Abstract
Aims:
To understand the epidemiology, progression, and predictive factors of urinary incontinence (UI) in community-dwelling Mexican adults aged ≥ 50 by sex and UI subtypes (stress, urge, and mixed).
Methods:
We analyzed longitudinal UI data in community-dwelling adults aged ≥ 50 (7783 women and 5843 men) for the 2012 to 2015 period of the Mexican Health and Aging Study. We estimated mixed, stress, and urgency incontinence prevalence (2012); 2-year cumulative incidence and remissions (2015); and progression (2012–2015). A multivariate analysis was undertaken to evaluate the predictive factors for UI and its subtypes by sex.
Results:
The prevalence of UI was higher (27.7%) for women (average age 65.9 ± 9.5) than 12.5% men (average age 67.4 ± 9.3) and increased with age in both sexes (26.7% in women 50 to 59, to 48.5% in ≥ 90; and 6.8% in men 50 to 59, to 26.2% ≥ 90). The most frequent UI subtypes were mixed in women and urge in men. The cumulative incidence of UI was higher in women (22.9%) than men (12.3%) while its remission was higher in men than women. Predictive factors for UI in both sexes were depressive symptoms, a higher number of concomitant diseases and a history of falls; while advanced age was a factor only for men.
Conclusions:
UI is a common health problem and its prevalence and severity increase with age. Addressing modifiable risk factors such as depression and falls could decrease the prevalence and incidence of UI and its subtypes. Further studies should also focus on the relationship between mixed UI and male mortality.
Keywords: incidence, prevalence, remission
1 |. INTRODUCTION
Urinary incontinence (UI), defined as the involuntary leakage of urine,1 is a health problem that impacts quality of life and primarily affects women and older men.1,2 UI is also a predictor for long-term care,1 hospitalization, falls,3 a decrease of physical performance, functional impairment, as well as abuse.4
Epidemiological data on UI vary widely, for example reports on the prevalence of UI in community-dwelling older adults range from 17% to 55% in women and from 11% to 34% in men.5 However, this prevalence is predicted to increase by more than 50% in the coming decades6 because of changes to the population structure. Data on the incidence of UI is scarce as most of the existing literature comes from transversal studies. Nevertheless, some studies suggest that the annual incidence of UI in older women ranges between 8% and 20%7 and 9% and 10% in older men.5 With regard to data on UI remission, the rates fluctuate from 22% to 49% in women2 and from 27% to 32% in men.5 Because of anatomical and physiological differences of the genitourinary tract in men and women, the progression of each UI subtype differs by sex.
The etiology of UI is multifactorial. The primary associated factors include increased age, ethnicity, educational level, a history of incontinence,2,7 increasing body mass index (BMI), urethral sphincter incompetence or damage (either from prostate surgery in men, or pregnancy or vaginal birth om women),2,8 overactive bladder syndrome, alterations to the central nervous system, and compensatory mechanisms brought on by diseases such as diabetes mellitus, multimorbidity, impaired physical function and mobility, cognitive impairment, and falls.2,5,8,9 An association between depression and UI has also been reported, although it remains unclear whether there is a causal relationship between the two symptoms, or if they stem from separate causes.5
There are few studies on UI in middle income countries. In Mexico particularly, there is little awareness of the subject, despite the rapid aging of the population. For this reason, the objective of this study was to understand the prevalence, incidence, remission, progression, and predictive factors of UI in the Mexican community-dwelling population aged 50 and older, by sex, and by UI subtype: stress urinary incontinence (SUI), urge urinary incontinence (UUI), and mixed urinary incontinence (MUI).
2 |. MATERIAL AND METHODS
2.1 |. Study population
The sample for this study was drawn from the Mexican Health and Aging Study (MHAS), an ongoing, longitudinal study of community-dwelling Mexican adults aged 50 and older who were interviewed in 2001, 2003, 2012, and 2015. The MHAS methodology has been previously reported.10 This study looks at adults of both sexes aged 50 and older who were asked about UI in 2012 and 2015 because interview questions regarding UI subtypes were included as of 2012.
The sample to estimate prevalence and progression of UI and its subtypes consisted of 13 626 adults (7783 women and 5843 men). The sample used to estimate the incidence, remission, and predictive factors of UI and its subtypes consisted of 11 530 people (6670 women and 4860 men), with baseline information regarding UI from 2012 and follow-up information from 2015. This last set of data excluded individuals who had died during the intervening period (398 women and 407 men) (Figure 1).
FIGURE 1.
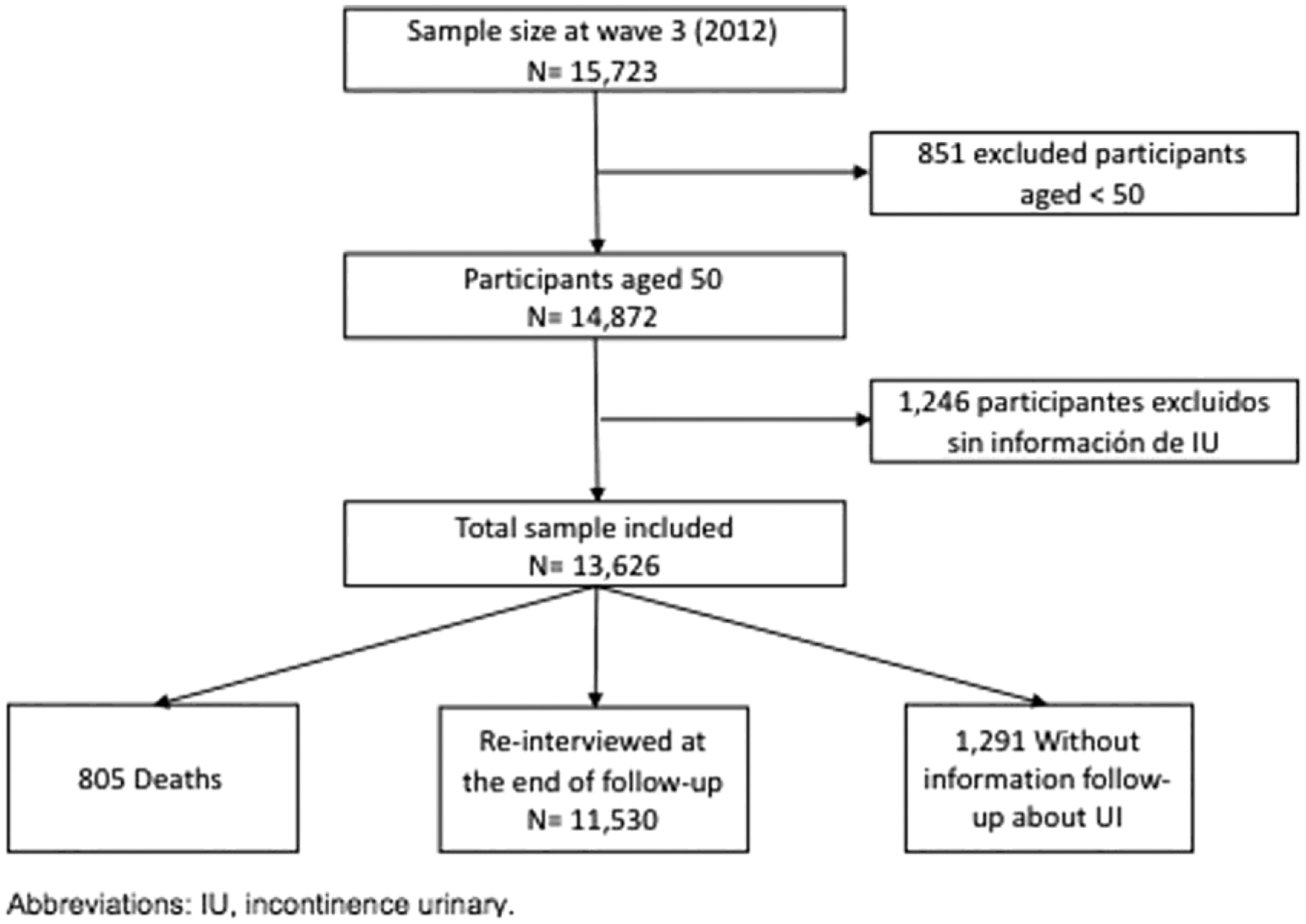
Sample selection flowchart
2.2 |. Definitions
Stress incontinence was present when the subject gave an affirmative answer to the question “During the last 2 years, have you experienced the involuntary leakage of urine when doing things like coughing, sneezing, picking things up or during exercise?” Urge incontinence was present when the subject gave an affirmative answer to the question “During the last 2 years, have you experienced the involuntary leakage of urine when you had the urge to urinate but couldn’t get to the bathroom in time?” Mixed incontinence was present when the subject answered both questions in the affirmative. When both questions were answered in the negative, UI was not considered to be present.
2.3 |. Variables
2.3.1 |. Outcome variables
The outcome variables indicate the UI status among the sample population in 2015. Using the questions about SUI and UUI, two dependent variables were established. The first dependent variable had two categories: with UI and without UI. The second dependent variable had four categories: without UI, with SUI, with UUI, and with MUI.
2.3.2 |. Covariates
Sociodemographic covariates
Age by decade group, educational level, marital status, number of children born (only for women), and type of residence (rural or urban).
Health, anthropometric and functional covariates
Self-perception of health status (“Would you say that your health is very good, good, fair, bad or very bad?”); the presence of depressive symptoms, evaluated using the modified version of the Center for Epidemiological Studies Depression Scale (CES-D) and using a score varying from 0 to 9 with a cutoff at five, after which higher scores indicate the presence of depressive symptoms11; the number of self-reported illnesses (“Has a doctor or medical professional ever told you that you have hypertension, diabetes, cancer, chronic obstructive pulmonary disease, arthritis, had a heart attack, or had a stroke?”); falls (“Have you fallen in the last 2 years?”); BMI, calculated using the subject’s weight in kilograms divided by the square of their body height in meters, and grouped according to the criteria proposed by the World Health Organization (WHO): normal weight (< 25.0 kg/m2), overweight (25 to < 30 kg/m2), and obese (≥ 30 kg/m2); the basic activities of daily life (BADL), defined as self-reported difficulties in bathing, eating, going to bed, using the bathroom, and getting dressed; and the instrumental activities of daily living (IADL), defined as self-reported difficulties with preparing meals, shopping for groceries and necessities, taking medicine, and managing money.
2.4 |. Statistical analysis
Using a descriptive analysis, this study estimated the prevalence, incidence and remission of UI and its subtypes. The progression of UI and its subtypes was estimated measuring changes in the prevalence of UI between 2012 and 2015. Finally, logistic regression models were used to evaluate the predictive factors for UI. Using a significance level of P< .05, Pearson χ2 test was used to analyze the association of each covariate with the dependent variables. In the longitudinal analysis we examined whether the 2012 baseline characteristics independently predicted the incidence of UI and its subtypes in 2015. Using bivariate and multivariate logistic regression models, the study modeled the 2015 UI status, controlling for the 2012 covariates: age by decade group, educational level, marital status, number of children (only for women), type of residence, self-perception of health status, the presence of depressive symptoms, number of self-reported illnesses, falls in the last 2 years, BMI, and limitations in BADL and IADL. Variables that were not significant in the bivariate analysis (P ≥ .05) were excluded in the longitudinal analyses, to obtain a more parsimonious model. Data processing was conducted using Stata version 11 (Stata Corp., College Station, TX).
3 |. RESULTS
In 2012, the prevalence of UI was 27.7% for women (with a mean age of 65.9 ± 9.5 years) and 12.5% for men (with a mean age of 67.4 ± 9.3 years). For both sexes, prevalence increased with age, except for SUI in women. For each age group, the prevalence of UI oscillated between 26.7% and 48.5% among women and 6.8% and 26.2% among men. The UI subtype with the highest prevalence was MUI (12.0%) in women and UUI (5.4%) in men.
For both, the prevalence of UI was higher among widows or those who lived alone, had a negative self-perception of their health status, depressive symptoms, a higher number of illnesses, a history of falls, or limitations in their BADLs and IADLs. Prevalence was also higher among women with a higher BMI and among men with lower educational levels (Tables 1,2).
TABLE 1.
Urinary incontinence prevalence, incidence and remission in women by UI subtype
| Variables | Total population (100%) | Prevalence, 2012 | Incidence (2012–2015) | Remission (2012–2015) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||||||||||
| Without UI | SUI | UUI | MUI | Total UI | SUI | UUI | MUI | Total UI | SUI | UUI | MUI | Total UI | ||
| Total | 7783 | 5628 (72.3) | 731 (9.4) | 488 (6.3) | 936 (12.0) | 2155 (27.7) | 405 (7.2) | 409 (7.3) | 473 (8.4) | 1287 (22.9) | 286 (39.1) | 218 (44.7) | 234 (25.0) | 738 (34.2) |
| Sociodemographic variables | ||||||||||||||
| Age | ||||||||||||||
| 50–59 | 2795 | 2050 (73.3) | 310 (11.1) | 150 (5.4) | 285 (10.2) | 745 (26.7) | 167 (8.1) | 107 (5.2) | 141 (6.9) | 415 (20.2) | 122 (39.4) | 75 (50.0) | 73 (25.6) | 270 (36.2) |
| 70–79 | 1577 | 1116 (70.8) | 124 (7.9) | 116 (7.4) | 221 (14.0) | 461 (29.2) | 72 (6.5) | 113 (10.1) | 106 (9.5) | 291 (26.1) | 46 (37.1) | 53 (45.7) | 59 (26.7) | 158 (34.3) |
| 60–69 | 2807 | 2043 72.8) | 254 (9.0) | 175 (6.2) | 335 (11.9) | 764 (27.2) | 147 (7.2) | 167 (8.2) | 188 (9.2) | 502 (24.6) | 106 (41.7) | 76 (43.4) | 87 (26.0) | 269 (35.2) |
| 80–89 | 538 | 385 (71.6) | 37 (6.9) | 40 (7.4) | 76 (14.1) | 153 (28.4) | 17 (4.4) | 21 (5.5) | 34 (8.8) | 72 (18.7) | 11 (29.7) | 12 (30.0) | 13 (17.1) | 36 (23.5) |
| 90+ | 66 | 34 (51.5) | 6 (9.1) | 7 (10.6) | 19 (28.8) | 32 (48.5) | 2 (5.9) | 1 (2.9) | 4 (11.8) | 7 (20.6) | 1 (16.7) | 2 (28.6) | 2 (10.5) | 5 (15.6) |
| Educational level | ||||||||||||||
| < 6 y | 3418 | 2470 (72.3) | 272 (8.0) | 228 (6.7) | 448 (13.1) | 948 (27.7) | 185 (7.5) | 200 (8.1) | 268 (10.9) | 653 (26.4) | 116 (42.6) | 126 (55.3) | 137 (30.6) | 379 (40.0) |
| 6 y | 1516 | 1090 (71.9) | 165 (10.9) | 92 (6.1) | 169 (11.1) | 426 (28.1) | 96 (8.8) | 95 (8.7) | 104 (9.5) | 295 (27.1) | 73 (44.2) | 45 (48.9) | 48 (28.4) | 166 (39.0) |
| > 6 y | 2040 | 1502 (73.6) | 232 (11.4) | 107 (5.2) | 199 (9.8) | 538 (26.4) | 124 (8.3) | 114 (7.6) | 101 (6.7) | 339 (22.6) | 97 (41.8) | 47 (43.9) | 49 (24.6) | 193 (35.9) |
| Marital status | ||||||||||||||
| Married | 128 | 114 (89.1) | 6 (4.7) | 2 (1.6) | 6 (4.7) | 14 (10.9) | 6 (5.3) | 10 (8.8) | 7 (6.1) | 23 (20.2) | 0 (0) | 1 (50.0) | 3 (50.0) | 4 (28.6) |
| Never married | 252 | 206 (81.7) | 20 (7.9) | 10 (4.0) | 16 (6.3) | 46 (18.3) | 12 (5.8) | 12 (5.8) | 18 (8.7) | 42 (20.4) | 8 (40.0) | 4 (40.0) | 5 (31.3) | 17 (37.0) |
| Divorced or unmarried | 3070 | 2247 (73.2) | 257 (8.4) | 197 (6.4) | 369 (12.0) | 823 (26.8) | 158 (7.0) | 149 (6.6) | 191 (8.5) | 498 (22.2) | 105 (40.9) | 82 (41.6) | 90 (24.4) | 277 (33.7) |
| Widowed | 4019 | 2816 (70.1) | 421 (10.5) | 266 (6.6) | 516 (12.8) | 1203 (29.9) | 228 (8.1) | 238 (8.5) | 257 (9.1) | 723 (25.7) | 172 (40.9) | 131 (49.2) | 135 (26.2) | 438 (36.4) |
| Number of children born | ||||||||||||||
| 0 | 171 | 124 (72.5) | 14 (8.2) | 12 (7.0) | 21 (12.3) | 47 (27.5) | 3 (2.4) | 5 (4.0) | 4 (3.2) | 12 (9.7) | 3 (21.4) | 0 (0) | 5 (23.8) | 8 (17.0) |
| 1 | 345 | 268 (77.7) | 35 (10.1) | 15 (4.3) | 27 (7.8) | 77 (22.3) | 14 (5.2) | 22 (8.2) | 19 (7.1) | 55 (20.5) | 11 (31.4) | 6 (40.0) | 8 (29.6) | 25 (32.5) |
| 2 or more | 6807 | 4876 (71.6) | 647 (9.5) | 440 (6.5) | 844 (12.4) | 1931 (28.4) | 380 (7.8) | 377 (7.7) | 440 (9.0) | 1197 (24.5) | 264 (40.8) | 206 (46.8) | 218 (25.8) | 688 (35.6) |
| Type of residence | ||||||||||||||
| Urban | 6402 | 4622 (72.2) | 626 (9.8) | 393 (6.1) | 761 (11.9) | 1780 (27.8) | 328 (7.1) | 354 (7.7) | 387 (8.4) | 1069 (23.1) | 244 (39.0) | 164 (41.7) | 185 (24.3) | 593 (33.3) |
| Rural | 1381 | 1006 (72.8) | 105 (7.6) | 95 (6.9) | 175 (12.7) | 375 (27.2) | 77 (7.7) | 55 (5.5) | 86 (8.5) | 218 (21.7) | 42 (40.0) | 54 (56.8) | 49 (28.0) | 145 (38.7) |
| Health, anthropomorphic and functional variables | ||||||||||||||
| Self-perception of health status | ||||||||||||||
| Very good - good | 2474 | 2028 (82.0) | 178 (7.2) | 111 (4.5) | 157 (6.3) | 446 (18.0) | 124 (6.1) | 118 (5.8) | 130 (6.4) | 372 (18.3) | 71 (39.9) | 51 (45.9) | 47 (29.9) | 169 (37.9) |
| Fair | 4183 | 2936 (70.2) | 438 (10.5) | 274 (6.6) | 535 (12.8) | 1247 (29.8) | 228 (7.8) | 238 (8.1) | 257 (8.8) | 723 (24.6) | 172 (39.3) | 131 (47.8) | 136 (25.4) | 439 (35.2) |
| Very bad - bad | 1125 | 663 (58.9) | 115 (10.2) | 103 (9.2) | 244 (21.7) | 462 (41.1) | 52 (7.8) | 53 (8.0) | 86 (13.0) | 191 (28.8) | 43 (37.4) | 36 (35.0) | 51 (20.9) | 130 (28.1) |
| Depressive symptoms | ||||||||||||||
| No | 3766 | 3012 (80.0) | 322 (8.6) | 182 (4.8) | 250 (6.6) | 754 (20.0) | 185 (6.1) | 196 (6.5) | 196 (6.5) | 577 (19.2) | 124 (38.5) | 91 (50.0) | 70 (28.0) | 285 (37.8) |
| Yes | 4017 | 2616 (65.1) | 409 (10.2) | 306 (7.6) | 686 (17.1) | 1401 (34.9) | 220 (8.4) | 213 (8.1) | 277 (10.6) | 710 (27.1) | 162 (39.6) | 127 (41.5) | 164 (23.9) | 453 (32.3) |
| Number of self-reported illnesses | ||||||||||||||
| 0 | 2545 | 2048 (80.5) | 204 (8.0) | 106 (4.2) | 187 (7.3) | 497 (19.5) | 131 (6.4) | 110 (5.4) | 115 (5.6) | 356 (17.4) | 88 (43.1) | 57 (53.8) | 61 (32.6) | 206 (41.4) |
| 1 | 2881 | 2111 (73.3) | 278 (9.6) | 174 (6.0) | 318 (11.0) | 770 (26.7) | 170 (8.1) | 144 (6.8) | 177 (8.4) | 491 (23.3) | 108 (38.8) | 82 (47.1) | 78 (24.5) | 268 (34.8) |
| 2 | 1742 | 1110 (63.7) | 193 (11.1) | 151 (8.7) | 288 (16.5) | 632 (36.3) | 79 (7.1) | 109 (9.8) | 133 (12.0) | 321 (28.9) | 66 (34.2) | 55 (36.4) | 65 (22.6) | 186 (29.4) |
| 3 or more | 615 | 359 (58.4) | 56 (9.1) | 57 (9.3) | 143 (23.3) | 256 (41.6) | 25 (7.0) | 46 (12.8) | 48 (13.4) | 119 (33.1) | 24 (42.9) | 24 (42.1) | 30 (21.0) | 78 (30.5) |
| Falls in the last 2 years | ||||||||||||||
| No | 4227 | 3241 (76.7) | 361 (8.5) | 226 (5.3) | 399 (9.4) | 986 (23.3) | 225 (6.9) | 203 (6.3) | 234 (7.2) | 662 (20.4) | 149 (41.3) | 117 (51.8) | 100 (25.1) | 366 (37.1) |
| Yes | 3536 | 2372 (67.1) | 368 (10.4) | 261 (7.4) | 535 (15.1) | 1164 (32.9) | 179 (7.5) | 205 (8.6) | 237 (10.0) | 621 (26.2) | 136 (37.0) | 101 (38.7) | 134 (25.0) | 371 (31.9) |
| Body mass index (BMI) (kg/m2) | ||||||||||||||
| < 25 | 2066 | 1578 (76.4) | 172 (8.3) | 116 (5.6) | 200 (9.7) | 488 (23.6) | 107 (6.8) | 103 (6.5) | 107 (6.8) | 317 (20.1) | 79 (45.9) | 46 (39.7) | 43 (21.5) | 168 (34.4) |
| ≥ 25 to < 30 | 2550 | 1846 (72.4) | 257 (10.1) | 149 (5.8) | 298 (11.7) | 704 (27.6) | 130 (7.0) | 138 (7.5) | 156 (8.5) | 424 (23.0) | 100 (38.9) | 64 (43.0) | 80 (26.8) | 244 (34.7) |
| ≥ 30 | 3167 | 2204 (69.6) | 302 (9.5) | 223 (7.0) | 438 (13.8) | 963 (30.4) | 168 (7.6) | 168 (7.6) | 210 (9.5) | 546 (24.8) | 107 (35.4) | 108 (48.4) | 111 (25.3) | 326 (33.9) |
| Basic activities of daily living (BADL) | ||||||||||||||
| 0 | 6614 | 4972 (75.2) | 608 (9.2) | 376 (5.7) | 658 (9.9) | 1642 (24.8) | 363 (7.3) | 347 (7.0) | 394 (7.9) | 1104 (22.2) | 240 (39.5) | 187 (49.7) | 183 (27.8) | 610 (37.1) |
| 1 | 661 | 383 (57.9) | 73 (11.0) | 48 (7.3) | 157 (23.8) | 278 (42.1) | 25 (6.5) | 37 (9.7) | 45 (11.7) | 107 (27.9) | 31 (42.5) | 15 (31.3) | 31 (19.7) | 77 (27.7) |
| 2 or more | 508 | 273 (53.7) | 50 (9.8) | 64 (12.6) | 121 (23.8) | 235 (46.3) | 17 (6.2) | 25 (9.2) | 34 (12.5) | 76 (27.8) | 15 (30.0) | 16 (25.0) | 20 (16.5) | 51 (21.7) |
| Instrumental activities of daily living (IADL) | ||||||||||||||
| 0 | 6790 | 5048 (74.3) | 631 (9.3) | 404 (5.9) | 707 (10.4) | 1742 (25.7) | 368 (7.3) | 359 (7.1) | 409 (8.1) | 1136 (22.5) | 252 (39.9) | 189 (46.8) | 192 (27.2) | 633 (36.3) |
| 1 | 620 | 376 (60.6) | 63 (10.2) | 47 (7.6) | 134 (21.6) | 244 (39.4) | 29 (7.7) | 35 (9.3) | 43 (11.4) | 107 (28.5) | 28 (44.4) | 21 (44.7) | 21 (15.7) | 70 (28.7) |
| 2 or more | 373 | 204 (54.7) | 37 (9.9) | 37 (9.9) | 95 (25.5) | 169 (45.3) | 8 (3.9) | 15 (7.4) | 21 (10.3) | 44 (21.6) | 6 (16.2) | 8 (21.6) | 21 (22.1) | 35 (20.7) |
TABLE 2.
Urinary incontinence prevalence, incidence and remission in men by UI subtype
| Variables | Total population (100%) | Prevalence, 2012 | Incidence (2012–2015) | Remission (2012–2015) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||||||||||||
| Without UI | SUI | UUI | MUI | Total UI | SUI | UUI | MUI | Total UI | SUI | UUI | MUI | Total UI | ||
| Total | 5843 | 5133 (87.8) | 141 (2.4) | 317 (5.4) | 272 (4.7) | 730 (12.5) | 107 (2.1) | 336 (6.6) | 187 (3.7) | 630 (12.3) | 76 (53.9) | 154 (48.6) | 96 (35.3) | 326 (44.7) |
| Sociodemographic variables | ||||||||||||||
| Age | ||||||||||||||
| 50–59 | 1679 | 1564 (93.2) | 23 (1.4) | 64 (3.8) | 28 (1.7) | 115 (6.8) | 19 (1.2) | 64 (4.1) | 34 (2.2) | 117 (7.5) | 16 (69.6) | 39 (60.9) | 13 (46.4) | 68 (59.1) |
| 60–69 | 2324 | 2047 (88.1) | 58 (2.5) | 133 (5.7) | 86 (3.7) | 277 (11.9) | 49 (2.4) | 134 (6.5) | 63 (3.1) | 246 (12.0) | 34 (58.6) | 71 (53.4) | 44 (51.2) | 149 (53.8) |
| 70–79 | 1323 | 1112 (84.1) | 45 (3.4) | 83 (6.3) | 83 (6.3) | 211 (15.9) | 25 (2.2) | 105 (9.4) | 64 (5.8) | 194 (17.4) | 18 (40.0) | 34 (41.0) | 23 (27.7) | 75 (35.5) |
| 90+ | 61 | 45 (73.8) | 2 (3.3) | 3 (4.9) | 11 (18.0) | 16 (26.2) | 1 (2.2) | 4 (8.9) | 2 (4.4) | 7 (15.6) | 1 (50.0) | 1 (33.3) | 2 (18.2) | 4 (25.0) |
| 80–89 | 456 | 345 (75.7) | 13 (2.9) | 34 (7.5) | 64 14.0) | 111 (24.3) | 13 (3.8) | 29 (8.4) | 24 (7.0) | 66 (19.1) | 7 (53.8) | 9 (26.5) | 14 (21.9) | 30 (27.0) |
| Educational level | ||||||||||||||
| < 6 y | 2273 | 1935 (85.1) | 73 (3.2) | 135 (5.9) | 130 (5.7) | 338 (14.9) | 65 (3.4) | 160 (8.3) | 116 (6.0) | 341 (17.6) | 46 (63.0) | 70 (51.9) | 57 (43.8) | 173 (51.2) |
| 6 y | 1125 | 1017 (90.4) | 21 (1.9) | 50 (4.4) | 37 (3.3) | 108 (9.6) | 21 (2.1) | 74 (7.3) | 35 (3.4) | 130 (12.8) | 14 (66.7) | 26 (52.0) | 17 (45.9) | 57 (52.8) |
| > 6 y | 1828 | 1675 (91.6) | 23 (1.3) | 90 (4.9) | 40 (2.2) | 153 (8.4) | 21 (1.3) | 102 (6.1) | 36 (2.1) | 159 (9.5) | 16 (69.6) | 58 (64.4) | 22 (55.0) | 96 (612.7) |
| Marital status | ||||||||||||||
| Married | 182 | 170 (93.4) | 2 (1.1) | 8 (4.4) | 2 (1.1) | 12 (6.6) | 1 (0.6) | 6 (3.5) | 4 (2.4) | 11 (6.5) | 2 (100) | 5 (62.5) | 2 (100) | 9 (75.0) |
| Never married | 302 | 277 (91.7) | 4 (1.3) | 15 (5.0) | 6 (2.0) | 25 (8.3) | 8 (2.9) | 17 (6.1) | 3 (1.1) | 28 (10.1) | 2 (50.0) | 8 (53.3) | 2 (33.3) | 12 (48.0) |
| Divorced or unmarried | 2367 | 2071 (87.5) | 60 (2.5) | 107 (4.5) | 129 (5.4) | 296 (12.5) | 41 (2.0) | 127 (6.1) | 66 (3.2) | 234 (11.3) | 39 (65.0) | 48 (44.9) | 42 (32.6) | 129 (43.6) |
| Widowed | 2621 | 2248 (85.8) | 69 (2.6) | 176 (6.7) | 128 (4.9) | 373 (14.2) | 57 (2.5) | 186 (8.3) | 114 (5.1) | 357 (15.9) | 33 (47.8) | 93 (52.8) | 50 (39.1) | 176 (47.2) |
| Type of Residence | ||||||||||||||
| Urban | 4626 | 4064 (87.9) | 113 (2.4) | 251 (5.4) | 198 (4.3) | 562 (12.1) | 67 (1.6) | 277 (6.8) | 142 (3.5) | 486 (12.0) | 62 (54.9) | 123 (49.0) | 76 (38.4) | 261 (46.4) |
| Rural | 1217 | 1049 (86.2) | 28 (2.3) | 66 (5.4) | 74 (6.1) | 168 (13.8) | 40 (3.8) | 59 (5.6) | 45 (4.3) | 144 (13.7) | 14 (50.0) | 31 (47.0) | 20 (27.0) | 65 (38.7) |
| Health, anthropomorphic, and functional variables | ||||||||||||||
| Self-perception of health status | ||||||||||||||
| Very good - good | 2435 | 2261 (92.9) | 38 (1.6) | 81 (3.3) | 55 (2.3) | 174 (7.1) | 35 (1.5) | 108 (4.8) | 41 (1.8) | 184 (8.1) | 28 (73.7) | 44 (54.3) | 23 (41.8) | 95 (54.6) |
| Fair | 2760 | 2373 (86.0) | 72 (2.6) | 183 (6.6) | 132 (4.8) | 387 (14.0) | 57 (2.4) | 186 (7.8) | 114 (4.8) | 357 (15.0) | 33 (45.8) | 93 (50.8) | 50 (37.9) | 176 (45.5) |
| Very bad - bad | 646 | 478 (74.0) | 31 (4.8) | 53 (8.2) | 84 (13.0) | 168 (26.0) | 15 (3.1) | 42 (8.8) | 32 (6.7) | 89 (18.6) | 15 (48.4) | 17 (32.1) | 23 (27.4) | 55 (37.2) |
| Depressive symptoms | ||||||||||||||
| No | 3800 | 3485 (91.7) | 60 (1.6) | 162 (4.3) | 93 (2.4) | 315 (8.3) | 67 (1.9) | 217 (6.2) | 95 (2.7) | 379 (10.9) | 32 (53.3) | 81 (50.0) | 39 (41.9) | 152 (48.3) |
| Yes | 2043 | 1628 (79.7) | 81 (4.0) | 155 (7.6) | 179 (8.8) | 415 (20.3) | 40 (2.5) | 119 (7.3) | 92 (5.7) | 251 (15.4) | 44 (54.3) | 73 (47.1) | 57 (31.8) | 174 (41.9) |
| Number of self-reported illnesses | ||||||||||||||
| 0 | 2785 | 2540 (91.2) | 46 (1.7) | 114 (4.1) | 85 (3.1) | 245 (8.8) | 40 (1.6) | 131 (5.2) | 65 (2.6) | 236 (9.3) | 28 (60.9) | 59 (51.8) | 32 (37.6) | 119 (48.6) |
| 1 | 1876 | 1634 (87.1) | 52 (2.8) | 112 (6.0) | 78 (4.2) | 242 (12.9) | 37 (2.3) | 130 (8.0) | 66 (4.0) | 233 (14.3) | 30 (57.7) | 59 (52.7) | 35 (44.9) | 124 (52.1) |
| 2 | 906 | 731 (80.7) | 32 (3.5) | 65 (7.2) | 78 (8.6) | 175 (19.3) | 22 (3.0) | 59 (8.1) | 38 (5.2) | 119 (16.3) | 16 (50.0) | 24 (36.9) | 22 (28.2) | 62 (35.4) |
| 3 or more | 276 | 208 (75.4) | 11 (4.0) | 26 (9.4) | 31 (11.2) | 68 (24.6) | 8 (3.8) | 16 (7.7) | 18 (8.7) | 42 (20.2) | 2 (18.2) | 12 (46.2) | 7 (22.6) | 21 (30.9) |
| Falls in the last 2 years | ||||||||||||||
| No | 4025 | 3622 (90.0) | 75 (1.9) | 191 (4.7) | 137 (3.4) | 403 (10.0) | 65 (1.8) | 216 (6.0) | 105 (2.9) | 386 (10.7) | 42 (56.0) | 91 (47.6) | 57 (41.6) | 190 (47.1) |
| Yes | 1805 | 1480 (82.0) | 66 (3.7) | 125 (6.9) | 134 (7.4) | 325 (18.0) | 42 (2.8) | 120 (8.1) | 80 (5.4) | 242 (16.4) | 34 (51.5) | 62 (49.6) | 39 (29.1) | 135 (41.5) |
| Body mass index (BMI) (kg/m2) | ||||||||||||||
| < 25 | 1859 | 1624 (87.4) | 43 (2.3) | 102 (5.5) | 90 (4.8) | 235 (12.6) | 37 (2.3) | 92 (5.7) | 65 (4.0) | 194 (11.9) | 19 (44.2) | 51 (50.0) | 30 (33.3) | 100 (42.6) |
| ≥ 25 to < 30 | 2444 | 2163 (88.5) | 55 (2.3) | 123 (5.0) | 103 (4.2) | 281 (11.5) | 46 (2.1) | 149 (6.9) | 62 (2.9) | 257 (11.9) | 31 (56.4) | 56 (45.5) | 41 (39.8) | 128 (45.6) |
| ≥ 30 | 1540 | 1326 (86.1) | 43 (2.8) | 92 (6.0) | 79 (5.1) | 214 (13.9) | 24 (1.8) | 95 (7.2) | 60 (4.5) | 179 (13.5) | 26 (60.5) | 47 (51.1) | 25 (31.6) | 98 (45.8) |
| Basic activities of daily living (BADL) | ||||||||||||||
| 0 | 5315 | 4761 (89.6) | 115 (2.2) | 257 (4.8) | 182 (3.4) | 554 (10.4) | 97 (2.0) | 315 (6.6) | 152 (3.2) | 564 (11.8) | 63 (54.8) | 131 (51.0) | 72 (39.6) | 266 (48.0) |
| 1 | 289 | 210 (72.7) | 11 (3.8) | 31 (10.7) | 37 (12.8) | 79 (27.3) | 6 (2.9) | 15 (7.1) | 19 (9.0) | 40 (19.0) | 7 (63.6) | 13 (41.9) | 10 (27.0) | 30 (38.0) |
| 2 or more | 239 | 142 (59.4) | 15 (6.3) | 29 (12.1) | 53 (22.2) | 97 (40.6) | 4 (2.8) | 6 (4.2) | 16 (11.3) | 26 (18.3) | 6 (40.0) | 10 (34.5) | 14 (26.4) | 30 (30.9) |
| Instrumental activities of daily living (IADL) | ||||||||||||||
| 0 | 5395 | 4817 (89.3) | 116 (2.2) | 258 (4.8) | 204 (3.8) | 578 (10.7) | 100 (2.1) | 318 (6.6) | 167 (3.5) | 585 (12.1) | 65 (56.0) | 133 (51.6) | 83 (40.7) | 281 (48.6) |
| 1 | 247 | 174 (70.4) | 15 (6.1) | 37 (15.0) | 21 (8.5) | 73 (29.6) | 4 (2.3) | 12 (6.9) | 12 (6.9) | 28 (16.1) | 7 (46.7) | 17 (45.9) | 5 (23.8) | 29 (39.7) |
| 2 or more | 201 | 122 (60.7) | 10 (5.0) | 22 (10.9) | 47 (23.4) | 79 (39.3) | 3 (2.5) | 6 (4.9) | 8 (6.6) | 17 (13.9) | 4 (40.0) | 4 (18.2) | 8 (17.0) | 16 (20.3) |
The cumulative incidence of UI was 22.9% in women, and 12.3% in men and increased with age for both. With regard to UI subtype, MUI had the highest incidence in women (8.4%), as did UUI in men (6.6%). As our descriptive analyses show, the UI incidence for both increased when respondents reported advanced age, a negative self-perception of health status, the presence of depressive symptoms, a higher number of illnesses, a history of falls in the last 2 years, and a higher number of limitations in BADL and IADL (Tables 1,2).
The UI remission rate for women was 34.2% and 44.7% for men; this rate decreased with age for both sexes. SUI was the UI subtype that showed the highest remission rates among men (53.9%); as was UUI among women (44.7%). For both sexes, UI remission was higher among adults of a younger age who did not report having other illnesses and did not report having limitations in their BADL and IADL (Tables 1,2).
Between 2012 and 2015, a higher proportion of men (71.5%) reported no UI symptoms when compared with women (62.8%). For both sexes, and for both SUI and UUI subtypes, remission was the most frequent change experienced. However, 19.7% of women with UUI advanced to MUI, and 16.5% of men who had MUI in 2012 had died by 2015 (Table 3).
TABLE 3.
Transitions of urinary incontinence and its subtypes over a two-year period
| UI status in 2015 n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Sex | UI status in 2012 | Without UI | SUI | UUI | MUI | Deceased | No answer |
| Women | Without UI | 3536 (62.8) | 405 (7.2) | 409 (7.3) | 473 (8.4) | 258 (4.6) | 547 (9.7) |
| SUI | 286 (39.1) | 191 (26.1) | 46 (6.3) | 121 (16.6) | 31 (4.2) | 56 (7.7) | |
| UUI | 218 (44.7) | 37 (7.6) | 64 (13.1) | 96 (19.7) | 40 (8.2) | 33 (6.8) | |
| MUI | 234 (25.0) | 111 (11.9) | 94 (10.0) | 349 (37.3) | 69 (7.4) | 79 (8.4) | |
| Men | Without UI | 3655 (71.5) | 107 (2.1) | 336 (6.6) | 187 (3.7) | 321 (6.3) | 507 (9.9) |
| SUI | 76 (53.9) | 10 (7.1) | 14 (9.9) | 11 (7.8) | 14 (9.9) | 16 (11.3) | |
| UUI | 154 (48.6) | 8 (2.5) | 67 (21.1) | 35 (11.0) | 27 (8.5) | 26 (8.2) | |
| MUI | 96 (35.3) | 12 (4.4) | 33 (12.1) | 59 (21.7) | 45 (16.5) | 27 (9.9) | |
Results from the longitudinal regressions showed that when looking into predictive factors for the incidence of UI by sex. The presence of depressive symptoms, a higher number of illnesses, and a history of falls in the last 2 years were all predictive factors for UI incidence in women. Also, in women, depressive symptoms were a predictor for SUI and MUI; having two, three or more illnesses predicted UUI and MUI; and a history of falls in the last 2 years predicted UUI and MUI. For men, the predictive factors for UI were advanced age, the presence of depressive symptoms, a higher number of illnesses and limitations in their BADL. Specifically, the likelihood of having any UI subtype increased with age; the presence of depressive symptoms was a predictor of MUI; having two, three or more illnesses were a predictor of SUI and MUI; while having limitations in their BADL was a predictor of MUI (Table 4).
TABLE 4.
Predictors of urinary incontinence incidence in 2015
| Predictive factors of incontinence in 2015 | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| UI Total OR (CI, 95%) |
SUI OR (CI, 95%) |
UUI OR (CI, 95%) |
MUI OR (CI, 95%) |
UI Total OR (CI, 95%) |
SUI OR (CI, 95%) |
UUI OR (CI, 95%) |
MUI OR (CI, 95%) |
|
| Age group (reference: 50–59) | ||||||||
| 60–69 | 1.16 (0.99–1.35) | 0.89 (0.70–1.13) | 1.45 (1.12–1.88)** | 1.22 (0.97–1.55) | 1.48 (1.17–1.87)* | 1.78 (1.04–3.06)*** | 1.52 (1.11–2.07)* | 1.23 (0.80–1.89) |
| 70–79 | 1.32 (1.09–1.58)** | 0.87 (0.65–1.18) | 1.93 (1.44–2.58)* | 1.34 (1.01–1.77)*** | 2.37 (1.84–3.05)* | 1.89 (1.03–3.48)*** | 2.45 (1.76–3.40)* | 2.45 (1.58–3.80)* |
| 80–89 | 1.09 (0.80–1.48) | 0.70 (0.41–1.19) | 1.20 (0.72–2.00) | 1.40 (0.91–2.14) | 3.41 (2.40–4.85)* | 4.08 (1.94–8.54)* | 2.93 (1.82–4.72)* | 3.93 (2.23–6.92)* |
| 90 and older | 2.45 (0.89–6.72) | 1.72 (0.36–8.18) | 1.32 (0.16–10.60) | 4.56 (1.36–15.28)*** | 4.65 (1.82–11.91)** | 4.42 (0.55–35.70) | 5.05 (1.60–15.93)* | 4.33 (0.92–20.40) |
| Depressive symptoms (reference: no) | 1.42 (1.24–1.63)* | 1.50 (1.19–1.83)* | 1.23 (0.99–1.52) | 1.57 (1.28–1.92)* | 1.30 (1.08–1.56)** | 1.18 (0.78–1.78) | 1.13 (0.89–1.44) | 1.74 (1.27–2.37)* |
| Number of self-reported illnesses (reference: none) | ||||||||
| 1 | 1.30 (1.11–1.53)** | 1.31 (1.03–1.67)*** | 1.21 (0.93–1.57) | 1.43 (1.11–1.83)* | 1.43 (1.17–1.74)* | 1.35 (0.85–2.13) | 1.46 (1.13–1.88)** | 1.37 (0.96–1.97) |
| 2 | 1.68 (1.40–2.03)* | 1.25 (0.92–1.69) | 1.80 (1.35–2.42)* | 2.02 (1.53–2.68)* | 1.77 (1.38–2.28)* | 1.99 (1.16–3.43)** | 1.73 (1.24–2.40)** | 1.74 (1.13–2.69)** |
| 3 or more | 2.08 (1.58–2.73)* | 1.37 (0.86–2.19) | 2.44 (1.64–3.63)* | 2.44 (1.66–3.60)* | 2.20 (1.47–3.27)* | 2.54 (1.12–5.76)** | 1.75 (0.99–3.09) | 2.65 (1.46–4.83)** |
| Falls in the last 2 years (reference: no) | 1.22 (1.06–1.39)** | 1.12 (0.90–1.39) | 1.30 (1.05–1.61)*** | 1.27 (1.04–1.55)*** | 1.42 (1.18–1.71)* | 1.49 (1.00–2.24) | 1.34 (1.05–1.70)** | 1.56 (1.14–2.14)** |
| Basic activities of daily living (BADL) (reference: none) | ||||||||
| 1 | 1.24 (0.96–1.61) | 1.01 (0.64–1.58) | 1.35 (0.91–2.00) | 1.37 (0.95–1.97) | 1.42 (0.96–2.09) | 1.08 (0.44–2.65) | 1.00 (0.57–1.75) | 2.34 (1.36–4.04)** |
| 2 or more | 1.43 (1.00–2.04)*** | 1.25 (0.68–2.28) | 1.50 (0.89–2.53) | 1.53 (0.95–2.47) | 1.37 (0.82–2.29) | 1.04 (0.33–3.32) | 0.61 (0.25–1.50) | 2.60 (1.35–4.99)** |
| Instrumental activities of daily living (IADL) (reference: none) | ||||||||
| 1 | 1.06 (0.81–1.38) | 1.10 (0.71–1.71) | 1.00 (0.66–1.51) | 1.05 (0.72–1.53) | 1.14 (0.72–1.80) | 1.07 (0.37–3.08) | 1.07 (0.57–2.03) | 1.26 (0.65–2.46) |
| 2 or more | 1.12 (0.72–1.75) | 0.87 (0.38–1.99) | 1.14 (0.59–2.19) | 1.30 (0.72–2.33) | 1.00 (0.54–1.85) | 1.13 (0.30–4.32) | 1.01 (0.40–2.57) | 0.93 (0.39–2.22) |
< .001.
< .005.
< .05.
4 |. DISCUSSION
Our results are in line with previous studies where the prevalence of UI and its subtypes is higher in women.2,12,13 And as previous research our results also show that for both sexes, prevalence increases with age, except for SUI among women. With regard to UI subtypes, we found a higher prevalence of MUI in women aged 60 and older and in men aged 80 and older. In men aged 80 to 89, the prevalence of MUI doubled the prevalence of UUI; and this increased in men 90 and older where the prevalence of MUI tripled that of UUI.
Previous studies suggest that the increasing prevalence of MUI with age is a result of having UUI (which can be induced by a stressor) as a preliminary stage that can progress to MUI; it has been shown that the prolonged presence of one type of UI increases the risk for the incidence of another type.14 For men, this can be related to prostate conditions.12 Research also suggests that MUI is the dominant UI subtype among women of advanced age,7,15 while SUI is more common among younger women with previous pelvic floor trauma and uterine prolapse related to vaginal birth.15 As our results suggest, previous studies show that UUI is the most prevalent UI subtype among older men, followed by MUI and then by SUI.12,16
With regard to the incidence of UI and its subtypes in women, findings of our analysis suggest a higher incidence when compared with previous research.2,17 This could be due to the definitions employed, the way that questions were asked of participants, and the selected sample population involved. For example, results from the HRS, a longitudinal study of older adults from the United States, reported a two-year incidence of UI in community-dwelling women aged 50 between 11.8% and 13.3%. However, even if the same questions were included in MHAS and HRS, the HRS added two filter questions before asking about SUI and UUI. The first was if women had UI symptoms in the 12 months before the baseline and the second was how many days in the past month. If respondents had a negative answer they did not ask about SUI and UUI.2 This could explain the difference in findings. For men, there are few studies focusing in UI incidence. However, the results of our study are consistent with other studies; UI incidence in men increases with age and is almost half when compared with UI incidence in women.18
Our results showed higher UI remission rates in men when compared to women, in line with what has been observed in other populations.13 In both men and women, the lowest remission rate was for MUI. Previous studies suggest that owing to the clinical complexity of MUI, this remission would be the least probable when compared to SUI or UUI.15 In men, the highest remission rates were in those participants with SUI, followed by those with UUI. In women, UUI had the highest remission rates. This is explained by its predisposing conditions, such as urinary tract infections and intestinal dysfunction which are both highly susceptible to improvement, with or without treatment.13
One of our findings suggest that MUI can be an important prognostic factor for mortality in men, as 16.5% of those men who had symptoms of MUI in 2012 had died by 2015. A systematic review published in 2016 found that UI is a predictor of mortality, primarily for men, although it is not clear whether this is a causal relationship or if UI may simply reflect generally deteriorated health.19 With regard to predisposing factors for UI. In this study, age, the presence of depressive symptoms, the number of concomitant diseases, a history of falls, and limitations in BADL were all predictors of the incidence of UI and its subtypes.
Age was a predictor of UI and its subtypes, particularly among men, which can be attributed to the development of urethral sphincter dysfunction associated with older ages.20 Depressive symptoms were also a significant risk factor for UI, as well as for SUI and MUI among women and for MUI among men.21 It has been suggested that changes in the levels of the neurotransmitter serotonin which characterize depressive states are favorable to UI because serotonin is involved in vesicle function as well as the operation of the urethral sphincter.22,23 It has also been proposed that the autonomous nervous system dysfunction associated with depression increases the levels of circulating cortisol and catecholamines, inducing physiological changes to the urethral sphincter.22
Higher number of concomitant illnesses has also been previously associated with a higher likelihood of developing UI in both sexes,17 as was shown in our study. One recent study of older adults in the United States reported that only 11% of women with UI did not have other conditions, and women with more chronic conditions reported a higher incidence of MUI, as well as more severe symptoms.24 Other studies have documented the association of a history of falls with UI.3,9 A study using this same data set (MHAS) reported that UI is strongly associated with falls, especially recurrent falls.23 Finally, the presence of two or more limitations in BADL predicted only UI in women and MUI in men. These findings contrast with those observed by Komesu et al, who found that having two or more limitations in BADL is a predictor of UUI and MUI in older women.2
4.1 |. Strengths and limitations
Our study has some limitations that should be considered. First, because of the limited access to medical care in Mexico the use of self-reported UI and other chronic conditions may produce underestimations.25 Second, the survey does not offer information regarding the quantity of urine leaked or the severity of UI symptoms. Third, the data on remission does not include information on medical or surgical interventions, so it is not possible to conclude whether the remissions occurred naturally or were a result of treatment. The strengths of our study are first, the strong representativeness of Mexican adults aged 50 and older, and its prospective design which permitted the establishment of relationships between UI and the predictive variables. The study also offers information about the incidence and remission of UI and its subtypes, indicators which reveal key aspects about the dynamic of the illness. The findings regarding the behavior of this health problem among men are particularly useful, as there are few such studies in this area.12
5 |. CONCLUSIONS
This is the first Mexican longitudinal study that presents evidence on the epidemiology, progression, and predictive factors of UI and its subtypes, using a national, representative sample of men and women aged 50 and older who live at home rather than in a hospital or institution. Information from this study can be used to guide medical attention and properly shape interventions for UI for older adults. As this study shows, UI is a frequent health problem that increases and becomes more severe with age. Modifiable UI risk factors, such as depression and falls, require increased attention, which would result in a decrease in the prevalence and incidence of UI and its subtypes. More research is required into the relationship between mixed urinary incontinence and mortality in men. It is recommended that medical professionals routinely inquire about UI symptoms to their older patients, offering them guidelines and treatment options for managing this illness according to each patient’s characteristics and needs.
Footnotes
ETHICAL CONSIDERATIONS
The MHAS study was approved by the Ethics Committee at the University of Texas Medical Branch (UTMB), the National Institute of Statistics and Geography (Instituto Nacional de Estadística y Geografía; INEGI) and the National Institute of Public Health (Instituto Nacional de Salud Pública; INSP). Oral consent was obtained from all participants, in accordance with the ethical principles for medical research involving human subjects as established in the Declaration of Helsinki.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
REFERENCES
- 1.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–178. [DOI] [PubMed] [Google Scholar]
- 2.Komesu YM, Schrader RM, Ketai LH, Rogers RG, Dunivan GC. Epidemiology of mixed, stress, and urgency urinary incontinence in middle-aged/older women: the importance of incontinence history. Int Urogynecol J. 2016;27(5):763–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiarelli PE, Mackenzie LA, Osmotherly PG. Urinary incontinence is associated with an increase in falls: a systematic review. Aust J Physiother. 2009;55(2):89–95. [DOI] [PubMed] [Google Scholar]
- 4.Ostaszkiewicz J. A conceptual model of the risk of elder abuse posed by incontinence and care dependence. Int J Older People Nurs. 2018;13(2):e12182. [DOI] [PubMed] [Google Scholar]
- 5.Buckley BS, Lapitan MC. Epidemiology Committee of the Fourth International Consultation on Incontinence. Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265–270. [DOI] [PubMed] [Google Scholar]
- 6.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol. 2009;114(6):1278–1283. [DOI] [PubMed] [Google Scholar]
- 7.Hunskaar S, Burgio K, Diokno A, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence in women. Urology. 2003;62(4 Suppl 1):16–23. [DOI] [PubMed] [Google Scholar]
- 8.Thuroff JW, Abrams P, Andersson KE, et al. EAU guidelines on urinary incontinence. Eur Urol. 2011;59(3):387–400. [DOI] [PubMed] [Google Scholar]
- 9.Foley AL, Loharuka S, Barrett JA, et al. Association between the Geriatric Giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age Ageing. 2012;41(1):35–40. [DOI] [PubMed] [Google Scholar]
- 10.Wong R, Michaels-Obregon A, Palloni A. Cohort profile: The Mexican Health and Aging Study (MHAS). Int J Epidemiol. 2017;46(2):e2–e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monserud MA, Wong R. Depressive symptoms among older Mexicans: the role of widowhood, gender, and social integration. Res Aging. 2015;37(8):856–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diokno AC, Estanol MV, Ibrahim IA, Balasubramaniam M. Prevalence of urinary incontinence in community dwelling men: a cross sectional nationwide epidemiological survey. Int Urol Nephrol. 2007;39(1):129–136. [DOI] [PubMed] [Google Scholar]
- 13.Herzog AR, Diokno AC, Brown MB, Normolle DP, Brock BM. Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol. 1990;45(2):M67–M74. [DOI] [PubMed] [Google Scholar]
- 14.Minassian VA, Yan XS, Pitcavage J, Stewart WF. Mixed incontinence masked as stress induced urgency urinary incontinence. J Urol. 2016;196(4):1190–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minassian VA, Bazi T, Stewart WF. Clinical epidemiological insights into urinary incontinence. Int Urogynecol J. 2017;28(5): 687–696. [DOI] [PubMed] [Google Scholar]
- 16.Tikkinen KA, Agarwal A, Griebling TL. Epidemiology of male urinary incontinence. Curr Opin Urol. 2013;23(6):502–508. [DOI] [PubMed] [Google Scholar]
- 17.Erekson EA, Cong X, Townsend MK, Ciarleglio MM. Ten-year prevalence and incidence of urinary incontinence in older women: a longitudinal analysis of the health and retirement study. J Am Geriatr Soc. 2016;64(6):1274–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ostbye T, Seim A, Krause KM, et al. A 10-year follow-up of urinary and fecal incontinence among the oldest old in the community: the Canadian Study of Health and Aging. Can J Aging. 2004;23(4):319–331. [DOI] [PubMed] [Google Scholar]
- 19.John G, Bardini C, Combescure C, Dallenbach P. Urinary incontinence as a predictor of death: a systematic review and meta-analysis. PLoS One. 2016;11(7):e0158992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Juan Escudero JU, Ramos de Campos M, Ordono Dominguez F, Fabuel Deltoro M, Navalon Verdejo P, Zaragoza Orts J. Radical prostatectomy complications: evolution and conservative management of urinary incontinence. Actas Urol Esp. 2006;30(10):991–997. [DOI] [PubMed] [Google Scholar]
- 21.Morrisroe SN, Rodriguez LV, Wang PC, Smith AL, Trejo L, Sarkisian CA. Correlates of 1-year incidence of urinary incontinence in older Latino adults enrolled in a community-based physical activity trial. J Am Geriatr Soc. 2014;62(4):740–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Melville JL, Fan MY, Rau H, Nygaard IE, Katon WJ. Major depression and urinary incontinence in women: temporal associations in an epidemiologic sample. Am J Obstet Gynecol. 2009;201(5):e491–e497. [DOI] [PubMed] [Google Scholar]
- 23.Agudelo-Botero M, Giraldo-Rodriguez L, Murillo-Gonzalez JC, Mino-Leon D, Cruz-Arenas E. Factors associated with occasional and recurrent falls in Mexican community-dwelling older people. PLoS One. 2018;13(2):e0192926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Markland AD, Vaughan CP, Okosun IS, Goode PS, Burgio KL, Johnson TM 2nd. Cluster analysis of multiple chronic conditions associated with urinary incontinence among women in the USA. BJU Int. 2018;122(6):1041–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Downer B, Chen NW, Wong R, Markides KS. Self-reported health and functional characteristics of Mexican and Mexican American adults aged 80 and over. J Aging Health. 2016;28(7):1239–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]


