Summary
Background
Atrial fibrillation (AF) is the most common persistent cardiac arrhythmia. This study aimed to estimate its prevalence and explore associated factors in adults aged 18 years or older in China.
Methods
Study data were derived from a national sample from July 2020 to September 2021. Participants were recruited using a multistage stratified sampling method from twenty-two provinces, autonomous regions, and municipalities in China. AF was determined based on a history of diagnosed AF or electrocardiogram results.
Findings
A total of 114,039 respondents were included in the final analysis with a mean age of 55 years (standard deviation 17), 52·1% of whom were women. The crude prevalence of AF was 2·3% (95% confidence interval [CI] 1·7-2·8) and increased with age. The age-standardized AF prevalence was 1·6% (95% CI 1·6-1·7%) overall, and 1·7% (1·6-1·8%), 1·4% (1·3-1·5%), 1·6% (95% CI 1·5-1·7%), and 1·7% (1·6-1·9%) in men, women, urban areas, and rural areas, respectively. The prevalence was higher in the central regions (2·5%, 2·3-2·7%) than in the western regions (1·5%, 1·0-2·0%) and eastern regions (1·1%, 1·0-1·2%) in the overall population, either in the gender or residency subgroups. The associated factors for AF included age (per 10 years; odds ratio 1·41 [95% CI 1·38-1·46]; p < 0·001), men (1·34 [1·24-1·45]; p < 0·001), hypertension (1·22 [1·12-1·33]; p < 0·001), coronary heart disease (1·44 [1·28-1·62]; p < 0·001), chronic heart failure (3·70 [3·22-4·26]; p < 0·001), valvular heart disease (2·13 [1·72-2·63]; p < 0·001), and transient ischaemic attack/stroke (1·22 [1·04-1·43]; p = 0·013).
Interpretation
The prevalence of AF was 1.6% in the Chinese adult population and increased with age, with significant geographic variation. Older age, male sex, and cardiovascular disease were potent factors associated with AF. It is crucial to increase the awareness of AF and disseminate standardized treatment in clinical settings to reduce the disease burden.
Funding
This research was supported the Nature Science Foundation of Hubei province (No: 2017CFB204).
Keywords: Atrial fibrillation, Prevalence, Factor, Adult, China
Abbreviations: AF, atrial fibrillation; BMI, body mass index; CHD, coronary heart disease; CHF, chronic heart failure; CI, confidence interval; DM, diabetes mellitus; ECG, electrocardiogram; HTN, hypertension; OR, odds ratio; SD, standard deviation; TIA, transient ischaemic attack
Research in context.
Evidence before this study
We searched PubMed and the China National Knowledge Infrastructure database for articles published up to September 30, 2021 using the English and Chinese terms “atrial fibrillation”, “prevalence”, “epidemiology”, and “China”. In 2004, the prevalence of AF in China in individuals between the ages of 30 and 85 years was 0·61%, as reported by Zhou. In 2013, Li reported that the AF prevalence was 1·80% in individuals aged 60 years or older in Shanghai City. In 2015, using a medical insurance database of 471,446 individuals in Southwest China, Guo reported that the prevalence of incident AF in subjects older than 20 years was 0·2%. In southern China, the prevalence of AF among participants older than 35 years was 1·46% from 2015 to 2017. Du et al. performed another national community-based survey showed the weighted AF prevalence was 1·8% between 2014 and 2016. In 2018, Wang et al. reported that the prevalence of AF was 2·31% in adults older than 40 years from October 2014 to November 2015. However, no nationwide studies of AF prevalence and associated factors in adults older than 18 years in China have been reported.
Added value of this study
Our large, national, cross-sectional study was undertaken in a sample of 114,039 Chinese adults aged 18 years or older from twenty-two provinces, autonomous regions, and municipalities where have all established the provincial Atrial Fibrillation Center Alliances. Clinical criteria or electrocardiogram results were used to diagnose AF. Our results show that the overall prevalence of AF was 1·6% and increased with age, with significant geographical variation. Senior age, men, hypertension, hyperlipidaemia, coronary heart disease, chronic heart failure, valvular heart disease, and stroke/transient ischaemic attack were identified as major associated factors for AF.
Implications of all the available evidence
Our findings suggest an increase in the prevalence of AF compared with previous studies. Our study calls for new national policies and programs for the prevention and detection of AF. Specifically, raising awareness of diseases, screening for AF using smart tools, and disseminating standardized treatment in high-risk individuals should be public health priorities.
Alt-text: Unlabelled box
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, and is associated with substantial disability and mortality. AF is estimated to affect 2-4% of the adult population worldwide.1,2 In general, the prevalence of AF is projected to increase with population aging and social industrialization, especially in developing countries, such as China. Over the past two decades, several epidemiological studies on AF prevalence have been conducted in China. In 2004, Zhou et al. reported that the prevalence of AF was 0·61% based on a national epidemiological survey performed in subjects aged 30 to 85 years old in China.3 In southern China, the AF prevalence among participants older than 35 years was 1·46% from 2015 to 2017.4 A cross-sectional study, conducted in northeast China between September 2017 and March 2019, found that the overall AF prevalence was 1·1% in participants older than 40 years.5 However, two national epidemiological studies showed a higher prevalence of AF in populations with similar ages. A nationally representative study found that the standardized prevalence of AF was 2.3% from October 2014 to November 2015,6 and another national community-based survey showed that the weighted AF prevalence was 1.8% between 2014 and 20167, respectively. The inconsistency of the results can be mainly attributed to various participant characteristics, sample sizes, regions, and investigation methods. China has the largest population in the world spread over a vast territory. These studies were either national surveys conducted years to decades ago or based on a small sample restricted to certain areas. Therefore, the results are not representative of the current AF prevalence in the general Chinese population.
Since 2017, the China Cardiovascular Association has promoted Atrial Fibrillation Center programmes, aiming to enhance overall comprehensive management capabilities and reduce the burden of AF in China.8,9 To provide key information needed for the development of national policies to promote the construction of the Atrial Fibrillation Center, we performed a large, national epidemiological study of adults older than 18 years to estimate the prevalence of AF and explore associated factors for AF in China.
Methods
Study design and participants
The national epidemiology study was part of the real-world study of Chinese atrial fibrillation (RWS-CAF, registration number: ChiCTR1900021250), which was a multicentre, observational, cohort study. Briefly, we used a multistage, stratified cluster sampling procedure to recruit community-dwelling residents aged 18 years or older (Appendix 1). In stage one, we selected twenty-two provinces, autonomous regions, and municipalities that have all established the provincial Atrial Fibrillation Center Alliances (Appendix 2), and divided them into three major geographical regions of China (i.e., Eastern, Central, and Western China). Then, three prefecture-level cities/areas from each provincial region stratified by economic level (based on the median provincial gross domestic product) were randomly selected. The list of selected prefecture-level cities is summarized in Appendix 3. In stage two, we randomly selected two cities and counties from selected prefecture-level cities based on the level of economic development, which represent samples from urban and rural areas, respectively. In stage three, urban districts and rural townships were randomly selected from every city and county. Finally, participants aged 18 years or older were cluster recruited via telephone and household visits from the selected urban residential and rural village communities, which were randomly selected from urban districts and rural townships. We determined the sample size of each sampling area based on the 2010 China census data.10
We only enrolled permanent residents (those living in their current residence for 6 months or longer) in the selected communities. A total of 329 study sites (193 urban and 136 rural communities) participated in the study. We excluded individuals who were unable to complete the ECG examination due to physical disabilities, pregnancy or breastfeeding. The study protocol was approved by the Institutional Committee on Human Research at Renmin Hospital of Wuhan University (Wuhan, China). Written informed consent was obtained from all study participants. Patients and the public were not involved in the design, conduct, reporting or dissemination of this research. The details of the organization, survey process and quality control are supplemented in Appendix 1.
Data collection and definitions
We collected data on demographic information, lifestyle factors (e.g., smoking, drinking), and medical history using a questionnaire during the face-to-face interviews. Medical history was obtained according to participants’ medical records or self-reports, and information regarding hypertension (HTN), hyperlipidaemia, diabetes mellitus (DM), coronary heart disease (CHD), chronic heart failure (CHF), valvular heart disease, stroke, and transient ischaemic attack (TIA) was obtained. The CHA2DS2-VASc score was calculated from the sum of the risk factors of congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke, vascular disease, age 65-74 years, and sex category (female); weighing each by 1 except for stroke and age ≥ 75 years, which were weighed by 2.1 If a participant had a medical history of AF, information, such as AF pattern and treatment, was also recorded in detail. Five patterns of AF were distinguished, based on medical records, presentation, duration, and spontaneous termination of AF episodes, in participants previously diagnosed with AF. The definition of diseases was supplemented in the Appendix 1.
Twelve-lead body surface electrocardiogram (ECG) or a single-lead ECG was obtained for all participants in a quiet situation using a recorder from Shinall Technology (http://www.xinluomed.com). The ECG recordings were separately analysed by two well-trained cardiologists; another investigating cardiologist reviewed the results when their analysis results were inconsistent. If there was uncertainty about the presence of AF, the ECGs were adjudicated by a consensus group. Consistent with the recent European Society of Cardiology guidelines,1 AF was defined as a standard 12-lead ECG recording or a single-lead ECG tracing of ≥ 30 s showing heart rhythm with no discernible repeating P waves and irregular RR intervals or a documented medical history of diagnosed AF. We also obtained physical measurements, including height, weight, and blood pressure, following standard protocols.11,12 Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2), and obesity was defined as a BMI ≥ 28 kg/m2.13
Statistical analysis
We estimated the prevalence of AF among all participants. All calculations were weighted to represent the general adult population aged 18 years or older in China according to the 2010 population census,9 and were stratified by sampling clusters. Age-standardized rates of AF prevalence were also calculated using data from the 2010 Chinese census.10 Sampling weights at each level were equal to the reciprocal of the relevant sampling probability. Continuous variables are presented as the mean ± standard deviation (SD), and categorical variables are presented as counts and percentages (%). We used all participants for whom the variables of interest were available. We did not impute missing data. Means were compared with Analysis of Variance, and proportions were compared with the Chi-square test. Cochran-Armitage test was used to evaluate the trend of AF prevalence in different age groups. Multivariate logistic regression with stepwise model was performed to estimate the association of the odds of AF with age (per 10 years), sex, residence location, geographical regions (east, central, west), ethnic origin, marital status, education level, obesity, current smoker, current drinker, and medical history (including HTN, DM, hyperlipidaemia, CHD, CHF, valvular heart disease, and TIA/stroke). Four models were built to assess factors applicable among the total population, and three geographical regions. All analyses were performed using SAS 9.4 (SAS Institute, NC, USA) or SPSS V.20.0 software (IBM, West Grove, Pennsylvania, USA), and statistical significance was defined as p < 0·05 with two-tailed testing.
Role of the funding source
The study funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author had full access to the data and the final responsibility to submit for publication.
Results
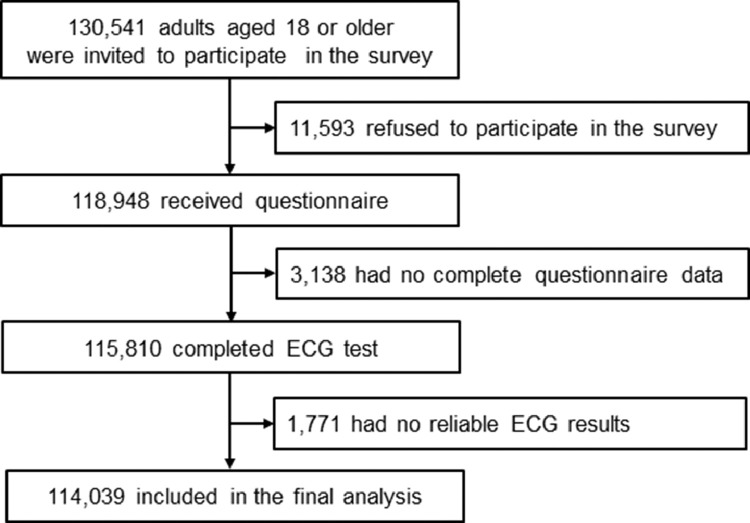
Between July 2020 and September 2021, a total of 130,541 (61,584 men and 68,957 women) individuals were approached through the survey. A total of 115,810 people (55,723 men and 60,087 women) completed the study. The overall response rate was 88·7% (90·5% men and 87·1% women). Response rates in three geographical regions and twenty-two provincial regions are presented in Appendix 4. After excluding individuals with unreliable ECG tests, 114,039 participants were enrolled in the final analysis (Figure 1). The mean age of the participants was 55 years (SD 17). In total, 59,431 (52·1%) participants were women, and 72,837 (63·9%) resided in urban areas. The characteristics of the study population are presented in Table 1.
Figure 1.
Flow of participants through the study.
Table 1.
Demographic characteristics of the study population.
| Overall | No AF | AF | p value | |
|---|---|---|---|---|
| 114039 (100%) | 111435 (97·7%) | 2604 (2·3%) | ||
| Sex | ||||
| Men | 54608 (47·9%) | 53195 (47·7%) | 1413 (54·3%) | <0·001 |
| Women | 59431 (52·1%) | 58240 (52·3%) | 1191 (45·7%) | ·· |
| Age (years) | ||||
| Mean | 55 (17) | 54 (17) | 65 (14) | <0·001 |
| 18-29 | 10750 (9·4%) | 10704 (9·6%) | 46 (1·8%) | <0·001 |
| 30-39 | 14852 (13·0%) | 14722 (13·2%) | 130 (5·0%) | ·· |
| 40-49 | 15972 (14·0%) | 15776 (14·2%) | 196 (7·5%) | ·· |
| 50-59 | 22399 (19·6%) | 21983 (19·7%) | 416 (16·0%) | ·· |
| 60-69 | 25516 (22·4%) | 24800 (22·2%) | 716 (27·5%) | ·· |
| 70-79 | 18311 (16·1%) | 17582 (15·8%) | 729 (28·0%) | ·· |
| ≥80 | 6239 (5·5%) | 5868 (5·3%) | 371 (14·2%) | ·· |
| Residence location | ||||
| Urban | 72837 (63·9%) | 71071 (63·8%) | 1766 (67·8%) | <0·001 |
| Rural | 41202 (36·1%) | 40364 (36·2%) | 838 (32·2%) | ·· |
| Geographical region | ||||
| East | 60192 (52·8%) | 58934 (52·9%) | 1258 (48·3%) | <0·001 |
| Central | 36113 (31·7%) | 35207 (31·6%) | 906 (34·8%) | ·· |
| West | 17734 (15·5%) | 17294 (15·5%) | 440 (16·9%) | ·· |
| Education attainment | ||||
| Primary school or less | 67878 (59·5%) | 66114 (59·3%) | 1764 (67·7%) | <0·001 |
| Middle and High school | 24409 (21·4%) | 23881 (21·4%) | 528 (20·3%) | ·· |
| College and higher | 21752 (19·1%) | 21440 (19·3%) | 312 (12·0%) | ·· |
| Ethnic Group | ||||
| Han | 108848 (95·4%) | 106359(95.4%) | 2489 (95·6%) | 0.771 |
| Non-Han | 5191 (4·6%) | 5076 (4·6%) | 115 (4·4%) | ·· |
| Marital status | ||||
| Married | 101571 (89·1%) | 99205 (89·0%) | 2366 (90·9%) | 0·003 |
| Widowed, divorced, single, or other | 12468 (10·9%) | 12230 (11·0%) | 238 (9·1%) | ·· |
| Current smoker | 12583 (11·0%) | 12278 (11·0%) | 305 (11·7%) | 0·268 |
| Current drinker | 9628 (8·4%) | 9381 (8·4%) | 247 (9·5%) | 0·053 |
| Obesity (BMI≥28 kg/m2) | 10969 (9·6%) | 10676 (9·6%) | 293 (11·3%) | 0·004 |
| Medical History | ||||
| HTN | 29859 (26·2%) | 28824 (25·9%) | 1035 (39·7%) | <0·001 |
| DM | 11151 (9·8%) | 10688 (9·6%) | 463 (17·8%) | <0·001 |
| Hyperlipidaemia | 11270 (9·9%) | 10833 (9·7%) | 437 (16·8%) | <0·001 |
| CHD | 8982 (7·9%) | 8390 (7·5%) | 592 (22·7%) | <0·001 |
| CHF | 2756 (2·4%) | 2364 (2·1%) | 392 (15·1%) | <0·001 |
| Valvular heart disease | 1137 (1·0%) | 998 (0·9%) | 139 (5·3%) | <0·001 |
| TIA/stroke | 3339 (2·9%) | 3088 (2·8%) | 251 (9·6%) | <0·001 |
Data are reported as n (%) or mean (SD).
AF=atrial fibrillation, BMI=body mass index, CHD=coronary heart disease, CHF=chronic heart failure, DM= diabetes mellitus, HTN=hypertension, TIA=transient ischaemic attack.
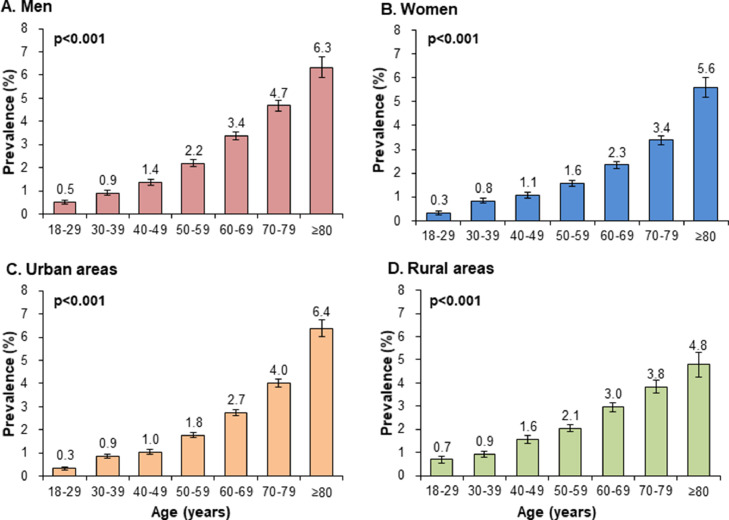
Overall, 2·3% (2,604, 95% confidence interval [CI] 1·7-2·8%) of the study population had AF. Among participants with AF, 1,463 (56·2%) cases had a medical history of AF and 1,141 (43·8%) cases of newly diagnosed AF, 101 (3·9%) cases and 2,503 (96·1%) cases of AF were diagnosed with valvular and non-valvular AF, respectively. People with AF were more likely to be men, older, urban residents, married, obese, and have HTN, DM, hyperlipidaemia, CHD, CHF, valvular heart disease, and TIA/stroke, as well as have a lower educational level than those without AF (Table 1). Among participants previously diagnosed with AF, the mean age was 69 years (12), 45·0% were women, 5·9% had valvular AF, and 93·1% had a CHA2DS2-VASc score greater than 1 in participants with non-valvular AF (Appendix 5). 32·1% of patients received anticoagulation therapy, and the anticoagulation rate was higher in urban areas than that in rural areas (390 [36·6%] vs 79 [19·8%]; p < 0·001, Appendix 5). The crude AF prevalence was higher in men than in women (2·6% [2·5-2·7%] vs 2·0% [1·9-2·1%]; p < 0·001), and in urban areas than in rural areas (2·4% [2·2-2·6%] vs 2·0% [1·8-2·2%]; p < 0·001). The prevalence of AF increased with age both in the total population (Appendix 6) and in three geographical regions (Appendix 7), and the overall prevalence increased from 0·4% (46 of 10,750, 0·3-0·5%) at ages of 18-29 years to 5·9% (371/6,239, 5·4-6·5%) at ages of 80 years or older (p < 0·001). AF prevalence also increased with age in both men and women, urban areas and rural areas (Figure 2). Regional variations occurred for AF prevalence, and prevalence was higher in the central (2·5%, 2·3-2·7%) and western regions (2·5%, 2·3-2·7%) than in the eastern region (2·1%, 2·0-2·2%; p < 0·001, Appendix 7).
Figure 2.
Prevalence of AF based on sex, residence and age group. Bars represent proportion and error bars for the 95% CI. Age-specific prevalence of AF in men (A) and women (B), urban areas (C) and rural areas (D).
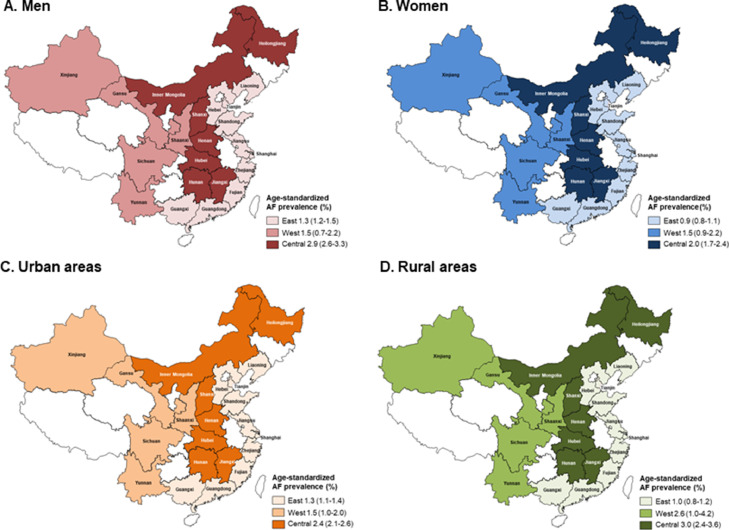
After weighing and adjusting using data from the 2010 Chinese census, the age-standardized prevalence of AF was 1·6% (95% CI 1·6-1·7%) overall. Compared with men, women had a lower age-standardized AF prevalence (women 1·4% [95% CI 1·3-1·5%] vs. men 1·7% [1·6-1·8%]). No significant difference was noted between urban and rural areas (urban areas 1·6% [95% CI 1·5-1·7%] vs. rural areas 1·7% [1·6-1·9%]). The age-standardized AF prevalence varies by geographical region, and the prevalence was highest in the central region (2·5%, 2·3-2·7%), followed by the western (1·5%, 1·0-2·0%) and eastern regions (1·1%, 1·0-1·2%). The central region had also higher age-standardized AF prevalence compared with western and eastern regions for both the men and women, urban and rural areas (Figure 3).
Figure 3.
Age-standardized AF prevalence in three geographical regions. Age-standardized AF prevalence in men (A) and women (B) as well as urban (C) and rural (D) subgroups in three geographical regions.
In multivariate logistic regression analysis of the total population, AF was significantly associated with older age (per 10 years; odds ratio 1·41 [95% CI 1·38-1·46]; p < 0·001), men (1·34 [1·24-1·45]; p < 0·001), HTN (1·22 [1·12-1·33]; p < 0·001), CHD (1·44 [1·28-1·62]; p < 0·001), CHF (3·70 [3·22-4·26]; p < 0·001), valvular heart disease (2·13 [1·72-2·63]; p < 0·001), and TIA/stroke (1·22 [1·04-1·43]; p = 0·013) after adjusting for residence location, geographical regions, ethnic origin, marital status, education level, obesity, current smoker, current drinker, and hyperlipidaemia (Table 2).Among the eastern region, older age, men, and have a HTN, hyperlipidaemia, CHD, CHF, valvular heart disease, and TIA/stroke remained significantly associated with the prevalence of AF. However, hyperlipidaemia and TIA/stroke were no longer significantly associated factors among the central region. Moreover, non-Han nationality (1·75 [1·25-2·44]; p = 0·001) became a new factor among the western region, but men remained nonsignificant (Table 2).
Table 2.
Association of different patient characteristics and atrial fibrillation in multivariate logistic regression models.
| OR (95%CI) | p value | |
|---|---|---|
| Model 1: Among eastern region | ||
| Age (per 10 years) | 1·47 (1·42-1·53) | <0·001 |
| Sex | ||
| Men | 1·36 (1·21-1·52) | <0·001 |
| Women | 1 (ref) | ·· |
| HTN | ||
| Yes | 1·22 (1·08-1·39) | 0·002 |
| No | 1 (ref) | ·· |
| Hyperlipidaemia | ||
| Yes | 1·35 (1·15-1·59) | 0·001 |
| No | 1 (ref) | ·· |
| CHD | ||
| Yes | 1·35 (1·12-1·62) | 0·002 |
| No | 1 (ref) | ·· |
| CHF | ||
| Yes | 3·70 (2·92-4·69) | <0·001 |
| No | 1 (ref) | ·· |
| Valvular heart disease | ||
| Yes | 1·81 (1·31-2·52) | <0·001 |
| No | 1 (ref) | ·· |
| TIA/stroke | ||
| Yes | 1·31 (1·01-1·69) | 0·041 |
| No | 1 (ref) | ·· |
| Model 2: Among central region | ||
| Age (per 10 years) | 1·38 (1·31-1·44) | <0·001 |
| Sex | ||
| Men | 1·40 (1·22-1·60) | <0·001 |
| Women | 1 (ref) | ·· |
| HTN | ||
| Yes | 1·22 (1·06-1·42) | 0·007 |
| No | 1 (ref) | ·· |
| CHD | ||
| Yes | 1·79 (1·48-2·15) | <0·001 |
| No | 1 (ref) | ·· |
| CHF | ||
| Yes | 3·03 (2·41-3·82) | <0·001 |
| No | 1 (ref) | ·· |
| Valvular heart disease | ||
| Yes | 1·84 (1·30-2·59) | <0·001 |
| No | 1 (ref) | ·· |
| Model 3: Among western region | ||
| Age (per 10 years) | 1·38 (1·28-1·49) | <0·001 |
| Ethnic origin | ||
| Non-Han | 1·75 (1·25-2·44) | 0·001 |
| Han | 1 (ref) | ·· |
| Hyperlipidaemia | ||
| Yes | 1·60 (1·26-2·02) | <0·001 |
| No | 1 (ref) | ·· |
| CHD | ||
| Yes | 1·34 (1·03-1·73) | 0·030 |
| No | 1 (ref) | ·· |
| CHF | ||
| Yes | 4·54 (3·45-5·99) | <0·001 |
| No | 1 (ref) | ·· |
| Valvular heart disease | ||
| Yes | 6·71 (4·10-10·98) | <0·001 |
| No | 1 (ref) | ·· |
| TIA/stroke | ||
| Yes | 1·64 (1·15-2·33) | 0·007 |
| No | 1 (ref) | ·· |
| Model 4: Among the total population | ||
| Age (per 10 years) | 1·41 (1·38-1·46) | <0·001 |
| Sex | ||
| Men | 1·34 (1·24-1·45) | <0·001 |
| Women | 1 (ref) | ·· |
| HTN | ||
| Yes | 1·22 (1·12-1·33) | <0·001 |
| No | 1 (ref) | ·· |
| CHD | ||
| Yes | 1·44 (1·28-1·62) | <0·001 |
| No | 1 (ref) | ·· |
| CHF | ||
| Yes | 3·70 (3·22-4·26) | <0·001 |
| No | 1 (ref) | ·· |
| Valvular heart disease | ||
| Yes | 2·13 (1·72-2·63) | <0·001 |
| No | 1 (ref) | ·· |
| TIA/stroke | ||
| Yes | 1·22 (1·04-1·43) | 0·013 |
| No | 1 (ref) | ·· |
CHD=coronary heart disease, CHF=chronic heart failure, CI=confidence interval, DM= diabetes mellitus, HTN=hypertension, OR=odds ratio, ref=reference, TIA=transient ischaemic attack.
Discussion
To our knowledge, the present large national investigation provided important information on AF in China. First, our results showed that the overall prevalence of AF was 1·6% in Chinese adults. This value is greater than previous estimates and indicates a 146% increase compared with the previous study performed in 2004.3 Second, the prevalence of AF increases with age, and men had a higher AF prevalence than women, but significant differences were not noted between urban and rural residents. Moreover, the AF prevalence presented an obvious geographic variation, with a greater prevalence in the central region. Third, factors associated with AF included older age, men and previous cardiovascular diseases, with a subtle difference among the three geographical regions. Considering the vast population of China, the burden of AF is heavy. AF remains an important public health problem in China that requires attention.
Since the study reported by Zhou et al. two decades ago,3 several epidemiological surveys on AF prevalence have been performed in China. However, there has been a lack of national epidemiological studies of AF during the past five years. Previous studies have reported inconsistent results due to the differences in study design and participant characteristics. Ten years ago, Li Lihua and colleagues enrolled 3,922 individuals aged 60 years or older and found that the AF prevalence was 1·80% in Shanghai City.14 Two other studies conducted in Northeast and South China found AF prevalence rates of 1·10% and 1·46% in individuals older than 40 years and 35 years, respectively.4,5 However, two national cross-sectional studies conducted at five years ago showed standardized prevalence rate of AF of 2.31% and 1.8%,6,7 which were all higher than those in regional surveys.4,5 The inconsistent results suggest that many complex factors influence AF prevalence, such as population characteristics, survey methodology, regional medical service capacity and economic level, etc. AF prevalence is positively correlated with advancing age, but data on adults aged younger than 35 years are lacking in China. Guo Yutao et al. in 2015 used a medical insurance database from 2001 to 2012 in Southwest China to identify that the prevalence of incident AF was 0·2% in subjects aged 20 years or older.15 However, the data were restricted to hospital medical records and did not include on-site investigations. The prevalence of AF may not reflect the true prevalence in adults in China. Our results revealed that the AF prevalence was 1·6% in Chinese adults aged 18 years or older, and increased from 0·4% in the age group of 18–29 years to 5·9% in the age group including those 80 years or older. Our data suggest the need to channel more attention to the young population with AF because the prevalence may not be not as low as expected.
Our findings suggest that AF has become more common across China in the past 20 years. Several potential reasons could be account for the substantial increase. First, extended longevity has become a more obvious sociodemographic phenomenon with rapid population aging in China. The acceleration of population aging has exceeded that of many developed countries, and the proportion of adults aged 60 years and older is expected to increase from 12.4% to 28% between 2010 and 2040.16,17 Aging populations and subsequent cardiovascular diseases are the primary drivers of AF development and progression.18, 19, 20 Second, convenient screening tools developed in recent years, such as smart watches and long-term single-lead patches, greatly facilitate the detection and diagnosis of AF.21 Other self-service devices with intelligent algorithms provide more choices for opportunistic screening of AF, especially in patients with paroxysmal and asymptomatic AF.22 Third, benefiting from the rapid growth of the economy, the country's medical insurance payment ability, disease management capability of disease and residents’ health awareness have all been substantially improved in China. As a result, the frequency of medical treatment for the general population and the diagnosis rate of AF have gradually increased. This condition subsequently puts a large number of populations at risk of cardioembolic stroke and systemic embolization. However, the anticoagulation therapy has improved substantially compared with a previous study,7 despite exist the urban-rural disparity, which may be attributed to the construction of the Atrial Fibrillation Center.
Our results found that AF was more frequent in men than in women. Theoretically, oestrogen has a protective effect on the cardiovascular system, which is related to the low prevalence of cardiovascular disease in premenopausal women.23,24 In women, a lower risk factor burden of cardiovascular disease and frequent primary prevention strategies, including adoption of healthy lifestyle behaviours and use of proven medicines, collectively play a protective role to reduce the risk of AF.25,26 It should be emphasized that the prevalence of AF was similar between urban areas and rural areas, but showed a large difference among geographical regions. Similar to the geographic variability in other cardiovascular diseases, AF has increased sharply in rural areas as well as urban areas in recent decades. However, its diagnosis rate is closely related to the local economic level, medical service capacity and health awareness, which exhibit considerable geographical disparity.27, 28, 29, 30 In general, the Eastern China has the highest levels of economic hygiene and the greatest proportion of young adults, which contributes to the lowest prevalence of AF. Unlike the central and eastern regions, non-Han ethnicity became a significant factor associated with AF, while male gender was no longer significant in the western region. This finding suggests that a fundamental structural change is needed to address AF in China. Improvement in adherence to treatment is as important as education and screening. These issues include educating patients, training physicians, and improving medical insurance coverage.
Compared with other Asian countries, China appears to have a higher prevalence of AF. For example, a previous study conducted in 2006 found the estimated overall prevalence of AF in Japanese adults aged greater than 40 years was 1.6% .31 Yonezawa Y reported a 0.92% of AF prevalence rate in Japanese adults aged 20 years or older from April 2013 to March 2014, with a rate four times higher in men (1.46%) than in women (0.37%).32 In South Korea, the prevalence of AF in the total adult population was observed to be 0.67% in 2015.33 The estimated AF prevalence was 2.8% for age ≥ 65 years in Thailand,34 and 1.5% for age ≥55 years in Singapore.35 Nonetheless, our studies found several common associated factors for AF, such as older age, men, cardiac disease, and TIA/stroke. In addition to differences in population characteristics and survey methods, the lower level of the national health economy could be an important factor that causes a higher AF prevalence in China than those in other Asian countries.
The present study had several potential limitations. First, the major limitation is that self-report questionnaires and medical history may introduce inevitable errors, and potentially lead to bias in the estimation of the prevalence and associated factors. Second, although the included sample was corrected in the final analysis, population migration and exclusion criteria exist in the survey inevitably introduce selection bias. Third, considering the operability and the consistency of the diagnostic criteria, we still used traditional ECG as a screening tool for AF and did not include mobile devices with smart or long recording durations. This study design mainly underestimates the prevalence of paroxysmal AF. Fourth, AF is a heterogeneous disease, and many pathogenic factors could lead to AF. Thus, it is difficult to determine all potential risk factors or predictors, and the interpretation of relevant results might be inconclusive. Finally, as the 2020 population census has not been fully released and is not available, therefore the AF prevalence was weighted according to the 2010 population census. In general, the Chinese population structure presents an aging trend, so it would inevitably affect and lead to AF underestimation the estimates in the current study.
In conclusion, our data indicate that AF is currently more prevalent in the adult population than previously reported in China, and old age, men, and cardiovascular disease are major associated factors for AF. These results suggest a serious situation in terms of prevention and control of AF in China. Strengthening screening and education programs supplemented by protocols and policies that improve adherence to treatment are key issues, that urgently need to be solved to reduce AF burden in China.
Contributors
Congxin Huang, He Huang, and Shaobo Shi had the idea for and designed the study. Shaobo Shi, Yanhong Tang, and Qingyan Zhao led the data collection. Yanhong Tang, Qiangsun Zheng, Yigang Li, Liangrong Zheng, Yiqiang Yuan, Jingquan Zhong, Jian Xu, Yanqing Wu, Jing Xu, Lin Chen, Shufeng Li, Jian Jiang, Jingfeng Wang, Jie Fan, Minglong Chen, Baopeng Tang, Wei Li, Qiang Wu, Bei Shi, Shenghua Zhou, Xingsheng Zhao, Yuehui Yin, Zheng Zhang, Guoqiang Zhong, Xuebin Han, Fan Liu, Ming Wu, and Lianjun Gao organized on-site investigation projects in various province. Shaobo Shi, Bo Yang, and Qingyan Zhao did the statistical analysis supported by Hong Yan, and Bin Yu. Shaobo Shi, Qingyan Zhao and Yanhong Tang wrote the draft report. All authors contributed to acquisition, analysis, or interpretation of data. All authors, revised the report and approved the final version before submission.
Data sharing
Article components including study protocol, statistical analysis approach, and de-identified data will be available for investigators following approval from the Institutional Review Board of Renmin Hospital of Wuhan University (Wuhan, China). Petitions can be sent to the corresponding author.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
All authors declare no competing interests.
Acknowledgments
We thank Junbo Ge, Yong Huo and other consultants for their instructions and contributions through the whole process of study; Shinall Technology for providing database network and screening equipment. We acknowledge the support provided by all partnership, including The Second Affiliated Hospital of Xi'an Jiaotong University; Xinhua Hospital Affiliated To Shanghai Jiao Tong University School of Medicine; The First Affiliated Hospital; Zhejiang University School of Medicine; Henan Provincial Chest Hospital; Qilu Hospital of Shandong University; Anhui Provincial Hospital; The Second Affiliated Hospital of Nanchang University; Tianjin Chest Hospital; Fujian Provincial Hospital; The Second Affiliated Hospital of Harbin Medical University; West China Hospital of Sichuan University; Sun Yat-sen Memorial Hospital; The Second People's Hospital of Yunnan Province; Jiangsu Province Hospital; The First Affiliated Hospital of Xinjiang Medical University; The Affiliated Hospital of Guizhou Medical University; Guizhou Provincial People's Hospital; Affiliated Hospital of Zunyi Medical University; The Second Xiangya Hospital of Central South University; Inner Mongolia Autonomous Region People's Hospital; The Second Affiliated Hospital of Chongqing Medical University, The First Hospital of Lanzhou University; The First Affiliated Hospital of Guangxi Medical University; Shanxi Cardiovascular Hospital; The Second Hospital of Hebei Medical University; Hainan General Hospital; The First Affiliated Hospital of Dalian Medical University. We thank all provincial and regional officers and research staff in China for their collection of data.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100439.
Contributor Information
He Huang, Email: huanghe1977@whu.edu.cn.
Congxin Huang, Email: huangcongxin@vip.163.com.
Appendix. Supplementary materials
References
- 1.Hindricks G., Potpara T., Dagres N., et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42:373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin E.J., Muntner P., Alonso A., et al. Heart disease and stroke statistics-2019 update: a report From the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 3.Zhou Z.Q., Hu D.Y., Chen J., Zhang R.H., Li K.B., Zhao X.L. An epidemiological survey of atrial fibrillation in China. Zhonghua Nei Ke Za Zhi. 2004;43:491–494. in Chinese. [PubMed] [Google Scholar]
- 4.Deng H., Guo P., Zheng M., et al. Epidemiological Characteristics of atrial fibrillation in southern china: results from the Guangzhou heart study. Sci Rep. 2018;8:17829. doi: 10.1038/s41598-018-35928-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xing L., Lin M., Du Z., Jing L., Tian Y., Yan H., et al. Epidemiology of atrial fibrillation in northeast China: a cross-sectional study, 2017-2019. Heart. 2020;106:590–595. doi: 10.1136/heartjnl-2019-315397. [DOI] [PubMed] [Google Scholar]
- 6.Wang X., Fu Q., Song F., Li W., Yin X., Yue W., et al. Prevalence of atrial fibrillation in different socioeconomic regions of China and its association with stroke: Results from a national stroke screening survey. Int J Cardiol. 2018;271:92–97. doi: 10.1016/j.ijcard.2018.05.131. [DOI] [PubMed] [Google Scholar]
- 7.Du X., Guo L., Xia S., Du J., Anderson C., Arima H., et al. Atrial fibrillation prevalence, awareness and management in a nationwide survey of adults in China. Heart. 2021;107(7):535–541. doi: 10.1136/heartjnl-2020-317915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao Q.Y., Shi S.B., Huang H., Jiang H., Yang B., Wu G., et al. Contemporary characteristics, management, and outcomes of patients hospitalized for atrial fibrillation in China: results from the real-world study of Chinese atrial fibrillation registry. Chin Med J (Engl) 2020;133(23):2883–2884. doi: 10.1097/CM9.0000000000001151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atrial Fibrillation Center. https://www.china-afc.org/. Accessed 16 November 2021.
- 10.National Bureau of Statistics of China. 2010 Population census. October 20, 2013. http://www.stats.gov.cn/english/ Statisticaldata/CensusData/.
- 11.Writing Group of 2018 Chinese Guidelines for the Management of Hypertension Chinese hypertension league, Chinese society of cardiology, Chinese medical doctor association hypertension committee, hypertension branch of China international exchange and promotive association for medical and health care, hypertension branch of Chinese geriatric medical association. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2019;24(1):24–56. in Chinese. [Google Scholar]
- 12.http://www.nhc.gov.cn/ewebeditor/uploadfile/2013/08/20130808141055922.pdf
- 13.Zhou BF; Cooperative Meta-Analysis Group of the Working Group on Obesity in China Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults-study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 14.Li L.H., Sheng C.S., Hu B.C., et al. The prevalence, incidence, management and risks of atrial fibrillation in an elderly Chinese population: a prospective study. BMC Cardiovasc Disord. 2015;15:31. doi: 10.1186/s12872-015-0023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo Y., Tian Y., Wang H., Si Q., Wang Y., Lip G.Y.H. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: new insights into the global burden of atrial fibrillation. Chest. 2015;147:109–119. doi: 10.1378/chest.14-0321. [DOI] [PubMed] [Google Scholar]
- 16.Fang E.F., Xie C., Schenkel J.A., et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64 doi: 10.1016/j.arr.2020.101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ye P., Jin Y., Er Y., et al. A scoping review of national policies for healthy ageing in Mainland China from 2016 to 2020. Lancet Reg Health West Pac. 2021;12 doi: 10.1016/j.lanwpc.2021.100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.North B.J., Sinclair D.A. The intersection between aging and cardiovascular disease. Circ Res. 2012;110:1097–1108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao D., Liu J., Wang M., Zhang X., Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16:203–212. doi: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- 20.Staerk L., Sherer J.A., Ko D., Benjamin E.J., Helm R.H. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120:1501–1517. doi: 10.1161/CIRCRESAHA.117.309732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freedman B., Camm J., Calkins H., et al. Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation. 2017;135:1851–1867. doi: 10.1161/CIRCULATIONAHA.116.026693. [DOI] [PubMed] [Google Scholar]
- 22.Mairesse G.H., Moran P., Van Gelder I.C., et al. Screening for atrial fibrillation: a European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLAECE) Europace. 2017;19:1589–1623. doi: 10.1093/europace/eux177. [DOI] [PubMed] [Google Scholar]
- 23.Knowlton A.A., Lee A.R. Estrogen and the cardiovascular system. Pharmacol Ther. 2012;135:54–70. doi: 10.1016/j.pharmthera.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy E. Estrogen signaling and cardiovascular disease. Circ Res. 2011;109:687–696. doi: 10.1161/CIRCRESAHA.110.236687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walli-Attaei M., Joseph P., Rosengren A., et al. Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;396:97–109. doi: 10.1016/S0140-6736(20)30543-2. [DOI] [PubMed] [Google Scholar]
- 26.Millett E.R.C., Peters S.A.E., Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018;363:k4247. doi: 10.1136/bmj.k4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan R., Li W., Yin L., Wang Y., Bo J. PURE-China Investigators. Cardiovascular Diseases and Risk-Factor Burden in Urban and Rural Communities in High-, Middle-, and Low-Income Regions of China: A Large Community-Based Epidemiological Study. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Center for Cardiovascular Diseases, China . Encyclopedia of China Publishing House; Beijing: 2020. Annual Report on Cardiovascular health and Diseases in China 2019. [Google Scholar]
- 29.Chen Y., Li L., Zhang Q., Clarke R., Chen J., Guo Y., et al. Use of drug treatment for secondary prevention of cardiovascular disease in urban and rural communities of China: China Kadoorie Biobank Study of 0.5 million people. Int J Cardiol. 2014;172:88–95. doi: 10.1016/j.ijcard.2013.12.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gu D., Gupta A., Muntner P., et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112:658–665. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 31.Iguchi Y., Kimura K., Aoki J., et al. Prevalence of atrial fibrillation in community-dwelling Japanese aged 40 years or older in Japan: analysis of 41,436 non-employee residents in Kurashiki-city. Circ J. 2008;72(6):909–913. doi: 10.1253/circj.72.909. [DOI] [PubMed] [Google Scholar]
- 32.Yonezawa Y., Horinaka S., Shirakawa C., Kogure Y. Estimated glomerular filtration ratio is a better index than creatinine clearance (Cockcroft-Gault) for predicting the prevalence of atrial fibrillation in the general Japanese population. Hypertens Res. 2018;41(6):451–459. doi: 10.1038/s41440-018-0032-6. [DOI] [PubMed] [Google Scholar]
- 33.Lee S.R., Choi E.K., Han K., Cha M.J., Oh S. Prevalence of non-valvular atrial fibrillation based on geographical distribution and socioeconomic status in the Entire Korean population. Korean Circ J. 2018;48(7):622–634. doi: 10.4070/kcj.2017.0362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suwanwela N.C., Chutinet A., Autjimanon H., et al. Atrial fibrillation prevalence and risk profile from novel community-based screening in Thailand: A prospective multi-centre study. Int J Cardiol Heart Vasc. 2021;32 doi: 10.1016/j.ijcha.2020.100709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yap K.B., Ng T.P., Ong H.Y. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J Electrocardiol. 2008;41(2):94–98. doi: 10.1016/j.jelectrocard.2007.03.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.