Abstract
The potential for virtual healthcare to improve access to primary care services in Canada has long been a topic of discussion; however, implementation has been slow despite growing interest among the public. Non-essential service lockdowns implemented in 2020 in response to the COVID-19 pandemic catalyzed rapid and widespread uptake of virtual healthcare delivery. It is important to consider how to maintain equitable access to virtual care following the pandemic. We conducted a narrative scoping review to understand barriers related to the sustained adoption of virtual primary care delivery in Canada. Barriers at the system, healthcare provider, and patient levels were related to digital health infrastructure, and the regulatory environment governing virtual care provision and remuneration for healthcare professionals. The article identifies areas where policy shifts by health system leaders could sustain the longer-term availability of Canadian virtual care services.
Introduction
Use of information and communication technologies by physicians to provide patients with health services has been described using various terms, such as digital health, mobile health, telehealth, and telemedicine.1-5 For simplicity, we refer to electronically mediated physician-patient consultations as virtual healthcare delivery, or virtual care. Specific technologies and approaches in virtual care vary. Synchronous methods, such as telephone or video-conferencing, allow the physicians and patients to communicate directly with each other, while in asynchronous methods, such as secure messaging, text, or e-mail, the physician uploads information to a platform which the patient can access.6 Either method may include the use of Electronic Health Record (EHR) systems.3,7,8 Virtual care may be provided by patients’ regular primary care physicians, or may be provided by private companies, or “virtual walk-in clinics,” where the patient has no prior relationship with the care provider.8-10
Virtual care in its various forms has been viewed as a tool for improving access to health services for people who face difficulties travelling to facilities for in-person care.2,6,11-18 It is also seen as a way to meet growing demands on healthcare systems1,3,6,11-13,16 and potentially reduce healthcare costs.2,6,11,12,19,20 Virtual care is appealing to the public, due to its convenience compared to in-person services.6,9,17,21-23
Despite public interest in Canada in using virtual healthcare, and expansion of private sector virtual care services,8-10,24,25 integration in medical practices has been slow.1,2,6,15 International studies and reports have pointed out that adoption of virtual care involves a range of social and technical factors.19,26,27 They have identified a number of potential barriers to adoption, including: uncertainty over licensing requirements and legal liability5,16; risks to patient confidentiality and data security5,19,26; lack of EHR system interoperability5,13,16,19; digital infrastructure limitations16,26; changes to physicians’ workflow and need for virtual care training16,26; cost to patients due to lack of virtual care insurance coverage5,19; patients’ low digital health literacy and lack of access to suitable communications devices or internet connectivity3,5,13,19; and preference for in-person services.16,19 There are also concerns about equitable access to virtual care by socially or economically marginalized populations, and about virtual services contributing to fragmentation of care.5,13,19 The same barriers could contribute to slow uptake of virtual care in Canada.
The onset of the COVID-19 pandemic in 2020 and necessity of reducing viral transmission prompted an abrupt shift toward adoption of virtual care.5,7,23,28 Provincial governments and health authorities across Canada instituted temporary regulatory changes to enable virtual care provision.11,21-23,28-33 Use of virtual care rose dramatically in the first six months of the pandemic,11,21,23,28-30,34,35 but as restrictions eased, virtual visits declined.34,36,37 It is unknown to what extent virtual care will be sustained as the threat from COVID-19 recedes, or how widespread adoption will impact existing health inequities.
In order to better understand where policy shifts can promote integration of virtual healthcare delivery while mitigating potential unintended consequences of widespread adoption, we conducted a narrative scoping review38,39 aimed at identifying barriers to the adoption of virtual primary care in Canada.
Methods
Our review involved two stages; first, a literature search informed by the PRISMA Extension for Scoping Reviews,40,41 followed by a narrative synthesis using qualitative content analysis.38,42 The literature search involved several phases. Initially, we carried out exploratory searches in PubMed Central and Google using broad terms, such as “telehealth,” “virtual care,” “barriers,” and “challenges,” with Boolean connectors used to narrow the results. The first ten pages of results were screened for relevance, which generated 42 journal articles and grey literature items. We refined the strategy for following searches to limit results to items published within the past 10 years which describe the use of patient-physician virtual visits for primary care in Canada.
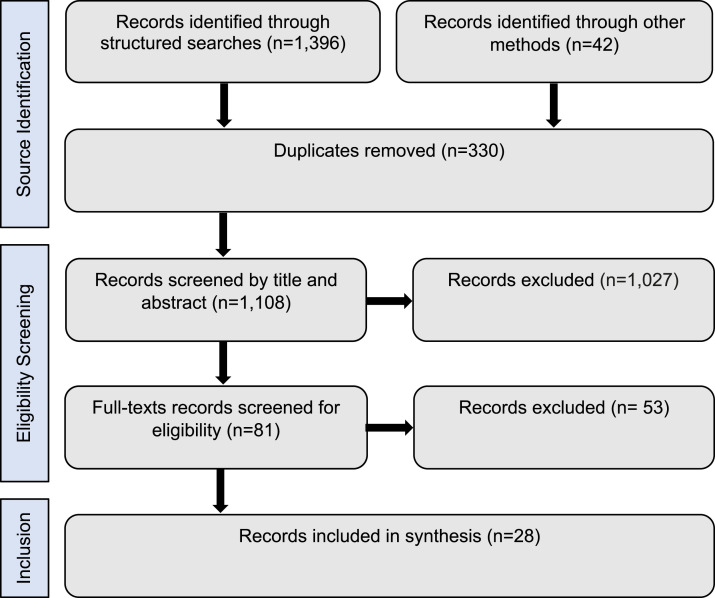
Searches in PubMed Central, MEDLINE@Ovid, EMBASE, and Scopus generated a total of 1,396 results (See Table 1), which were pooled with items from the exploratory search. Duplicates were removed and sources were screened for relevance (See Figure 1). Exclusion criteria included: items mentioning virtual care or Canada only in passing; items focused primarily on EHR systems, artificial intelligence, or electronic health monitoring; records focused on specific health conditions (such as mental health), or populations (such as paediatrics, or older adults); and research protocols.
Table 1.
Scoping review searches.
| Search platform | Search terms/strings | Results |
|---|---|---|
| PubMed Central | (((((“virtual care”[All Fields] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND “canada”[MeSH Terms] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) OR ((“digital health”[All Fields] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND “canada”[MeSH Terms] AND “2012/04/08”[PDat]: “2022/04/05”[PDat])) OR ((“telemedicine ”[All Fields] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND “canada”[MeSH Terms] AND “2012/04/08”[PDat]: “2022/04/05”[PDat])) OR ((“ehealth”[All Fields] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND “canada”[MeSH Terms] AND “2012/04/08”[PDat]: “2022/04/05”[PDat])) OR ((“mobile health”[All Fields] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND “canada”[MeSH Terms] AND “2012/04/08”[PDat]: “2022/04/05”[PDat]) AND (“2012/04/08”[PDat]: “2022/04/05”[PDat]) | 748 |
| MEDLINE@Ovid | Telemedicine/ AND Canada/ Date range: 2012-2022 | 218 |
| EMBASE | (‘canada’/mj AND [2012-2022]/py) AND ((‘virtual care’ AND [2012-2022]/py) OR (telemedicine AND [2012-2022]/py) OR (‘digital health’ AND [2012-2022]/py) OR (‘mobile health’ AND [2012-2022]/py) OR (‘ehealth’ AND [2012-2022]/py)) | 64 |
| Scopus | (KEY (“virtual care”) OR KEY (“telemedicine”) OR KEY (“digital health”) OR KEY (“mobile health”) OR KEY (“ehealth”)) AND KEY (“canada”) AND (LIMIT-TO (PUBYEAR, 2022) OR LIMIT-TO (PUBYEAR, 2021) OR LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019) OR LIMIT-TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016) OR LIMIT-TO (PUBYEAR, 2015) OR LIMIT-TO (PUBYEAR, 2014) OR LIMIT-TO (PUBYEAR, 2013)) AND (LIMIT-TO (LANGUAGE, “English”)) AND (LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re”)) – limited to 2013-2022 | 366 |
Figure 1.
PRISMA-ScR source selection diagram.
Remaining items (n = 28) were analyzed thematically.38,42 The COVID-19 pandemic represented an important contextual change, and we noted whether records presented research conducted before (articles n = 11; grey literature n = 4), or during the pandemic (articles n = 10; grey literature n = 3). The review only included publicly available records and did not require ethics approval.
Barriers to virtual healthcare adoption
Barriers to Canadian adoption of virtual primary care delivery were identified at contextual/systemic, physician, and patient levels.
Systemic barriers
Canada’s digital communication infrastructure is extensive, but limited cellular network coverage and internet bandwidth were barriers for virtual care in rural and remote areas,2,11,14,28,35 although a study of the Ontario Telemedicine Network found that only 0.2% of visits using that system were missed due to technical difficulties.18 Poor interoperability between EHR systems can also be a barrier to virtual care. There are no comprehensive Canadian standards or metrics for EHR system interoperability.1,15 Available information suggests that provinces and territories, and sometimes health authorities within provinces, use a variety of systems.1,2,4,8,15,43
Disturbing the status quo when adopting virtual care was identified as a barrier within health systems.1,2,11,43 Licensing virtual care provision falls within the jurisdiction of the provincial and territorial governments and varies across Canada.1,2,8,17,28,43 Patient privacy and personal health data are strongly protected in Canada, and prior to the COVID-19 pandemic, there were questions about what actions healthcare providers needed to take to comply with requirements, and what liability they might be exposed to when providing virtual services.1,2,4,11,15,23,28,43
Provincial and territorial governments also determine publicly funded healthcare coverage and remuneration. Prior to the pandemic, remuneration for virtual care was identified as an important barrier, with coverage of virtual care varying between jurisdictions and not all delivery modes included in fee schedules.1,4,6,8,10,15,17,28,29,33,43 For example, British Columbia started reimbursing care providers for video or text/e-mail consultations before other provinces,44 and in Ontario, providers were required to use a specific telemedicine platform for reimbursed video-consultations.29,30
The COVID-19 pandemic prompted several changes related to virtual care. In particular, provincial and territorial governments extended publicly funded coverage to include more virtual care modes and remunerate primary care physicians for virtual care.10,23,28-30,33 Interoperability with health information systems remained a challenge, however, with one study reporting that 76% of physician participants were using platforms that were not EHR-integrated and 41% were concerned about lack of data-sharing.11
Barriers for care providers
While care providers’ expectations about virtual care could slow implementation, Canadian physicians tended to view positively using virtual care for suitable conditions, especially after gaining experience.21,23,28,45 Younger and newly trained care providers were also open to virtual care.44,46 However, studies indicate that before the pandemic only a small minority offered virtual visits.44,45
Some research found that care providers expressed concerns about digital infrastructure.2,11,23 A study from British Columbia showed that two thirds of patients using virtual care saw providers other than their regular doctors,44 and physicians expressed concerns about weakened therapeutic relationships and risks of fragmented care.1,20,23 Integrating virtual care technologies could also potentially disrupt care providers’ work.6 Physicians highlighted that virtual visits did not enable them to apply a full range of diagnostic techniques during an examination, limiting the care they could provide.23,28,33 Additional time demands from providing virtual care were moderate,6,11,17 but responding to requests could increase workload.6,17
Barriers for care providers related to regulation and licensing included the length and complexity of the process, and variation in requirements between jurisdictions.1,15 Physicians were concerned about protecting patient confidentiality during virtual visits and the possibility of legal liability in the event of security breaches.8,11,20,45 Remuneration systems were also barriers. Care providers were sometimes unsure about whether or not they would be reimbursed for virtual care they provided,2,23,45,46 which could discourage them from offering virtual services.
When lockdowns were instituted in 2020 to prevent COVID-19 transmission, primary care physicians had to use virtual care delivery11,21-23,28-30. Care providers expressed concerns about limited administrative and technological resources, and uncertainty about the quality of virtual care.11,23,28,33 Some initially worried about their lack of previous experience, but they reported becoming more confident over time.23 According to one study, costs of providing virtual care and lack of adequate training were rarely mentioned, being identified as problems by only 10.5% and 9% of respondents, respectively.11 Overall, the number of physicians offering virtual care services increased rapidly11,28-30; one study in Ontario found an increase from 7.0% in 2019 to 85.9% in 202029 and another found that 96.6% of respondents offered some type of virtual care.11 While virtual care offerings increased, care providers often preferred familiar technologies, with telephone and text, e-mail, or secure messaging use growing more quickly than video consultations.11,29,33
Barriers faced by patients
A “digital divide” rooted in unequal skills and access to suitable technology was widely identified as a potential barrier for patients.1,8,11,14,17,22,23,34,43,47,48 There is no pan-Canadian data on digital health literacy,1 but a British Columbia study found that virtual care use was highest in the 20-44 age group.44 Data also indicate that people aged 65+ were less likely to use virtual care.1,14,22,30,34,44,48 Although coverage in rural areas is lower,2,34 a large proportion of Canadians live in areas with high-speed internet and cellular coverage.48 Income is a strong predictor of internet use in Canada,14,34,47 and by extension a factor in virtual care use.
Patients’ negative perception of virtual care was not identified as a main barrier to adoption. Canadian patients reported concerns over data security and privacy,48 and loss of human contact during virtual visits,35,48 but often described virtual care as convenient and expressed willingness to use it when other options are not readily available.2,6,20,21,23,44,47 One report found a large majority are open to some use of virtual care services.1 Cost may be a barrier to access for lower income patients, however, when private virtual walk-in clinics charge fees for services and are not covered by publicly funded services or private health insurance.1,8,10
Studies show that a rapid increase in virtual care usage occurred early in the pandemic, driven by lock-downs.11,17,21,22,29,30,34,35 In Ontario, these increases were statistically similar across income quintiles, suggesting that lower income users were not strongly disadvantaged in the shift to virtual services.29 Virtual care use among older adults also increased rapidly alongside use by the general population during the pandemic; however, virtual care could still be challenging for those who have cognitive or physical impairments.22,29,30,34 Recent data indicate that virtual care usage declined in 2021 following the removal of lockdowns, but constitutes a larger proportion of patient-reported visits than pre-pandemic.34,36
Policy shifts
This review found that patients in Canada are willing to use virtual care and are generally satisfied with those services.2,21,22,29,30,35,44,47 A digital divide exists in Canada, but it is shrinking as high-speed internet and cellular coverage expands and internet-connected devices have become common.14,49-52 Increased virtual care use during the COVID-19 pandemic showed that many patients are able to use those services.11,21,29,30,34,35 Relatively few Canadian primary care professionals offered virtual services before the pandemic; however,1,21,30,45 private sector virtual walk-in clinics expanded to meet consumer demand.8-10,24,25,53 There are policy shifts that could encourage sustained increases in virtual care provision by primary care providers over the long term, while mitigating unintended consequences.
Shift 1: Expand publicly funded coverage of virtual care delivery
Provincial and territorial healthcare policy-makers are cautious about additional costs, but the 2015 Advisory Panel on Healthcare Innovation pointed out that changes in remuneration systems are needed to encourage physicians to offer virtual care.15 Private sector virtual walk-in clinics are available, but patients often have to pay for memberships or out-of-pocket fees.9,10,25 Some provinces cover visits to virtual clinics, and extending coverage to include virtual services delivered by primary care providers would help to address cost barriers faced by lower income patients, particularly if coverage includes low-cost delivery modes, such as telephones, text, secure messages, or e-mail.6,8,9,11,37 Such a policy shift would reassure primary care providers that they will be reimbursed for providing virtual services.
The 2020 report of the Virtual Care Task Force convened by the Canadian Medical Association, the College of Family Physicians of Canada, and the Royal College of Physicians and Surgeons of Canada, recommended that provincial and territorial governments adopt fee schedules which establish a revenue-neutral balance of incentives between virtual and in-person visits.8 We echo that recommendation. The 2015 Advisory Panel on Healthcare Innovation suggested forming a commission to study the costs and advantages of different fee structures.15 No commission was established, but we suggest carrying out research to evaluate costs and health impacts from virtual care and identify suitable remuneration rates.1,8,28,37 British Columbia and Ontario, which have relatively long histories of integrating virtual care within their fee-for-service payment models,8,18,44 could help inform remuneration policy development in other jurisdictions.
Shift 2: Update regulations to support adoption of virtual care
Data security in Canadian health systems is an issue as recent large-scale cyber-attacks in Saskatchewan and Newfoundland and Labrador illustrate.54,55 Canada also lacks nationally agreed upon standards for electronic record system interoperability,1,8,11,15 which could contribute to fragmentation of care when patients access services from multiple in-person and virtual care providers.1,8,11,24,25,43,44 Finally, physicians who are interested in offering virtual care services to patients in other jurisdictions face challenges when they attempt to negotiate varied licensing requirements in different provinces and territories.1,2,8,11,17,25 Lack of clarity around how privacy, data security, and licensing requirements apply to virtual care has discouraged physicians from offering those services.1,2,8,11,20,45
Multiple studies and reports have recommended the adoption of nation-wide standards or licensing frameworks for virtual care provision.1,8,11,15,17,25 In the United States, a white paper by the Institute for Healthcare Improvement suggested that standards for virtual care should include metrics to ensure appropriate use, system-wide processes for protecting patient data, and safety and incident reporting to track data on safety indicators.5 Similarly, the 2020 Virtual Care Task Force report recommended establishing pan-Canadian frameworks for patient-centred, quality-based virtual care governance, which would include agreements on health information exchange, technical architecture, harmonized legislation, and shared patient and provider registries with unique identifiers for each patient and each provider.8
Canadian provinces and territories are empowered to set healthcare regulations, and they have delegated much of the responsibility for licensing care providers to the colleges, societies and associations representing health professionals. That regulatory system presents challenges for achieving nationwide frameworks, but cross-jurisdictional agreements are possible. The Advisory Panel on Healthcare Innovation suggested that the federal Privacy Commissioner and provincial and territorial commissioners collaborate to establish shared understandings on the protection of patient privacy, which would also allow EHR interoperability.15 Professional organizations are also able to collaborate across jurisdictions to adopt shared models for licensing virtual care providers. The Virtual Care Task Force report suggested supporting efforts by the Federation of Medical Regulatory Authorities of Canada (FMRAC) to simplify regulation and licensure of qualified physicians to practice across jurisdictions.8 One option for a shared agreement on virtual care would be to adopt the Framework for Telemedicine developed by FMRAC in 2019.56 Developing and adopting pan-Canadian frameworks will give virtual care providers clearer guidance and reduce important barriers.
Conclusion
Virtual care expanded rapidly as part of the public health response to the COVID-19 pandemic. Virtual care has some disadvantages compared to traditional in-person services. It depends on having adequate digital and communication infrastructure and is not suitable for providing care for all health conditions. Virtual services are often appropriate for providing routine primary care, however, and mixed service delivery could make valuable contributions to the Canadian health system.
The review presented here suggests that for healthcare providers and patients, barriers are interlinked and are often responses to regulatory environments shaped at the health system level. Provincial and territorial policy shifts undertaken in collaboration with provincial and national medical colleges and associations, such as including virtual care delivery within publicly funded service coverage and updating regulatory frameworks, have the potential to maintain increased adoption of virtual care following the COVID-19 pandemic.
ORCID iD
Patrick B. Patterson https://orcid.org/0000-0002-5538-1723
References
- 1.Canadian Medical Association . Virtual care in Canada: discussion paper. Canadian Medical Association. 2019. Available at: https://www.cma.ca/sites/default/files/pdf/News/Virtual_Care_discussionpaper_v2EN.pdf [Google Scholar]
- 2.Exner-Pirot H. Challenges to telehealth implementation. In: Exner-Pirot H, Norbye B, Butler L, eds. Northern and Indigenous Health and Health Care. University of Saskatchewan; 2018, chap 28. [Google Scholar]
- 3.Smith B, Magnani JW. New technologies, new disparities: the intersection of electronic health and digital health literacy. Int J Cardiol. 2019;292:280-282. doi: 10.1016/j.ijcard.2019.05.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw J, Jamieson T, Agarwal P, Griffin B, Wong I, Bhatia RS. Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique. J Telemed Telecare. 2018;24(9):608-615. doi: 10.1177/1357633x17730444 [DOI] [PubMed] [Google Scholar]
- 5.Perry AF, Frederico F, Huebner J. Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care. IHI White Paper. Institute for Healthcare Improvement; 2021. [Google Scholar]
- 6.Stamenova V, Agarwal P, Kelley L, et al. Uptake and patient and provider communication modality preferences of virtual visits in primary care: a retrospective cohort study in Canada. BMJ Open. 2020;10(7):e037064. doi: 10.1136/bmjopen-2020-037064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong A, Bhyat R, Srivastava S, Boissé Lomax L, Appireddy R. Patient care during the COVID-19 pandemic: use of virtual care. J Med Internet Res. 2021;23(1):e20621. doi: 10.2196/20621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Medical Association , The College of Family Physicians of Canada, Royal College of Physicians and Surgeons of Canada. Virtual Care: Recommendations for Scaling Up Virtual Medical Services. 2020. Available at: https://www.cma.ca/sites/default/files/pdf/virtual-care/ReportoftheVirtualCareTaskForce.pdf [Google Scholar]
- 9.Kobewka D, Forster AJ. On-line doctors: a disruptive innovation? Healthc Manage Forum. 2018;31(4):160-162. doi: 10.1177/0840470418780022 [DOI] [PubMed] [Google Scholar]
- 10.Matthewman S, Spencer S, Lavergne MR, McCracken RK, Hedden L. An environmental scan of virtual “walk-in” clinics in Canada: comparative study. J Med Internet Res. 2021;23(6):e27259. doi: 10.2196/27259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohammed HT, Hyseni L, Bui V, et al. Exploring the use and challenges of implementing virtual visits during COVID-19 in primary care and lessons for sustained use. PLoS One. 2021;16(6):e0253665. doi: 10.1371/journal.pone.0253665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snoswell CL, North JB, Caffery LJ. Economic advantages of telehealth and virtual health practitioners: return on investment analysis. JMIR Perioperat Med. 2020;3(1):e15688. doi: 10.2196/15688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liaw WR, Jetty A, Coffman M, et al. Disconnected: a survey of users and nonusers of telehealth and their use of primary care. J Am Med Inform Assoc. 2019;26(5):420-428. doi: 10.1093/jamia/ocy182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Latulippe K, Hamel C, Giroux D. Social health inequalities and ehealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res. 2017;19(4):e136. doi: 10.2196/jmir.6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naylor D, Girard F, Mintz J, Fraser N, Jenkins T, Power C. Unleashing Innovation: Excellent Healthcare for Canada - Report of the Advisory Panel on Healthcare Innovation; 2015. Available at: https://www.canada.ca/content/dam/canada/health-canada/migration/healthy-canadians/publications/health-system-systeme-sante/report-healthcare-innovation-rapport-soins/alt/report-healthcare-innovation-rapport-soins-eng.pdf [Google Scholar]
- 16.Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016;11(1):146. doi: 10.1186/s13012-016-0510-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bearnes RD, Feenstra B, Malcolm J, et al. Virtual care and the pursuit of the quadruple aim: a case example. Healthc Manage Forum. 2020;34(1):9-14. doi: 10.1177/0840470420952468 [DOI] [PubMed] [Google Scholar]
- 18.O’Gorman LD, Hogenbirk JC, Warry W. Clinical telemedicine utilization in Ontario over the Ontario telemedicine network. Telemed J E Health. 2016;22(6):473-479. doi: 10.1089/tmj.2015.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Vera K, Challa P, Liu RH, et al. Virtual primary care implementation during COVID-19 in high-income Countries: a scoping review. Telemed J E Health. 2021. doi: 10.1089/tmj.2021.0377 [DOI] [PubMed] [Google Scholar]
- 20.LeBlanc M, Petrie S, Paskaran S, Carson DB, Peters PA. Patient and provider perspectives on eHealth interventions in Canada and Australia: a scoping review. Rural Remote Health. 2020;20(3):5754. doi: 10.22605/rrh5754 [DOI] [PubMed] [Google Scholar]
- 21.Canadian Medical Association . What Canadians think about virtual health care. Canadian Medical Association. 2020. Available at: https://www.cma.ca/sites/default/files/pdf/virtual-care/cma-virtual-care-public-poll-june-2020-e.pdf [Google Scholar]
- 22.Canada Health Infoway . Canadian digital health survey 2021: what Canadians think. Canada Health Infoway. 2021. Available at: https://www.infoway-inforoute.ca/en/component/edocman/4011-canadian-digital-health-survey-2021-what-canadians-think/view-document?Itemid=101 [Google Scholar]
- 23.Breton M, Sullivan EE, Deville-Stoetzel N, et al. Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Fam Pract. 2021;22(1):192. doi: 10.1186/s12875-021-01543-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glauser W. Virtual care has potential to fragment primary care and disturb continuity of care, warn doctors. CMAJ. 2019;191(37):E1038-E1039, doi: 10.1503/cmaj.1095796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hardcastle L, Ogbogu U. Virtual care: enhancing access or harming care? Healthc Manage Forum. 2020;33(6):288-292. doi: 10.1177/0840470420938818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization . WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. World Health Organization; 2019. [PubMed] [Google Scholar]
- 27.World Health Organization . Global Strategy on Digital Health 2020-2025. World Health Organization; 2021. [Google Scholar]
- 28.Brunet F, Malas K, Desrosiers ME. Will telemedicine survive after COVID-19? Healthc Manage Forum. 2021;34(5):256-259. doi: 10.1177/08404704211031264 [DOI] [PubMed] [Google Scholar]
- 29.Bhatia RS, Chu C, Pang A, Tadrous M, Stamenova V, Cram P. Virtual care use before and during the COVID-19 pandemic: a repeated cross-sectional study. CMAJ Open. 2021;9(1):E107-E114. doi: 10.9778/cmajo.20200311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chu C, Cram P, Pang A, Stamenova V, Tadrous M, Bhatia RS. Rural telemedicine use before and during the COVID-19 pandemic: repeated cross-sectional study. J Med Internet Res. 2021;23(4):e26960. doi: 10.2196/26960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glauser W. Virtual care is here to stay, but major challenges remain. CMAJ. 2020;192(30):E868-E869. doi: 10.1503/cmaj.1095884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baumgart DC. Digital advantage in the COVID-19 response: perspective from Canada’s largest integrated digitalized healthcare system. NPJ Digit Med. 2020;3(1):114. doi: 10.1038/s41746-020-00326-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson C, Dupuis JB, Goguen P, Grenier G. Changes to telehealth practices in primary care in New Brunswick (Canada): a comparative study pre and during the COVID-19 pandemic. PLoS One. 2021;16(11):e0258839. doi: 10.1371/journal.pone.0258839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193(6):E200-E210. doi: 10.1503/cmaj.202303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rush KL, Seaton C, Li E, Oelke ND, Pesut B. Rural use of health service and telemedicine during COVID-19: The role of access and eHealth literacy. Health Informatics J. 2021;27(2):14604582211020064. doi: 10.1177/14604582211020064 [DOI] [PubMed] [Google Scholar]
- 36.Canada Health Infoway . Canadians’ Health Care Experiences during COVID 19: Uptake of Virtual Care; 2022. Available at: https://www.infoway-inforoute.ca/en/component/edocman/3828-canadians-health-care-experiences-during-covid-19/view-document [Google Scholar]
- 37.Mehrotra A, Bhatia RS, Snoswell CL. Paying for telemedicine after the pandemic. JAMA. 2021;325(5):431-432. doi: 10.1001/jama.2020.25706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hart C. Doing a Literature Review: Releasing the Social Science Research Imagination. SAGE Publications; 1998. [Google Scholar]
- 39.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 40.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 41.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 43.Alami H, Gagnon MP, Fortin JP. Some multidimensional unintended consequences of telehealth utilization: a multi-project evaluation synthesis. Int J Health Policy Manage. 2019;8(6):337-352. doi: 10.15171/ijhpm.2019.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGrail KM, Ahuja MA, Leaver CA. Virtual visits and patient-centered care: results of a patient survey and observational study. J Med Internet Res. 2017;19(5):e177. doi: 10.2196/jmir.7374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Canada Health Infoway . 2018 Canadian physician survey: physicians’ use of digital health and information technologies in practice. Canada Health Infoway. 2018. Available at: https://www.infoway-inforoute.ca/en/component/edocman/3643-2018-canadian-physician-survey/view-document?Itemid=101 [Google Scholar]
- 46.Doak S, Schwager A, Hensel JM. Exposure to and attitudes regarding electronic healthcare (e-Health) among physician assistants in Canada: a national survey study. Health Soc Care Community. 2020;28(3):1049-1057. doi: 10.1111/hsc.12938 [DOI] [PubMed] [Google Scholar]
- 47.Kelley LT, Phung M, Stamenova V, et al. Exploring how virtual primary care visits affect patient burden of treatment. Int J Med Inform. 2020;141:104228. doi: 10.1016/j.ijmedinf.2020.104228 [DOI] [PubMed] [Google Scholar]
- 48.Mangin D, Parascandalo J, Khudoyarova O, Agarwal G, Bismah V, Orr S. Multimorbidity, eHealth and implications for equity: a cross-sectional survey of patient perspectives on eHealth. BMJ Open. 2019;9(2):e023731. doi: 10.1136/bmjopen-2018-023731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Canadian Radio – Television and Telecommunications Commission . Broadband fund: closing the digital divide in Canada. Government of Canada. 2021. Available at: https://crtc.gc.ca/eng/internet/internet.htm [Google Scholar]
- 50.Statistics Canada . Data from: smartphone use and smartphone habits by gender and age group. 2018. Ottawa, ON. [Google Scholar]
- 51.Statistics Canada . Data from: dwelling characteristics and household equipment at time of interview, Canada, regions and provinces. 2021. Ottawa, ON. [Google Scholar]
- 52.Statistics Canada . Access to the Internet in Canada, 2020; 2021. Accessed March 9, 2022. Available at: https://www150.statcan.gc.ca/n1/daily-quotidien/210531/dq210531d-eng.pdf [Google Scholar]
- 53.Owens B. Telemedicine on the rise but lagging in Canada. CMAJ. 2018;190(38):E1149-E1150. doi: 10.1503/cmaj.109-5634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.CBC News . N.L. health-care cyberattack is worst in Canadian history, says cybersecurity expert. Canadian Broadcasting Corporation/Radio-Canada; 2022. Available at: https://www.cbc.ca/news/canada/newfoundland-labrador/nl-cyber-attack-worst-canada-1.6236210. Accessed March 4, 2022. [Google Scholar]
- 55.Eneas B. eHealth cyberattack affected millions of files, was one of Sask.’s worst breaches ever: privacy commissioner. CBC News. CBC/Radio-Canada; 2021. Available at: https://www.cbc.ca/news/canada/saskatchewan/privacy-commissioner-ehealth-ransomware-attack-1.5866119. Accessed January 8, 2021. [Google Scholar]
- 56.Federation of Medical Regulatory Authorities of Canada . Framework on telemedicine. Ottawa, ON: Federation of Medical Regulatory Authorities of Canada; 2019. [Google Scholar]