Abstract
While mature cystic teratomas are relatively common ovarian neoplasms typically comprising of multiple embryologic cell types, a specific monodermal subtype involving thyroid tissue, struma ovarii, can rarely be seen. This case reviews typical imaging characteristics with MRI and ultrasound of struma ovarii and details possible complications from these masses with intraoperative and histologic correlation.
Introduction:
We report a case of a premenopausal woman who presented with pelvic pain, nausea, and vomiting for three days with subsequent imaging demonstrating struma ovarii complicated by torsion and rupture. Struma ovarii is a subtype of ovarian teratoma, in which monodermal (thyroid) tissue comprises the majority of the tumor. Imaging can suggest a teratoma filled with colloid material. Potential complications include torsion, rupture, and malignant transformation. We share key imaging findings in this case of struma ovarii with torsion, and rupture, which prompted timely surgical intervention.
Case Description:
A 32-year-old woman with no significant past medical history presented with pelvic pain, nausea, and vomiting for three days. She did not exhibit clinical symptoms of hyperthyroidism. Initial ultrasound at outside hospital (images not available) demonstrated a 12 cm “complex adnexal mass” that raised concern for an endometrioma or hemorrhagic cyst, and a magnetic resonance imaging (MRI) exam was recommended.
MRI demonstrated a 10.5 cm solid and cystic left adnexal mass with heterogenous, dependent solid spherical components (Figure 1a), similar to the previously described “boba” sign (1), which describes globules of fat and keratin within a mature cystic teratoma. The dependent “boba” was T2-dark, T1-intermediate signal intensity without diffusion restriction. The dominant cyst was midline with two smaller T2-hypointense structures on the right (Figure 1b). There was no macroscopic fat or enhancement was appreciated within the mass. Additionally, there was mild twisting of the left ovarian vascular pedicle and rupture of the cyst wall with adjacent inflammatory reaction within the peritoneum (Figure 1a). The mass was abnormally located in the midline pelvis, and the uterus was tilted towards the left (Figure 1b). These findings raised concern for ovarian torsion and cyst rupture.
Figure 1.

A picture of boba tea, a popular drink consisting of green or black tea mixed with condensed milk and syrup poured over chewy tapioca balls, otherwise known as boba.
Repeat ultrasound was performed to confirm the diagnosis of ovarian torsion. It showed a multilocular, avascular, hypoechoic mass containing small hyperechoic foci with associated comet tail artifact, suggestive of colloid material (Figure 2). No echogenic plug was seen making the lesion less likely to represent a typical dermoid cyst. Evaluation of the ovarian parenchyma for parenchymal edema and Doppler flow was limited due to large size of the mass. Overall, imaging findings remained suspicious for an atypical dermoid cyst with torsion and rupture.
Figure 2.
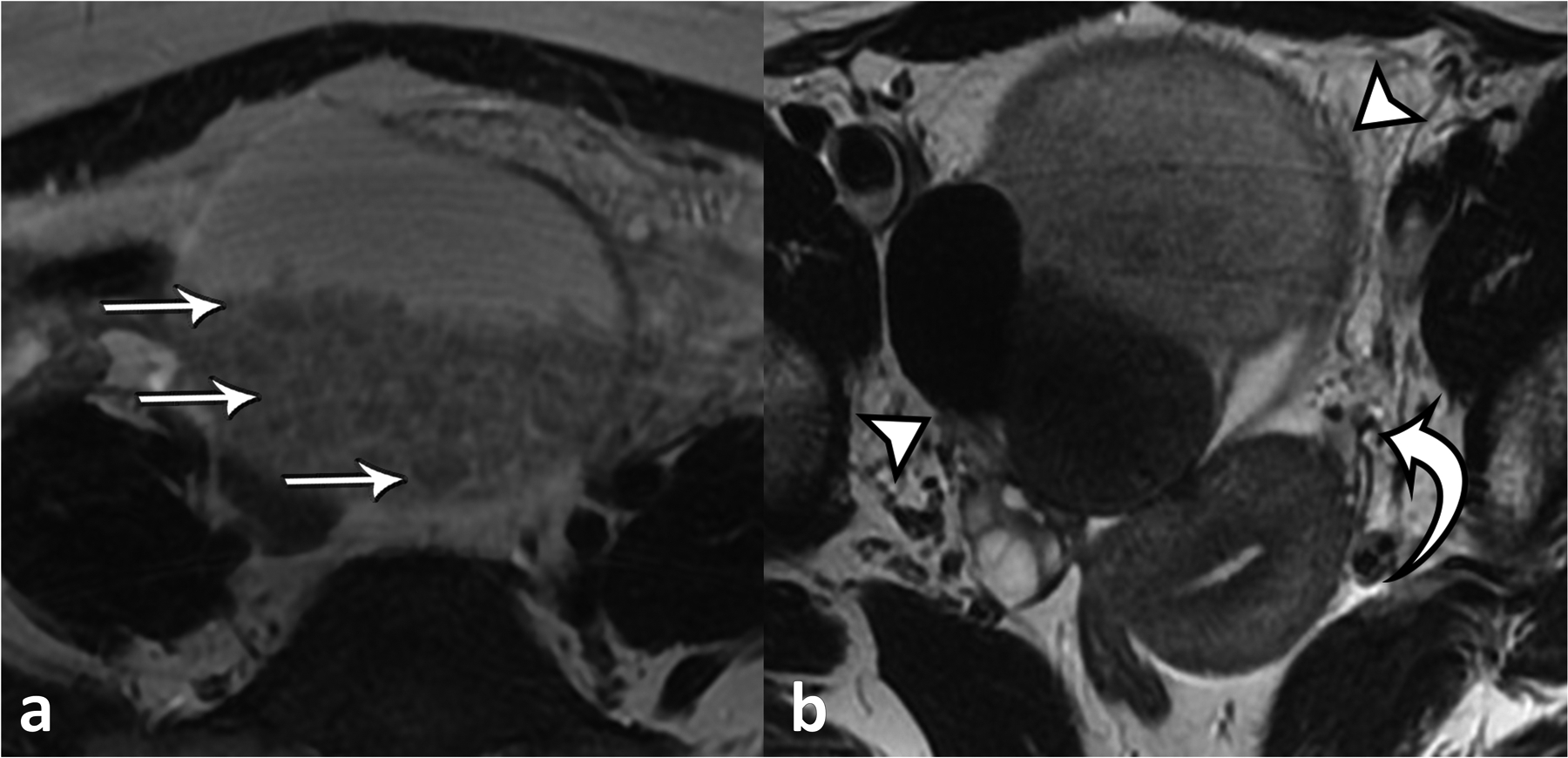
a) Axial T2-weighted MRI of the pelvis demonstrating large mixed cystic and solid mass centered in the midline pelvis with numerous rounded globules (straight arrows) are seen within, reflecting the “boba sign”. The cyst contents exhibited iso- to hypointense signal on T1-weighted imaging and did not show signal drop-out on out-of-phase imaging or fat suppression or internal enhancement was observed (not shown). b) Axial T2-weighted MRI of the pelvis shows a large, multilocular mass with components with iso- and hypointense signal (arrowheads). The uterus is tilted towards the left (curved arrow), indicative of torsion. Engorged gonadal vessels were also present (not shown).
The patient underwent a laparoscopic left ovarian cystectomy, which demonstrated a 10 cm cyst filling the pelvis. Peritoneal inflammation was appreciated, and omental adhesions at the level of the sigmoid colon contained spilled contents from the cyst (Figure 3a). The cyst was filled with clear yellow gelatinous material with solid and crystalline components, compatible with colloid material seen with struma ovarii. Within the dominant cyst, two additional cystic structures were noted, also filled with the same substance. The left adnexa was twisted once at the infundibulopelvic ligament (Figure 3b). The left ovary was viable after cystectomy and was preserved.
Figure 3.
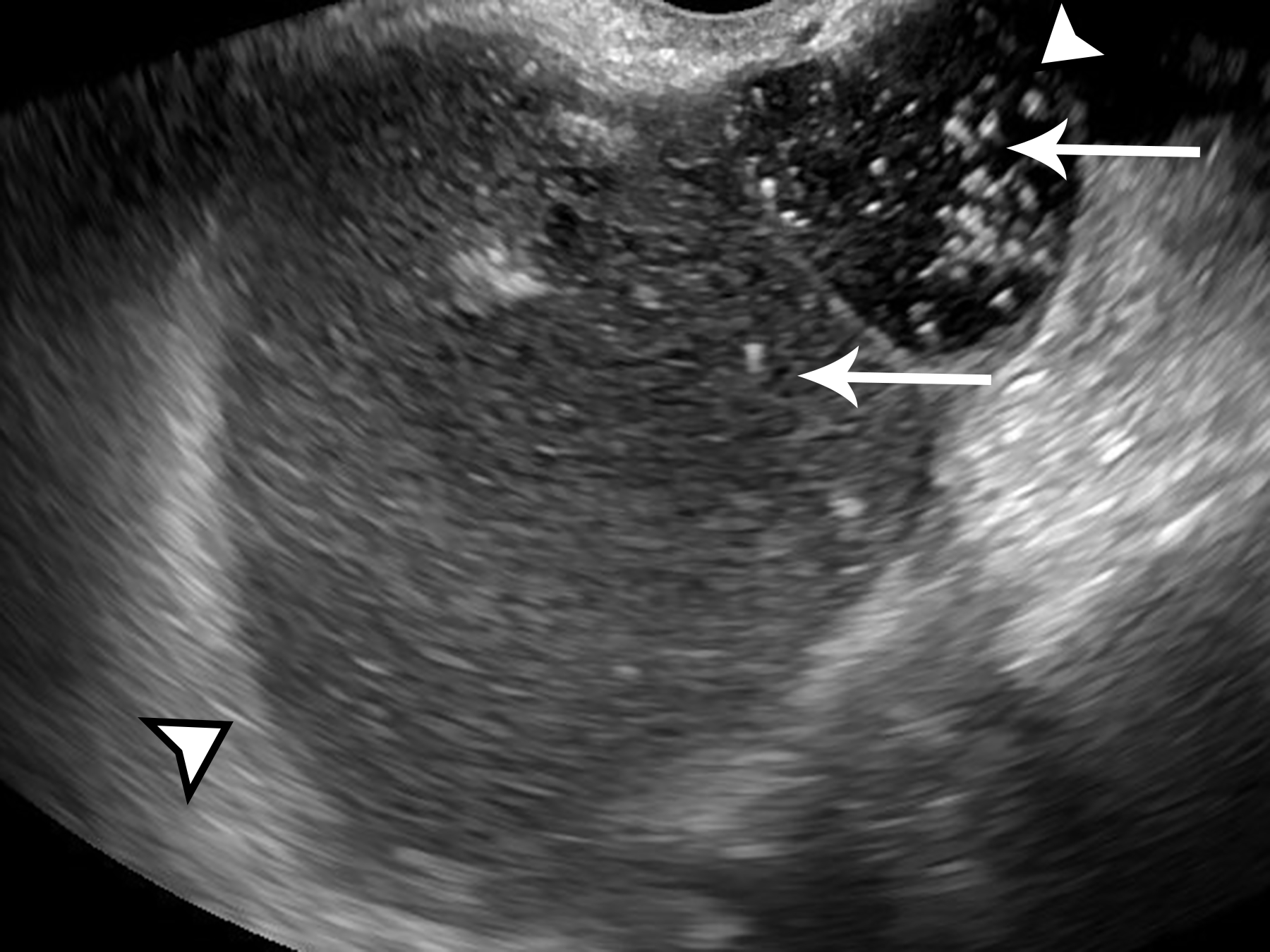
Ultrasound image of the left adnexa in the longitudinal plane, obtained with endovaginal technique, shows multilocular cystic mass with varying internal echogenicity (arrowheads). Multiple echogenic foci with comet-tail artifact are present (arrows).
Histologic analysis revealed thyroid tissue in all components. The cystic spaces contained colloid, and the solid portions demonstrated thyroid follicles (Figure 4). Thyroglobulin and thyroid transcription factor (TTF-1) immunohistochemical staining were positive, confirming the diagnosis. Postoperative laboratory testing demonstrated markedly elevated anti-thyroglobulin level, normal TSH, and a normal thyroid ultrasound. The patient otherwise recovered from the surgery without complication.
Figure 4.
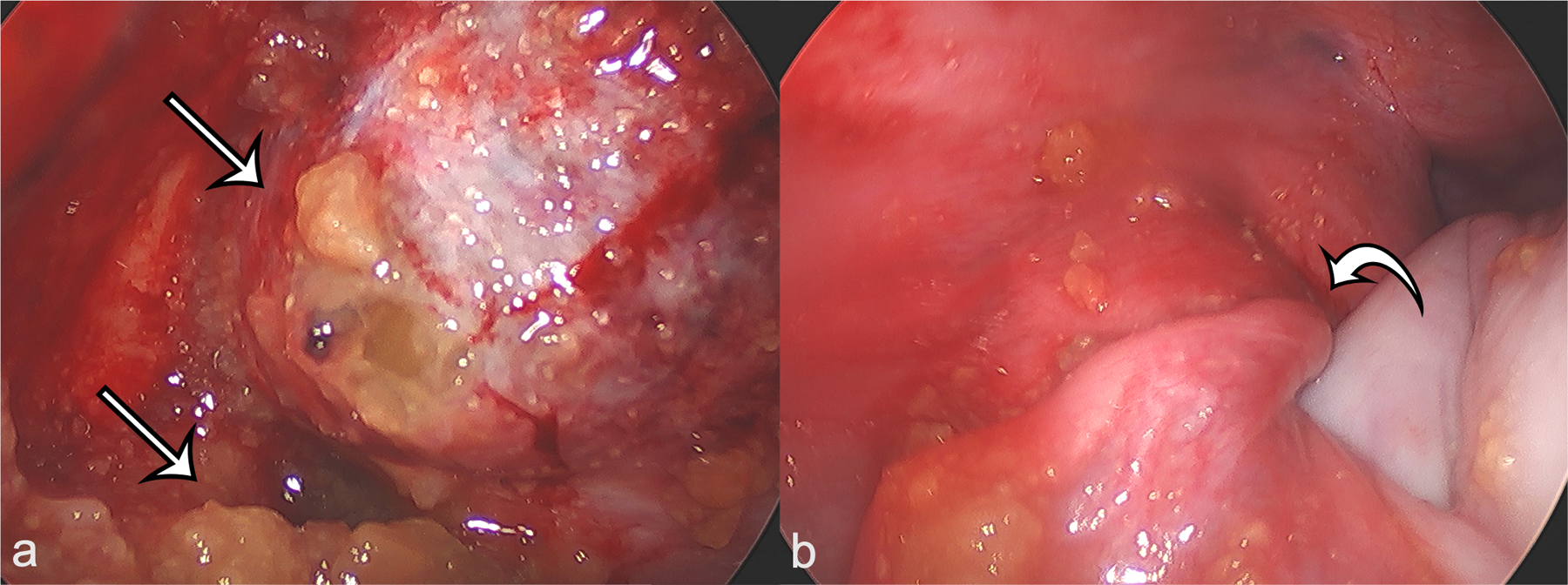
a) Intraoperative laparoscopic image of the left adnexa demonstrates ruptured yellow, gelatinous contents (arrows) of the teratoma, which were confirmed to be thyroid colloid on microscopic review. b) Intraoperative laparoscopic image of the left adnexa demonstrates twisting of the left infundibulopelvic ligament (curved arrow), confirming the diagnosis of ovarian torsion.
Discussion:
The previously described boba sign (1) described floating globules of fat and keratin, with striking similarity to “boba” within a bubble tea, as a pathognomonic sign for a mature cystic teratoma. In this follow-up of the previously described classic sign, we again see spherical debris within a cystic and solid pelvic mass, but layered in a dependent manner. Unlike the previously described case, no internal fat contents were observed. The current case demonstrates that the diagnosis of atypical – in this case, monodermal – teratoma can be suggested by the boba sign and lack of internal enhancement.
Ovarian teratomas are the most common germ cell tumor with mature teratomas representing the most common subtype (2, 3). These benign tumors contain tissue from endodermal, ectodermal, and mesodermal layers, and are often well-differentiated. Malignant transformation is rare, with squamous cell carcinoma accounting for the majority of cases (4). Common diagnostic findings within mature teratomas include the boba sign on MRI, presence of macroscopic fat as evidenced by low density on computed tomography (CT) or fat suppression on MR, dot-dash sign on ultrasound corresponding to hair, or dense calcification on CT or MR corresponding to bone and teeth.
In the monodermal subtype, a single tissue type creates the majority of the mass. Three separate subtypes have been described, neuroectodermal, struma ovarii, and carcinoid (2). In struma ovarii, thyroid tissue is predominant and can be identified both microscopically or macroscopically (5). Struma ovarii can have variable presentation on MRI with cystic spaces demonstrating variable signal intensity on T1- and T2-weighted imaging. The areas that contain colloid material typically demonstrate high density on CT (6) and hypointense signal on both T1- and T2-weighted imaging (5).Typically, struma ovarii has no enhancement or fat. On ultrasound imaging, a comet tail artifact within a large cystic lesion can suggest colloid; however, comet tail artifact in the ovary can be a benign finding or be seen with serous neoplasms (7). Rarely, struma ovarii can be complicated by malignancy such as papillary and follicular thyroid carcinoma.
Potential complications of teratomas can include torsion, rupture, hyperthyroidism, and pseudo-Meig’s syndrome (pleural effusion and ascites related to the teratoma). Our case also highlights several imaging and clinical features of ovarian torsion, which, despite being well-recognized as a complication of large masses, remains challenging both clinically and by imaging, particularly in the presence of large ovarian masses. Findings of torsion present in our case included: pain with an associated neoplasm, abnormal uterine tilt, abnormal position of the left ovary, and twisting of the vascular pedicle (8). In the setting of large ovarian lesions, these key imaging features aid in making the diagnosis of torsion. Additional complications and symptoms of ovarian teratomas can include abdominal pain, vaginal bleeding, abdominal distension, back pain, and frequent urination; tumor rupture may cause acute severe abdominal pain. Rarely, struma ovarii can be a cause for hyperthyroidism (9). This clinical presentation with pelvic pain, nausea and vomiting was concerning and challenging to differentiate between diagnosis of ovarian torsion versus a ruptured ovarian dermoid resulting in chemical peritonitis.
In conclusion, ovarian teratomas are frequently encountered benign neoplasms with several pathognomonic imaging appearances, including the “boba” sign. Our case highlights that the “boba” sign can also apply to struma ovarii, a monodermal subtype of ovarian teratoma that is composed to thyroid tissue and colloid material. Our case also demonstrates several key imaging findings of ovarian teratoma complications – ovarian torsion and cyst rupture – that radiologists should be familiar with, to prompt timely diagnosis and surgical intervention.
Figure 5.
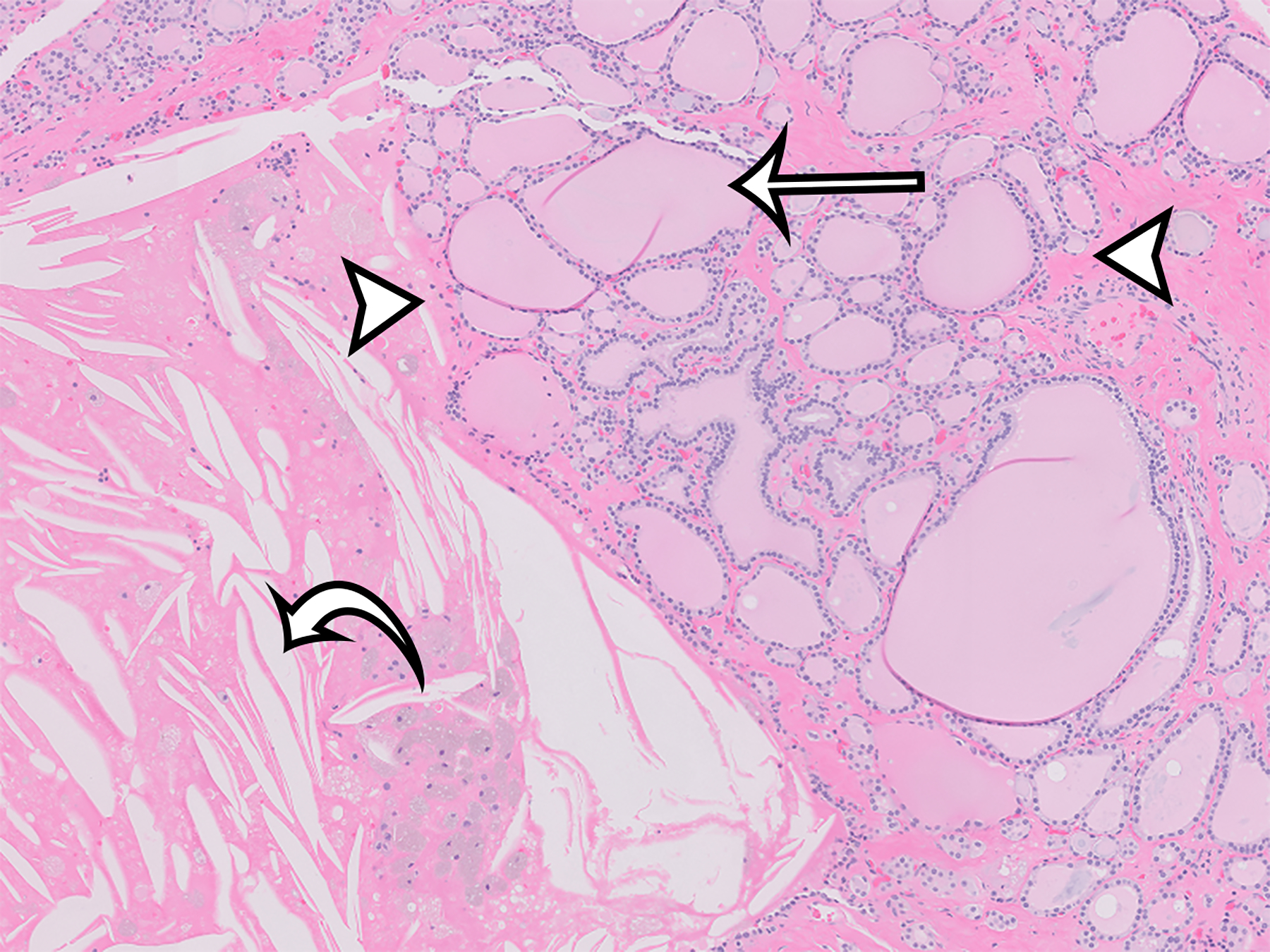
Hematoxylin and eosin stain of the solid portion of the cyst at 5x magnification demonstrates rounded thyroid follicles (arrowheads) containing pink colloid (straight arrow). Cholesterol clefts (curved arrow) indicate areas of degenerative change. Corresponding immunohistochemical stains for thyroglobulin and TTF-1 were positive (not shown).
Funding
This work was supported by the NIBIB T32 grant funding (T32EB001631).
Footnotes
Conflicts of Interest/Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
The authors have no financial or proprietary interests in any material discussed in this article.
References:
- 1.Chang AY, Sun DC, Ohliger MA, Abuzahriyeh T, Choi HH. Boba sign: a novel sign for floating balls within a mature cystic teratoma. Abdom Radiol [Internet] Springer; 2020. [cited 2021 Apr 15];45(9):2931–2933. Available from: 10.1007/s00261-020-02647-8 [DOI] [PubMed] [Google Scholar]
- 2.Saleh M, Bhosale P, Menias CO, et al. Ovarian teratomas: clinical features, imaging findings and management [Internet]. Abdom Radiol Springer; 2021. [cited 2021 Apr 15]. p. 3. Available from: 10.1007/s00261-020-02873-0 [DOI] [PubMed] [Google Scholar]
- 3.Outwater EK, Siegelman ES, Hunt JL. Ovarian Teratomas: Tumor Types and Imaging Characteristics. Radiographics [Internet] Radiological Society of North America Inc; 2001. [cited 2021 Apr 15];21(2):475–490. Available from: www.rsna.org [DOI] [PubMed] [Google Scholar]
- 4.Hackethal A, Brueggmann D, Bohlmann MK, Franke FE, Tinneberg HR, Münstedt K. Squamous-cell carcinoma in mature cystic teratoma of the ovary: systematic review and analysis of published data [Internet]. Lancet Oncol Lancet Publishing Group; 2008. [cited 2021 Apr 15]. p. 1173–1180. Available from: https://pubmed.ncbi.nlm.nih.gov/19038764/ [DOI] [PubMed] [Google Scholar]
- 5.Yamashita Y, Hatanaka Y, Takahashi M, Miyazaki K, Okamura H. Struma ovarii: MR appearances. Abdom Imaging [Internet] Springer; 1997. [cited 2021 Apr 15];22(1):100–102. Available from: https://link.springer.com/article/10.1007/s002619900150 [DOI] [PubMed] [Google Scholar]
- 6.Shen J, Xia X, Lin Y, Zhu W, Yuan J. Diagnosis of Struma ovarii with medical imaging. Abdom Imaging [Internet] Abdom Imaging; 2011. [cited 2021 Apr 15];36(5):627–631. Available from: https://pubmed.ncbi.nlm.nih.gov/21104246/ [DOI] [PubMed] [Google Scholar]
- 7.Tierney NM, Ward K, O’boyle M, Saenz C. Comet Tail Artifact on Pelvic Ultrasound Associated with Borderline Serous Tumor of the Ovary Case Report. Open J Clin Med Case Rep 2015;1. [Google Scholar]
- 8.Strachowski LM, Choi HH, Shum DJ, Horrow MM. Pearls and Pitfalls in Imaging of Pelvic Adnexal Torsion: Seven Tips to Tell It’s Twisted. Radiographics [Internet] NLM (Medline); 2021. [cited 2021 Apr 15];41(2):625–640. Available from: 10.1148/rg.2021200122 [DOI] [PubMed] [Google Scholar]
- 9.Teale E, Gouldesbrough DR, Peacey SR. Graves’ disease and coexisting struma ovarii: Struma expression of thyrotropin receptors and the presence of thyrotropin receptor stimulating antibodies. Thyroid [Internet] Thyroid; 2006. [cited 2021 Apr 15]. p. 791–793. Available from: https://pubmed.ncbi.nlm.nih.gov/16910883/ [DOI] [PubMed] [Google Scholar]


