Mini et al. published an article that named “Use of the ductal curvature index to assess the risk of ductal stenting in patients with duct-dependent pulmonary circulation” (1). Patent ductus arteriosus stenting is used as an alternative to surgical shunt procedures in newborns with pulmonary atresia. Ductus arteriosus in pulmonary atresia with some congenital heart defects such as pulmonary atresia and ventricular septal defect/tetralogy of Fallot, pulmonary atresia and transposition of great arteries/congenital corrected transposition of the great arteries, and pulmonary atresia and single ventricle/isomerism are very bizarre. This kind of patent ductus arteriosus has increased tortuosity and curvature (1,2). Tortuous vessels have various phenotypes such as curving, angulation, looping and increased coils formation (3). Increased tortuosity makes very difficult of stenting the patent ductus. To determine the difficulty level of ductus stenting, some concepts like such as tortuosity index, curvature index have been transferred to pediatric interventional cardiology from adult cardiology. However, there is a confusion about the use of tortuosity index and curvature index at the article.
In the retrospective analysis, the authors calculated the ductal curvature index to contribute to risk stratification of ductal stenting procedures. And they found that the ductal curvature index ≥0.45 was showing a high-risk group, in which procedures is associated with some complications or risk of early surgery (1). But unfortunately, they used tortuosity index formula instead of curvature calculation.
The actual curvature rate formula is derived by dividing the length of the outer curvature of the vessel by the centrally measured length of the vessel (4,5). Curvature is defined as inverse radius and is measured any single point along the path. And tortuosity should depend on the severity of curvature. Several types of methods are used to evaluate the tortuosity index. Simply, tortuosity is classified as type I if the vessel is relatively straight, as type II if it has one turn, and as type III if it has multiple turns (3). This evaluation is a basic or quantitative assessment of the tortuosity index. In most publications, the tortuosity is classified in this way, making type III the most challenging group. Moreover, the tortuosity index could be measured qualitative way using its formula. This is what the authors have tried to say in the article, but it given wrongly expressed as the curvature index formula. The formula must be as follows: tortuosity index = (L1 − L2)/L1. By definition, L1 should be the entire length of the ductus to be measured, namely, the actual length, while L2 should be the direct distance from the aortic origin of the ductus to the pulmonary end (6-11). How to take the measurements is shown in Figure 1. I would like to emphasize again that this is the tortuosity index formula, not the curvature index. The formula was adopted from a previously study by Quershi et al. in the text (2). But unfortunately, Qureshi et al. used the formula incorrectly, and more the formula was given the study totally deficient (2).
Figure 1.
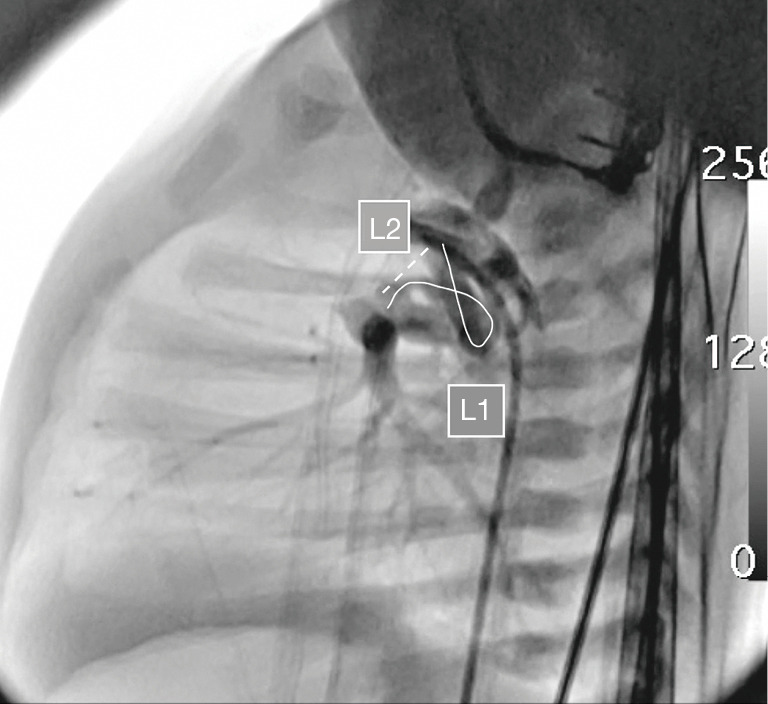
Vertical tortuous ductus arteriosus and tortuosity index measurements are seen in the lateral angiographic view of the tetralogy of Fallot with pulmonary atresia in a cyanotic newborn baby. Length 1 (L1) indicates the actual length of the curved ductus. Length 2 (L2) is the shortest distance between the ductus arteriosus ampulla and the pulmonary entry point.
As a result, what the authors have compared in the table and in the text is the simplified tortuosity index (classified as I, II, III) and the numeric tortuosity index, wrongly called the curvature index. The curvature ratio has not been measured at all. The curvature index term in the entire text should be interpreted by replacing it with the concept of tortuosity index, so as not to misguide the reader.
Conclusions
Tortuosity index and curvature ratio measurement in ductus arteriosus stenting in cyanotic newborns are useful tools in determining difficulty. However, not uncommonly errors are made in formulas related with them. The minireview is written clarify this issue with giving the highlighted the correct formula.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at available at https://tp.amegroups.com/article/view/10.21037/tp-22-107/coif). The author has no conflicts of interest to declare.
References
- 1.Mini N, Schneider MBE, Zartner PA. Use of the ductal curvature index to assess the risk of ductal stenting in patients with duct-dependent pulmonary circulation. Transl Pediatr 2021;10:1307-16. 10.21037/tp-21-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qureshi AM, Goldstein BH, Glatz AC, et al. Classification scheme for ductal morphology in cyanotic patients with ductal dependent pulmonary blood flow and association with outcomes of patent ductus arteriosus stenting. Catheter Cardiovasc Interv 2019;93:933-43. 10.1002/ccd.28125 [DOI] [PubMed] [Google Scholar]
- 3.Han HC. Twisted blood vessels: symptoms, etiology and biomechanical mechanisms. J Vasc Res 2012;49:185-97. 10.1159/000335123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belvroy VM, de Beaufort HWL, van Herwaarden JA, et al. Tortuosity of the descending thoracic aorta: Normal values by age. PLoS One 2019;14:e0215549. 10.1371/journal.pone.0215549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belvroy VM, de Beaufort HWL, van Herwaarden JA, et al. Tortuosity of the Descending Thoracic Aorta in Patients with Aneurysm and Type B Dissection. World J Surg 2020;44:1323-30. 10.1007/s00268-019-05328-w [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain RC, Ezekian JE, Sturgeon GM, et al. Preprocedural three-dimensional planning aids in transcatheter ductal stent placement: A single-center experience. Catheter Cardiovasc Interv 2020;95:1141-8. 10.1002/ccd.28669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dougherty G, Varro J. A quantitative index for the measurement of the tortuosity of blood vessels. Med Eng Phys 2000;22:567-74. 10.1016/S1350-4533(00)00074-6 [DOI] [PubMed] [Google Scholar]
- 8.Ciurică S, Lopez-Sublet M, Loeys BL, et al. Arterial Tortuosity. Hypertension 2019;73:951-60. 10.1161/HYPERTENSIONAHA.118.11647 [DOI] [PubMed] [Google Scholar]
- 9.Wood NB, Zhao SZ, Zambanini A, et al. Curvature and tortuosity of the superficial femoral artery: a possible risk factor for peripheral arterial disease. J Appl Physiol (1985) 2006;101:1412-8. 10.1152/japplphysiol.00051.2006 [DOI] [PubMed] [Google Scholar]
- 10.Zhang X, Luo M, Fang K, et al. Application of 3D curvature and torsion in evaluating aorta tortuosity. Commun Nonlinear Sci Numer Simul 2021;95:105619 10.1016/j.cnsns.2020.105619 [DOI] [Google Scholar]
- 11.Ojha V, Ganga KP, Goyal A, et al. Greater Curvature, Centerline or Straightened Centerline Length - Which length is Most Accurate for Preprocedural Planning in Thoracic Endovascular Aortic Repair? Ann Vasc Surg 2022;78:123-31. 10.1016/j.avsg.2021.05.050 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


