Abstract
Background
Pneumonia produced by coinfection with Pneumocystis jirovecii (PJ) and cytomegalovirus (CMV) in infants and young children without timely diagnosis and treatment is often fatal due to the limitations of traditional tests. More accurate and rapid diagnostic methods for multiple infections are urgently needed.
Case Presentation
Here, we report a case of a 2-month-old boy with pneumonia caused by Pneumocystis jirovecii (PJ) and cytomegalovirus (CMV) without HIV infection. Chest computed tomography (CT) showed massive exudative consolidation in both lungs. Microscopic examination of stained sputum and smear specimens and bacterial and fungal culture tests were all negative, and CMV nucleic acid and antibody tests were positive. After a period of antiviral and anti-infective therapy, pulmonary inflammation was not relieved. Subsequently, sputum and venous blood samples were analysed by metagenomic next-generation sequencing (mNGS), and the sequences of PJ and CMV were acquired. The patient was finally diagnosed with pneumonia caused by PJ and CMV coinfection. Anti-fungal combined with anti-viral therapy was given immediately. mNGS re-examination of bronchoalveolar lavage fluid (BALF) also revealed the same primary pathogen. Therapy was stopped due to the request of the patient’s guardian. Hence, the child was discharged from the hospital and eventually died.
Conclusion
This case emphasizes the combined use of mNGS and traditional tests in the clinical diagnosis of mixed lung infections in infants without HIV infection. mNGS is a new adjunctive diagnostic method that can rapidly discriminate multiple causes of pneumonia.
Keywords: metagenomic next-generation sequencing, Pneumocystis jirovecii, cytomegalovirus, pneumonitis, HIV-negative
Background
Pneumocystis jirovecii (PJ) and cytomegalovirus (CMV) are two of the most prevalent opportunistic pathogens causing lung infection in immunocompromised hosts and newborns, especially in premature babies.1–3 It has been shown in clinical research that CMV can be transmitted through breast milk, and almost 90% of newborns are infected asymptomatically via this route during the perinatal period.4 Pneumocystis jirovecii pneumonia (PJP) was quite common in human immunodeficiency virus (HIV)-infected patients in the past. Since the introduction of HAART (highly active antiretroviral therapy) its incidence in this group has decreased, but non-HIV-infected patients are currently the main group at risk.5 In recent years, metagenomic next-generation sequencing (mNGS) has been widely used in the detection of infectious pathogens and is of particular use for the detection of infrequent and emerging pathogens. Moreover, it is more sensitive than traditional methods in the detection of lung infections.6 Here, we report a case of an infant patient with a mixed infection of PJ and CMV detected in sputum, blood, and bronchoalveolar lavage fluid (BALF) by mNGS.
Case Presentation
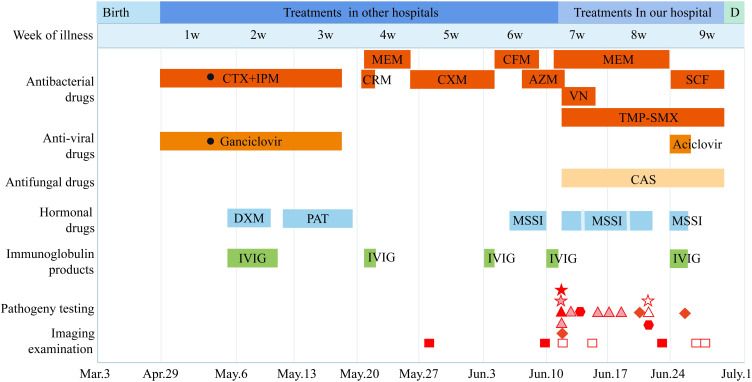
A baby boy was born to nonconsanguineous parents on March 3 with an uneventful birth history. He was the first child of a mother with a history of healthy pregnancy. However, after nearly two months, he developed a fever for no obvious reason. The highest body temperature was 38.4 °C, accompanied by scattered bleeding spots and mild skin yellowing, without coughing and vomiting symptoms. He was sent to two local hospitals for treatment successively. The diagnosis included cholestatic hepatitis, CMV infection, immune thrombocytopenic purpura, acute laryngitis, and hydrocele. The result of serological tests for CMV antibodies IgM and IgG demonstrated positivity for both. The quantitative assessment of CMV nucleic acid levels in the mother’s milk revealed levels of 2.66×104 copies/mL, and in the baby’s urine, the level was 1.83×106 copies/mL by quantitative polymerase chain reaction (qPCR). Bone marrow morphology exhibited three-line hyperplasia with megakaryocytic dysplasia. Immune investigations showed that humoral immunity and B-cell immune functions were barrier-free. The ratio of CD4+ cells/CD8+ cells decreased, while the ratio of CD4− cells/CD8− cells increased. During hospitalization, he was given dexamethasone (DXM), prednisone acetate tablets (PAT), intravenous immunoglobulin (IVIG), cefotaxime (CTX), and imipenem (IPM) for anti-infection treatment and ganciclovir antiviral treatment. The patient was transferred to another hospital for treatment three weeks later and was administered meropenem (MEM), ceftriaxone sodium (CRM), cefuroxime sodium (CXM), cefixime (CFM) and azithromycin (AZM), and ganciclovir injection. The fever subsided on May 28, he developed cough symptoms, and chest computed tomography (CT) showed large exudation of both lungs. A few days later, dyspnoea appeared, and the “three concave sign” was present. After injection of methylprednisolone sodium succinate (MSSI), the symptoms of dyspnoea were not relieved. Re-examination with CT imaging showed large consolidation in both lungs with a small amount of pneumothorax. Acute respiratory distress syndrome (ARDS) was diagnosed, and percutaneous oxygen saturation levels fluctuated between 30–60%. Then, he was transferred to our hospital in a critical condition with the consent of his parents. The main treatment process of the patient before entering our hospital is shown in Figure 1 (part of the detailed information has been lost because the patient’s guardian could not provide it all).
Figure 1.
Timeline of the patient’s clinical manifestations and treatment.
Notes:  : CT;
: CT;  : CR;
: CR;  : blood culture;
: blood culture;  : sputum culture;
: sputum culture;  : BALF culture;
: BALF culture;  : NGS of blood;
: NGS of blood;  : NGS of sputum;
: NGS of sputum;  : NGS of BALF;
: NGS of BALF;  :G test;
:G test;  : CMV test;
: CMV test;  : time is not clear.
: time is not clear.
Abbreviations: D, death; CTX, cefotaxime; IPM, imipenem; DXM, dexamethasone; PAT, prednisone acetate tablets; IVIG, intravenous immunoglobulin; MEM, meropenem; CRM, ceftriaxone sodium; CXM, cefuroxime sodium; CFM, cefixime; AZM, azithromycin; MSSI, methylprednisolone sodium succinate for injection; VN, vancomycin; TMP-SMX, trimethoprim-sulfamethoxazole; CAS, caspofungin; SCF, cefoperazone sodium and sulbactam sodium for injection.
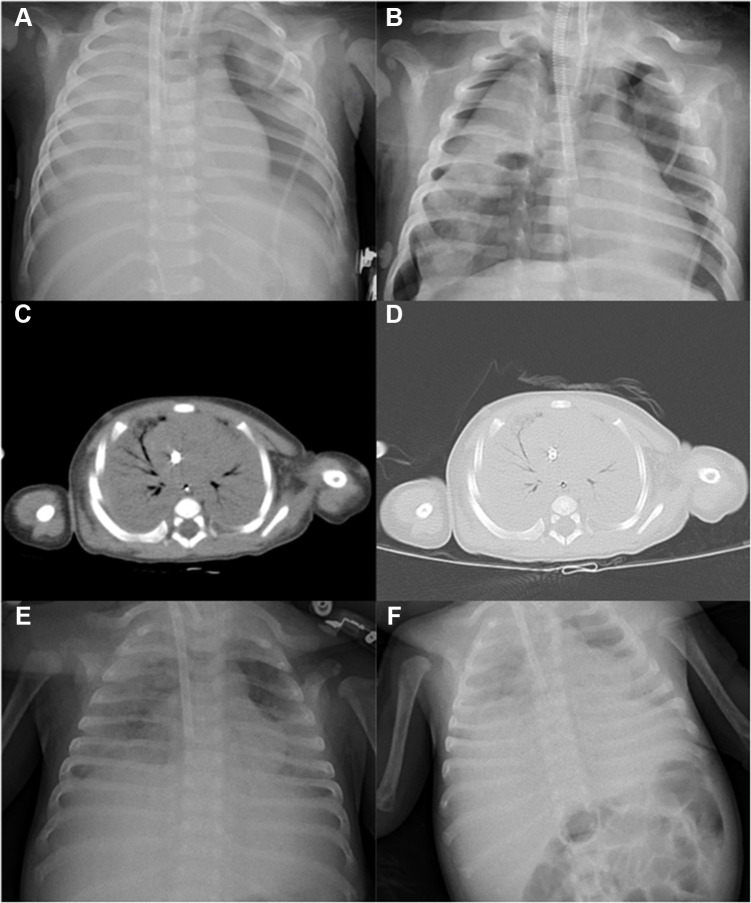
The child had repeated fever for more than one month, coughing for two weeks, and dyspnoea for three days. On June 12, the temperature observed during the physical examination was 35.5°C, the blood pressure was 95/75 mmHg, the pulse was 109 beats per minute, venoarterial extracorporeal membrane oxygenation (VA-ECMO)-assisted mechanical ventilation (inspiratory time 0.65 s) was required, and a respiration rate of 30 breaths per minute was observed. Moist rales could be heard in both lungs. Figure 2 shows the overall radiographic course after admission. Laboratory results were as follows: white blood cell (WBC) count of 8.22×109/L, neutrophil (NEUT) count of 7.22×109 /L, lymphocyte (LYMP) count of 0.70×109 /L, haemoglobin (Hb) level of 118 g/L, and platelet (PLT) count of 22×109 /L. The results of blood biochemical indicators showed that the lactate dehydrogenase (LDH) level rose to 2882 U/L (reference range 150–250 U/L), and the level of creatine kinase-MB (CK-MB) increased to 100 U/L (reference range 0–18 U/L). The blood ammonia (BA) level was 85.0 µmol/L, the pro-brain natriuretic peptide (pro-BNP) level was 7169.0 pg/mL, the high-sensitivity cardiac troponin t test (hs-cTnT) levels was 157.5 pg/mL, and the nerve specific enolase (NSE, electroluminescence method) level was 204.30 ng/mL. Tests for the nucleic acid detection of SARS-CoV-2 and other common respiratory pathogens, including Mycoplasma pneumoniae, Chlamydia pneumoniae, adenovirus, parainfluenza virus, respiratory syncytial virus, and influenzas A and B, were all negative. Syphilis, HIV, and hepatitis C virus tests were all negative by serology. The 1,3-beta-D-glucan test (BDG, G test) was positive (785.6 pg/mL). The results of acid-fast sputum smear and mycobacterial culture were all negative. The blood and sputum smear and culture of bacteria and fungi were also negative. On the same day, two of the child’s venous blood samples and one bronchial sputum sample (the sputum samples were collected using hermetical suction tubes under the process of endotracheal intubation) were sent for microbial culture and mNGS testing. Digital chest radiography (CR) showed a large amount of exudation and consolidation (Figure 2A), and the patient was diagnosed with suspected polypathic pneumonia caused by PJP and CMV. Oral trimethoprim-sulfamethoxazole (TMP-SMX, 120 mg/kg·dose Q6H) combined with caspofungin (CAS, 14.4 mg, daily), MEM (100 mg Q8H), and vancomycin (VN, 50 mg QD) were used for anti-infective treatment, and MSSI (10 mg Q12H) was used as anti-inflammatory therapy. For the symptoms of thrombocytopenia caused by immunodeficiency, heparin (0.5 mL/h) was administered for anticoagulation, and blood products, such as the appropriate types of platelets and red blood cells, were infused to support the treatment.
Figure 2.
Imaging data of lungs. (A) on the 1st day of admission, CR showed exudation in both lungs and large effusion in the right pleural cavity. (B) CR indicated a large amount of diffuse patchy exudation in both lung fields on the 4th day. (C and D) Chest CT scans showed dense shadow and consolidation were diffused in both lungs on the 12th day. (E and F) on the day before discharge day, CR showed exudation and consolidation still existed in large areas of the lungs.
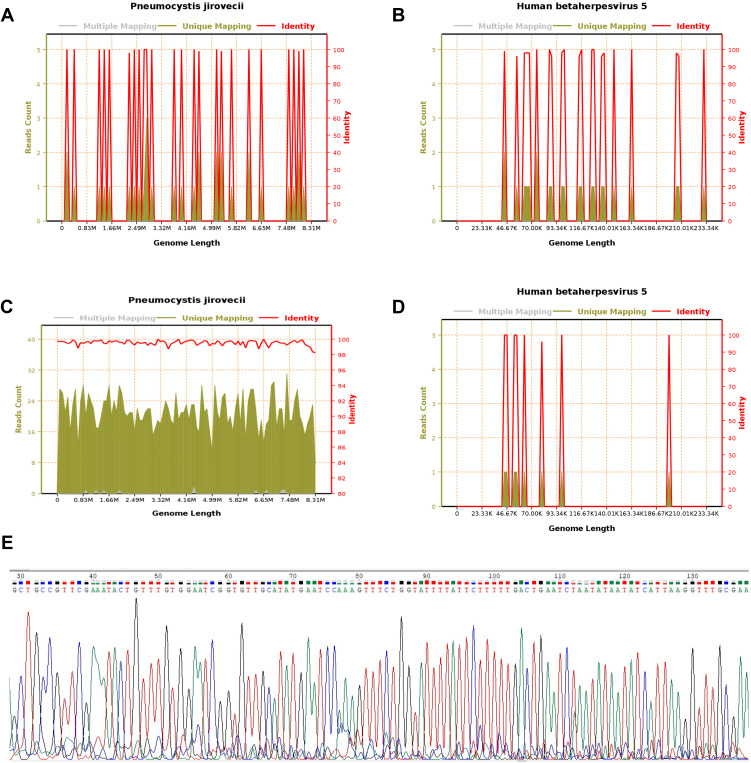
Two days later, the sputum culture result was negative. Nevertheless, the mNGS results showed that PJ and CMV nucleic acid sequences were found in both sputum and venous blood, and the tests were performed by Genskey Medical Technology Co., Ltd. (Beijing, China) using the procedures described by Grumaz et al.7 The database referenced during analysis of the sequencing data contains 12,895 species of bacteria, 11,120 species of viruses, 1582 species of fungi, 312 species of parasites, 184 species of mycoplasma/chlamydia, and 177 species of mycobacteria. The other microorganisms detected by mNGS are listed in Table 1, which were mainly common bacteria and were not considered to be the cause of invasive lung infections. The genomic coverage depth map of the sequence obtained by mNGS is shown in Figures 3A–D. We also verified PJ infection by Sanger sequencing (Figure 3E). Using these results combined with other physical examination results, the patient was diagnosed with PJ and CMV caused multipathogenic pneumonia. The causative agent of pneumocystis is generally known to be unculturable in vitro. Although the NGS results showed the presence of other microbial sequences, multiple blood culture and sputum culture results were negative, At the same time, the number of DNA copies of CMV was less than 2000 copies/mL, and CR showed that there was still a large amount of exudation in the lungs (Figure 2B). TMP-SMX (120 mg/kg·dose Q6H) combined with CAS (14.4 mg, QD) as well as MEM (100 mg Q8H) was continued for 11 days (Figure 1).
Table 1.
The Pathogen and Sequence Reads Detected by mNGS in Different Specimen Types
| Sample Testing Time (Date) | Sputum | Blood | BALF |
|---|---|---|---|
| June 12, 2021 | June 12, 2021 | June 22, 2021 | |
| Pathogen and Sequence Reads (n) | CMV (8) P. jirovecii (2110) Streptococcus peroris (18) Streptococcus parasanguinis (8) Rothia mucilaginosa (11) Staphylococcus saprophyticus (6) |
CMV (23) P. jirovecii (32) Corynebacterium casei (15) Staphylococcus hominis (8) Staphylococcus saprophyticus (7) Staphylococcus epidermidis (2) Cutibacterium acnes (14) Moraxella osloensis (11) Micrococcus luteus (4) |
CMV (140) P. jirovecii (17) EBV (1) Staphylococcus hominis (137) Cutibacterium acnes (439) Micrococcus luteus (188) Moraxella osloensis (332) Streptococcus peroris (23) Streptococcus mitis (15) |
Abbreviations: CMV, cytomegalovirus; P. jiroveci, Pneumocystis jiroveci; EBV, Epstein-Barr virus.
Figure 3.
Blood mGNS gene sequence coverage depth map for PJ (A) and CMV (B); sputum mGNS gene sequence coverage depth map for PJ (C) and CMV (D). Multiple Mapping: Multiple comparing 2 or more species. Unique Mapping: unique comparison to a certain species. Identity: the identity of the sequence compared to the reference genome. The abscissa is the size and location of the genome; the ordinate on the left is the number of sequenced sequences of the reference genome; the ordinate on the right is the consistency of the sequenced sequence with the reference genome. Peak map of PJ nucleic acid by Sanger sequencing (E).
Eleven days after admission, the child’s condition was not alleviated. The ECMO support time was quite long, while the lung infection remained serious. The G test value increased (2419.3 pg/mL). The patient underwent bronchoscopy with a collection of BALF for routine examination and mNGS experiment. The smear and culture results were negative, and the mNGS results showed that the level of Pneumocystis infection decreased but CMV levels increased (Table 1). CT showed that both lungs were white with pneumothorax and pleural effusion (Figure 2C and D). Anti-infective treatment with MEM (100 mg Q8H) and CAS (50 mg QOD) was continued to prevent infection. Cefoperazone sodium and sulbactam sodium were administered (SCF, 400 mg Q8H) combined with TMP-SMX tablets (150 mg Q6H). Given that the number of platelets and lymphocytes were low in the patient, acyclovir (10 mg/kg·dose Q8H) and IVIG (2.5 g/day) antiviral therapy were added for 2 days. Flow cytometry of peripheral blood cells showed that the CD3+ T cells/lymphocyte level was 52.32% (normal range 58.4–81.56%), and the CD4+ T cells/CD8+ T cells level was 4.2 (normal range 0.80–2.60). The diagnosis of immunodeficiency could not be excluded. After the following few days of treatment, the child was still in critical condition, and the G test value increased more (4138.0 pg/mL). CR showed that the lungs were still exuding severely (Figure 2E and F). The treatment, including ECMO, was suspended upon the request of the family. The child was eventually discharged after consent was obtained. Unfortunately, according to the telephone follow-up one week later, the child died two days later after leaving the hospital.
Discussion
This report is a case of an HIV-negative two-month-old child with coinfection of Pneumocystis and CMV, with observed platelet reduction and lymphocytopenia. CMV infection in the neonatal period can occur either in the uterus (congenital infection) or at a postnatal age (acquired cytomegalovirus infection). Acquired infection can occur through contact with the virus excreted by the infected person, blood transfusion, vaginal secretions, or spread through breast milk.8 In this case, the positivity of CMV DNA detected in the mother’s milk may have been responsible for the child’s CMV infection, as well as the symptoms of cholestatic hepatitis, immune thrombocytopenic purpura, severe pneumonia, and other related infections. Many steroid hormone drugs are used in the treatment of children in the early stage. It has been reported in the literature that the destruction of immune cells caused by a large number of steroid hormones can increase the risk of PJ infection, which suggests the possibility of coinfection of CMV and PJ in patients.9,10 Due to the use of HAART, PJP is currently rarer in HIV-infected groups; the symptoms of PJP progress more slowly, and the fungal burden is higher, so it is also easier to diagnose. In contrast, individuals not infected with HIV who have PJP exhibit rapid progression and severe respiratory symptoms, and the mortality rate is relatively higher at approximately 30–60%.11 Clinical cases of PJ and CMV coinfection have been reported, BDG and LDH concentrations were helpful to establish the diagnosis of PJP for early treatment.12 However, these indicators have poor specificity, and BDG can be easily interfered by many factors, such as systemic inflammation, albumin infusion, and the use of certain antibiotics.13 The immune system of infants and young children is immature, once PJP occurs, the symptoms are more severe and life-threatening than adults, in such cases, the deficiencies of existing conventional diagnostic methods will become the hurdle for the diagnosis of PJP mixed infection. Although the detection of PJ via BALF or lung biopsy is the gold standard for diagnosing PJP, these techniques are not always suitable for children because of their high invasiveness. Therefore, timely diagnosis and treatment of PJP are essential for patients, especially infants and young children. Fortunately, mNGS, a noninvasive technology for identifying microbial pathogens, matches this challenge. The sensitivity of mNGS in diagnosing PJP is significantly higher than that of GMS (Gomori’s Methenamine Silver) and measurement of serum BDG levels, especially in the recognition of PJP and CMV or Epstein–Barr virus (EBV) coinfection.14 In this case, the child’s serum BDG level always suggested fungal infection, but the results of sputum smear, staining microscopy, and culture were all negative, reflecting the limitations of traditional detection methods. The diagnostic method based on polymerase chain reaction (PCR) has good sensitivity and specificity for PJP detection, but a commercial kit for its assessment has not been approved for clinical application in China.15,16 The uses of mNGS in the coinfection of CMV and PJP have been reported in the literature. However, to date, only 6 studies have reported 20 successful cases of using NGS to diagnose PJP and CMV lung infections in BALF or blood samples (Supplementary Table S1). Yan et al also performed mNGS studies on the blood samples of 34 children with suspected sepsis in the Paediatric Intensive Care Unit to detect the microbial genome sequences of potential pathogens, including PJP and CMV, which revealed that the number of fungal and protozoan species in immunodeficient children is significantly higher than that in immunocompetent children.17 In this case report, Pneumocystis was detected in sputum, blood, and BALF, but it was the second case in which Pneumocystis was detected in a sputum sample, and the number of sequence reads of PJ was much higher than that in blood samples at the same time. It is also the first case in which three different samples of blood, sputum, and BALF were tested by mNGS technology in one infant, and positive results were obtained in all of them. Regrettably, only BALF was examined 10 days later, and sputum and blood were not again examined. Ideally, there should be results for these 3 types of samples taken at the same time. However, it must be assumed that after these 10 days, the level of PJ dropped because BAL1F assessment is more sensitive than sputum assessment, the cost of testing should also be considered. It can also be seen from Supplementary Table S1 that the NGS readings vary greatly, and the cut-off value for the NGS markers used for PJP and CMV diseases is currently uncertain. Studies have shown that the top 15 specific reads or the relative read ratio in fungi are higher than 85%, which may be a satisfactory cut-off value for the clinical diagnosis of PJP.16,18–22
Traditional diagnostic techniques for microbial pathogens include culture and isolation, serological detection of specific antibodies or antigens, and molecular identification of microbial nucleic acids (DNA or RNA). Most molecular tests require specific primers or probes and only target a limited number of pathogens. However, metagenomic methods can be used to assess all the DNA or RNA present in the sample, allowing the analysis of the entire microbiome in the patient sample and the human host genome or transcription group. The traditional microbial detection methods currently used can only be used to detect one or a limited number of pathogens at a time, and most of them require the successful cultivation of microbes in clinical samples. mNGS can be used to identify a wide range of pathogens, viruses, bacteria, fungi, and/or parasites by culturing or directly based on uniquely identifiable DNA and/or RNA sequences in clinical samples.23 In the case of uncertainty as to which pathogen is the cause of infection, traditional diagnostic methods, such as qPCR and nested PCR, have significant limitations. mNGS can provide the advantage of multiple detections in the diagnosis of complex mixed infections, and the detection time can be shortened to less than 48 hours; this technique can thus be used clinically as a diagnostic strategy for suspected pathogen infection. Although the cost of mNGS is higher than that of traditional detection methods, its price is decreasing each year with the popularization of clinical applications. At present, 7 cases utilizing mNGS technology in infant lung infection have been reported, mainly in detecting pathogenic bacteria in the blood and BALF samples, and the results of routine culture in 3 cases were also negative (Supplementary Table S2).22,24–29 According to our report, the three mNGS test results were positive, but the blood culture and multiple sputum culture experiments failed to detect pathogens. In previous diagnostic and treatment plans for children with a lung infection, when the growth of pathogenic bacteria was not found in routine blood culture and sputum culture, it brought great difficulties to diagnosis and treatment. The reason may be that the culture medium is not suitable, or the number of bacteria is small, but the pathogenicity is strong. BALF collection is harmful to younger and more seriously ill infants, and this patient had immunodeficiency and low platelet levels. The NGS assessment of sputum samples reduces the harm to patients, and the results were no different from the blood and BALF results. This technique provides a reference for the clinical treatment of severe pneumonia in infants and young children, and sputum NGS is a good choice. Of course, when mNGS testing determines the pathogenicity of pathogens in clinical diagnosis, the results must be carefully interpreted in the clinical context, especially when atypical or new infectious nucleic acid sequences are found in clinical samples.
In our case report, the diagnosis of PJ and CMV pulmonary mixed infection in the patient was confirmed through the detection of the nucleic acid sequences of PJ and CMV in the blood and sputum using mNGS on the second day of the patient’s stay in our hospital, and the treatment plan was adjusted to anti-fungal combined anti-viral therapy in time. Unfortunately, the patient had not been diagnosed with Pneumocystis infection in the previous hospital, which delayed diagnosis, and lack of proper treatment ultimately decreased the patient’s chances of survival. The child did not have any immunosuppressive background or predisposition, but due to the young age and the immaturity of the immune system, PJ colonization (asymptomatic) is often observed in this age range. In the context of coinfections, blinded “drug bombardment”, which lowers immunity (for example, through the use of prednisone), could facilitate the deterioration of the general condition of the patient and/or facilitate infection with another pathogen (CMV was most likely the first pathogen transferred from the mother but CMV infection also lasted longer; afterwards, PJ infection began to regress after administration of proper drugs). mNGS could be a useful method for the detection of mixed infections to prevent overtreatment. Unfortunately, it is difficult to clinically differentiate between colonization (asymptomatic) and PJ infection in non-HIV patients (mNGS also has no relevant research for the time being). Early bronchoscopy and mNGS examinations are recommended, combined with BDG, LDH, lungs CT and other test results, to achieve effective and rapid diagnosis of PJ mixed infection. Culture-independent NGS technology will increase the diagnosis rate of rare paediatric pathogens and help in the identification of viral infections. This approach shortens the time required for clinical diagnosis and provides accurate solutions for the rational use of antibacterial drugs. Although this patient eventually died, mNGS technology displayed a significant advantage in diagnosing the disease.
Acknowledgments
We appreciate that the Guangdong Detection Center of Microbiology provided technical support in strain identification.
Funding Statement
This research was supported by the National Natural Science Foundation of China (81871734, 82072380), Key R & D Program of Jiangsu Province (BE2020646), Research Foundation for advanced talents of Guangdong Provincial People’s Hospital (KJ012021097).
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Statement
We obtained written informed consent including data and images for publication from the guardian of the patient. This study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital (KY-N-2022003-03) and conducted according to the Declaration of Helsinki. All research data were de-identified and anonymously analyzed.
Disclosure
The authors declare that they have no conflict of interest.
References
- 1.Sepkowitz KA. Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis. 2002;34(8):1098–1107. doi: 10.1086/339548 [DOI] [PubMed] [Google Scholar]
- 2.Restrepo-Gualteros SM, Gutierrez MJ, Villamil-Osorio M, Arroyo MA, Nino G. Challenges and clinical implications of the diagnosis of cytomegalovirus lung infection in children. Curr Infect Dis Rep. 2019;21(7):24. doi: 10.1007/s11908-019-0681-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rojas P, Friaza V, García E, et al. Early acquisition of pneumocystis jirovecii colonization and potential association with respiratory distress syndrome in preterm newborn infants. Clin Infect Dis. 2017;65(6):976–981. doi: 10.1093/cid/cix454 [DOI] [PubMed] [Google Scholar]
- 4.Coclite E, Di Natale C, Nigro G. Congenital and perinatal cytomegalovirus lung infection. J Matern Fetal Neonatal Med. 2013;26(17):1671–1675. doi: 10.3109/14767058.2013.794207 [DOI] [PubMed] [Google Scholar]
- 5.Salzer HJF, Schäfer G, Hoenigl M, et al. Clinical, diagnostic, and treatment disparities between HIV-infected and non-HIV-infected immunocompromised patients with Pneumocystis jirovecii pneumonia. Respiration. 2018;96(1):52–65. doi: 10.1159/000487713 [DOI] [PubMed] [Google Scholar]
- 6.Qian YY, Wang HY, Zhou Y, et al. Improving pulmonary infection diagnosis with metagenomic next generation sequencing. Front Cell Infect Microbiol. 2020;10:567615. doi: 10.3389/fcimb.2020.567615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grumaz S, Stevens P, Grumaz C, et al. Next-generation sequencing diagnostics of bacteremia in septic patients. Genome Med. 2016;8(1):73. doi: 10.1186/s13073-016-0326-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamprecht K, Maschmann J, Jahn G, Poets CF, Goelz R. Cytomegalovirus transmission to preterm infants during lactation. J Clin Virol. 2008;41(3):198–205. doi: 10.1016/j.jcv.2007.12.005 [DOI] [PubMed] [Google Scholar]
- 9.Aviles R, Boyce TG, Thompson DM. Pneumocystis carinii pneumonia in a 3-month-old infant receiving high-dose corticosteroid therapy for airway hemangiomas. Mayo Clin Proc. 2004;79(2):243–245. doi: 10.4065/79.2.243 [DOI] [PubMed] [Google Scholar]
- 10.Yu Q, Jia P, Su L, Zhao H, Que C. Outcomes and prognostic factors of non-HIV patients with pneumocystis jirovecii pneumonia and pulmonary CMV co-infection: a retrospective cohort study. BMC Infect Dis. 2017;17(1):392. doi: 10.1186/s12879-017-2492-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cillóniz C, Dominedò C, Álvarez-Martínez MJ, et al. Pneumocystis pneumonia in the twenty-first century: HIV-infected versus HIV-uninfected patients. Expert Rev Anti Infect Ther. 2019;17(10):787–801. doi: 10.1080/14787210.2019.1671823 [DOI] [PubMed] [Google Scholar]
- 12.Borstnar S, Lindic J, Tomazic J, et al. Pneumocystis jirovecii pneumonia in renal transplant recipients: a national center experience. Transplant Proc. 2013;45(4):1614–1617. doi: 10.1016/j.transproceed.2013.02.107 [DOI] [PubMed] [Google Scholar]
- 13.Del Corpo O, Butler-Laporte G, Sheppard DC, Cheng MP, McDonald EG, Lee TC. Diagnostic accuracy of serum (1-3)-β-D-glucan for Pneumocystis jirovecii pneumonia: a systematic review and meta-analysis. Clin Microbiol Infect. 2020;26(9):1137–1143. doi: 10.1016/j.cmi.2020.05.024 [DOI] [PubMed] [Google Scholar]
- 14.Jiang J, Bai L, Yang W, et al. Metagenomic next-generation sequencing for the diagnosis of Pneumocystis jirovecii pneumonia in non-HIV-infected patients: a retrospective study. Infect Dis Ther. 2021;10(3):1733–1745. doi: 10.1007/s40121-021-00482-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fillaux J, Berry A. Real-time PCR assay for the diagnosis of Pneumocystis jirovecii pneumonia. Methods Mol Biol. 2013;943:159–170. doi: 10.1007/978-1-60327-353-4_11 [DOI] [PubMed] [Google Scholar]
- 16.Zhang F, Chen J, Huang H, et al. Application of metagenomic next-generation sequencing in the diagnosis and treatment guidance of Pneumocystis jirovecii pneumonia in renal transplant recipients. Eur J Clin Microbiol Infect Dis. 2021;40(9):1933–1942. doi: 10.1007/s10096-021-04254-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yan G, Liu J, Chen W, et al. Metagenomic next-generation sequencing of bloodstream microbial cell-free nucleic acid in children with suspected sepsis in pediatric intensive care unit. Front Cell Infect Microbiol. 2021;11:665226. doi: 10.3389/fcimb.2021.665226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xie Y, Ruan B, Jin L, Zhu B. Case report: next-generation sequencing in diagnosis of pneumonia due to Pneumocystis jirovecii and cytomegalovirus in a patient with HIV infection. Front Med. 2021;8:653294. doi: 10.3389/fmed.2021.653294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J, Han Y, Feng J. Metagenomic next-generation sequencing for mixed pulmonary infection diagnosis. BMC Pulm Med. 2019;19(1):252. doi: 10.1186/s12890-019-1022-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y, Ai JW, Cui P, Zhang WH, Wu HL, Ye MZ. A cluster of cases of pneumocystis pneumonia identified by shotgun metagenomics approach. J Infect. 2019;78(2):158-169. doi: 10.1016/j.jinf.2018.08.013 [DOI] [PubMed] [Google Scholar]
- 21.Xie D, Xian Y, You J, et al. Co-Infection Pneumonia with Mycobacterium abscessus and Pneumocystis jiroveci in a Patient without HI V Infection Diagnosed by Metagenomic Next-Generation Sequencing. Infect Drug Resist. 2021;14:879-888. doi: 10.2147/IDR.S292768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang. S. H, Meng. X. Y, Bai. Z. J, Li. Y, Wu. S. Y. X-Linked Hyper IgM Syndrome Manifesting as Recurrent Pneumocystis jirovecii Pneumonia: A Case Report. J Trop Pediatr. 2020;66 (6), 648-654. doi: 10.1093/tropej/fmaa023 [DOI] [PubMed] [Google Scholar]
- 23.Chiu CY, Miller SA. Clinical metagenomics. Nat Rev Genet. 2019;20(6):341-355. doi: 10.1038/s41576-019-0113-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen SH, Lin L, Yu G, et al. Pseudomembranous laryngotracheobronchitis due to coinfection with human bocavirus 1 and Mycoplasma pn pneumonia: a case report. Transl Pediatr. 2021;10(3):673–678. doi: 10.21037/tp-20-278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qin L, Zhang FZ, Yang TY, Tao XF, Tang LF. Pulmonary Nocardia infection in a child with idiopathic pulmonary hemosiderosis. BMC Pulm Med. 2021;21(1):182. doi: 10.1186/s12890-021-01544-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu YR, Ai T. Plastic bronchitis associated with Botrytis cinerea infection in a child: a case report. World J Clin Cases. 2020;8(20):5019–5024. doi: 10.12998/wjcc.v8.i20.5019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ba H, Peng H, Cheng L, et al. Case report: talaromyces marneffei infection in a Chinese child with a complex heterozygous CARD9 mutation. Front Immunol. 2021;12:685546. doi: 10.3389/fimmu.2021.685546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin Y, Wang BX, Zhang NN, et al. Metagenomic analysis identified Stenotrophomonas maltophilia pneumonia in an infant suffering from unexplained very severe pneumonia. Front Pediatr. 2019;7:380. doi: 10.3389/fped.2019.00380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Ai L, Zhou Y, et al. Rapid and precise diagnosis of pneumonia coinfected by Pneumocystis jirovecii and Aspergillus fumigatus assisted by next-generation sequencing in a patient with systemic lupus erythematosus: a case report. Ann Clin Microbiol Antimicrob. 2021;20(1):47. doi: 10.1186/s12941-021-00448-5 [DOI] [PMC free article] [PubMed] [Google Scholar]