Abstract
Purpose:
The aim of this study was to determine the time at which physeal arrest is achieved after percutaneous physiodesis, and whether immediate postoperative growth rate affects the time to reach physeal arrest.
Methods:
Radiostereometric analysis, with implantation of tantalum balls as radiographic markers on each side of the physes, was used to measure residual longitudinal growth in 21 children (10 boys and 11 girls) after percutaneous physiodesis for leg length discrepancy or extreme tall stature. In total, 25 femoral and 20 tibial physes were operated on. Median age at surgery was 13.9 years (range = 11.4–16.1). Radiostereometric analysis was performed postoperatively and after 3, 6, 9, 12, 26, and 52 weeks. Longitudinal growth rate <50 µm per week was defined as physeal arrest. Descriptive statistics were used for evaluation.
Results:
Physeal arrest was obtained in 19 of the 21 children (40 physes) within 12 weeks postoperatively. One child was reoperated on in three out of four physes because of continued growth, and in one child, delayed physeal arrest was present at 26 weeks postoperatively. Time to physeal arrest was longer in physes with a higher immediate postoperative growth rate.
Conclusion:
Postoperative follow-up with radiostereometric analysis at 12 and 15 weeks can determine whether physeal arrest has been achieved. The immediate postoperative growth rate after physiodesis seems to affect the time to physeal arrest. This implies that the risk for complications is greater for children during an accelerated growth period, for example, in boys, younger children and in distal femoral physes.
Level of evidence:
level III.
Keywords: Percutaneous physiodesis, physeal arrest, radiostereometric analysis, leg length discrepancy, tall stature
Introduction
Percutaneous physiodesis around the knee is widely used for treating leg length discrepancy (LLD) and has also been used for treating expected extremely tall stature. 1 There is a risk that complete physiodesis does not occur, which can result in malalignment or failed length correction.2–5 For this reason, we routinely follow children treated with percutaneous physiodesis postoperatively with radiostereometric analysis (RSA) until physeal arrest is achieved. RSA is a very precise technique with errors of measurements of translation <50 µm for this specific follow-up.6,7 The distal femoral physis has a higher growth rate than the proximal tibial physis. It is therefore reasonable to assume that it would take a longer time to achieve physeal arrest in the distal femur than in the proximal tibia. Young children have more residual growth than older children, which could mean that it would take a longer time to achieve physeal arrest in younger children. Furthermore, boys grow at a faster rate than girls, which could mean that girls reach physeal closure sooner than boys. The aim of this study was to measure the time between physiodesis and physeal arrest in relation to the type of physis (femur or tibia), sex, and age by RSA and to create an algorithm for follow-up after physiodesis.
Material and methods
Twenty-one children (10 boys, 11 girls, 25 femoral physes, 20 tibial physes) underwent percutaneous physiodesis under fluoroscopy using an 8-mm drill. Median age at surgery was 13.9 years (girls = 11.4–15.6; boys = 12.4–16.1). The indication for surgery was LLD in fifteen children and extremely tall stature in six children. To facilitate radiostereometric follow-up with segment motion analysis, tantalum balls with a diameter of 0.8 mm were inserted percutaneously using a stainless-steel cannula with a beveled tip and a hand-operated piston. Three medial and three lateral markers were inserted in a triangular pattern in both the metaphysis and the epiphysis on both sides of the growth plate (Figure 1). RSA was used to determine the three-dimensional skeletal dynamics of the epiphysis relative to the metaphysis, which indicated the rate of growth retardation. 6 Each RSA examination was performed with the patient in the supine position using two 90 degree-angulated roentgen tubes. This position facilitated simultaneous exposure of the knee with the implanted tantalum markers to a combined reference and calibration device with similar tantalum markers placed at known positions on two separate unipolar films. The two-dimensional distances between the images of the tantalum markers on the two films provided the input data for computerized conversion to a three-dimensional coordinate system using UmRSA software (RSA BioMedical, Umeå, Sweden; rsabiomedical.com). Thereafter, the three-dimensional dynamics of growth retardation between consecutive RSA examinations could be calculated. RSA was performed postoperatively and after 3, 6, 9, 12, 26, and 52 weeks. Physeal arrest was defined as a longitudinal growth rate <50 µm per week, which is the lower limit of detection of the method. 7
Figure 1.

Radiostereophotogrammetric analysis postoperatively of patient no. 5. The tantalum markers in the epiphysis and metaphysis of both tibia and femur are marked with a circle. Additional markers in the image are from the reference and calibration device.
Statistics
Descriptive statistics were performed using mean or median and range for continuous variables and absolute numbers and percentages for categorical and ordinal variables. The results are presented with interquartile range (IQR). To have an equal number of patients in the groups compared, an initial growth rate below or above 95 µm/week and age below or above 13.9 years were chosen as limits.
Results
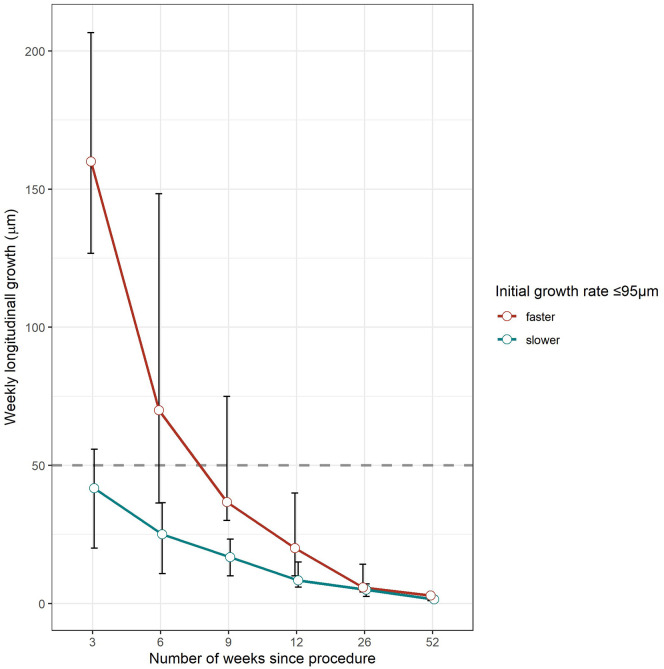
The median immediate postoperative growth rate (at 3 weeks postoperatively) was 95 µm/week (range = 3.3–276.7 µm/week) (Table 1). The first patient in the series continued to grow in three out of four operated physes. The distal femoral physis of the left leg went to physeal arrest after 26 weeks (additional RSA controls were performed at 21 and 36 weeks due to the continued growth). The other three physes continued to grow and underwent a re-physiodesis with the Blount staples 38 weeks after the primary drill physiodesis. Continued RSA analyses confirmed physeal arrest in all physes 3 weeks after the reoperation. In one patient (no. 14), the distal femoral physis stopped growing at 26 weeks. In all remaining children, physeal arrest occurred within 12 weeks (tibia median, 6 weeks; femur median, 9 weeks) (Table 1). Physes with immediate postoperative longitudinal growth rate >95 μm/week showed a median growth rate with IQR <50 μm/week at 12 weeks postoperatively, while those with postoperative growth rate ≤95 μm/week stopped correspondingly at 6 weeks postoperatively (Figure 2). Femoral physes, boys, and children <14 years of age at the time of surgery showed a median growth rate with IQR <50 μm/week at 12 weeks postoperatively. Children ≥14 years of age reached the desired median growth rate at 9 weeks, while for girls and tibial physes, this occurred at 6 weeks (Figures 3–5).
Table 1.
Individual postoperative growth rates after percutaneous physiodesis.
| Patient number | Age at operation (years, months) | Male/female | Tibia = T, femur = F | Longitudinal growth µm (in bold first time <50 µm/week) | |||||
|---|---|---|---|---|---|---|---|---|---|
| 3 weeks | 6 weeks | 9 weeks | 12 weeks | 26 weeks | 52 weeks | ||||
| 1 | 12.4 | M | T | 166.0 | 150.0 | 147.0 | 177.0 | 230.0 | <50.0* |
| M | F | 217.0 | 230.0 | 253.0 | 270.0 | 316.0 | <50.0* | ||
| M | T | 173.0 | 180.0 | 187.0 | 217.0 | 222.0 | <50.0* | ||
| M | F | 230.0 | 187.0 | 200.0 | 163.0 | 27.0 | <50.0 | ||
| 2 | 15.1 | M | F | 160.0 | 36.0 | 23.0 | 6.7 | 2.5 | 2.9 |
| 3 | 13.1 | M | T | 140.0 | 20.0 | 13.3 | 20.0 | 9.2 | 5.4 |
| 4 | 12.7 | M | T | 26.7 | 26.7 | 20.0 | 23.0 | 3.3 | 1.7 |
| M | F | 53.3 | 53.3 | 10.0 | 10.0 | 2.5 | 2.9 | ||
| M | T | 10.0 | 10.0 | 3.3 | 0.0 | 4.2 | 1.2 | ||
| M | F | 83.3 | 83.3 | 23.3 | 13.3 | 5.0 | 2.5 | ||
| 5 | 13.9 | F | T | 30.0 | 3.3 | 16.7 | 13.3 | 3.3 | 0.8 |
| F | F | 103.3 | 46.7 | 30.0 | 16.7 | 5.0 | 1.2 | ||
| 6 | 15.3 | F | F | 46.7 | 96.7 | 36.7 | 30.0 | 5.0 | 2.5 |
| 7 | 11.4 | F | T | 206.7 | 100.0 | 60.0 | 16.7 | 15.8 | 6.2 |
| 8 | 13 | F | F | 237.7 | 146.7 | 50.0 | 26.7 | 2.5 | 0.8 |
| 9 | 15.1 | F | T | 66.7 | 33.3 | 3.3 | 6.7 | 0.8 | 0.4 |
| F | F | 126.7 | 70.0 | 73.3 | 13.3 | 0.6 | 6.7 | ||
| F | T | 60.0 | 30.0 | 6.7 | 6.7 | 2.5 | 0.4 | ||
| F | F | 103.3 | 70.0 | 36.7 | 6.7 | 14.2 | 1.7 | ||
| 10 | 14 | F | T | 13.3 | 36.7 | 10.0 | 6.7 | 8.3 | 0.4 |
| F | F | 3.3 | 20.0 | 3.3 | 6.7 | 8.3 | 3.8 | ||
| F | T | 13.3 | 10.0 | 26.7 | 13.3 | 14.2 | 2.5 | ||
| F | F | 20.0 | 10.0 | 16.7 | 3.3 | 5.0 | 1.2 | ||
| 11 | 14.8 | M | F | 126.7 | 126.7 | 30.0 | 30.0 | 5.8 | 0.0 |
| 12 | 14.1 | M | F | 53.3 | 53.3 | 36.7 | 3.3 | 5.8 | 0.4 |
| 13 | 16.1 | M | T | 30.0 | 30.0 | 16.7 | 26.7 | 2.5 | 0.8 |
| M | F | 113.3 | 53.3 | 46.7 | 6.7 | 5.0 | 2.9 | ||
| 14 | 13.8 | M | T | 136.7 | 136.7 | 40.0 | 26.7 | 13.3 | 0.8 |
| M | F | 206.7 | 206.7 | 123.3 | 93.3 | 14.2 | 4.6 | ||
| 15 | 14.1 | M | T | 20.0 | 39.0 | 30.0 | 30.0 | 0.8 | 0.4 |
| M | F | 110.0 | 18.7 | 30.0 | 10.0 | 1.7 | 1.2 | ||
| 16 | 12.1 | F | F | 36.7 | 20.0 | 20.0 | 6.7 | 1.7 | 1.7 |
| 17 | 13.4 | M | T | 210.0 | 42.7 | 30.0 | 23.3 | 9.2 | 0.8 |
| M | F | 276.7 | 153.3 | 76.7 | 40.0 | 4.2 | 2.9 | ||
| 18 | 12.5 | M | F | 3.3 | 3.3 | 53.3 | 20.0 | Missing | 9.6 |
| 19 | 11.5 | F | T | 86.7 | 0.0 | 20.0 | 3.3 | 7.5 | 2.5 |
| F | F | 96.7 | 46.7 | 13.3 | 20.0 | 0.0 | 2.9 | ||
| 20 | 12 | F | T | 56.7 | 13.3 | 13.3 | 3.3 | 6.7 | Missing |
| F | F | 146.7 | 36.7 | 36.7 | 0.0 | 5.0 | Missing | ||
| F | T | 50.0 | 23.3 | 23.3 | 10.0 | 9.2 | Missing | ||
| F | F | 143.3 | 30.0 | 30.0 | 3.3 | 5.8 | Missing | ||
| 21 | 12.8 | F | T | 60.0 | 35.7 | 3.3 | Missing | Missing | Missing |
| F | F | 193.3 | 23.3 | 26.7 | Missing | Missing | Missing | ||
| F | T | 50.0 | 16.0 | 13.3 | Missing | Missing | Missing | ||
| F | F | 170.0 | 33.3 | 16.7 | Missing | Missing | Missing | ||
*Patient no 1 reoperated on both tibia and right femur as a result of the RSA results after 26 weeks.
Figure 2.
Growth rate after physiodesis in relation to immediate postoperative growth rate (at 3 weeks). Growth rate <50 µm/week (the dotted line) is considered physeal arrest. The interquartile range is illustrated by error bars in the figure.
Figure 3.
Growth rate after physiodesis in relation to age. Growth rate <50 µm/week (the dotted line) is considered physeal arrest. The interquartile range is illustrated by error bars in the figure.
Figure 4.
Growth rate after physiodesis for femur and tibia. Growth rate <50 µm/week (the dotted line) is considered physeal arrest. The interquartile range is illustrated by error bars in the figure.
Figure 5.
Growth rate after physiodesis for boys and girls. Growth rate <50 µm/week (the dotted line) is considered physeal arrest. The interquartile range is illustrated by error bars in the figure.
Discussion
Physiodesis is a relatively safe intervention, although complications are potentially serious resulting in malalignment or LLD if they are not identified early. Most centers provide follow-up after physiodesis but only by clinical and radiographic means. In our view, plain radiographs do not provide sufficient information to decide whether the physis is still active (Figure 6(a) and (b)) because it is often still visible on radiographs long after physeal arrest. Subsequent malalignment indicates that physeal growth is not terminated but by then, it is too late for correction by re-physiodesis. Accordingly, we have routinely used RSA for follow-up after percutaneous physiodesis for more than 15 years. Growth arrest after percutaneous physiodesis is not instantaneous, but in almost all cases, physeal growth has stopped within 12 weeks after physiodesis (Table 1 and Figures 2–5). The distal femur normally grows at a faster rate than the distal tibia and boys normally grow faster than girls. The common factor is a higher immediate postoperative growth rate as illustrated in Figures 2–5. This study shows that the growth rate at the time of physiodesis is an important indicator of the time to reach physeal arrest. This suggests that in children in periods of accelerated growth, careful follow-up should be considered to detect continued growth after physiodesis if RSA is not available for follow-up. While the number of patients in this study is relatively small, the method used is very precise,6,7 thereby reducing the number of patients needed for us to achieve significant results.
Figure 6.
Patient no 5. radiographs at (a) 6 weeks and (b) 6 months postoperatively showing visible physes. The tibia physis went to physeal arrest at 3 weeks postoperatively and the femur physis at 6 weeks postoperatively according to the RSA results (Table 1). Even at 6 months, it is not possible to rule out activity in the physis, although signs of physiodesis are present.
In some patients, early reduction in growth rates was followed by accelerating growth (patient no. 1, 5, 6, 10, 15, 18, and 19). A reasonable explanation could be that drilling the physis sometimes results in a small collapse of the physis that would tend to resemble growth retardation. After this early collapse, the physis continues to grow resulting in accelerating growth values. The amount of physis needing to be destroyed using the percutaneous technique is not known. In an RSA study by Gunderson et al., 8 the amount of physis destroyed varied between 17% and 69%. They found a negative correlation between postoperative growth and the amount of physis destroyed. We did not perform computed tomography (CT) scans of the patients in this study, but it could have been of value to determine the relationship between immediate postoperative growth rate and the amount of physis destroyed. In three children, postoperative RSA results are missing due to patient noncompliance. We did not admit these patients for new RSA measurements at that point as we recognized that physeal arrest had already been achieved. Nevertheless, the missing data are a limitation of this study. The statistical analysis focused on physes, not patients. It is likely that measurements of postoperative growth in different physes in the same patient are dependent measurements. We used descriptive statistics instead of a mixed model statistical analysis to overcome this limitation. As a consequence of this study, we now perform RSA after 12 and 15 weeks. If the growth rate is <50 µm/week between 12 and 15 weeks post-surgery, we feel confident to cease follow-up of that patient. If the growth rate is >50 µm/week, we repeat the RSA and decide on a case-by-case basis when to intervene with re-physiodesis (Figure 7). Our suggestion is that RSA is repeated within 6 weeks. If repeated RSA shows no sign of decrease in growth rate, re-physiodesis should be considered.
Figure 7.
Algorithm for follow-up after physiodesis.
Different surgical techniques, that is, the percutaneous screw technique, 9 are likely to demonstrate different lag times to physeal arrest. According to the data in this study, there is some remaining growth following drill physiodesis. However, excluding the one patient who had a reoperation in three out of four physes and the patient with delayed physeal arrest, this growth is very small, median 0.6 mm (range = 0.2–1.8 mm) during follow-up, thus not clinically significant. The use of RSA allows for clinicians to determine the surgical technique with the fewest complications and the least amount of lag following physiodesis.
Acknowledgments
The authors thank Håkan Lejon for computing the RSA data and Axel Ström, MSc for statistical assistance.
Footnotes
Author contributions: M.W. contributed to the data acquisition; analysis; interpretation of data; and writing. M.E contributed to the data acquisition; analysis; and interpretation of data. G.H. contributed to the design of study; data acquisition; analysis; and interpretation of data. H.L.-P. contributed to the design of study; data acquisition; analysis; interpretation of data; and writing.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the Regional and Governmental Funds for Clinical Research FoU.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the local ethical committee 27 October 2020 Dnr 2020-05041.
Informed consent: Informed consent was given to all patients in the study.
References
- 1. Benyi E, Berner M, Bjernekull I, et al. Efficacy and safety of percutaneous epiphysiodesis operation around the knee to reduce adult height in extremely tall adolescent girls and boys. Int J Pediatr Endocrinol 2010; 2010: 740629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scott AC, Urquhart BA, Cain TE. Percutaneous vs modified phemister epiphysiodesis of the lower extremity. Orthopedics 1996; 19(10): 857–861. [DOI] [PubMed] [Google Scholar]
- 3. Kemnitz S, Moens P, Fabry G. Percutaneous epiphysiodesis for leg length discrepancy. J Pediatr Orthop B 2003; 12: 69–71. [DOI] [PubMed] [Google Scholar]
- 4. Blair VP, 3rd, Walker SJ, Sheridan JJ, et al. Epiphysiodesis: a problem of timing. J Pediatr Orthop 1982; 2(3): 281–284. [PubMed] [Google Scholar]
- 5. Makarov MR, Dunn SH, Singer DE, et al. Complications associated with epiphysiodesis for management of leg length discrepancy. J Pediatr Orthop 2018; 38(7): 370–374. [DOI] [PubMed] [Google Scholar]
- 6. Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand Suppl 1989; 60(232): 1–51. [PubMed] [Google Scholar]
- 7. Lauge-Pedersen H, Hägglund G, Johnsson R. Radiostereometric analysis for monitoring percutaneous physiodesis. A preliminary study. J Bone Joint Surg Br 2006; 88(11): 1502–1507. [DOI] [PubMed] [Google Scholar]
- 8. Gunderson RB, Horn J, Kibsgård T, et al. Negative correlation between extent of physeal ablation after percutaneous permanent physiodesis and postoperative growth: volume computer tomography and radiostereometric analysis of 37 physes in 27 patients. Acta Orthop 2013; 84(4): 426–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sidharthan S, Kehoe C, Wang G, et al. Monitoring with tantalum beads demonstrates no clinically significant growth following percutaneous transphyseal screw epiphysiodesis. J Child Orthop 2021; 15(Suppl. 1): 59. [Google Scholar]