28 No published EOC risk prediction model takes into account the simultaneous effects of the established EOC susceptibility genetic variants (rare and common), residual FH and other known RFs.
Using complex segregation analysis, we previously developed an EOC risk prediction algorithm that considered the effects of PVs in BRCA1 and BRCA2 and explicit FH of EOC and breast cancer (BC).11 The algorithm modelled the residual, unexplained familial aggregation using a polygenic model that captured other unobserved genetic effects. The model did not explicitly include the effects of other established intermediate-risk PVs in genes such as RAD51C, RAD51D and BRIP1, 12–14 29 which are now included on routine gene panel tests, the effects of recently developed EOC Polygenic Risk Scores (PRSs) or the known RFs.
Here we present a methodological framework for extending this model to incorporate the explicit effects of PVs in RAD51C, RAD51D and BRIP1 for which reliable age-specific EOC risk estimates are currently available, up-to-date PRSs and the known EOC RFs (table 1). We used this multifactorial model to evaluate the impact of negative predictive testing in families with rare PVs and to assess the extent of EOC risk stratification that can be achieved in the general population, women with a FH of EOC and those carrying rare PVs. We evaluated the performance of a subset of this model in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS),2 where women from the general population were followed up prospectively.
Table 1.
Summary of components of the EOC risk model
| RF group | RF category | Comments |
| FH | Explicit FH of ovarian and other cancers (breast, prostate, male breast and pancreatic) | Considers families of arbitrary size and structure, including affected and unaffected relatives |
| Sex | Sex of all family members | |
| Age | Ages at cancer diagnosis or current ages/age at death of family members | |
| Genetic factors | ||
| Rare truncating/pathogenic variants | BRCA1 | |
| BRCA2 | ||
| RAD51D | ||
| RAD51C | ||
| BRIP1 | ||
| Common genetic variants | Polygenic Risk Score | Explaining 5% of the polygenic variance |
| Unobserved genetic effects | Residual polygenic component | Accounts for the residual familial aggregation of EOC |
| Lifestyle/hormonal/reproductive | ||
| Height | Measured in cm (five categories) | |
| Body Mass Index | Measured in kg/m2 (three categories) | |
| Parity | Number of live births (three categories) | |
| Endometriosis | Yes/no | |
| Use of oral contraception | Years of use (five categories) | |
| Use of hormone replacement therapy | Never/ever | |
| Tubal ligation | Yes/no | |
| Breast tumour pathology | Oestrogen, progesterone, HER2 receptor, CK14, CK5/6 status | As implemented in the BOADICEA breast cancer model |
| Demographic factors | ||
| Country of origin | Country | Defines the underlying incidences used |
| Birth cohort | Defined by the person’s year of birth | Eight calendar year-specific sets of incidences |
| Family ethnicity | Ashkenazi Jewish origin | |
BOADICEA, Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm; EOC, epithelial tubo-ovarian cancer; FH, family history; RF, risk factor.
Methods
EOC risk prediction model development
No large datasets are currently available that include data on all known genetic and other EOC RFs. Therefore, we used a synthetic approach, described previously,30 to extend our previous EOC model11 by capitalising on published estimates of the associations of each RF with EOC. This approach was shown to provide valid risk estimates in the case of BC.30–32
Under the assumption that the effects of rare PVs, RFs and polygenic component are multiplicative on EOC risk, the incidence at age for individual i was modelled as
| (1) |
where is the baseline incidence. is the age-specific log-relative risk (log-RR) associated with individual ’s PV carrier status (explained further), relative to the baseline. The log-RR for non-carriers is 0. is the polygenotype for individual , assumed to follow a standard normal distribution in the general population, and is the age-specific log-RR associated with the polygene, relative to the baseline incidence. is the log-RR associated with risk-factor at age , which may depend on PV carrier status, and is the corresponding indicator variable showing the category of risk-factor for the individual. The baseline incidence was determined by constraining the overall incidences to agree with the population EOC incidence. To allow appropriately for missing RF information, only those RFs measured on a given individual are considered.
Major gene (MG) effects
To include the effects of RAD51D, RAD51C and BRIP1, we used the approach described previously where PVs in these genes were assumed to be risk alleles of a single MG locus.33 A dominant model of inheritance was assumed for all rare PVs. To define the penetrance, we assumed the following order of dominance when an individual carried more than one PV (ie, the risk was determined by the highest-risk PV and any lower-risk PVs ignored): BRCA1, BRCA2, RAD51D, RAD51C and BRIP1.33 The population allele frequencies for RAD51D, RAD51C and BRIP1 and EOC relative risks (RRs) were obtained from published data (online supplemental table S3).14 29 Although PVs in PALB2, ATM, MLH1, MSH2 and MSH6 have been reported to be associated with EOC risk, PVs in MLH1, MHS2 and MSH6 are primarily associated with risk of specific subtypes of EOC (endometrioid and clear cell),17 and at the time of development, precise EOC age-specific risk estimates for PALB2 and ATM PV carriers were not available. Therefore, these were not considered at this stage.
jmedgenet-2021-107904supp001.pdf (2.2MB, pdf)
Epidemiological RFs
The RFs incorporated into the model include parity, use of oral contraception and MHT, endometriosis, tubal ligation, BMI and height. We assumed that the RFs were categorical and that individuals’ categories were fixed for their lifetime, although the RRs were allowed to vary with age. The RR estimates used in equation (1) and population distributions for each RF were obtained from large-scale external studies and from national surveillance data sources using a synthetic approach as previously described.30 Where possible, we used RR estimates that were adjusted for the other RFs included in the model and distributions from the UK. Details of the population distributions and RRs used in the model are given in online supplemental table S2. As in the Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA),30 in order to decrease the runtime, we combined the RFs with age-independent RRs into a single factor (specifically parity, tubal ligation, endometriosis, BMI and height).
Incorporating PRSs
We included an EOC susceptibility PRS, assumed to form part of the polygene, using the methods previously developed.11 30 The polygenic component decomposes into a measured component due to the PRS ( ) and an unmeasured component representing other familial effects ( ):
| (2) |
summarises the effects of multiple common variants and is assumed normally distributed with mean 0 and variance in the general population, with . The parameter is the proportion of the overall polygenic variance (after excluding the effects of all MGs) explained by the PRS. is normally distributed with mean 0 and variance . The approach used to calculate is described in the online supplemental material. This implementation allows the effect size of the PRS to be dynamically varied, allowing an arbitrary PRS.
Here, to illustrate the model’s risk-stratification potential, we considered the latest validated EOC PRS developed by the Ovarian Cancer Association Consortium,34 which is composed of 36 variants (online supplemental table S1) and has a log variance of 0.099, accounting for 5.0% of the overall polygenic variance in the model. This 36-variant PRS was found to perform equally well as those comprising more variants based on penalised regression or Bayesian approaches.34
Other model components
The previous version11 modelled the incidence of EOC and first female BC. To align with BOADICEA,30 the model was extended to take account of female contralateral BC and the associations of BRCA1/2 PVs with pancreatic cancer, male BC and prostate cancer (online supplemental methods).
Model validation
Study subjects
A partial model validation was carried out in a nested case–control sample of women of self-reported European ancestry participating in UKCTOCS. Based on the data available, we were able to validate the model on the basis of FH, PRS and RFs. Details of the UKCTOCS study design, blood sampling process, DNA extraction and processing, variant selection, genotyping and data processing are described in the online supplemental Methods and published elsewhere.35 Women with an FH of two or more relatives with EOC or who were known carriers of BRCA1/2 PVs were not eligible to participate in UKCTOCS. In summary, the following self-reported information was collected at recruitment and used for model validation: parity, use of oral contraception and MHT, tubal ligation, BMI and height (online supplemental table S4). As the study participants were genotyped for only 15 Single Nucleotide Polymorphisms (SNPs) known at the time to be associated with EOC risk, it was not possible to use the more recently developed PRS for model validation. Instead, as the model can accommodate an arbitrary PRS, a PRS based on the 15 available SNPs was used35 (online supplemental table S5), for which . The UKCTOCS study participants were independent of the sets used to generate this PRS.35 Study participants were not screened for PVs in BRCA1, BRCA2, RAD51C, RAD51D or BRIP1.
Pedigree construction
The UKCTOCS recruitment questionnaire collected only summary data on FH of BC and EOC. Since the risk algorithm uses explicit FH information, these data were used to reconstruct the pedigrees, which included information on incidences in the first-degree and second-degree relatives (online supplemental methods).
Statistical analysis
All UKCTOCS participants were followed up using electronic health record linkage to national cancer and death registries. For this study, they were censored at either their age at EOC, their age at other (non-EOC) first cancer diagnosis, their age at death or age 79. To assess the model performance, a weighted approach was used whereby each participant was assigned a sampling weight based on the inverse of the probability of being included in the nested case–control study, given their disease status. Since all incident cancer cases were included, cases were assigned a weight of 1. The cases were matched to two random controls (women with no EOC cancer) recruited at the same regional centre, age at randomisation and year at recruitment.
We assessed the model calibration and discrimination of the predicted 5-year risks. Women older than 74 years at entry were excluded. Cases that developed EOC beyond 5 years were treated as unaffected. For controls with a less than 5 years of follow-up, we predicted the EOC risks to the age at censoring. For all other controls and cases, we predicted 5-year risks.
To assess model calibration, we partitioned the weighted sample into quintiles of predicted risk. Within each quintile, we compared the weighted mean of predicted risk to the weighted observed incidence using the Hosmer-Lemeshow (HL) χ2 test.36 To assess RR calibration, the predicted and observed RRs were calculated relative to the corresponding means of risks over all quintiles. We also compared the expected (E) with the observed (O) EOC risk within the prediction interval by calculating the ratio of expected to observed cases (E/O). The 95% CI for the ratio was calculated assuming a Poisson distribution.37
We assessed the model discrimination between women who developed and did not develop EOC within 5 years using the area under the receiver operating characteristic curve (AUC) (online supplemental methods).
Results
Model description
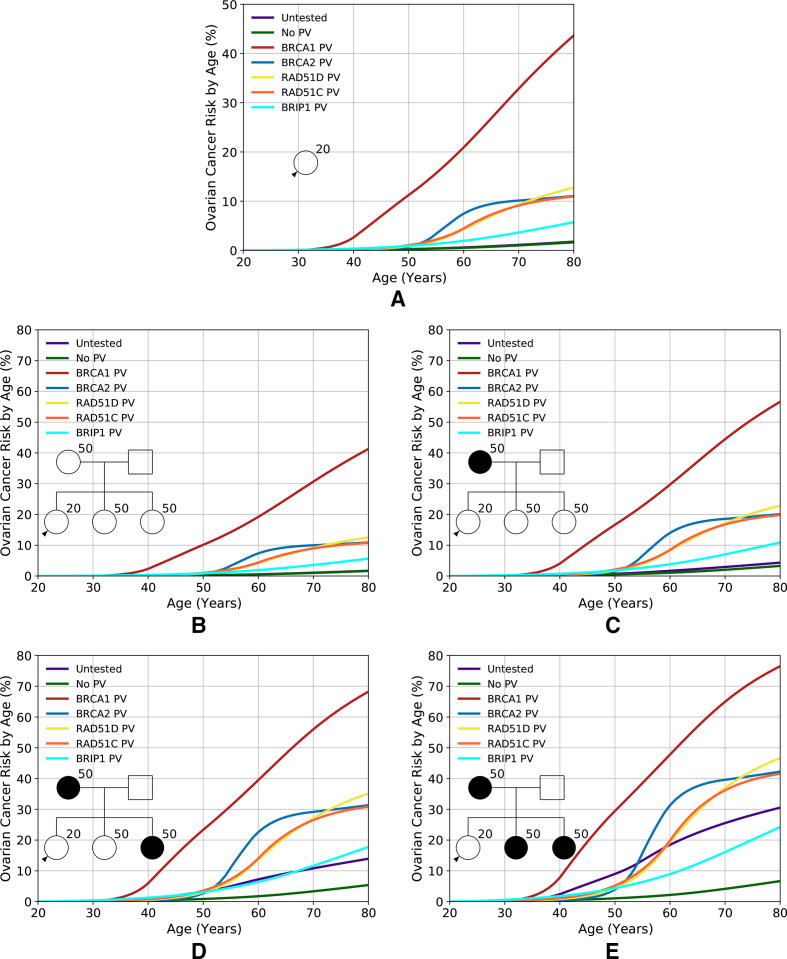
RAD51D, RAD51C and BRIP1, based on the assumed allele frequencies and RRs, account for 2.5% of the overall model polygenic variance. Figure 1 shows the predicted EOC risks for carriers of PVs in BRCA1, BRCA2, RAD51D, RAD51C and BRIP1 for various FH scenarios. With unknown FH, the risks for carriers of PVs in RAD51D, RAD51C and BRIP1 are 13%, 11% and 6%, respectively. For example, for a BRIP1 PV carrier, the risk varies from 6% for a woman without EOC FH to 18% for a woman with two affected first-degree relatives. The model can also be used to predict risks in families in which PVs are identified but where other family members test negative (online supplemental figure S1). For women with an FH of EOC, the reduction in EOC risk after negative predictive testing is greatest for BRCA1 PVs, with the risks being close to (though still somewhat greater than) population risk. This effect was most noticeable for women with a strong FH. Although a risk reduction is also seen for women whose mother carried a PV in BRCA2, RAD51D, RAD51C or BRIP1, the reduction is less marked. As expected, the predicted risks are still elevated compared with the population.
Figure 1.
Predicted lifetime (age 20–80 years) EOC risk by PV and family history. Each fgure shows the risks assuming the woman is untested, has no PVs or carries a PV in BRCA1, BRCA2, RAD51D, RAD51C or BRIP1. (A) Assuming an unknown family history. (B–E) Assuming an increasing number of affected first-degree relatives, as indicated by the pedigree diagram inserts. Predictions are based on UK EOC population incidence. EOC, epithelial tubo-ovarian cancer; PV, pathogenic variant.
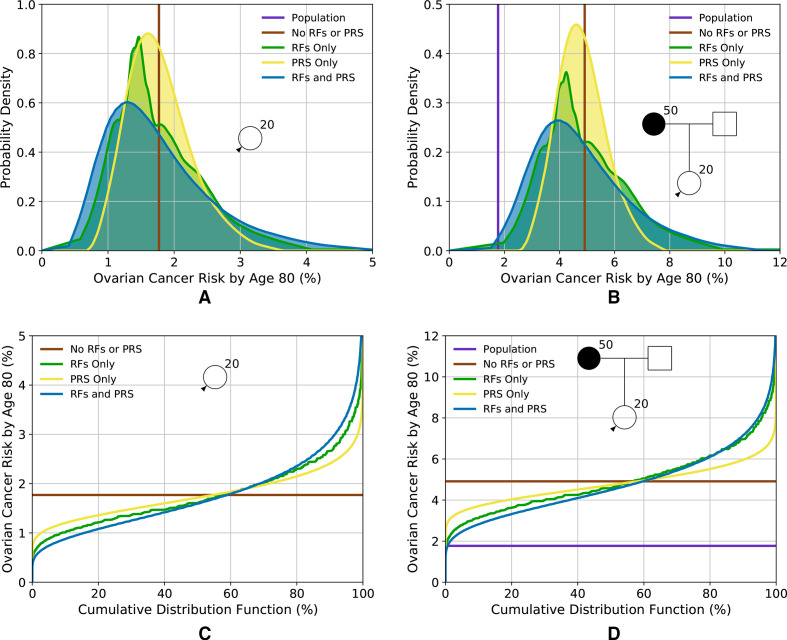
Figure 2 and online supplemental figure S2 show distributions of lifetime risk and risk by age 50, respectively, for women untested for PVs, based on RFs and PRS, for two FH scenarios: (1) unknown FH (ie, equivalent to a woman from the general population); and (2) having a mother diagnosed with EOC at age 50. Table 2 shows the corresponding proportion of women falling into different risk categories. The variation in risk is greatest when including both the RFs and PRS. When considered separately, the distribution is widest for the RFs. Using the RFs and PRS combined, predicted lifetime risks vary from 0.5% for the first percentile to 4.6% for the 99th for a woman with unknown FH and from 1.9% to 10.3% for a woman with an affected mother.
Figure 2.
Predicted lifetime (age 20–80 years) EOC risk for a woman untested for PVs based on the different predictors of risk (RFs and PRS). (A, C) Risk for a woman with an unknown family history (equivalent to the distribution of risk in the population); (B, D) risk for a woman with a mother affected at age 50. (A, B) Probability density function against absolute risk; (C, D) absolute risk against cumulative distribution. The vertical line (A) and the horizontal line (C) (labelled ‘no RFs or PRS’) are equivalent to the population risk of EOC. The ‘population’ risk is shown separately in (B, D). Predictions are based on UK EOC population incidences. EOC, epithelial tubo-ovarian cancer; PRS, Polygenic Risk Score; RF, risk factor.
Table 2.
Percentage of women falling in different risk categories by status of PV in one of the high-risk or intermediate-risk genes included in the model and family history of cancer
| PV status | Family history | Risk categories | Lifetime risk | Risk to age 50 | Ref fig. | ||||
| RF | PRS | RF and PRS | RF | PRS | RF and PRS | ||||
| Untested | NA | Population | 99.9 | 100.0 | 99.4 | 100.0 | 100.0 | 100.0 | Figure 2A, C and online supplemental figure S2A, C |
| Moderate | 0.1 | 0.0 | 0.6 | 0.0 | 0.0 | 0.0 | |||
| High | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |||
| M 50 | Population | 59.1 | 61.8 | 61.7 | 100.0 | 100.0 | 100.0 | Figure 2B, D and online supplemental figure S2B, D | |
| Moderate | 40.3 | 38.2 | 37.1 | 0.0 | 0.0 | 0.0 | |||
| High | 0.6 | 0.0 | 1.2 | 0.0 | 0.0 | 0.0 | |||
| BRCA1 | NA | Population | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | Figure 3A and online supplemental figure S3A |
| Moderate | 0.0 | 0.0 | 0.0 | 1.5 | 0.1 | 4.1 | |||
| High | 100.0 | 100.0 | 100.0 | 98.5 | 99.9 | 95.6 | |||
| M 50 | Population | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | Figure 3B and online supplemental figure S3B | |
| Moderate | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | |||
| High | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 99.8 | |||
| BRCA2 | NA | Population | 1.6 | 0.1 | 4.7 | 100.0 | 100.0 | 99.9 | Figure 3C and online supplemental figure S3C |
| Moderate | 42.8 | 37.7 | 42.3 | 0.0 | 0.0 | 0.1 | |||
| High | 55.6 | 62.2 | 52.9 | 0.0 | 0.0 | 0.0 | |||
| M 50 | Population | 0.0 | 0.0 | 0.1 | 95.9 | 99.9 | 95.3 | Figure 3D and online supplemental figure S3D | |
| Moderate | 1.9 | 0.1 | 4.7 | 4.0 | 0.1 | 4.5 | |||
| High | 98.1 | 99.9 | 95.3 | 0.0 | 0.0 | 0.2 | |||
| RAD51D | NA | Population | 0.6 | 0.0 | 2.1 | 100.0 | 100.0 | 99.8 | Figure 3E and online supplemental figure S3E |
| Moderate | 24.5 | 18.3 | 30.8 | 0.0 | 0.0 | 0.2 | |||
| High | 75.0 | 81.7 | 67.1 | 0.0 | 0.0 | 0.0 | |||
| M 50 | Population | 0.0 | 0.0 | 0.0 | 93.5 | 99.6 | 92.6 | Figure 3F and online supplemental figure S3F | |
| Moderate | 0.6 | 0.0 | 2.0 | 6.3 | 0.4 | 7.0 | |||
| High | 99.4 | 100.0 | 98.0 | 0.2 | 0.0 | 0.4 | |||
| RAD51C | NA | Population | 1.8 | 0.1 | 4.9 | 99.8 | 100.0 | 99.3 | Figure 3G and online supplemental figure S3G |
| Moderate | 44.4 | 39.3 | 43.1 | 0.2 | 0.0 | 0.7 | |||
| High | 53.7 | 60.6 | 52.0 | 0.0 | 0.0 | 0.0 | |||
| M 50 | Population | 0.0 | 0.0 | 0.1 | 85.8 | 96.2 | 85.0 | Figure 3H and online supplemental figure S3H | |
| Moderate | 2.0 | 0.1 | 5.0 | 13.6 | 3.8 | 13.7 | |||
| High | 98.0 | 99.9 | 95.0 | 0.6 | 0.0 | 1.3 | |||
| BRIP1 | NA | Population | 43.6 | 34.0 | 45.7 | 100.0 | 100.0 | 99.7 | Figure 3I and online supplemental figure 3I |
| Moderate | 52.3 | 65.0 | 47.4 | 0.0 | 0.0 | 0.3 | |||
| High | 4.1 | 1.0 | 6.9 | 0.0 | 0.0 | 0.0 | |||
| M 50 | Population | 2.1 | 0.1 | 4.8 | 93.0 | 99.3 | 91.4 | Figure 3J and online supplemental figure 3J | |
| Moderate | 43.5 | 38.9 | 44.5 | 6.8 | 0.7 | 8.1 | |||
| High | 54.5 | 61.1 | 50.7 | 0.3 | 0.0 | 0.5 | |||
The ‘population’ risk category is defined as lifetime risk of <5% and risk to age 50 of <3%. ‘Moderate’ risk category is defined as a lifetime risk of 5% or greater but less than 10% and a risk to age 50 of 3% or greater but less than 5%. ‘High’ risk category is defined as a lifetime risk of 10% or greater and a risk to age 50 of 5% or greater. The population lifetime risk is 1.8%, and the population risk to age 50 is 0.27%
EOC, epithelial tubo-ovarian cancer; M 50, mother diagnosed with EOC at age 50; NA, unknown family history; PV, pathogenic variant.
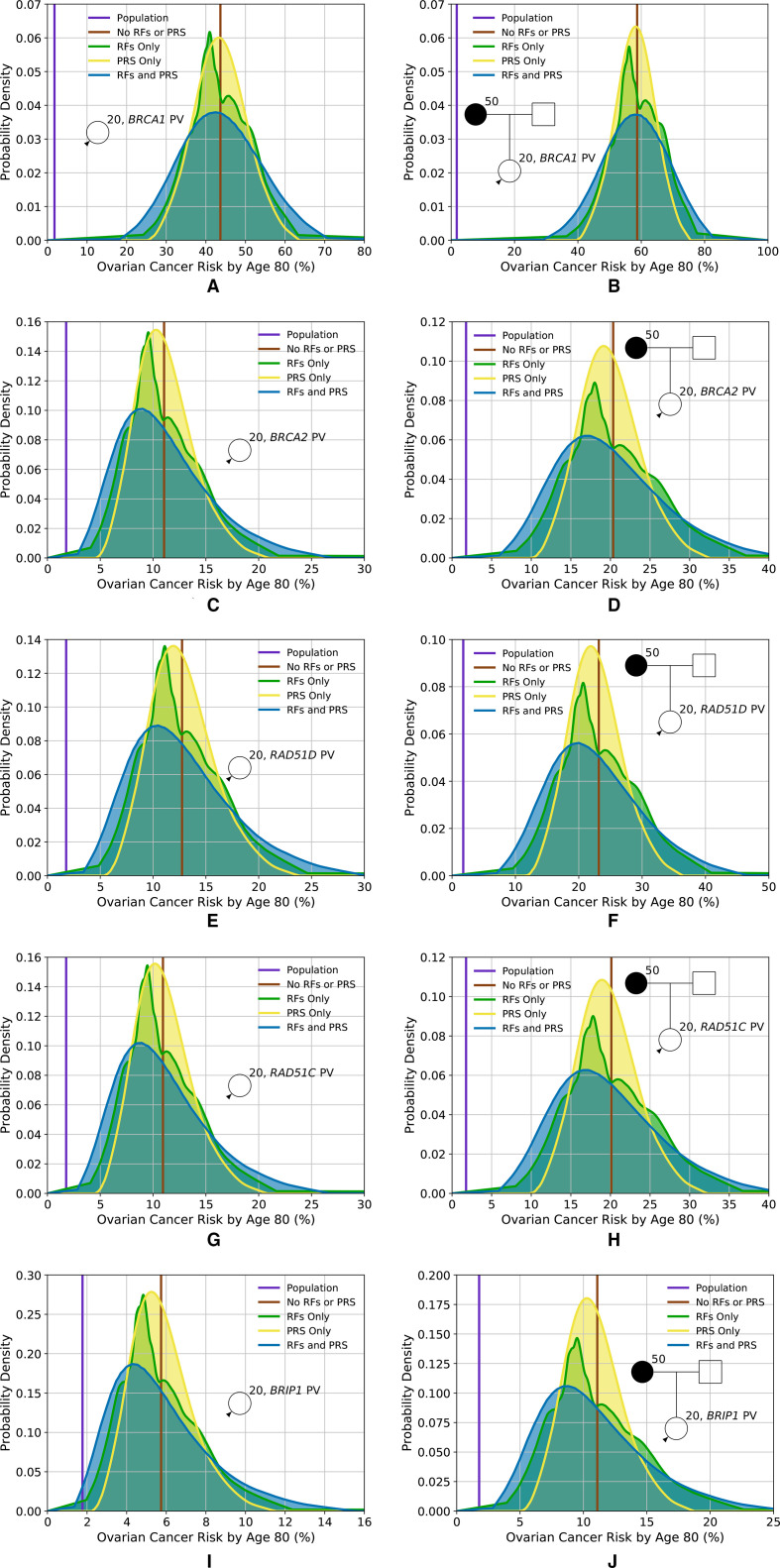
Figure 3 shows the predicted lifetime EOC risk for carriers of PVs in BRCA1, BRCA2, RAD51D, RAD51C and BRIP1 based on RFs and PRS for two FH scenarios. Taking a RAD51D PV carrier, for example, based on PV testing and FH alone, the predicted risks are 13% when FH is unknown and 23% when having a mother diagnosed with EOC at age 50. When RFs and the PRS are considered jointly, risks vary from 4% for those at the 1st percentile to 28% for the 99th with unknown FH and from 9% to 43% with an affected mother. Table 1 shows the proportion of women with PVs falling into different risk categories. Based on the combined distribution, 33% of RAD51D PV carriers in the population are expected to have a lifetime EOC risk of less than 10%. Similarly, the distributions of risk for BRIP1 PV carriers are shown in figure 3I, J and in table 1. Based on the combined RFs and PRS distributions, 46% of BRIP1 PV carriers in the population are expected to have lifetime risks of less than 5%; 47% to have risks between 5% and 10%, and 7% to have risks of 10% or greater. A BRIP1 PV carrier with an affected mother, on the basis of FH alone, has a lifetime risk of 11%. However, when the RFs and PRS are considered, 50% of those would be reclassified as having lifetime risks of less than 10%.
Figure 3.
Predicted lifetime EOC risk for a woman who has a PV in one of the high-risk or intermediate-risk genes included in the model, based on the different predictors of risk (RFs and PRS), for two family histories. (A, B) Lifetime risk for a carrier of a PV in BRCA1; (C, D) lifetime risk for a carrier of a PV in BRCA2; (E, F) lifetime risk for a carrier of a PV in RAD51D; (G, H) lifetime risk for a carrier of a PV in RAD51C; (I, J) lifetime risk for a carrier of a PV in BRIP1. (A, C, E, G, I) Risks for an unknown family history; (B, D, F, H, J) risks for a woman whose mother is diagnosed with EOC at age 50. Predictions based on UK ovarian cancer incidences. EOC, epithelial tubo-ovarian cancer; PRS, Polygenic Risk Score; PV, pathogenic variant; RF, risk factor.
Online supplemental figures S4 and S5 show the probability trees describing the reclassification of women as more information (RFs, PRS and testing for PVs in the MGs) is added to the model for a woman with unknown FH and a woman with a mother diagnosed at age 50, respectively, based on the predicted lifetime risks. Online supplemental figures S4A and S5A show the reclassification resulting from adding RFs, MG and PRS sequentially, while online supplemental figures S4B and S5B assume the order RFs, PRS and then MG. Assuming the three risk categories for lifetime risks are <5% and ≥5% but <10% and≥10%, there is significant reclassification as more information is added.
Model validation
After censoring, 1961 participants with 374 incident cases and 1587 controls met the 5-year risk prediction eligibility criteria. Online supplemental table S5 summarises their characteristics at baseline.
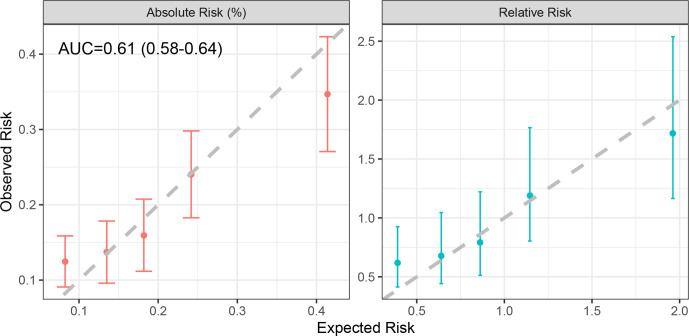
The model considering FH, the 15-variant PRS and a subset of the RFs (but not including testing for PVs in the MGs) demonstrated good calibration in both absolute and relative predicted risk (figure 4). Over the 5-year period, the model predicted 391 EOCs, close to the 374 observed (E/O=1.05, 95% CI: 0.94 to 1.16). The model was well calibrated across the quintiles of predicted risk (HL p=0.08), although there was a suggestion of an underprediction of risk in the lowest quintile (absolute risk E/O=0.66, 95% CI: 0.52 to 0.91; RR E/O=0.63, 95% CI: 0.42 to 0.95). The AUC for assessing discrimination of these model components was 0.61 (95% CI: 0.58 to 0.64).
Figure 4.
Calibration of the absolute and relative predicted 5-year EOC risks, showing the observed and expected risks by quintile. The bars show the 95% CIs for the observed risks. Relative risks were calculated relative to the overall mean of observed and predicted risks. AUC, area under the receiver operating characteristic curve.
When looking at individual factors, FH predicted the widest 5 year risk variability (SD=0.0013; range: 0.04% to 4.0%), followed by RFs (SD=0.0010; range: 0.02% to 0.7%) and PRS (SD=0.0009; range: 0.05% to 1.0%, online supplemental figure S6). As expected, their sequential inclusion increased the variability (SD=0.0018; online supplemental figure S6).
Discussion
The EOC risk prediction model presented here combines the effects of FH, the explicit effects of rare moderate-risk to high-risk PVs in five established EOC susceptibility genes, a 36-variant PRS and other clinical and epidemiological factors (table 1). The model provides a consistent approach for estimating EOC risk on the basis of all known factors and allows for prevention approaches to be targeted at those at highest risk.
The results demonstrate that in the general population (unknown FH), the existing PRS and RF alone identify 0.6% of women who have a lifetime risk of >5% (table 2). On the other hand, for women with FH, 37.1% of women would have a predicted risk between 5% and 10% and 1.2% would have an EOC risk of ≥10% (table 2). The results show that the RFs provide a somewhat greater level of risk stratification than the 36-variant PRS. However, discrimination is greater when both are considered jointly. These results were in line with the observed risk distributions in the validation dataset, but direct comparisons were not possible due to the different variants included in the PRSs and limited RFs in the validation study. The results also show that significant levels of risk recategorisation can occur for carriers of PVs in moderate-risk or high-risk susceptibility genes.
The comprehensive risk model is based on a synthetic approach previously used for BC30 and makes several assumptions. In particular, we assumed that the risks associated with known RFs and the PRS combine multiplicatively. We have not assessed this assumption in the present study; however, published studies found no evidence of deviations from the multiplicative model for the combined effect of the RFs and the PRS,28 suggesting that this assumption is reasonable. The model assumes that the RFs are also independent of the residual polygenic component that captures the effect of FH. However, for the RFs included, we used estimates from published studies that have adjusted for the other known EOC RFs. The observation that the model was calibrated on the RR scale in the UKCTOCS validation study also suggests that these assumptions are broadly valid.
Similarly, the model assumes that the relative effect-sizes of RFs and the PRS are similar in women carrying PVs in BRCA1, BRCA2, RAD51C, RAD51D and BRIP1 to those without PVs in these genes. Evidence from studies of BRCA1 and BRCA2 PV carriers suggests that this assumption is plausible: PRSs for EOC have been shown to be associated with similar RRs in the general population and in BRCA1 and BRCA2 PV carriers.34 38 39 The current evidence also suggests that known RFs have similar effect sizes in BRCA1 and BRCA2 PV carriers as in non-carriers.40 41 No studies have so far assessed the joint effects of RAD51C, RAD51D and BRIP1 PVs with the PRS, but the observation that FH modifies EOC risk for RAD51C/D PV carriers29 suggests that similar arguments are likely to apply. Large prospective studies are required to address these questions in more detail. We were not able to validate these assumptions explicitly in UKCTOCS because gene-panel testing data were not available.
Other RFs for EOC that have been reported in the literature include breast feeding42 and age at menarche and menopause.25 However, the evidence for these RFs is still limited. Our model is flexible enough to allow for additional RFs to be incorporated in the future.
We validated the 5-year predicted risks on the basis of FH, RFs and PRS available in an independent dataset from a prospective trial.2 A key strength was that EOC was a primary outcome in UKCTOCS. All cases were reviewed and confirmed by an independent outcome review committee.2 The results indicated that absolute and RRs were well calibrated overall and in the top quintiles of predicted risk. However, there was some underprediction of EOC in the bottom quintile. This could be due to differences in the RF distributions in those who volunteer to participate in research (self-selected more healthy individuals43) compared with the general population or due to random variations in the effects of the RFs in UKCTOCS compared with other studies. Alternatively, the multiplicative assumption may break down in the lowest-risk category. Further, large prospective cohorts will be required to determine whether the underprediction in the lowest risk category reflects a systematic miscalibration of the model or is due to chance. Although the AUC based on model components in this validation study was modest; it is not surprising given that only a subset of the model predictors were used, and UKCTOCS recruited primarily low-risk women. Inclusion of the optimal PRS,34 all RFs and information on PVs in the five genes that account for a large fraction of the EOC FRR are expected to lead to an increase in AUC.
The current validation study has some limitations. The underlying model accounts for FH information on both affected and unaffected family members, but the UKCTOCS recruitment questionnaire did not include information on unaffected family members. Family sizes and ages for unobserved family members were imputed using demographic data. In addition, since information on whether the affected family members were from the paternal or maternal side was absent, we assumed all the affected family members were from the same (maternal) side. This may result in inaccuracies in risk predictions. A further limitation is that UKCTOCS was undertaken to assess screening of low-risk women and therefore is not necessarily representative of a true population cohort, as women with a FH of two or more relatives with EOC or who were known carriers of BRCA1/2 PVs were not eligible to participate in the randomised controlled trial. Data were not available on the rare moderate-risk and high-risk PVs, and we were only able to assess a PRS with 15 variants, rather than the more informative 36-variant PRS. Therefore, it has not been possible to validate the full model presented here. Future analyses in other cohorts will be required to further validate the full model.
In summary, we have presented a methodological framework for a comprehensive EOC risk prediction model that considers the currently known genetic and epidemiological RFs and explicit FH. The model allows users to obtain consistent, individualised EOC risks. It can also be used to identify target populations for studies to assess novel prevention strategies (such as salpingectomy) or early detection approaches by identifying those at higher risk of developing the disease for enrolment into such studies. Future independent studies should aim to validate the full model, including the full PRS and rare PVs in diverse settings. The model is available via the CanRisk Tool (www.canrisk.org), a user-friendly web tool that allows users to obtain future risks of developing EOC.
Acknowledgments
The authors are particularly grateful to those throughout the UK who are participating in the trial and to the centre leads and the entire medical, nursing and administrative staff who work on the UK Collaborative Trial of Ovarian Cancer Screening.
Footnotes
Twitter: @ProfManchanda
Contributors: Conceptualisation: ACA, PPDP and DFE. Methodology: AL, XY, ACA, DFE, PPDP and JT. Software: AL, XY, APC, TC and SA. Investigation: AL, XY, ACA, PPDP, DFE, SAG, SJR, FG, RM, FWM and MT. Data curation: AGM, AR and GL. Formal analysis: AL, XY, JT and NM. Funding acquisition: ACA, IJ, UM and RM. Resources: PPDP, AGM, AR, JT, SAG, SJR, IJ, UM and RM. Supervision: ACA. Visualisation: AL and XY. Writing, original draft: AL, XY and ACA. Writing, review and editing: all authors.
Funding: This work has been supported by grants from Cancer Research UK (C12292/A20861 and PPRPGM-Nov20\100002). The analysis is part of PROMISE, which was funded through Cancer Research UK PRC Programme Grant A12677 and by The Eve Appeal. University College London investigators received support from the National Institute for Health Research University College London Hospitals Biomedical Research Centre and from MRC core funding (MR_UU_12023). KCTOCS was core funded by the Medical Research Council (G9901012 and G0801228), Cancer Research UK (C1479/A2884) and the Department of Health with additional support from the Eve Appeal. The work received support through the PERSPECTIVE I&I project which is funded by the Government of Canada through Genome Canada (#13529) and the Canadian Institutes of Health Research (#155865), the Ministère de l’Économie et de l'Innovation du Québec through Genome Québec, the Quebec Breast Cancer Foundation, the CHU de Quebec Foundation and the Ontario Research Fund. FMW is co-Director of the multi-institutional CanTest Collaborative, which is funded by Cancer Research UK (C8640/A23385). MT was funded by the European Union Seventh Framework Programme (2007–2013)/European Research Council (310018).
Competing interests: DFE, ACA, APC, AL and TC are listed as creators of the BOADICEA model, which has been licensed to Cambridge Enterprise for commercialisation. UM has shares in Abcodia awarded to her by UCL.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
The model is freely available online (www.canrisk.org). For access to UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) dataset, which is subject to General Data Protection Regulations rules, please contact the UKCTOCS Biobank coordinator (s.apostolidou@ucl.ac.uk). The data access process is outlined online (http://uklwc.mrcctu.ucl.ac.uk/access-process/).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by local ethical review committees. UK Collaborative Trial of Ovarian Cancer Screening was approved by the UK North West Multicentre Research Ethics Committees (North West MREC 00/8/34) on 21 June 2000 with site-specific approval from the local regional ethics committees and the Caldicott guardians (data controllers) of the primary care trusts. The SNP protocol was approved by NRES Committee North West - Liverpool Central (14/NW1026) in June 2014.
References
- 1. Cancer Research UK . Ovarian Cancer Statistics [Ovarian cancer statistics for the UK]. Available: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer
- 2. Jacobs IJ, Menon U, Ryan A, Gentry-Maharaj A, Burnell M, Kalsi JK, Amso NN, Apostolidou S, Benjamin E, Cruickshank D, Crump DN, Davies SK, Dawnay A, Dobbs S, Fletcher G, Ford J, Godfrey K, Gunu R, Habib M, Hallett R, Herod J, Jenkins H, Karpinskyj C, Leeson S, Lewis SJ, Liston WR, Lopes A, Mould T, Murdoch J, Oram D, Rabideau DJ, Reynolds K, Scott I, Seif MW, Sharma A, Singh N, Taylor J, Warburton F, Widschwendter M, Williamson K, Woolas R, Fallowfield L, McGuire AJ, Campbell S, Parmar M, Skates SJ. Ovarian cancer screening and mortality in the UK Collaborative trial of ovarian cancer screening (UKCTOCS): a randomised controlled trial. Lancet 2016;387:945–56. 10.1016/S0140-6736(15)01224-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosenthal AN, Fraser LSM, Philpott S, Manchanda R, Burnell M, Badman P, Hadwin R, Rizzuto I, Benjamin E, Singh N, Evans DG, Eccles DM, Ryan A, Liston R, Dawnay A, Ford J, Gunu R, Mackay J, Skates SJ, Menon U, Jacobs IJ, United Kingdom Familial Ovarian Cancer Screening Study collaborators . Evidence of stage shift in women diagnosed with ovarian cancer during phase II of the United Kingdom familial ovarian cancer screening study. J Clin Oncol 2017;35:1411–20. 10.1200/JCO.2016.69.9330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ludwig KK, Neuner J, Butler A, Geurts JL, Kong AL. Risk reduction and survival benefit of prophylactic surgery in BRCA mutation carriers, a systematic review. Am J Surg 2016;212:660–9. 10.1016/j.amjsurg.2016.06.010 [DOI] [PubMed] [Google Scholar]
- 5. Manchanda R, Legood R, Antoniou AC, Gordeev VS, Menon U. Specifying the ovarian cancer risk threshold of 'premenopausal risk-reducing salpingo-oophorectomy' for ovarian cancer prevention: a cost-effectiveness analysis. J Med Genet 2016;53:591–9. 10.1136/jmedgenet-2016-103800 [DOI] [PubMed] [Google Scholar]
- 6. Manchanda R, Legood R, Pearce L, Menon U. Defining the risk threshold for risk reducing salpingo-oophorectomy for ovarian cancer prevention in low risk postmenopausal women. Gynecol Oncol 2015;139:487–94. 10.1016/j.ygyno.2015.10.001 [DOI] [PubMed] [Google Scholar]
- 7. Parker WH, Feskanich D, Broder MS, Chang E, Shoupe D, Farquhar CM, Berek JS, Manson JE. Long-term mortality associated with oophorectomy compared with ovarian conservation in the nurses' health study. Obstet Gynecol 2013;121:709–16. 10.1097/AOG.0b013e3182864350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rocca WA, Gazzuola-Rocca L, Smith CY, Grossardt BR, Faubion SS, Shuster LT, Kirkland JL, Stewart EA, Miller VM. Accelerated accumulation of multimorbidity after bilateral oophorectomy: a population-based cohort study. Mayo Clin Proc 2016;91:1577–89. 10.1016/j.mayocp.2016.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parker WH, Jacoby V, Shoupe D, Rocca W. Effect of bilateral oophorectomy on women's long-term health. Womens Health 2009;5:565–76. 10.2217/WHE.09.42 [DOI] [PubMed] [Google Scholar]
- 10. Gaba F, Manchanda R. Systematic review of acceptability, cardiovascular, neurological, bone health and HRT outcomes following risk reducing surgery in BRCA carriers. Best Pract Res Clin Obstet Gynaecol 2020;65:46–65. 10.1016/j.bpobgyn.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 11. Jervis S, Song H, Lee A, Dicks E, Harrington P, Baynes C, Manchanda R, Easton DF, Jacobs I, Pharoah PPD, Antoniou AC. A risk prediction algorithm for ovarian cancer incorporating BRCA1, BRCA2, common alleles and other familial effects. J Med Genet 2015;52:465–75. 10.1136/jmedgenet-2015-103077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Loveday C, Turnbull C, Ramsay E, Hughes D, Ruark E, Frankum JR, Bowden G, Kalmyrzaev B, Warren-Perry M, Snape K, Adlard JW, Barwell J, Berg J, Brady AF, Brewer C, Brice G, Chapman C, Cook J, Davidson R, Donaldson A, Douglas F, Greenhalgh L, Henderson A, Izatt L, Kumar A, Lalloo F, Miedzybrodzka Z, Morrison PJ, Paterson J, Porteous M, Rogers MT, Shanley S, Walker L, Eccles D, Evans DG, Renwick A, Seal S, Lord CJ, Ashworth A, Reis-Filho JS, Antoniou AC, Rahman N, Breast Cancer Susceptibility Collaboration (UK) . Germline mutations in RAD51D confer susceptibility to ovarian cancer. Nat Genet 2011;43:879–82. 10.1038/ng.893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Loveday C, Turnbull C, Ruark E, Xicola RMM, Ramsay E, Hughes D, Warren-Perry M, Snape K, Eccles D, Evans DG, Gore M, Renwick A, Seal S, Antoniou AC, Rahman N, Breast Cancer Susceptibility Collaboration (UK) . Germline RAD51C mutations confer susceptibility to ovarian cancer. Nat Genet 2012;44:475–6. author reply 6. 10.1038/ng.2224 [DOI] [PubMed] [Google Scholar]
- 14. Ramus SJ, Song H, Dicks E, Tyrer JP, Rosenthal AN, Intermaggio MP, Fraser L, Gentry-Maharaj A, Hayward J, Philpott S, Anderson C, Edlund CK, Conti D, Harrington P, Barrowdale D, Bowtell DD, Alsop K, Mitchell G, Cicek MS, Cunningham JM, Fridley BL, Alsop J, Jimenez-Linan M, Poblete S, Lele S, Sucheston-Campbell L, Moysich KB, Sieh W, McGuire V, Lester J, Bogdanova N, Dürst M, Hillemanns P, Odunsi K, Whittemore AS, Karlan BY, Dörk T, Goode EL, Menon U, Jacobs IJ, Antoniou AC, Pharoah PDP, Gayther SA, AOCS Study Group, Ovarian Cancer Association Consortium . Germline mutations in the BRIP1, BARD1, PALB2, and NBN genes in women with ovarian cancer. J Natl Cancer Inst 2015;107. 10.1093/jnci/djv214. [Epub ahead of print: 27 08 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yang X, Leslie G, Doroszuk A, Schneider S, Allen J, Decker B, Dunning AM, Redman J, Scarth J, Plaskocinska I, Luccarini C, Shah M, Pooley K, Dorling L, Lee A, Adank MA, Adlard J, Aittomäki K, Andrulis IL, Ang P, Barwell J, Bernstein JL, Bobolis K, Borg Åke, Blomqvist C, Claes KBM, Concannon P, Cuggia A, Culver JO, Damiola F, de Pauw A, Diez O, Dolinsky JS, Domchek SM, Engel C, Evans DG, Fostira F, Garber J, Golmard L, Goode EL, Gruber SB, Hahnen E, Hake C, Heikkinen T, Hurley JE, Janavicius R, Kleibl Z, Kleiblova P, Konstantopoulou I, Kvist A, Laduca H, Lee ASG, Lesueur F, Maher ER, Mannermaa A, Manoukian S, McFarland R, McKinnon W, Meindl A, Metcalfe K, Mohd Taib NA, Moilanen J, Nathanson KL, Neuhausen S, Ng PS, Nguyen-Dumont T, Nielsen SM, Obermair F, Offit K, Olopade OI, Ottini L, Penkert J, Pylkäs K, Radice P, Ramus SJ, Rudaitis V, Side L, Silva-Smith R, Silvestri V, Skytte A-B, Slavin T, Soukupova J, Tondini C, Trainer AH, Unzeitig G, Usha L, van Overeem Hansen T, Whitworth J, Wood M, Yip CH, Yoon S-Y, Yussuf A, Zogopoulos G, Goldgar D, Hopper JL, Chenevix-Trench G, Pharoah P, George SHL, Balmaña J, Houdayer C, James P, El-Haffaf Z, Ehrencrona H, Janatova M, Peterlongo P, Nevanlinna H, Schmutzler R, Teo S-H, Robson M, Pal T, Couch F, Weitzel JN, Elliott A, Southey M, Winqvist R, Easton DF, Foulkes WD, Antoniou AC, Tischkowitz M. Cancer Risks Associated With Germline PALB2 Pathogenic Variants: An International Study of 524 Families. J Clin Oncol 2020;38:674–85. 10.1200/JCO.19.01907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lilyquist J, LaDuca H, Polley E, Davis BT, Shimelis H, Hu C, Hart SN, Dolinsky JS, Couch FJ, Goldgar DE. Frequency of mutations in a large series of clinically ascertained ovarian cancer cases tested on multi-gene panels compared to reference controls. Gynecol Oncol 2017;147:375–80. 10.1016/j.ygyno.2017.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pal T, Akbari MR, Sun P, Lee J-H, Fulp J, Thompson Z, Coppola D, Nicosia S, Sellers TA, McLaughlin J, Risch HA, Rosen B, Shaw P, Schildkraut J, Narod SA. Frequency of mutations in mismatch repair genes in a population-based study of women with ovarian cancer. Br J Cancer 2012;107:1783–90. 10.1038/bjc.2012.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dominguez-Valentin M, Sampson JR, Seppälä TT, Ten Broeke SW, Plazzer J-P, Nakken S, Engel C, Aretz S, Jenkins MA, Sunde L, Bernstein I, Capella G, Balaguer F, Thomas H, Evans DG, Burn J, Greenblatt M, Hovig E, de Vos Tot Nederveen Cappel WH, Sijmons RH, Bertario L, Tibiletti MG, Cavestro GM, Lindblom A, Della Valle A, Lopez-Köstner F, Gluck N, Katz LH, Heinimann K, Vaccaro CA, Büttner R, Görgens H, Holinski-Feder E, Morak M, Holzapfel S, Hüneburg R, Knebel Doeberitz Mvon, Loeffler M, Rahner N, Schackert HK, Steinke-Lange V, Schmiegel W, Vangala D, Pylvänäinen K, Renkonen-Sinisalo L, Hopper JL, Win AK, Haile RW, Lindor NM, Gallinger S, Le Marchand L, Newcomb PA, Figueiredo JC, Thibodeau SN, Wadt K, Therkildsen C, Okkels H, Ketabi Z, Moreira L, Sánchez A, Serra-Burriel M, Pineda M, Navarro M, Blanco I, Green K, Lalloo F, Crosbie EJ, Hill J, Denton OG, Frayling IM, Rødland EA, Vasen H, Mints M, Neffa F, Esperon P, Alvarez K, Kariv R, Rosner G, Pinero TA, Gonzalez ML, Kalfayan P, Tjandra D, Winship IM, Macrae F, Möslein G, Mecklin J-P, Nielsen M, Møller P. Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the prospective Lynch syndrome database. Genet Med 2020;22:15–25. 10.1038/s41436-019-0596-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kuchenbaecker KB, Ramus SJ, Tyrer J, Lee A, Shen HC, Beesley J, Lawrenson K, McGuffog L, Healey S, Lee JM, Spindler TJ, Lin YG, Pejovic T, Bean Y, Li Q, Coetzee S, Hazelett D, Miron A, Southey M, Terry MB, Goldgar DE, Buys SS, Janavicius R, Dorfling CM, van Rensburg EJ, Neuhausen SL, Ding YC, Hansen TVO, Jønson L, Gerdes A-M, Ejlertsen B, Barrowdale D, Dennis J, Benitez J, Osorio A, Garcia MJ, Komenaka I, Weitzel JN, Ganschow P, Peterlongo P, Bernard L, Viel A, Bonanni B, Peissel B, Manoukian S, Radice P, Papi L, Ottini L, Fostira F, Konstantopoulou I, Garber J, Frost D, Perkins J, Platte R, Ellis S, Godwin AK, Schmutzler RK, Meindl A, Engel C, Sutter C, Sinilnikova OM, Damiola F, Mazoyer S, Stoppa-Lyonnet D, Claes K, De Leeneer K, Kirk J, Rodriguez GC, Piedmonte M, O'Malley DM, de la Hoya M, Caldes T, Aittomäki K, Nevanlinna H, Collée JM, Rookus MA, Oosterwijk JC, Tihomirova L, Tung N, Hamann U, Isaccs C, Tischkowitz M, Imyanitov EN, Caligo MA, Campbell IG, Hogervorst FBL, Olah E, Diez O, Blanco I, Brunet J, Lazaro C, Pujana MA, Jakubowska A, Gronwald J, Lubinski J, Sukiennicki G, Barkardottir RB, Plante M, Simard J, Soucy P, Montagna M, Tognazzo S, Teixeira MR, Pankratz VS, Wang X, Lindor N, Szabo CI, Kauff N, Vijai J, Aghajanian CA, Pfeiler G, Berger A, Singer CF, Tea M-K, Phelan CM, Greene MH, Mai PL, Rennert G, Mulligan AM, Tchatchou S, Andrulis IL, Glendon G, Toland AE, Jensen UB, Kruse TA, Thomassen M, Bojesen A, Zidan J, Friedman E, Laitman Y, Soller M, Liljegren A, Arver B, Einbeigi Z, Stenmark-Askmalm M, Olopade OI, Nussbaum RL, Rebbeck TR, Nathanson KL, Domchek SM, Lu KH, Karlan BY, Walsh C, Lester J, Hein A, Ekici AB, Beckmann MW, Fasching PA, Lambrechts D, Van Nieuwenhuysen E, Vergote I, Lambrechts S, Dicks E, Doherty JA, Wicklund KG, Rossing MA, Rudolph A, Chang-Claude J, Wang-Gohrke S, Eilber U, Moysich KB, Odunsi K, Sucheston L, Lele S, Wilkens LR, Goodman MT, Thompson PJ, Shvetsov YB, Runnebaum IB, Dürst M, Hillemanns P, Dörk T, Antonenkova N, Bogdanova N, Leminen A, Pelttari LM, Butzow R, Modugno F, Kelley JL, Edwards RP, Ness RB, du Bois A, Heitz F, Schwaab I, Harter P, Matsuo K, Hosono S, Orsulic S, Jensen A, Kjaer SK, Hogdall E, Hasmad HN, Azmi MAN, Teo S-H, Woo Y-L, Fridley BL, Goode EL, Cunningham JM, Vierkant RA, Bruinsma F, Giles GG, Liang D, Hildebrandt MAT, Wu X, Levine DA, Bisogna M, Berchuck A, Iversen ES, Schildkraut JM, Concannon P, Weber RP, Cramer DW, Terry KL, Poole EM, Tworoger SS, Bandera EV, Orlow I, Olson SH, Krakstad C, Salvesen HB, Tangen IL, Bjorge L, van Altena AM, Aben KKH, Kiemeney LA, Massuger LFAG, Kellar M, Brooks-Wilson A, Kelemen LE, Cook LS, Le ND, Cybulski C, Yang H, Lissowska J, Brinton LA, Wentzensen N, Hogdall C, Lundvall L, Nedergaard L, Baker H, Song H, Eccles D, McNeish I, Paul J, Carty K, Siddiqui N, Glasspool R, Whittemore AS, Rothstein JH, McGuire V, Sieh W, Ji B-T, Zheng W, Shu X-O, Gao Y-T, Rosen B, Risch HA, McLaughlin JR, Narod SA, Monteiro AN, Chen A, Lin H-Y, Permuth-Wey J, Sellers TA, Tsai Y-Y, Chen Z, Ziogas A, Anton-Culver H, Gentry-Maharaj A, Menon U, Harrington P, Lee AW, Wu AH, Pearce CL, Coetzee G, Pike MC, Dansonka-Mieszkowska A, Timorek A, Rzepecka IK, Kupryjanczyk J, Freedman M, Noushmehr H, Easton DF, Offit K, Couch FJ, Gayther S, Pharoah PP, Antoniou AC, Chenevix-Trench G, KH L, ND L, B-T J, AH W, Easton DF, Offit K, Couch FJ, Gayther S, Pharoah PP, Antoniou AC, Chenevix-Trench G, tCoIoMoB B, EMBRACE, GEMO Study Collaborators, Breast Cancer Family Registry, HEBON, KConFab Investigators, Australian Cancer Study (Ovarian Cancer Investigators), Australian Ovarian Cancer Study Group, Consortium of Investigators of Modifiers of BRCA1 and BRCA2 . Identification of six new susceptibility loci for invasive epithelial ovarian cancer. Nat Genet 2015;47:164–71. 10.1038/ng.3185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Phelan CM, Kuchenbaecker KB, Tyrer JP, Kar SP, Lawrenson K, Winham SJ, Dennis J, Pirie A, Riggan MJ, Chornokur G, Earp MA, Lyra PC, Lee JM, Coetzee S, Beesley J, McGuffog L, Soucy P, Dicks E, Lee A, Barrowdale D, Lecarpentier J, Leslie G, Aalfs CM, Aben KKH, Adams M, Adlard J, Andrulis IL, Anton-Culver H, Antonenkova N, Aravantinos G, Arnold N, Arun BK, Arver B, Azzollini J, Balmaña J, Banerjee SN, Barjhoux L, Barkardottir RB, Bean Y, Beckmann MW, Beeghly-Fadiel A, Benitez J, Bermisheva M, Bernardini MQ, Birrer MJ, Bjorge L, Black A, Blankstein K, Blok MJ, Bodelon C, Bogdanova N, Bojesen A, Bonanni B, Borg Åke, Bradbury AR, Brenton JD, Brewer C, Brinton L, Broberg P, Brooks-Wilson A, Bruinsma F, Brunet J, Buecher B, Butzow R, Buys SS, Caldes T, Caligo MA, Campbell I, Cannioto R, Carney ME, Cescon T, Chan SB, Chang-Claude J, Chanock S, Chen XQ, Chiew Y-E, Chiquette J, Chung WK, Claes KBM, Conner T, Cook LS, Cook J, Cramer DW, Cunningham JM, D'Aloisio AA, Daly MB, Damiola F, Damirovna SD, Dansonka-Mieszkowska A, Dao F, Davidson R, DeFazio A, Delnatte C, Doheny KF, Diez O, Ding YC, Doherty JA, Domchek SM, Dorfling CM, Dörk T, Dossus L, Duran M, Dürst M, Dworniczak B, Eccles D, Edwards T, Eeles R, Eilber U, Ejlertsen B, Ekici AB, Ellis S, Elvira M, Eng KH, Engel C, Evans DG, Fasching PA, Ferguson S, Ferrer SF, Flanagan JM, Fogarty ZC, Fortner RT, Fostira F, Foulkes WD, Fountzilas G, Fridley BL, Friebel TM, Friedman E, Frost D, Ganz PA, Garber J, García MJ, Garcia-Barberan V, Gehrig A, Gentry-Maharaj A, Gerdes A-M, Giles GG, Glasspool R, Glendon G, Godwin AK, Goldgar DE, Goranova T, Gore M, Greene MH, Gronwald J, Gruber S, Hahnen E, Haiman CA, Håkansson N, Hamann U, Hansen TVO, Harrington PA, Harris HR, Hauke J, Hein A, Henderson A, Hildebrandt MAT, Hillemanns P, Hodgson S, Høgdall CK, Høgdall E, Hogervorst FBL, Holland H, Hooning MJ, Hosking K, Huang R-Y, Hulick PJ, Hung J, Hunter DJ, Huntsman DG, Huzarski T, Imyanitov EN, Isaacs C, Iversen ES, Izatt L, Izquierdo A, Jakubowska A, James P, Janavicius R, Jernetz M, Jensen A, Jensen UB, John EM, Johnatty S, Jones ME, Kannisto P, Karlan BY, Karnezis A, Kast K, Kennedy CJ, Khusnutdinova E, Kiemeney LA, Kiiski JI, Kim S-W, Kjaer SK, Köbel M, Kopperud RK, Kruse TA, Kupryjanczyk J, Kwong A, Laitman Y, Lambrechts D, Larrañaga N, Larson MC, Lazaro C, Le ND, Le Marchand L, Lee JW, Lele SB, Leminen A, Leroux D, Lester J, Lesueur F, Levine DA, Liang D, Liebrich C, Lilyquist J, Lipworth L, Lissowska J, Lu KH, Lubinński J, Luccarini C, Lundvall L, Mai PL, Mendoza-Fandiño G, Manoukian S, Massuger LFAG, May T, Mazoyer S, McAlpine JN, McGuire V, McLaughlin JR, McNeish I, Meijers-Heijboer H, Meindl A, Menon U, Mensenkamp AR, Merritt MA, Milne RL, Mitchell G, Modugno F, Moes-Sosnowska J, Moffitt M, Montagna M, Moysich KB, Mulligan AM, Musinsky J, Nathanson KL, Nedergaard L, Ness RB, Neuhausen SL, Nevanlinna H, Niederacher D, Nussbaum RL, Odunsi K, Olah E, Olopade OI, Olsson H, Olswold C, O'Malley DM, Ong K-R, Onland-Moret NC, Orr N, Orsulic S, Osorio A, Palli D, Papi L, Park-Simon T-W, Paul J, Pearce CL, Pedersen IS, Peeters PHM, Peissel B, Peixoto A, Pejovic T, Pelttari LM, Permuth JB, Peterlongo P, Pezzani L, Pfeiler G, Phillips K-A, Piedmonte M, Pike MC, Piskorz AM, Poblete SR, Pocza T, Poole EM, Poppe B, Porteous ME, Prieur F, Prokofyeva D, Pugh E, Pujana MA, Pujol P, Radice P, Rantala J, Rappaport-Fuerhauser C, Rennert G, Rhiem K, Rice P, Richardson A, Robson M, Rodriguez GC, Rodríguez-Antona C, Romm J, Rookus MA, Rossing MA, Rothstein JH, Rudolph A, Runnebaum IB, Salvesen HB, Sandler DP, Schoemaker MJ, Senter L, Setiawan VW, Severi G, Sharma P, Shelford T, Siddiqui N, Side LE, Sieh W, Singer CF, Sobol H, Song H, Southey MC, Spurdle AB, Stadler Z, Steinemann D, Stoppa-Lyonnet D, Sucheston-Campbell LE, Sukiennicki G, Sutphen R, Sutter C, Swerdlow AJ, Szabo CI, Szafron L, Tan YY, Taylor JA, Tea M-K, Teixeira MR, Teo S-H, Terry KL, Thompson PJ, Thomsen LCV, Thull DL, Tihomirova L, Tinker AV, Tischkowitz M, Tognazzo S, Toland AE, Tone A, Trabert B, Travis RC, Trichopoulou A, Tung N, Tworoger SS, van Altena AM, Van Den Berg D, van der Hout AH, van der Luijt RB, Van Heetvelde M, Van Nieuwenhuysen E, van Rensburg EJ, Vanderstichele A, Varon-Mateeva R, Vega A, Edwards DV, Vergote I, Vierkant RA, Vijai J, Vratimos A, Walker L, Walsh C, Wand D, Wang-Gohrke S, Wappenschmidt B, Webb PM, Weinberg CR, Weitzel JN, Wentzensen N, Whittemore AS, Wijnen JT, Wilkens LR, Wolk A, Woo M, Wu X, Wu AH, Yang H, Yannoukakos D, Ziogas A, Zorn KK, Narod SA, Easton DF, Amos CI, Schildkraut JM, Ramus SJ, Ottini L, Goodman MT, Park SK, Kelemen LE, Risch HA, Thomassen M, Offit K, Simard J, Schmutzler RK, Hazelett D, Monteiro AN, Couch FJ, Berchuck A, Chenevix-Trench G, Goode EL, Sellers TA, Gayther SA, Antoniou AC, Pharoah PDP, AOCS study group, EMBRACE Study, GEMO Study Collaborators, HEBON Study, KConFab Investigators, OPAL study group . Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat Genet 2017;49:680–691. 10.1038/ng.3826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Collaborative Group on Epidemiological Studies of Ovarian Cancer . Ovarian cancer and body size: individual participant meta-analysis including 25,157 women with ovarian cancer from 47 epidemiological studies. PLoS Med 2012;9:e1001200. 10.1371/journal.pmed.1001200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Collaborative Group On Epidemiological Studies Of Ovarian Cancer, Beral V, Gaitskell K, Hermon C, Moser K, Reeves G, Peto R. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet 2015;385:1835–42. 10.1016/S0140-6736(14)61687-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li K, Hüsing A, Fortner RT, Tjønneland A, Hansen L, Dossus L, Chang-Claude J, Bergmann M, Steffen A, Bamia C, Trichopoulos D, Trichopoulou A, Palli D, Mattiello A, Agnoli C, Tumino R, Onland-Moret NC, Peeters PH, Bueno-de-Mesquita HB, Gram IT, Weiderpass E, Sánchez-Cantalejo E, Chirlaque M-D, Duell EJ, Ardanaz E, Idahl A, Lundin E, Khaw K-T, Travis RC, Merritt MA, Gunter MJ, Riboli E, Ferrari P, Terry K, Cramer D, Kaaks R. An epidemiologic risk prediction model for ovarian cancer in Europe: the EPIC study. Br J Cancer 2015;112:1257–65. 10.1038/bjc.2015.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pearce CL, Stram DO, Ness RB, Stram DA, Roman LD, Templeman C, Lee AW, Menon U, Fasching PA, McAlpine JN, Doherty JA, Modugno F, Schildkraut JM, Rossing MA, Huntsman DG, Wu AH, Berchuck A, Pike MC, Pharoah PDP, Huntsman DG, AH W. Population distribution of lifetime risk of ovarian cancer in the United States. Cancer Epidemiol Biomarkers Prev 2015;24:671–6. 10.1158/1055-9965.EPI-14-1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rosner BA, Colditz GA, Webb PM, Hankinson SE. Mathematical models of ovarian cancer incidence. Epidemiology 2005;16:508–15. 10.1097/01.ede.0000164557.81694.63 [DOI] [PubMed] [Google Scholar]
- 26. Gaitskell K, Coffey K, Green J, Pirie K, Reeves GK, Ahmed AA, Barnes I, Beral V, Abbiss H, Abbott S, Alison R, Allen N, Armstrong M, Baker K, Balkwill A, Banks E, Barnes I, Beral V, Black J, Blanks R, Bradbury K, Brown A, Cairns B, Canfell K, Canoy D, Chadwick A, Crossley B, Crowe F, Ewart D, Ewart S, Fletcher L, Floud S, Gathani T, Gerrard L, Goodill A, Green J, Guiver L, Hozak M, Lingard I, Kan SW, Kirichek O, Langston N, Liu B, Moser K, Pirie K, Reeves G, Shaw K, Sherman E, Strange H, Sweetland S, Tipper S, Travis R, Trickett L, Wright L, Yang O, Young H, Banks E, Beral V, Carpenter L, Dezateux C, Green J, Patnick J, Peto R, Sudlow C. Tubal ligation and incidence of 26 site-specific cancers in the Million women study. Br J Cancer 2016;114:1033–7. 10.1038/bjc.2016.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pfeiffer RM, Park Y, Kreimer AR, Lacey JV, Pee D, Greenlee RT, Buys SS, Hollenbeck A, Rosner B, Gail MH, Hartge P. Risk prediction for breast, endometrial, and ovarian cancer in white women aged 50 Y or older: derivation and validation from population-based cohort studies. PLoS Med 2013;10:e1001492. 10.1371/journal.pmed.1001492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Clyde MA, Palmieri Weber R, Iversen ES, Poole EM, Doherty JA, Goodman MT, Ness RB, Risch HA, Rossing MA, Terry KL, Wentzensen N, Whittemore AS, Anton-Culver H, Bandera EV, Berchuck A, Carney ME, Cramer DW, Cunningham JM, Cushing-Haugen KL, Edwards RP, Fridley BL, Goode EL, Lurie G, McGuire V, Modugno F, Moysich KB, Olson SH, Pearce CL, Pike MC, Rothstein JH, Sellers TA, Sieh W, Stram D, Thompson PJ, Vierkant RA, Wicklund KG, Wu AH, Ziogas A, Tworoger SS, Schildkraut JM. Risk prediction for epithelial ovarian cancer in 11 United States–Based case-control studies: incorporation of epidemiologic risk factors and 17 confirmed genetic loci. Am J Epidemiol 2016;184:555–69. 10.1093/aje/kww091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yang X, Song H, Leslie G, Engel C, Hahnen E, Auber B, Horváth J, Kast K, Niederacher D, Turnbull C, Houlston R, Hanson H, Loveday C, Dolinsky JS, LaDuca H, Ramus SJ, Menon U, Rosenthal AN, Jacobs I, Gayther SA, Dicks E, Nevanlinna H, Aittomäki K, Pelttari LM, Ehrencrona H, Borg Åke, Kvist A, Rivera B, Hansen TVO, Djursby M, Lee A, Dennis J, Bowtell DD, Traficante N, Diez O, Balmaña J, Gruber SB, Chenevix-Trench G, Jensen A, Kjær SK, Høgdall E, Castéra L, Garber J, Janavicius R, Osorio A, Golmard L, Vega A, Couch FJ, Robson M, Gronwald J, Domchek SM, Culver JO, de la Hoya M, Easton DF, Foulkes WD, Tischkowitz M, Meindl A, Schmutzler RK, Pharoah PDP, Antoniou AC, kConFab Investigators . Ovarian and breast cancer risks associated with pathogenic variants in RAD51C and RAD51D. J Natl Cancer Inst 2020;112:1242–50. 10.1093/jnci/djaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee A, Mavaddat N, Wilcox AN, Cunningham AP, Carver T, Hartley S, Babb de Villiers C, Izquierdo A, Simard J, Schmidt MK, Walter FM, Chatterjee N, Garcia-Closas M, Tischkowitz M, Pharoah P, Easton DF, Antoniou AC. Boadicea: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med 2019;21:1708–18. 10.1038/s41436-018-0406-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pal Choudhury P, Maas P, Wilcox A, Wheeler W, Brook M, Check D, Garcia-Closas M, Chatterjee N. iCARE: an R package to build, validate and apply absolute risk models. PLoS One 2020;15:e0228198. 10.1371/journal.pone.0228198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pal Choudhury P, Brook MN, Hurson AN, Lee A, Mulder CV, Coulson P, Schoemaker MJ, Jones ME, Swerdlow AJ, Chatterjee N, Antoniou AC, Garcia-Closas M. Comparative validation of the BOADICEA and Tyrer-Cuzick breast cancer risk models incorporating classical risk factors and polygenic risk in a population-based prospective cohort of women of European ancestry. Breast Cancer Res 2021;23. 10.1186/s13058-021-01399-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee AJ, Cunningham AP, Tischkowitz M, Simard J, Pharoah PD, Easton DF, Antoniou AC. Incorporating truncating variants in PALB2, CHEK2, and ATM into the BOADICEA breast cancer risk model. Genet Med 2016;18:1190–8. 10.1038/gim.2016.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dareng EO, Tyrer J, Barnes DR, Jones MR, Yang X, Aben KKH, Adank MA, Agata SA, Andrulis IL, Anton-Culver H, Antonenkova NN, Aravantinos G, Arun BK, Augustinsson A, Balmaña J, Bandera EV, Barkardottir RB, Barrowdale D, Beckmann MW, Beeghly-Fadiel A, Benitez J, Bermisheva M, Bernardini MQ, Bjorge L, Black A, Bogdanova NV, Bonanni B, Borg A, Brenton J, Budzilowska A, Butzow R, Buys SS, Cai H, Caligo MA, Campbell I, Cannioto R, Cassingham H, Chang-Claude J, Chanock SJ, Chen K, Chiew Y-E, Chung WK, Claes KBM, Colanna S, Cook LS, Couch FJ, Daly MB, Dao F, Davies E, de la Hoya M, de Putter R, DePersia A, Devilee P, Diez O, Ding YC, Doherty JA, Domchek SM, Dörk T, du Bois A, Dürst M, Eccles DM, Eliassen HA, Engel C, Evans DG, Fasching P, Flanagan JM, Foretova L, Fortner RT, Friedman E, Ganz PA, Garber J, Gensini F, Giles GG, Glendon G, Godwin AK, Goodman MT, Greene MH, Gronwald J, Hahnen E, Haiman CA, Håkansson N, Hamann U, Hansen TVO, Harris HR, Hartman M, Heitz F, Hildebrandt MAT, Høgdall E, Høgdall CK, Hopper JL, Huang R-Y, Huff C, Hulick PJ, Huntsman DG, Imyanitov EN, Isaacs C, Anna Jakubowska A, James P, Janavicius R, Jensen A, Johannsson OT, John EM, Jones M, Kang D, Karlan BY, Karnezis A, Kelemen LE, Khusnutdinova E, Kiemeney LA, Kim B-G, Kjaer SK, Komenaka I, Kupryjanczyk J, Kurian AW, Kwong A, Lambrechts D, Larson MC, Lazaro C, ND L, Leslie G, Lester J, Lesueur F, Levine D, Li L, Li J, Loud JT, KH L, Lubiński J, Machackova E, Mai PL, Manoukian S, Marks J, Kim Matsuno R, Matsuo K, May T, McGuffog L, McLaughlin JR, McNeish IA, Mebirouk N, Menon U, Miller A, Milne RL, Minlikeeva A, Modugno F, Montagna M, Moysich KB, Munro E, Nathanson KL, Neuhausen SL, Nevanlinna H. Polygenic risk modelling for prediction of epithelial ovarian cancer risk. MedRxiv 2020. 10.1101/2020.11.30.20219220 [DOI] [Google Scholar]
- 35. Yang X, Leslie G, Gentry-Maharaj A, Ryan A, Intermaggio M, Lee A, Kalsi JK, Tyrer J, Gaba F, Manchanda R, Pharoah PDP, Gayther SA, Ramus SJ, Jacobs I, Menon U, Antoniou AC. Evaluation of polygenic risk scores for ovarian cancer risk prediction in a prospective cohort study. J Med Genet 2018;55:546–54. 10.1136/jmedgenet-2018-105313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Whittemore AS, Halpern J. Two-stage sampling designs for external validation of personal risk models. Stat Methods Med Res 2016;25:1313–29. 10.1177/0962280213480420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Terry MB, Liao Y, Whittemore AS, Leoce N, Buchsbaum R, Zeinomar N, Dite GS, Chung WK, Knight JA, Southey MC, Milne RL, Goldgar D, Giles GG, McLachlan S-A, Friedlander ML, Weideman PC, Glendon G, Nesci S, Andrulis IL, John EM, Phillips K-A, Daly MB, Buys SS, Hopper JL, MacInnis RJ. 10-Year performance of four models of breast cancer risk: a validation study. Lancet Oncol 2019;20:504–17. 10.1016/S1470-2045(18)30902-1 [DOI] [PubMed] [Google Scholar]
- 38. Barnes DR, Rookus MA, McGuffog L, Leslie G, Mooij TM, Dennis J, Mavaddat N, Adlard J, Ahmed M, Aittomäki K, Andrieu N, Andrulis IL, Arnold N, Arun BK, Azzollini J, Balmaña J, Barkardottir RB, Barrowdale D, Benitez J, Berthet P, Białkowska K, Blanco AM, Blok MJ, Bonanni B, Boonen SE, Borg Åke, Bozsik A, Bradbury AR, Brennan P, Brewer C, Brunet J, Buys SS, Caldés T, Caligo MA, Campbell I, Christensen LL, Chung WK, Claes KBM, Colas C, Collonge-Rame M-A, Cook J, Daly MB, Davidson R, de la Hoya M, de Putter R, Delnatte C, Devilee P, Diez O, Ding YC, Domchek SM, Dorfling CM, Dumont M, Eeles R, Ejlertsen B, Engel C, Evans DG, Faivre L, Foretova L, Fostira F, Friedlander M, Friedman E, Frost D, Ganz PA, Garber J, Gehrig A, Gerdes A-M, Gesta P, Giraud S, Glendon G, Godwin AK, Goldgar DE, González-Neira A, Greene MH, Gschwantler-Kaulich D, Hahnen E, Hamann U, Hanson H, Hentschel J, Hogervorst FBL, Hooning MJ, Horvath J, Hu C, Hulick PJ, Imyanitov EN, Isaacs C, Izatt L, Izquierdo A, Jakubowska A, James PA, Janavicius R, John EM, Joseph V, Karlan BY, Kast K, Koudijs M, Kruse TA, Kwong A, Laitman Y, Lasset C, Lazaro C, Lester J, Lesueur F, Liljegren A, Loud JT, Lubiński J, Mai PL, Manoukian S, Mari V, Mebirouk N, Meijers-Heijboer HEJ, Meindl A, Mensenkamp AR, Miller A, Montagna M, Mouret-Fourme E, Mukherjee S, Mulligan AM, Nathanson KL, Neuhausen SL, Nevanlinna H, Niederacher D, Nielsen FC, Nikitina-Zake L, Noguès C, Olah E, Olopade OI, Ong K-R, O'Shaughnessy-Kirwan A, Osorio A, Ott C-E, Papi L, Park SK, Parsons MT, Pedersen IS, Peissel B, Peixoto A, Peterlongo P, Pfeiler G, Phillips K-A, Prajzendanc K, Pujana MA, Radice P, Ramser J, Ramus SJ, Rantala J, Rennert G, Risch HA, Robson M, Rønlund K, Salani R, Schuster H, Senter L, Shah PD, Sharma P, Side LE, Singer CF, Slavin TP, Soucy P, Southey MC, Spurdle AB, Steinemann D, Steinsnyder Z, Stoppa-Lyonnet D, Sutter C, Tan YY, Teixeira MR, Teo SH, Thull DL, Tischkowitz M, Tognazzo S, Toland AE, Trainer AH, Tung N, van Engelen K, van Rensburg EJ, Vega A, Vierstraete J, Wagner G, Walker L, Wang-Gohrke S, Wappenschmidt B, Weitzel JN, Yadav S, Yang X, Yannoukakos D, Zimbalatti D, Offit K, Thomassen M, Couch FJ, Schmutzler RK, Simard J, Easton DF, Chenevix-Trench G, Antoniou AC, GEMO Study Collaborators, EMBRACE Collaborators, kConFab Investigators, HEBON Investigators, GENEPSO Investigators, Consortium of Investigators of Modifiers of BRCA and BRCA2 . Polygenic risk scores and breast and epithelial ovarian cancer risks for carriers of BRCA1 and BRCA2 pathogenic variants. Genet Med. In Press 2020;22:1653–66. 10.1038/s41436-020-0862-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kuchenbaecker KB, McGuffog L, Barrowdale D, Lee A, Soucy P, Dennis J, Domchek SM, Robson M, Spurdle AB, Ramus SJ, Mavaddat N, Terry MB, Neuhausen SL, Schmutzler RK, Simard J, Pharoah PDP, Offit K, Couch FJ, Chenevix-Trench G, Easton DF, Antoniou AC. Evaluation of polygenic risk scores for breast and ovarian cancer risk prediction in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 2017;109. 10.1093/jnci/djw302. [Epub ahead of print: 01 07 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Antoniou AC, Rookus M, Andrieu N, Brohet R, Chang-Claude J, Peock S, Cook M, Evans DG, Eeles R, Nogues C, Faivre L, Gesta P, van Leeuwen FE, Ausems MGEM, Osorio A, Caldes T, Simard J, Lubinski J, Gerdes A-M, Olah E, Fürhauser C, Olsson H, Arver B, Radice P, Easton DF, Goldgar DE, EMBRACE, GENEPSO, GEO-HEBON . Reproductive and hormonal factors, and ovarian cancer risk for BRCA1 and BRCA2 mutation carriers: results from the International BRCA1/2 carrier cohort study. Cancer Epidemiol Biomarkers Prev 2009;18:601–10. 10.1158/1055-9965.EPI-08-0546 [DOI] [PubMed] [Google Scholar]
- 41. Milne RL, Antoniou AC. Modifiers of breast and ovarian cancer risks for BRCA1 and BRCA2 mutation carriers. Endocr Relat Cancer 2016;23:T69–84. 10.1530/ERC-16-0277 [DOI] [PubMed] [Google Scholar]
- 42. Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-Feeding and risk of epithelial ovarian cancer. Cancer Causes Control 2012;23:919–27. 10.1007/s10552-012-9963-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Burnell M, Gentry-Maharaj A, Ryan A, Apostolidou S, Habib M, Kalsi J, Skates S, Parmar M, Seif MW, Amso NN, Godfrey K, Oram D, Herod J, Williamson K, Jenkins H, Mould T, Woolas R, Murdoch J, Dobbs S, Leeson S, Cruickshank D, Campbell S, Fallowfield L, Jacobs I, Menon U. Impact on mortality and cancer incidence rates of using random invitation from population registers for recruitment to trials. Trials 2011;12:61. 10.1186/1745-6215-12-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jmedgenet-2021-107904supp001.pdf (2.2MB, pdf)
Data Availability Statement
The model is freely available online (www.canrisk.org). For access to UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) dataset, which is subject to General Data Protection Regulations rules, please contact the UKCTOCS Biobank coordinator (s.apostolidou@ucl.ac.uk). The data access process is outlined online (http://uklwc.mrcctu.ucl.ac.uk/access-process/).