Abstract
Non-small cell lung cancer (NSCLC) is the leading cause of death by cancer worldwide. Despite developments in therapeutic approaches for the past few decades, the 5-year survival rate of patients with NSCLC remains low. NSCLC tumor is a complex, heterogeneous microenvironment, comprising blood vessels, cancer cells, immune cells, and stroma cells. Vascular endothelial growth factors (VEGFs) are a major mediator to induce tumor microvasculature and are associated with the progression, recurrence, and metastasis of NSCLC. Current treatment medicines targeting VEGF/VEGF receptor (VEGFR) pathway, including neutralizing antibodies to VEGF or VEGFR and receptor tyrosine kinase inhibitors, have shown good treatment efficacy in patients with NSCLC. VEGF is not only an important angiogenic factor but also an immunomodulator of tumor microenvironment (TME). VEGFs can suppress antigen presentation, stimulate activity of regulatory T (Treg) cells, and tumor-associated macrophages, which in turn promote an immune suppressive microenvironment in NSCLC. The present review focuses on the angiogenic and non-angiogenic functions of VEGF in NSCLC, especially the interaction between VEGF and the cellular components of the TME. Additionally, we discuss recent preclinical and clinical studies to explore VEGF/VEGFR-targeted compounds and immunotherapy as novel approaches targeting the TME for the treatment of NSCLC.
Keywords: NSCLC, tumor microenvironment, VEGF/VEGFR pathway, immunotherapy, clinical trials
1. Introduction
Lung cancer is a leading cause of cancer-related death, and non-small cell lung cancer (NSCLC) is the most common type of lung cancer 1. The prognosis of NSCLC remains poor, and the overall recovery and survival rates of patients remain low, as most patients with NSCLC have advanced cancer or extensive metastases before diagnosis 2-4. The tumor microenvironment (TME) of NSCLC is complex, comprising various types of immune cells and vasculature. Vascular endothelial growth factor (VEGF) is mainly secreted by the endothelial cells of blood vessels; however, it can also be generated by the immune cells of the TME, such as tumor-associated macrophages (TAM) 5, tumor-associated neutrophils (TAN) 6, 7, mast cells (MC) 8-10, myeloid-derived suppressor cells (MDSC) 11-13, and natural killer cells (NK) 14, 15. The VEGF is not only linked with multiple functions in angiogenesis but also suppresses immune cells and promotes local and systemic immunosuppression in cancer. In recent years, owing to the successful development of immune checkpoint inhibitors, vaccines, VEGF/VEGF receptor (VEGFR)-targeting compounds, and other immunotherapeutic agents for cancer treatment, a new approach to treat various tumors, which combines anti-angiogenic drugs with immunotherapy, has emerged 16. Emerging evidence demonstrates potential synergistic efficiency between VEGF/VEGFR-targeting compounds and immunotherapy for NSCLC treatment. In the present review, we focus on the angiogenic and non-angiogenic functions of VEGF in NSCLC, in particular, on the interaction between VEGF and the cellular components of the TME. In addition, we discuss recent preclinical and clinical studies to explore VEGF/VEGFR-targeted compounds and immunotherapy as novel approaches targeting the TME for NSCLC treatment.
2. Functions of VEGF/VEGFR in NSCLC
2.1 Angiogenic function: tumor vasculature
VEGF is mainly secreted by tumor cells, some stromal cells, and endothelial cells in the TME 17. The VEGF family comprises several members, including VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, VEGF-F, placental growth factor (PLGF), and endocrine gland-derived VEGF (EG-VEGF) 17, 18.
The members of the VEGF family perform their functions by binding with their receptors. VEGF receptors are categorized into two types: tyrosine kinase receptors (VEGF receptors, VEGFR), which include VEGFR-1, VEGFR-2, and VEGFR-3, and neuropilin receptors (NRPs), which include NRP-1 and NRP-2 19, 20. NRPs are the co-receptors of VEGF; the binding of VEGF and NRPs enhances the stability of the receptor complex 19.
The VEGF family members selectively bind to VEGFR. VEGF-A is the major member of the VEGF family for angiogenesis; it is expressed in all vascular tissues, macrophages, tumor cells, and other cells 21, 22. Moreover, it can bind to both VEGFR-1 and VEGFR-2, but it primarily binds to the latter for dimerization, autophosphorylation, and activation, thereby becoming crucial in downstream signaling, causing the proliferation and migration of endothelial cell, and performing angiogenic functions. 23-25.
VEGF-A binds to VEGFR-2 and activates phospholipase C γ (PLC-γ). Activated PLC-γ can hydrolyze the membrane component phosphatidylinositol-4,5-bisphosphate (PI(4,5)P2) to produce inositol triphosphate (IP3) and diacylglycerol (DAG). IP3 induces intracellular Ca2+ release and improves vascular permeability. Ca2+ causes protein kinase C (PKC) to bind and polymerize to the plasma membrane, which is activated by DAG; PKC can also act as an upstream activator of the Raf1-MEK1/2-ERK1/2 pathway, which is central to endothelial cell proliferation 26. The binding of VEGF-A to VEGFR-2 also phosphorylates phosphoinositide 3-Kinase (PI3K), and the activated PI3K binds to the substrate PIP2 converting it to phosphatidylinositol 3-phosphate (PIP3). PIP3 induces serine/threonine-specific protein kinase (AKT) phosphorylation, which activates endothelial nitric oxide synthase (eNOS) to produce nitric oxide (NO) and induces endothelial cell proliferation and migration 27, 28 (Figure 1).
Figure 1.
The VEGF-VEGFR signaling pathway. VEGF-A binds to VEGFR-2 for dimerization, autophosphorylation, and activation leading to endothelial cell survival, proliferation, permeability, and migration. mTOR, mammalian target of rapamycin; MAPK, mitogen-activated protein kinase; MEK, MAP kinase kinase.
VEGF-B mainly binds to VEGFR-1 and NRP-1, and plays an important role in tumor angiogenesis and in the improvement of ischemic conditions 29, 30. VEGF-C and VEGF-D mainly bind to VEGFR-3 and participate in lymphangiogenesis 30, 31. VEGF-D is associated with tumor metastasis to regional lymph nodes 32-34. Furthermore, PIGF mainly binds to VEGFR-1 and regulates the growth and maturation of blood vessels by regulating endothelial cell and parietal cell proliferation 35 (Figure 1).
2.2 Non-angiogenic function: role of VEGF in the functions of TME cell components in NSCLC
2.2.1 VEGF and cancer cells
Evidence suggests that VEGF acts in tumors not only by promoting angiogenesis but also by directly working on cancer cells 36. VEGF can promote tumor development and progression by interacting with receptors expressed on tumor cells through autocrine and/or paracrine mechanisms 37. In addition to tyrosine kinases, NRPs can regulate the function and transportation of growth factor receptors and integrins, thus playing a crucial role in mediating VEGF action on tumor cells 37. Autocrine VEGF in lung cancer has been shown to activate mitogen-activated protein kinase (MEK)/extracellular signal-regulated kinase (ERK) and PI3K/AKT signaling pathways to promote cell proliferation in NSCLC; additionally, NRP1 plays a central role in regulating VEGF-driven NSCLC cell proliferation 38. However, studies showed that blocking endogenous VEGF with bevacizumab, the VEGF antibody, did not inhibit NSCLC cell line growth, suggesting that VEGF alone does not maintain lung cancer cell proliferation in vitro 39, 40. We believe that the development of NSCLC is caused by a combination of factors in the TME. Therefore, in a single cell line without tumor angiogenesis or TME, blocking VEGF alone does not effectively inhibit tumor cell growth. it is likely that VEGF-VEGFR-targeted therapy also acts on the TME to reverse the immunosuppression therein, thus inhibiting tumor growth. Therefore, we infer that combining immunotherapy with VEGF-VEGFR-targeted therapy may exert better therapeutic effects on NSCLC.
2.2.2 VEGF and T cells
Tumor cells evade immune defence by suppressing T cell function, for example, by upregulating the expression levels of T cell checkpoints 41, 42. VEGF-A enhances the expression of PD-1 and other suppressive checkpoints, such as CTLA-4, on the surface of T cells, and suppresses the activity of CD8+ T cell, manifesting as a progressive state of dysfunction leading to the blocking of the effector function of T cells 43-45. The inhibitory functions of checkpoints could be reversed by anti-angiogenic agents, as when VEGF is blocked, tumor blood vessels decrease and tumor tissue hypoxia is induced, which in turn activates hypoxia-inducible factor (HIF-1α), and promotes cytokine production to activate CD8+ T cells 43-45. However, recently, studies have reported that tumor hypoxia, angiogenesis, and immunosuppression can modulate each other, thus promoting tumor progression and compromising the clinical effectiveness of antitumor therapy 46.
Furthermore, VEGF can directly inhibit T cell function. Continuous infusion of recombinant VEGF in non-tumor patients resulted in a decrease in the number of T cells and the ratio of T to B cells in lymph nodes and spleens 47. Additionally, recombinant VEGF-infused mice showed smaller thymus compared with control group mice infused with phosphate-buffered saline, indicating the immune suppressing quality of VEGF 48. In another study, inhibiting VEGF activity by endostatin, a VEGF specific antibody, enhanced infiltration of mature CD8+ T cells and reduced the number of immunosuppressive cells in tumors 49. VEGF-A directly inhibits T cell proliferation and cytotoxic activity through VEGFR-2 in advanced ovarian cancer 50. In addition, VEGF-A has been shown to induce the expression of the transcription factor thymocyte selection-associated high mobility group box (TOX) in T cells, which drives a depletion-specific transcriptional program in T cells. In the case of PD-1 blockade resistance, combined blockade of PD-1 and VEGF-A activities restores the anti-tumor function of T cells, resulting in better tumor control 51 (Figure 2A).
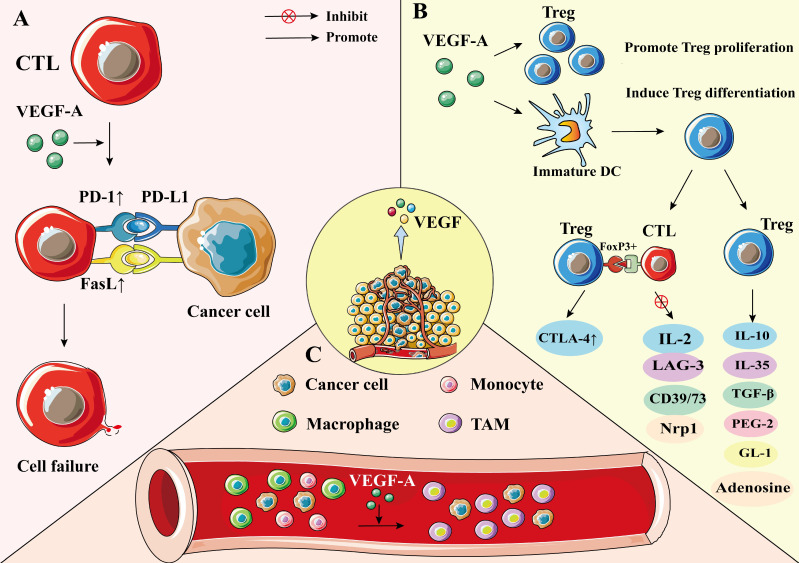
Figure 2.
The effect of VEGF on CTL, Treg, and TAM. A) VEGF-A enhances the expression of PD-1 and FasL on CTL, thereby promoting CTL cell failure and leading to immunosuppression. B) VEGF-A can make Treg recruited in the tumor microenvironment and increase the number of Treg. VEGF-A can induce Treg differentiation by producing immature DC. Treg cells inhibit the activation of target cells through FoxP3+ direct contact; up-regulate the expression of CTLA-4; inhibit the expression of IL-2, LAG-3, CD39/73, and NRP-1; or cause immunosuppression by producing soluble immunosuppressive molecules. C) Under the action of VEGF-A, monocytes/macrophages in the blood are gathered around tumor cells and differentiate into TAM. The M2 cells in TAM can promote tumorigenesis and development.
In addition to directly regulating T cell function, VEGF also can suppress T cell function by regulating Fas ligand (FasL) levels, which is upregulated by VEGF-A in the TME 52, 53. FasL is expressed on the surface of T cells and in tumor endothelium; however, it is not seen in a normal vascular system 48, 54. In human tumors, the expression of FasL in endothelial cells leads to the loss of CD8+ T cells 48, 54. In mice, endothelium-secreted FasL suppresses the infiltration of T cells in tumors, thus promoting tumor growth 48, 54 (Figure 2A).
2.2.3 VEGF and Treg
Treg cells are a major subset of CD4+ T cells. The characteristic phenotype of Treg cells is CD25+ CD4+ FoxP3+ T cell 55, 56. Some preclinical and clinical studies have shown that Treg cells are one of the most common immunosuppressive cell types in tumors 57, 58. They hinder immune surveillance against cancer in healthy individuals, prevent patients with tumors from producing effective anti-tumor immunity, and cause the occurrence and development of various malignant tumors, including NSCLC 59. Treg cells negatively regulate immune response through two mechanisms: (1) by direct contact to inhibit the activation of target cells, such as directly up-regulating the expression of CTLA-4 through FoxP3+, thus inhibiting the expression of IL-2, lymphocyte activating protein 3 (LAG-3), CD39/73, and NRP-1 to induce immunosuppression 60, 61, and (2) through a humoral and cytokine secretion mechanism, which involves inducing the production of soluble immunosuppressive molecules, such as IL-10, IL-35, transforming growth factor-β (TGF-β), adenosine, prostaglandin E-2 (PGE-2), or galactose lectin-1 (Gl-1) 60, 61.
In cancer patients, VEGF-A expression was positively correlated with levels of intratumoral Tregs 62. VEGF-A can promote Treg differentiation by inducing immature dendritic cell (DC) numbers 50. Additionally, VEGF-A can directly regulate Treg recruitment in the TME by binding with VEGFR2, which in turn stimulates the proliferation of Treg cells, and enhances the immunosuppressive function 50, 63, 64. Terme et al. reported that tumor-bearing mice show higher expression levels of VEGFR-2 on Treg cells than healthy mice, and that neutralizing VEGFR-2 by specific antibodies can reduce the proportion of Tregs in the spleen of nude mice, indicating that VEGFR-2 signaling plays an important role in regulating Treg functions 65. Furthermore, VEGF-A promotes the infiltration of Treg cells in the TME by binding to NRP-1 66. When the NRP-1 gene was knocked down in T cells, the number of Treg cells decreased, whereas the number of CD8+ T cells increased (Figure 2B) 66.
2.2.4 VEGF and TAM
TAMs are dynamic cells with multiple polarization states; they are important mediators of cancer development and progression 67. TAMs are present in all stages of tumor development, making them the most abundant immune cells in the TEM 68. There are two types of TAMs, M1 and M2 phenotypes. The M1 phenotype exhibits antitumor effects, whereas M2 is involved in promoting tumor progression 69. TAMs cause immunosuppression by producing cytokines, chemokines, growth factors, and triggering the release of suppressive immune checkpoint proteins in T cells 70. Hwang et al. showed that M2 TAM significantly enhanced the expression levels of VEGF-A and VEGF-C of NSCLC cells, whereas M1 TAM only upregulated the expression levels of VEGF-A in NSCLC cells, indicating that TAMs are significantly associated with vascular and lymph angiogenesis, which in turn promotes the progression of NSCLC 5. Additionally, TAM receptors, including Tyro3, Axl, and Mark, bias macrophage polarization toward a pro-tumor M2-like phenotype. These receptors are promising therapeutic targets for tumor-associated macrophages 71.
TAM of the TME is mainly differentiated from bone marrow-derived blood monocytes and monocytic MDSC under the stimulation of tumor cell-secreted cytokines, including VEGF-A, IL-4, and IL-10 68, 72. VEGF-A recruits TAM mainly by binding to VEGFR-1 on the TAM surface 50. TAM expresses PD-L1, which inhibits T cell receptor signaling upon binding to PD-1, leading to T cell inactivation 50. Moreover, M2 macrophages can also release VEGFA, VEGFC, and other growth factors, which may in turn promote cancer progression 70, 73 (Figure 2C).
2.2.5 VEGF and dendritic cells
DCs are antigen-presenting cells and have the strongest antigen presentation ability in vivo 74. DCs can produce cytokines and stimulate the differentiation of effector T and NK cells 75, 76. Therefore, DC dysfunction is one of the mechanisms leading to anti-tumor immunodeficiency.
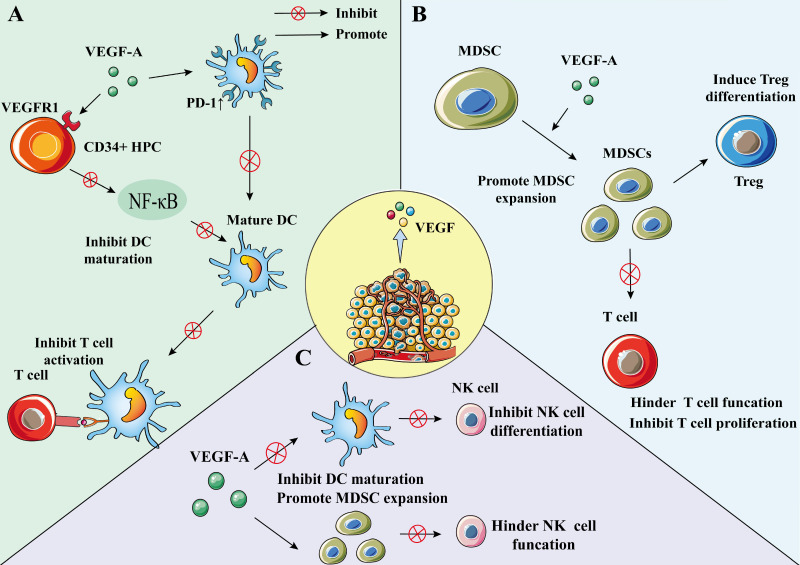
DC can be differentiated from the early stage of hematopoietic progenitor cell (HPC) 77; however, this process may be regulated by VEGF-A 78. Through VEGFR-1, VEGF-A can bind to HPC CD34+ cells and inhibit nuclear factor-κB (NF-κB), which is the activator of transcription factors in these cells, thereby inhibiting the differentiation and maturation of DC 78, 79. VEGF can also inhibit DC function by up-regulating PD-1 80. The inhibiton of DC maturation reduces T cell tumor infiltration and exerts immunosuppressive effect 80. Recent findings suggest that VEGF can impair mature DCs' migration ability and immune function through VEGFR-2-mediated RhoA-cofilin1 pathway 81.
Increased immature DCs in cancer patients are associated with increased VEGF levels, which are involved in mediating DC dysfunction 78. Bevacizumab can affect the maturation and function of DCs in vivo by slightly increasing DC numbers and significantly reducing immature myeloid cell numbers 82. Additionally, bevacizumab can reverse the inhibition of VEGF-induced monocyte differentiation into DC in vitro 83.
An investigation of the relationship between VEGF and DC cells using a mouse model found that recombinant VEGF significantly altered DC growth and development at relevant concentrations, with a reduction in the proportion of mature DCs in lymph nodes and spleens of mice 47.
Furthermore, the results of a clinical study evaluating the relationship between DC infiltration and VEGF expression in NSCLC (132 primary NSCLC treated with surgery) showed that the mean number of infiltrating DCs in the VEGF high expression group was lower than that in the low expression group 84, indicating that VEGF may regulate the infiltration of DC into NSCLC tumor (Figure 3A).
Figure 3.
The effect of VEGF on DC, MDSC, and NK cell. A) VEGF-A can bind to VEGFR1 on CD34+ HPC, inhibit NF-κB, an activator of transcription factors in these cells, and inhibit the differentiation and maturation of DC. VEGF-A can also increase the expression of PD-1 in DC, resulting in a decrease in the number of DCs. To inhibit the activation of T cells by mature DCs. Lead to immunosuppression. B) VEGF-A can promote the expansion of MDSC, and MDSC can inhibit the proliferation of tumor-specific T cells and promote the development of Treg. C) VEGF-A can inhibit the differentiation of NK cells by inhibiting DC maturation. VEGF can also increase the number of MDSCs and inhibit the function of NK cells.
2.2.6 VEGF and MDSC
MDSC is a heterogeneous population comprising immature myeloid cells, which are precursor cells of macrophages, DC, or granulocytes features 85. MDSCs are characterized by bone marrow origin, immaturity, and suppression of immune response 85. They can promote tumor cell survival, angiogenesis, tumor cell invading, and metastases 11, 86. Additionally, MDSC induces immune tolerance and can suppress effector T cells and NK cells to induce immune responses 85, 87. Moreover, MDSC could inhibit the growth of tumor-specific T cells and promote the development of Treg cells, which plays a pivotal role in immunosuppression and immune escape 86, 88, 89. MDSCs are also found to be involved in the differentiation of Treg cells. In cancer patients, an increase in MDSC in peripheral blood causes a decrease in mature DCs 90. Many studies have reported that MDSCs play an important role in mediating a variety of tumor-related immunosuppressive functions and tumor immune escape, including NSCLC 89, 91.
VEGF-A is a factor that can promote the amplification of MDSCs; the use of bevacizumab can inhibit VEGF function and MDSC proliferation 50, 92. Research on the effect of lactones on immune cells in the TME showed that MDSC proportion reduced in both the low- and high-dose endostatin groups compared to the control group 49 (Figure 3B).
2.2.7 VEGF and natural killer cells
NK cells are a subgroup of cytotoxic innate lymphoid cells in the innate immune system and have a unique killing effect on tumor cells 93. VEGF can inhibit the differentiation of NK cells by inhibiting DC maturation 78, 94. Furthermore, VEGF can increase the number of MDSCs and inhibit NK cell function, in turn leading to the phenomenon of immune escape 89, 95, 96.
Studies have shown that NK cells can secrete VEGF-A under hypoxic conditions, which is a characteristic of the TME 97. Under such hypoxic conditions, VEGF secretion is a transient phenomenon because when NK cells return to peripheral blood, this phenomenon can be reversed 97, 98 (Figure 3C).
In summary, VEGF not only promotes tumor growth by promoting angiogenesis but also acts on various immune cells in the TME, which leads to immunosuppression. Therefore, in treating NSCLC, the selection of VEGF-VEGFR-targeted drugs can inhibit tumors from two aspects.
3. VEGF-targeted therapy and immunotherapy for NSCLC
3.1 VEGF/VEGFR inhibitors and antibodies
VEGF is overexpressed in NSCLC; the expression levels are higher in the tumorous than the surrounding normal lung tissue 99. The high expression of VEGF is related to tumor recurrence, low survival rate, metastasis, and death 99, 100. VEGF is essential for tumor growth and immunosuppression. Therefore, targeted drugs that inhibit the VEGF pathway, such as anti-VEGF monoclonal antibodies and tyrosine kinase inhibitors (TKIs), are used for NSCLC treatment.
Over the past few decades, several VEGF inhibitors have been approved for NSCLC treatment. Among them, bevacizumab, a humanized monoclonal immunoglobulin G 1 (IgG1) antibody that can bind to VEGF-A, has shown good efficacy in treating NSCLC 101. Studies show that chemotherapy combined with bevacizumab prolongs progression-free survival (PFS) and overall survival (OS) in patients with NSCLC compared to chemotherapy alone 23. In addition to combination therapy with chemotherapeutics, bevacizumab has also shown encouraging effects in combination with immunotherapy 80. Data from several clinical trials involving the combination of several immune checkpoint inhibitors and bevacizumab show that when combined with immunotherapy, bevacizumab can prolong survival rate 80. Bevacizumab is also approved by the European Medicines Agency and the United States Food and Drug Administration as first-line treatment for advanced, metastatic, or recurrent NSCLC.
Another VEGF targeting antibody, ramucirumab, is a complete human IgG1 antibody, which can block the interaction between VEGFR-2 and VEGF ligand 102, 103. Ramucirumab functions by inhibiting its signaling pathway by selectively binding to VEGFR-2 104. Additionally, it blocks the activation of VEGFR-2 by ligands other than VEGF-A, including VEGF-C and VEGF-D 105.
Nintedanib is a small molecule TKI 106. In a phase III clinical study, the differences between patients with NSCLC treated with docetaxel with and without nintedanib were evaluated. PFS was significantly longer in patients treated with nintedanib than those in the placebo group 107. Moreover, the OS of docetaxel plus nintedanib was significantly longer than that of docetaxel plus placebo 107.
Furthermore, some other TKIs targeting the VEGF receptor pathway have been tested in clinical trials. For example, lorlatinib has shown clinical activity in patients with advanced NSCLC 108. Another phase II trial showed significantly longer PFS in some patients with NSCLC treated with fruquintinib 109.
3.2 Immune checkpoint inhibitor
The immune checkpoint is an immunomodulatory protein that can cause immunosuppression. Antibodies that block the receptors of cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) and programmed cell death protein (PD-1) or its ligand PD-L1 have been approved for clinical use 110. PD-1 and PD-L1 are mainly expressed in immune cells, such as NK cells, DC, CD4+, and CD8+ T cells 111-113. PD-1 interacts with its ligand PD-L1 to inhibit T cell activation and proliferation, leading to immune escape 114. Significant correlations were observed between the expression levels of PD-L1 and the expression levels of angiogenic factors, such as VEGFA and HIF-1α 115. CTLA-4 is an extracellular surface protein that can control immune suppression, mainly by stimulating T cell receptors 116.
The immune checkpoint inhibitors currently approved as first-line therapy fall into three main categories: Anti-PD-1, Anti-PD-L1, and Anti-CTLA-4. The main inhibitors used for first-line treatment of NSCLC include pembrolizumab 117-119, nivolumab 120, toripalimab 121, sintilimab (Anti-PD-1) 122, atezolizumab 26, 123, durvalumab (Anti-PD-L1) 124, 125, and lpilimumab (Anti-CTLA-4) 120, 126.
VEGF-A inhibits immune activation and induces immunosuppression by affecting various immune cells in the TME. Therefore, immune escape can be suppressed by inhibiting the effect of VEGF, and then combining immune checkpoint inhibitors to treat NSCLC. First, anti-angiogenic drugs can normalize tumor blood vessels and cause tumor immune cells (such as tumor-infiltrating lymphocytes) to increase in NSCLC. Immune checkpoint inhibitor can relieve the inhibition of PD-1 and PD-L1 on T cells, and the synergistic effect of the two shows better therapeutic effects on solid tumors 127. A clinical trial of anti-VEGF drugs combined with immune checkpoint inhibitors is currently underway (NCT04340882).
3.3 Vaccines and cell therapy
Cancer vaccines are an active immunotherapeutic intervention against malignancies. Their intended function is to bypass immune tolerance in the TME, thereby suppressing tumor survival. A new antigenic vaccine reported for the treatment of NSCLC combines NEO-PV-01 with PD-1 blockade; it induces T cells with cell-killing effects and has the ability to translocate to tumors 128. A Phase II trial showed the benefit of TG4010 (MVA-MUC1-IL2) vaccine in combination with first-line chemotherapy for advanced NSCLC 129.
Additionally, a clinical trial on the safety and feasibility of CRISPR-edited T cells in patients with refractory NSCLC has been completed 130. Another type of CAR-T cell therapy involves reprogramming the patient's T cells and infusing the modified T cells into the patient's body to attack the cancer cells. However, compared to malignant blood diseases, CAR-T cells have shown limited success in treating solid tumors, including NSCLC 131. Floris Dammeijer et al. found that tumor vaccines and cellular immunotherapy improved OS and PFS in patients with NSCLC, and that cellular immunotherapy was more effective than tumor vaccines 132. Combining VEGF-VEGFR-targeted therapy with a cancer vaccine to bypass immune tolerance in the TME may surpass the expectations of its effectiveness. Nevertheless, more preclinical and clinical studies will be needed to demonstrate this in the future.
3.4 Combining VEGF/VEGFR inhibitors and immunotherapy for NSCLC treatment
3.4.1 Preclinical studies
A preclinical study in a human lung adenocarcinoma xenograft model showed that bevacizumab improves the antitumor effect of cytokine-induced killer (CIK) cell transfer therapy 133. The CIK cells in the single treatment group showed no significant antitumor activity compared to the control group, while bevacizumab inhibited tumor growth and reached statistical significance 133. CIK cell therapy combined with VEGF inhibitor therapy showed significant antitumor activity compared to other groups 133. Similar studies in mouse models have also demonstrated that recombinant human endonuclease improves the therapeutic effect of employing CIK cells in lung cancer, revealing the mechanism of the antitumor effect of VEGF inhibitors in combination with immune cell therapy 134.
A study evaluating the synergistic effect of small-molecule tyrosine kinase inhibitor (bosutinib) and tumor vaccine showed that cabozantinib treatment combined with therapeutic tumor vaccine improved the proliferation and function of T cells 135. Tregs from mice treated with cabozantinib alone had a significantly lower ability to regulate CD4+ T cell proliferation than Tregs from control mice 135. Moreover, the regulatory ability of Tregs in mice treated with tumor vaccine alone reduced significantly 135. Surprisingly, the combination of cabozantinib and tumor vaccine application eliminated Treg function, as the CD4+ T cells of the mice with Treg were not significantly different from those of mice without Treg 135. Additionally, mice treated with cabozantinib combined with tumor vaccines showed a significant increase in both CD3+ lymphocyte and CD8+ T cell infiltration, indicating an increase in tumor killing effects 135. Other investigators have reported that a low-dose of anti-VEGFR2 antibodies can reprogram the immunosuppressive TME in a manner that enhances anti-cancer vaccine therapy 136.
In 2017, a Japanese research team reported a study using a mouse model, contributing new data on anti-tumor immunotherapy combining VEGF inhibitor (sunitinib) with agonist antibody of death receptor-5. Compared with a single therapy, combined therapy reduced tumor growth rate and increased the number of CD4+ Foxp3- and CD8+ T cells in patients with tumor 137.
Furthermore, VEGFR combined with T-lymphocyte adoptive transfer also showed potential clinical significance in cancer treatment. A preclinical study showed that adoptive transfer of human VEGFR-1 specificity with chimeric antigen receptor (CAR)-modified T lymphocytes (V-1CAR) can delay tumor growth and formation in mice 138. The results showed that in a mouse model of NSCLC cell A549 xenograft in NOD-SCID BALB/c mice, the growth of A549 xenografts was inhibited by V-1CAR modified T lymphocytes 138.
Moreover, a recent study found that anti-PD-L1 antibody combined with anti-VEGF antibody treatment inhibited tumor growth and increased CD8+ T cell infiltration compared with anti-VEGF monotherapy 139. These preclinical results support the idea that treatment efficacy can be improved by combining VEGF inhibitor with immunotherapy.
3.4.2 Clinical studies
Some clinical trials of anti-angiogenic drugs combined with immunotherapy for the treatment of NSCLC are ongoing (Table 1).
Table 1.
Data from clinical trials of anti-angiogenic drugs combined with immunotherapy for the treatment of NSCLC
| NCT ID | Relevant Compound(s) | Phase | Outcome Measures | Status | Study Title |
|---|---|---|---|---|---|
| NCT02366143 | Atezolizumab + Bevacizumab + Paclitaxel + Carboplatin | Ⅲ | PFS, 8.3 (95% CI, 7.7-9.8) OS, 19.2 (95% CI, 17.0-23.8) |
Completed | A Study of Atezolizumab in Combination with Carboplatin Plus (+) Paclitaxel With or Without Bevacizumab Compared with Carboplatin+Paclitaxel+Bevacizumab in Participants with Stage IV Non-Squamous Non-Small Cell Lung Cancer (NSCLC) |
| NCT02039674 | Pembrolizumab + Paclitaxel + Carboplatin + Bevacizumab | I/II | Objective Response Rate, DLT |
Completed | A Study of Pembrolizumab (MK-3475) in Combination with Chemotherapy or Immunotherapy in Participants with Non-small Cell Lung Cancer (MK-3475-021/KEYNOTE-021) |
| NCT01454102 | Bevacizumab + Nivolumab | I | ORR, 16.7% (95% CI, 2.1-48.4%) PFSR, 58.3% (95% CI, 27.0-80.1%) |
Completed | Study of Nivolumab (BMS-936558) in Combination with Gemcitabine/Cisplatin, Pemetrexed/Cisplatin, Carboplatin/Paclitaxel, Bevacizumab Maintenance, Erlotinib, Ipilimumab or as Monotherapy in Subjects with Stage IIIB/IV Non-small Cell Lung Cancer (NSCLC) (CheckMate 012) |
| NCT01633970 | Atezolizmab + Bevacizumab | I | DLT | Completed | A Study of Atezolizumab Administered in Combination with Bevacizumab and/or with Chemotherapy in Participants with Locally Advanced or Metastatic Solid Tumors |
| NCT02443324 | Ramucirumab + Pembrolizumab | I | DLT, DCR, Objective Response Rate |
Active, not recruiting | A Study of Ramucirumab Plus Pembrolizumab in Participants with Gastric or GEJ Adenocarcinoma, NSCLC, Transitional Cell Carcinoma of the Urothelium, or Biliary Tract Cancer |
| NCT02856425 | Pembrolizumab + Nintedanib | I | MTD | Recruiting | Trial of Pembrolizumab and Nintedanib |
| NCT04046614 | Nintedanib + Nivolumab | I/II | PFS, ORR | Recruiting | Feasibility and Safety of Nintedanib in Combination with Nivolumab in Pretreated Patients with Advanced or Metastatic NSCLC of Adenocarcinoma Histology |
| NCT03377023 | Nivolumab + Ipilimumab + Nintedanib | I/II | MTD, DCR, Objective Response Rate |
Active, not recruiting | Phase I/II Study of Nivolumab and Ipilimumab Combined with Nintedanib in Non-Small Cell Lung Cancer |
| NCT03689855 | Ramucirumab + Atezolizumab | II | ORR OS PFS |
Active, not recruiting | Ramucirumab and Atezolizumab After Progression on Any Immune Checkpoint Blocker in NSCLC |
| NCT00828009 | Bevacizumab + Tecemotide | II | PFS, 14.9 (95% CI, 11.0-20.9) OS, 42.7 (95% CI, 21.7-63.3) |
Completed; results published |
BLP25 Liposome Vaccine and Bevacizumab After Chemotherapy and Radiation Therapy in Treating Patients with Newly Diagnosed Stage IIIA or Stage IIIB Non-Small Cell Lung Cancer That Cannot Be Removed by Surgery |
| NCT02574078 | Bevacizumab + Nivolumab | I/II | PFS, 6.7 (4.1-NA) OS, 30.8 (8.8-NA) |
Completed; results published |
A Study of Nivolumab in Advanced Non-Small Cell Lung Cancer (NSCLC) |
| NCT02681549 | Pembrolizumab + Bevacizumab | II | BMRR, ORR | Recruiting | Pembrolizumab Plus Bevacizumab for Treatment of Brain Metastases in Metastatic Melanoma or Non-small Cell Lung Cancer |
| NCT03527108 | Nivolumab + Ramucirumab | II | DCR, ORR, PFS | Recruiting | Nivolumab Plus Ramucirumab in Patients With Recurrent, Advanced, Metastatic NSCLC |
| NCT02572687 | Ramucirumab + MEDI4736 | I | DLT, ORR, DCR | Completed | A Study of Ramucirumab (LY3009806) Plus MEDI4736 in Participants With Advanced Gastrointestinal or Thoracic Malignancies |
| NCT03786692 | Carboplatin + Pemetrexed + Bevacizumab + Atezolizumab | II | PFS, ORR | Recruiting | Phase II Randomized Trial of Carboplatin+Pemetrexed+Bevacizumab+/- Atezolizumab in Stage IV NSCLC |
| NCT02174172 | Atezolizumab + PEG-interferon alfa-2a + Bevacizumab | I | RP2D, RECIST | Completed | A Study to Assess the Safety and Tolerability of Atezolizumab in Combination With Other immune-modulating Therapies in Participants With Locally Advanced or Metastatic Solid Tumors |
| NCT03616691 | Atezolizumab+ Bevacizumab | II | ORR, PFS | Unknown | Atezolizumab Monotherapy and Consequent Therapy With Atezolizumab Plus Bevacizumab for NSCLC |
| NCT03647956 | Atezolizumab + Bevacizumab | II | Objective response rate, PFS, TTP, DoR |
Unknown | Atezolizumab in Combination With Bevacizumab, Carboplatin and Pemetrexed for EGFR-mutant Metastatic NSCLC Patients After Failure of EGFR Tyrosine Kinase Inhibitors |
| NCT03713944 | Carboplatin + Pemetrexed + Atezolizumab + Bevacizumab | II | PFS, ORR, DCR | Active, not recruiting | Carboplatin Plus Pemetrexed Plus Atezolizumab Plus Bevacizumab in Chemotherapy and Immunotherapy-naïve Patients With Stage IV Non-squamous Non-small Cell Lung Cancer |
| NCT03836066 | Atezolizumab + Bevacizumab | II | Efficacy of atezolizumab in combination with bevacizumab | Active, not recruiting | Atezolizumab Plus Bevacizumab in First-Line NSCLC Patients |
PFS: progression-free survival; OS: overall survival; CI: confidence interval; ORR: overall response rate; PFSR: progression-free survival rate; DLT: Dose-limiting toxicity; DCR: disease control rate; MTD: maximum tolerated dose; BMRR: brain metastasis response rate; RP2D: recommended phase II dose; RECIST: response evaluation criteria in solid Tumors; TTP: time to progression; DoR: duration of response.
In a phase III study (NCT02366143), to examine whether VEGF blockade enhances the efficacy of immunotherapy, atezolizumab was added to the combination of bevacizumab and chemotherapy treatment. At the time of data truncation, in the intent-to-treat wild-type (ITT-WT) population, the median PFS of the group with bevacizumab and atezolizumab was significantly longer than that of the group without atezolizumab 140. Furthermore, after 6 months of treatment, the PFS rate of the group with bevacizumab and atezolizumab was higher than that of the group without atezolizumab 140. In the Teff-high WT population, the median PFS was significantly longer in the group with atezolizumab than in the group without atezolizumab 140. Moreover, similar results were observed for OS in the ITT-WT population. However, the rate of objective response was not confirmed, and there were more data for the group with atezolizumab than for that without atezolizumab; the results were similar in the Teff-high WT population 140.
In a phase I study (NCT01454102), the efficacy of nivolumab in combination with bevacizumab was compared to the efficacy of nivolumab alone in patients with advanced NSCLC. The results showed that a higher proportion of subjects were progression-free and survived at 24 weeks in the nivolumab plus bevacizumab group than in the nivolumab monotherapy group. Moreover, the objective response rate (ORR) of nivolumab plus bevacizumab and nivolumab alone arms was 16.7% and 23.1%, respectively.
In another phase I study (NCT02443324), the effectiveness and safety of ramucirumab and pembrolizumab were evaluated in the treatment of different tumor entities, including NSCLC. The ORR of the treated population was 42.3%, and the median PFS was 9.3 months. However, the treated population did not reach the median OS 141.
A study on pembrolizumab plus paclitaxel plus carboplatin plus with/without bevacizumab in stage IIIB/IV NSCLC is also under evaluation (NCT02039674). The results of pembrolizumab plus bevacizumab showed an ORR of 56%, a PFS of 7.1 months, and a median OS of 16.7 months 142.
Moreover, an open phase IB study evaluating the safety, pharmacology, and initial efficacy of the combination of atezolizumab and bevacizumab in the treatment of advanced solid tumors including NSCLC has been completed. However, the results of the study have not yet been published (NCT01633970).
Many studies are currently ongoing. A phase IB trial has been launched with the aim to evaluate the efficacy of pembrolizumab and nintedanib in the treatment of solid tumors, including advanced NSCLC (NCT02856425), and participants are being recruited. A phase I/II study of the efficacy of nivolumab and ipilimumab combined with nintedanib in NSCLC has been initiated, but no results have been published so far (NCT03377023). Additionally, a Phase I/II trial evaluating the feasibility and safety of nintedanib in combination with nivolumab in pretreated patients with advanced or metastatic adenocarcinoma histologic NSCLC has been initiated and is currently recruiting participants (NCT04046614).
Overall, the combination of immunotherapy and VEGF-VEGFR-targeted therapy for NSCLC has yielded encouraging results for such treatment. However, for best therapeutic results, the effects of different anti-angiogenic medications, drug doses, and timing of the combination of the two drugs need to be addressed in future clinical trials.
4. Conclusion and Perspectives
This review evaluated the latest knowledge on two therapies, VEGF-VEGFR-targeted therapy and immunotherapy, for the treatment of NSCLC. In addition to promoting tumor angiogenesis, VEGF also promotes immunosuppression in NSCLC. The application of a combination of VEGF/VEGFR-targeted therapy and immunotherapy in preclinical and clinical studies has shown good efficacy in the treatment of NSCLC by regulating the immunosuppressive TME. Results from the currently enrolling clinical studies also support that the combination therapy is a promising approach for the treatment of NSCLC. Future preclinical and clinical studies need to address some key questions, such as what are the specific biomarkers in response to the combination therapy? This therapeutic approach targeting the TME certainly has complex biological effects. Combination therapy may further increase this complexity, posing an increased risk of toxicity and the possibility of immune-related adverse events. For example, immunotherapy can sometimes lead to serious immune-related adverse events, and these toxic reactions can usually be resolved by stopping treatment or reducing the dose. Therefore, it is important to optimize the dose, timing of administration, and sequence of administration of VEGF-VEGFR-targeted drug therapy and immunotherapy in future clinical studies. Since the use of VEGF-VEGFR-targeted drugs allows the drugs or immune cells in immunotherapy to reach the tumor site more easily through normalized blood vessels, the dose of immunotherapy drugs can be reduced appropriately in combination therapy.
While the employment of combination therapy offers a promising future for NSCLC treatment, further studies must investigate how these therapeutic strategies interact with each other to regulate the immunosuppressive TME and kill cancer cells. New technologies, such as single-cell sequencing and spatial transcriptomics, may improve our knowledge. These technologies can help us understand the interactions among angiogenesis, cancer cells, and immune cells of the immunosuppressive TME of NSCLC. Meanwhile, we can design new approaches to target angiogenic and immunosuppressive environment for NSCLC treatment.
Acknowledgments
This work was supported by Science and Technology Research Fund of Sichuan Administration of Traditional Chinese Medicine (No. 2021MS528), and the Science and Technology Strategic Cooperation Programs of Luzhou Municipal People's Government and Southwest Medical University (Grant nos. 2019LZXNYDJ25, and 2019LZXNYDJ45).
Author Contributions
YZ, SG, JD, JL, and ZX wrote the first draft of manuscript and first revision; all authors revised the manuscript for second times before submission. All authors contributed to manuscript revision, read and approved the submitted version.
References
- 1.Thai AA, Solomon BJ, Sequist LV, Gainor JF, Heist RS. Lung cancer. Lancet. 2021;398:535–54. doi: 10.1016/S0140-6736(21)00312-3. [DOI] [PubMed] [Google Scholar]
- 2.Hao C, Liu G, Tian G. Autophagy inhibition of cancer stem cells promotes the efficacy of cisplatin against non-small cell lung carcinoma. Ther Adv Respir Dis. 2019;13:1753466619866097. doi: 10.1177/1753466619866097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toyokawa G, Yamada Y, Tagawa T, Oda Y. Significance of spread through air spaces in early-stage lung adenocarcinomas undergoing limited resection. Thorac Cancer. 2018;9:1255–61. doi: 10.1111/1759-7714.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herbst RS, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553:446–54. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 5.Hwang I, Kim JW, Ylaya K, Chung EJ, Kitano H, Perry C. et al. Tumor-associated macrophage, angiogenesis and lymphangiogenesis markers predict prognosis of non-small cell lung cancer patients. J Transl Med. 2020;18:443. doi: 10.1186/s12967-020-02618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Palma M, Biziato D, Petrova TV. Microenvironmental regulation of tumour angiogenesis. Nat Rev Cancer. 2017;17:457–74. doi: 10.1038/nrc.2017.51. [DOI] [PubMed] [Google Scholar]
- 7.Guimarães-Bastos D, Frony AC, Barja-Fidalgo C, Moraes JA. Melanoma-derived extracellular vesicles skew neutrophils into a pro-tumor phenotype. J Leukoc Biol. 2021. [DOI] [PubMed]
- 8.Komi DEA, Khomtchouk K, Santa Maria PL. A Review of the Contribution of Mast Cells in Wound Healing: Involved Molecular and Cellular Mechanisms. Clinical reviews in allergy & immunology. 2020;58:298–312. doi: 10.1007/s12016-019-08729-w. [DOI] [PubMed] [Google Scholar]
- 9.McHale C, Mohammed Z, Gomez G. Human Skin-Derived Mast Cells Spontaneously Secrete Several Angiogenesis-Related Factors. Frontiers in immunology. 2019;10:1445. doi: 10.3389/fimmu.2019.01445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sammarco G, Varricchi G, Ferraro V, Ammendola M, De Fazio M, Altomare DF, Mast Cells, Angiogenesis and Lymphangiogenesis in Human Gastric Cancer. International journal of molecular sciences. 2019. 20. [DOI] [PMC free article] [PubMed]
- 11.Rahma OE, Hodi FS. The Intersection between Tumor Angiogenesis and Immune Suppression. Clinical cancer research: an official journal of the American Association for Cancer Research. 2019;25:5449–57. doi: 10.1158/1078-0432.CCR-18-1543. [DOI] [PubMed] [Google Scholar]
- 12.Vetsika E-K, Koukos A, Kotsakis A. Myeloid-Derived Suppressor Cells: Major Figures that Shape the Immunosuppressive and Angiogenic Network in Cancer. Cells. 2019. 8. [DOI] [PMC free article] [PubMed]
- 13.Mortezaee K. Myeloid-derived suppressor cells in cancer immunotherapy-clinical perspectives. Life Sci. 2021;277:119627. doi: 10.1016/j.lfs.2021.119627. [DOI] [PubMed] [Google Scholar]
- 14.Albini A, Bruno A, Noonan DM, Mortara L. Contribution to Tumor Angiogenesis From Innate Immune Cells Within the Tumor Microenvironment: Implications for Immunotherapy. Front Immunol. 2018;9:527. doi: 10.3389/fimmu.2018.00527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan Y, Chambers CB, Tabatabai T, Hatley H, Delfino KR, Robinson K. et al. Renal cell tumors convert natural killer cells to a proangiogenic phenotype. Oncotarget. 2020;11:2571–85. doi: 10.18632/oncotarget.27654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang M, Herbst RS, Boshoff C. Toward personalized treatment approaches for non-small-cell lung cancer. Nat Med. 2021;27:1345–56. doi: 10.1038/s41591-021-01450-2. [DOI] [PubMed] [Google Scholar]
- 17.Apte RS, Chen DS, Ferrara N. VEGF in Signaling and Disease: Beyond Discovery and Development. Cell. 2019;176:1248–64. doi: 10.1016/j.cell.2019.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uemura A, Fruttiger M, D'Amore PA, De Falco S, Joussen AM, Sennlaub F. et al. VEGFR1 signaling in retinal angiogenesis and microinflammation. Prog Retin Eye Res. 2021;84:100954. doi: 10.1016/j.preteyeres.2021.100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dallinga MG, Habani YI, Schimmel AWM, Dallinga-Thie GM, van Noorden CJF, Klaassen I, The Role of Heparan Sulfate and Neuropilin 2 in VEGFA Signaling in Human Endothelial Tip Cells and Non-Tip Cells during Angiogenesis In Vitro. Cells. 2021. 10. [DOI] [PMC free article] [PubMed]
- 20.Sarabipour S, Mac Gabhann F. VEGF-A121a binding to Neuropilins - A concept revisited. Cell Adh Migr. 2018;12:204–14. doi: 10.1080/19336918.2017.1372878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLaren J, Prentice A, Charnock-Jones DS, Millican SA, Müller KH, Sharkey AM. et al. Vascular endothelial growth factor is produced by peritoneal fluid macrophages in endometriosis and is regulated by ovarian steroids. J Clin Invest. 1996;98:482–9. doi: 10.1172/JCI118815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Claesson-Welsh L, Welsh M. VEGFA and tumour angiogenesis. J Intern Med. 2013;273:114–27. doi: 10.1111/joim.12019. [DOI] [PubMed] [Google Scholar]
- 23.Chu BF, Otterson GA. Incorporation of Antiangiogenic Therapy Into the Non-Small-Cell Lung Cancer Paradigm. Clin Lung Cancer. 2016;17:493–506. doi: 10.1016/j.cllc.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 24.Goel HL, Mercurio AM. VEGF targets the tumour cell. Nat Rev Cancer. 2013;13:871–82. doi: 10.1038/nrc3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Das M, Wakelee H. Targeting VEGF in lung cancer. Expert Opin Ther Targets. 2012;16:395–406. doi: 10.1517/14728222.2012.669752. [DOI] [PubMed] [Google Scholar]
- 26.Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N. et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. The New England journal of medicine. 2018;378:2288–301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 27.Olsson A-K, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling - in control of vascular function. Nat Rev Mol Cell Biol. 2006;7:359–71. doi: 10.1038/nrm1911. [DOI] [PubMed] [Google Scholar]
- 28.Holmes K, Roberts OL, Thomas AM, Cross MJ. Vascular endothelial growth factor receptor-2: structure, function, intracellular signalling and therapeutic inhibition. Cell Signal. 2007;19:2003–12. doi: 10.1016/j.cellsig.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Korpela H, Hätinen O-P, Nieminen T, Mallick R, Toivanen P, Airaksinen J. et al. Adenoviral VEGF-B186R127S gene transfer induces angiogenesis and improves perfusion in ischemic heart. iScience. 2021;24:103533. doi: 10.1016/j.isci.2021.103533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou Y, Zhu X, Cui H, Shi J, Yuan G, Shi S. et al. The Role of the VEGF Family in Coronary Heart Disease. Front Cardiovasc Med. 2021;8:738325. doi: 10.3389/fcvm.2021.738325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chakraborty A, Upadhya R, Usman TA, Shetty AK, Rutkowski JM. Chronic VEGFR-3 signaling preserves dendritic arborization and sensitization under stress. Brain Behav Immun. 2021;98:219–33. doi: 10.1016/j.bbi.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Otrock ZK, Makarem JA, Shamseddine AI. Vascular endothelial growth factor family of ligands and receptors: Review. Blood Cells, Molecules, and Diseases. 2007;38:258–68. doi: 10.1016/j.bcmd.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 33.Al-Shareef H, Hiraoka S-I, Tanaka N, Shogen Y, Lee A-D, Bakhshishayan S. et al. Use of NRP1, a novel biomarker, along with VEGF-C, VEGFR-3, CCR7 and SEMA3E, to predict lymph node metastasis in squamous cell carcinoma of the tongue. Oncology Reports. 2016;36:2444–54. doi: 10.3892/or.2016.5116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sopo M, Anttila M, Hämäläinen K, Kivelä A, Ylä-Herttuala S, Kosma V-M. et al. Expression profiles of VEGF-A, VEGF-D and VEGFR1 are higher in distant metastases than in matched primary high grade epithelial ovarian cancer. BMC Cancer. 2019;19:584. doi: 10.1186/s12885-019-5757-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kong X, Bu J, Chen J, Ni B, Fu B, Zhou F. et al. PIGF and Flt-1 on the surface of macrophages induces the production of TGF-β1 by polarized tumor-associated macrophages to promote lung cancer angiogenesis. Eur J Pharmacol. 2021;912:174550. doi: 10.1016/j.ejphar.2021.174550. [DOI] [PubMed] [Google Scholar]
- 36.Frezzetti D, Gallo M, Maiello MR, D'Alessio A, Esposito C, Chicchinelli N. et al. VEGF as a potential target in lung cancer. Expert Opin Ther Targets. 2017;21:959–66. doi: 10.1080/14728222.2017.1371137. [DOI] [PubMed] [Google Scholar]
- 37.Goel HL, Mercurio AM. VEGF targets the tumour cell. Nature reviews Cancer. 2013;13:871–82. doi: 10.1038/nrc3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barr MP, Gray SG, Gately K, Hams E, Fallon PG, Davies AM. et al. Vascular endothelial growth factor is an autocrine growth factor, signaling through neuropilin-1 in non-small cell lung cancer. Molecular cancer. 2015;14:45. doi: 10.1186/s12943-015-0310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li H, Takayama K, Wang S, Shiraishi Y, Gotanda K, Harada T. et al. Addition of bevacizumab enhances antitumor activity of erlotinib against non-small cell lung cancer xenografts depending on VEGF expression. Cancer Chemother Pharmacol. 2014;74:1297–305. doi: 10.1007/s00280-014-2610-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Naumov GN, Nilsson MB, Cascone T, Briggs A, Straume O, Akslen LA. et al. Combined vascular endothelial growth factor receptor and epidermal growth factor receptor (EGFR) blockade inhibits tumor growth in xenograft models of EGFR inhibitor resistance. Clinical cancer research: an official journal of the American Association for Cancer Research. 2009;15:3484–94. doi: 10.1158/1078-0432.CCR-08-2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lei X, Lei Y, Li J-K, Du W-X, Li R-G, Yang J. et al. Immune cells within the tumor microenvironment: Biological functions and roles in cancer immunotherapy. Cancer Lett. 2020;470:126–33. doi: 10.1016/j.canlet.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 42.Galassi C, Musella M, Manduca N, Maccafeo E, Sistigu A. The Immune Privilege of Cancer Stem Cells: A Key to Understanding Tumor Immune Escape and Therapy Failure. Cells. 2021. 10. [DOI] [PMC free article] [PubMed]
- 43.Voron T, Colussi O, Marcheteau E, Pernot S, Nizard M, Pointet AL. et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J Exp Med. 2015;212:139–48. doi: 10.1084/jem.20140559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martino EC, Misso G, Pastina P, Costantini S, Vanni F, Gandolfo C. et al. Immune-modulating effects of bevacizumab in metastatic non-small-cell lung cancer patients. Cell Death Discov. 2016;2:16025. doi: 10.1038/cddiscovery.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Almeida PE, Mak J, Hernandez G, Jesudason R, Herault A, Javinal V. et al. Anti-VEGF Treatment Enhances CD8 T-cell Antitumor Activity by Amplifying Hypoxia. Cancer immunology research. 2020;8:806–18. doi: 10.1158/2326-6066.CIR-19-0360. [DOI] [PubMed] [Google Scholar]
- 46.Bannoud N, Dalotto-Moreno T, Kindgard L, García PA, Blidner AG, Mariño KV. et al. Hypoxia Supports Differentiation of Terminally Exhausted CD8 T Cells. Front Immunol. 2021;12:660944. doi: 10.3389/fimmu.2021.660944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gabrilovich D, Ishida T, Oyama T, Ran S, Kravtsov V, Nadaf S. et al. Vascular endothelial growth factor inhibits the development of dendritic cells and dramatically affects the differentiation of multiple hematopoietic lineages in vivo. Blood. 1998;92:4150–66. [PubMed] [Google Scholar]
- 48.Ohm JE, Gabrilovich DI, Sempowski GD, Kisseleva E, Parman KS, Nadaf S. et al. VEGF inhibits T-cell development and may contribute to tumor-induced immune suppression. Blood. 2003;101:4878–86. doi: 10.1182/blood-2002-07-1956. [DOI] [PubMed] [Google Scholar]
- 49.Liu X, Nie W, Xie Q, Chen G, Li X, Jia Y. et al. Endostatin reverses immunosuppression of the tumor microenvironment in lung carcinoma. Oncol Lett. 2018;15:1874–80. doi: 10.3892/ol.2017.7455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bourhis M, Palle J, Galy-Fauroux I, Terme M. Direct and Indirect Modulation of T Cells by VEGF-A Counteracted by Anti-Angiogenic Treatment. Frontiers in immunology. 2021;12:616837. doi: 10.3389/fimmu.2021.616837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim CG, Jang M, Kim Y, Leem G, Kim KH, Lee H, VEGF-A drives TOX-dependent T cell exhaustion in anti-PD-1-resistant microsatellite stable colorectal cancers. Sci Immunol. 2019. 4. [DOI] [PubMed]
- 52.Tang R, Xu J, Zhang B, Liu J, Liang C, Hua J. et al. Ferroptosis, necroptosis, and pyroptosis in anticancer immunity. J Hematol Oncol. 2020;13:110. doi: 10.1186/s13045-020-00946-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Flores-Mendoza G, Rodríguez-Rodríguez N, Rubio RM, Madera-Salcedo IK, Rosetti F, Crispín JC. Fas/FasL Signaling Regulates CD8 Expression During Exposure to Self-Antigens. Frontiers in immunology. 2021;12:635862. doi: 10.3389/fimmu.2021.635862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dorothee G, Vergnon I, Menez J, Echchakir H, Grunenwald D, Kubin M. et al. Tumor-infiltrating CD4+ T lymphocytes express APO2 ligand (APO2L)/TRAIL upon specific stimulation with autologous lung carcinoma cells: role of IFN-alpha on APO2L/TRAIL expression and -mediated cytotoxicity. J Immunol. 2002;169:809–17. doi: 10.4049/jimmunol.169.2.809. [DOI] [PubMed] [Google Scholar]
- 55.Ohkura N, Sakaguchi S. Transcriptional and epigenetic basis of Treg cell development and function: its genetic anomalies or variations in autoimmune diseases. Cell research. 2020;30:465–74. doi: 10.1038/s41422-020-0324-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mikami N, Kawakami R, Sakaguchi S. New Treg cell-based therapies of autoimmune diseases: towards antigen-specific immune suppression. Curr Opin Immunol. 2020;67:36–41. doi: 10.1016/j.coi.2020.07.004. [DOI] [PubMed] [Google Scholar]
- 57.Zappasodi R, Sirard C, Li Y, Budhu S, Abu-Akeel M, Liu C. et al. Rational design of anti-GITR-based combination immunotherapy. Nat Med. 2019;25:759–66. doi: 10.1038/s41591-019-0420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Han P, Hou Y, Zhao Y, Liu Y, Yu T, Sun Y. et al. Low-dose decitabine modulates T-cell homeostasis and restores immune tolerance in immune thrombocytopenia. Blood. 2021;138:674–88. doi: 10.1182/blood.2020008477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tanaka A, Sakaguchi S. Regulatory T cells in cancer immunotherapy. Cell Res. 2017;27:109–18. doi: 10.1038/cr.2016.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Deng G, Song X, Fujimoto S, Piccirillo CA, Nagai Y, Greene MI. Foxp3 Post-translational Modifications and Treg Suppressive Activity. Frontiers in immunology. 2019;10:2486. doi: 10.3389/fimmu.2019.02486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ohue Y, Nishikawa H. Regulatory T (Treg) cells in cancer: Can Treg cells be a new therapeutic target? Cancer Sci. 2019;110:2080–9. doi: 10.1111/cas.14069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun L, Xu G, Liao W, Yang H, Xu H, Du S. et al. Clinicopathologic and prognostic significance of regulatory T cells in patients with hepatocellular carcinoma: a meta-analysis. Oncotarget. 2017;8:39658–72. doi: 10.18632/oncotarget.17340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shitara K, Nishikawa H. Regulatory T cells: a potential target in cancer immunotherapy. Ann N Y Acad Sci. 2018;1417:104–15. doi: 10.1111/nyas.13625. [DOI] [PubMed] [Google Scholar]
- 64.Fukumura D, Kloepper J, Amoozgar Z, Duda DG, Jain RK. Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat Rev Clin Oncol. 2018;15:325–40. doi: 10.1038/nrclinonc.2018.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Terme M, Pernot S, Marcheteau E, Sandoval F, Benhamouda N, Colussi O. et al. VEGFA-VEGFR pathway blockade inhibits tumor-induced regulatory T-cell proliferation in colorectal cancer. Cancer Res. 2013;73:539–49. doi: 10.1158/0008-5472.CAN-12-2325. [DOI] [PubMed] [Google Scholar]
- 66.Hansen W, Hutzler M, Abel S, Alter C, Stockmann C, Kliche S. et al. Neuropilin 1 deficiency on CD4+Foxp3+ regulatory T cells impairs mouse melanoma growth. J Exp Med. 2012;209:2001–16. doi: 10.1084/jem.20111497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou K, Cheng T, Zhan J, Peng X, Zhang Y, Wen J. et al. Targeting tumor-associated macrophages in the tumor microenvironment. Oncology letters. 2020;20:234. doi: 10.3892/ol.2020.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vitale I, Manic G, Coussens LM, Kroemer G, Galluzzi L. Macrophages and Metabolism in the Tumor Microenvironment. Cell Metab. 2019;30:36–50. doi: 10.1016/j.cmet.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 69.Myers KV, Amend SR, Pienta KJ. Targeting Tyro3, Axl and MerTK (TAM receptors): implications for macrophages in the tumor microenvironment. Molecular cancer. 2019;18:94. doi: 10.1186/s12943-019-1022-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lin Y, Xu J, Lan H. Tumor-associated macrophages in tumor metastasis: biological roles and clinical therapeutic applications. J Hematol Oncol. 2019;12:76. doi: 10.1186/s13045-019-0760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Park JE, Dutta B, Tse SW, Gupta N, Tan CF, Low JK. et al. Hypoxia-induced tumor exosomes promote M2-like macrophage polarization of infiltrating myeloid cells and microRNA-mediated metabolic shift. Oncogene. 2019;38:5158–73. doi: 10.1038/s41388-019-0782-x. [DOI] [PubMed] [Google Scholar]
- 72.Lapeyre-Prost A, Terme M, Pernot S, Pointet AL, Voron T, Tartour E. et al. Immunomodulatory Activity of VEGF in Cancer. Int Rev Cell Mol Biol. 2017;330:295–342. doi: 10.1016/bs.ircmb.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 73.Lia A, Annese T, Fornaro M, Giannini M, D'Abbicco D, Errede M, Perivascular and endomysial macrophages expressing VEGF and CXCL12 promote angiogenesis in anti-HMGCR immune-mediated necrotizing myopathy. Rheumatology (Oxford) 2021. [DOI] [PubMed]
- 74.Morante-Palacios O, Fondelli F, Ballestar E, Martínez-Cáceres EM. Tolerogenic Dendritic Cells in Autoimmunity and Inflammatory Diseases. Trends in immunology. 2021;42:59–75. doi: 10.1016/j.it.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 75.Bosch NC, Voll RE, Voskens CJ, Gross S, Seliger B, Schuler G. et al. NF-κB activation triggers NK-cell stimulation by monocyte-derived dendritic cells. Ther Adv Med Oncol. 2019;11:1758835919891622. doi: 10.1177/1758835919891622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lucarini V, Melaiu O, Tempora P, D'Amico S, Locatelli F, Fruci D. Dendritic Cells: Behind the Scenes of T-Cell Infiltration into the Tumor Microenvironment. Cancers. 2021. 13. [DOI] [PMC free article] [PubMed]
- 77.Anirudh S, Rosenberger A, Schwarzenberger E, Schaefer C, Strobl H, Zebisch A, TNFα Rescues Dendritic Cell Development in Hematopoietic Stem and Progenitor Cells Lacking C/EBPα. Cells. 2020. 9. [DOI] [PMC free article] [PubMed]
- 78.Han Z, Dong Y, Lu J, Yang F, Zheng Y, Yang H. Role of hypoxia in inhibiting dendritic cells by VEGF signaling in tumor microenvironments: mechanism and application. Am J Cancer Res. 2021;11:3777–93. [PMC free article] [PubMed] [Google Scholar]
- 79.Khan KA, Kerbel RS. Improving immunotherapy outcomes with anti-angiogenic treatments and vice versa. Nat Rev Clin Oncol. 2018;15:310–24. doi: 10.1038/nrclinonc.2018.9. [DOI] [PubMed] [Google Scholar]
- 80.Chen DS, Hurwitz H. Combinations of Bevacizumab With Cancer Immunotherapy. Cancer J. 2018;24:193–204. doi: 10.1097/PPO.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 81.Long J, Hu Z, Xue H, Wang Y, Chen J, Tang F. et al. Vascular endothelial growth factor (VEGF) impairs the motility and immune function of human mature dendritic cells through the VEGF receptor 2-RhoA-cofilin1 pathway. Cancer Sci. 2019;110:2357–67. doi: 10.1111/cas.14091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Osada T, Chong G, Tansik R, Hong T, Spector N, Kumar R. et al. The effect of anti-VEGF therapy on immature myeloid cell and dendritic cells in cancer patients. Cancer Immunol Immunother. 2008;57:1115–24. doi: 10.1007/s00262-007-0441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Strauss L, Volland D, Kunkel M, Reichert TE. Dual role of VEGF family members in the pathogenesis of head and neck cancer (HNSCC): possible link between angiogenesis and immune tolerance. Med Sci Monit. 2005;11:BR280–BR92. [PubMed] [Google Scholar]
- 84.Inoshima N, Nakanishi Y, Minami T, Izumi M, Takayama K, Yoshino I. et al. The influence of dendritic cell infiltration and vascular endothelial growth factor expression on the prognosis of non-small cell lung cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2002;8:3480–6. [PubMed] [Google Scholar]
- 85.Hegde S, Leader AM, Merad M. MDSC: Markers, development, states, and unaddressed complexity. Immunity. 2021;54:875–84. doi: 10.1016/j.immuni.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dysthe M, Parihar R. Myeloid-Derived Suppressor Cells in the Tumor Microenvironment. Adv Exp Med Biol. 2020;1224:117–40. doi: 10.1007/978-3-030-35723-8_8. [DOI] [PubMed] [Google Scholar]
- 87.Weber R, Groth C, Lasser S, Arkhypov I, Petrova V, Altevogt P. et al. IL-6 as a major regulator of MDSC activity and possible target for cancer immunotherapy. Cellular immunology. 2021;359:104254. doi: 10.1016/j.cellimm.2020.104254. [DOI] [PubMed] [Google Scholar]
- 88.Tesi RJ. MDSC; the Most Important Cell You Have Never Heard Of. Trends Pharmacol Sci. 2019;40:4–7. doi: 10.1016/j.tips.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 89.Ma J, Xu H, Wang S. Immunosuppressive Role of Myeloid-Derived Suppressor Cells and Therapeutic Targeting in Lung Cancer. J Immunol Res. 2018;2018:6319649. doi: 10.1155/2018/6319649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Almand B, Resser JR, Lindman B, Nadaf S, Clark JI, Kwon ED. et al. Clinical significance of defective dendritic cell differentiation in cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2000;6:1755–66. [PubMed] [Google Scholar]
- 91.Fleming V, Hu X, Weber R, Nagibin V, Groth C, Altevogt P. et al. Targeting Myeloid-Derived Suppressor Cells to Bypass Tumor-Induced Immunosuppression. Front Immunol. 2018;9:398. doi: 10.3389/fimmu.2018.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Koinis F, Vetsika EK, Aggouraki D, Skalidaki E, Koutoulaki A, Gkioulmpasani M. et al. Effect of First-Line Treatment on Myeloid-Derived Suppressor Cells' Subpopulations in the Peripheral Blood of Patients with Non-Small Cell Lung Cancer. J Thorac Oncol. 2016;11:1263–72. doi: 10.1016/j.jtho.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 93.Myers JA, Miller JS. Exploring the NK cell platform for cancer immunotherapy. Nat Rev Clin Oncol. 2021;18:85–100. doi: 10.1038/s41571-020-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang L, Dai Y, Zhu F, Qiu Z, Wang Y, Hu Y. Efficacy of DC-CIK-based immunotherapy combined with chemotherapy in the treatment of intermediate to advanced non-small cell lung cancer. Am J Transl Res. 2021;13:13076–83. [PMC free article] [PubMed] [Google Scholar]
- 95.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nature Reviews Immunology. 2009;9:162–74. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kolahian S, Oz HH, Zhou B, Griessinger CM, Rieber N, Hartl D. The emerging role of myeloid-derived suppressor cells in lung diseases. Eur Respir J. 2016;47:967–77. doi: 10.1183/13993003.01572-2015. [DOI] [PubMed] [Google Scholar]
- 97.Hawke LG, Whitford MKM, Ormiston ML. The Production of Pro-angiogenic VEGF-A Isoforms by Hypoxic Human NK Cells Is Independent of Their TGF-beta-Mediated Conversion to an ILC1-Like Phenotype. Front Immunol. 2020;11:1903. doi: 10.3389/fimmu.2020.01903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Krzywinska E, Kantari-Mimoun C, Kerdiles Y, Sobecki M, Isagawa T, Gotthardt D. et al. Loss of HIF-1α in natural killer cells inhibits tumour growth by stimulating non-productive angiogenesis. Nature communications. 2017;8:1597. doi: 10.1038/s41467-017-01599-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Eguchi R, Wakabayashi I. HDGF enhances VEGF-dependent angiogenesis and FGF-2 is a VEGF-independent angiogenic factor in non-small cell lung cancer. Oncology reports. 2020;44:14–28. doi: 10.3892/or.2020.7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jung WY, Min K-W, Oh YH. Increased VEGF-A in solid type of lung adenocarcinoma reduces the patients' survival. Sci Rep. 2021;11:1321. doi: 10.1038/s41598-020-79907-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Garcia J, Hurwitz HI, Sandler AB, Miles D, Coleman RL, Deurloo R. et al. Bevacizumab (Avastin®) in cancer treatment: A review of 15 years of clinical experience and future outlook. Cancer Treat Rev. 2020;86:102017. doi: 10.1016/j.ctrv.2020.102017. [DOI] [PubMed] [Google Scholar]
- 102.Nakagawa K, Garon EB, Seto T, Nishio M, Ponce Aix S, Paz-Ares L. et al. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:1655–69. doi: 10.1016/S1470-2045(19)30634-5. [DOI] [PubMed] [Google Scholar]
- 103.Syed YY. Ramucirumab: A Review in Hepatocellular Carcinoma. Drugs. 2020;80:315–22. doi: 10.1007/s40265-020-01263-6. [DOI] [PubMed] [Google Scholar]
- 104.Spratlin JL, Cohen RB, Eadens M, Gore L, Camidge DR, Diab S. et al. Phase I pharmacologic and biologic study of ramucirumab (IMC-1121B), a fully human immunoglobulin G1 monoclonal antibody targeting the vascular endothelial growth factor receptor-2. J Clin Oncol. 2010;28:780–7. doi: 10.1200/JCO.2009.23.7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Janning M, Loges S. Anti-Angiogenics: Their Value in Lung Cancer Therapy. Oncol Res Treat. 2018;41:172–80. doi: 10.1159/000488119. [DOI] [PubMed] [Google Scholar]
- 106.Kovalchuk B, Berghoff AS, Karreman MA, Frey K, Piechutta M, Fischer M. et al. Nintedanib and a bi-specific anti-VEGF/Ang2 nanobody selectively prevent brain metastases of lung adenocarcinoma cells. Clin Exp Metastasis. 2020;37:637–48. doi: 10.1007/s10585-020-10055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Reck M, Kaiser R, Mellemgaard A, Douillard J-Y, Orlov S, Krzakowski M. et al. Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol. 2014;15:143–55. doi: 10.1016/S1470-2045(13)70586-2. [DOI] [PubMed] [Google Scholar]
- 108.Shaw AT, Solomon BJ, Chiari R, Riely GJ, Besse B, Soo RA. et al. Lorlatinib in advanced ROS1-positive non-small-cell lung cancer: a multicentre, open-label, single-arm, phase 1-2 trial. Lancet Oncol. 2019;20:1691–701. doi: 10.1016/S1470-2045(19)30655-2. [DOI] [PubMed] [Google Scholar]
- 109.Lu S, Chen G, Sun Y, Sun S, Chang J, Yao Y. et al. A Phase III, randomized, double-blind, placebo-controlled, multicenter study of fruquintinib in Chinese patients with advanced nonsquamous non-small-cell lung cancer - The FALUCA study. Lung cancer (Amsterdam, Netherlands) 2020;146:252–62. doi: 10.1016/j.lungcan.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 110.Bagchi S, Yuan R, Engleman EG. Immune Checkpoint Inhibitors for the Treatment of Cancer: Clinical Impact and Mechanisms of Response and Resistance. Annu Rev Pathol. 2021;16:223–49. doi: 10.1146/annurev-pathol-042020-042741. [DOI] [PubMed] [Google Scholar]
- 111.Cha J-H, Chan L-C, Li C-W, Hsu JL, Hung M-C. Mechanisms Controlling PD-L1 Expression in Cancer. Mol Cell. 2019;76:359–70. doi: 10.1016/j.molcel.2019.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sivori S, Pende D, Quatrini L, Pietra G, Della Chiesa M, Vacca P. et al. NK cells and ILCs in tumor immunotherapy. Mol Aspects Med. 2021;80:100870. doi: 10.1016/j.mam.2020.100870. [DOI] [PubMed] [Google Scholar]
- 113.Dammeijer F, van Gulijk M, Mulder EE, Lukkes M, Klaase L, van den Bosch T, The PD-1/PD-L1-Checkpoint Restrains T cell Immunity in Tumor-Draining Lymph Nodes. Cancer cell. 2020. 38. [DOI] [PubMed]
- 114.Jiang X, Wang J, Deng X, Xiong F, Ge J, Xiang B. et al. Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Molecular cancer. 2019;18:10. doi: 10.1186/s12943-018-0928-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Koh YW, Lee SJ, Han J-H, Haam S, Jung J, Lee HW. PD-L1 protein expression in non-small-cell lung cancer and its relationship with the hypoxia-related signaling pathways: A study based on immunohistochemistry and RNA sequencing data. Lung Cancer. 2019;129:41–7. doi: 10.1016/j.lungcan.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 116.Chen R, Ganesan A, Okoye I, Arutyunova E, Elahi S, Lemieux MJ. et al. Targeting B7-1 in immunotherapy. Med Res Rev. 2020;40:654–82. doi: 10.1002/med.21632. [DOI] [PubMed] [Google Scholar]
- 117.Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F. et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. The New England journal of medicine. 2018;378:2078–92. doi: 10.1056/NEJMoa1801005. [DOI] [PubMed] [Google Scholar]
- 118.Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gümüş M, Mazières J. et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. The New England journal of medicine. 2018;379:2040–51. doi: 10.1056/NEJMoa1810865. [DOI] [PubMed] [Google Scholar]
- 119.Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP. et al. Pembrolizumab for the treatment of non-small-cell lung cancer. The New England journal of medicine. 2015;372:2018–28. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 120.Hellmann MD, Paz-Ares L, Bernabe Caro R, Zurawski B, Kim S-W, Carcereny Costa E. et al. Nivolumab plus Ipilimumab in Advanced Non-Small-Cell Lung Cancer. The New England journal of medicine. 2019;381:2020–31. doi: 10.1056/NEJMoa1910231. [DOI] [PubMed] [Google Scholar]
- 121.Wang Z, Ying J, Xu J, Yuan P, Duan J, Bai H. et al. Safety, Antitumor Activity, and Pharmacokinetics of Toripalimab, a Programmed Cell Death 1 Inhibitor, in Patients With Advanced Non-Small Cell Lung Cancer: A Phase 1 Trial. JAMA Netw Open. 2020;3:e2013770. doi: 10.1001/jamanetworkopen.2020.13770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gao S, Li N, Gao S, Xue Q, Ying J, Wang S. et al. Neoadjuvant PD-1 inhibitor (Sintilimab) in NSCLC. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2020;15:816–26. doi: 10.1016/j.jtho.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 123.Herbst RS, Giaccone G, de Marinis F, Reinmuth N, Vergnenegre A, Barrios CH. et al. Atezolizumab for First-Line Treatment of PD-L1-Selected Patients with NSCLC. The New England journal of medicine. 2020;383:1328–39. doi: 10.1056/NEJMoa1917346. [DOI] [PubMed] [Google Scholar]
- 124.Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R. et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. The New England journal of medicine. 2017;377:1919–29. doi: 10.1056/NEJMoa1709937. [DOI] [PubMed] [Google Scholar]
- 125.Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R. et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. The New England journal of medicine. 2018;379:2342–50. doi: 10.1056/NEJMoa1809697. [DOI] [PubMed] [Google Scholar]
- 126.Baas P, Scherpereel A, Nowak AK, Fujimoto N, Peters S, Tsao AS. et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;397:375–86. doi: 10.1016/S0140-6736(20)32714-8. [DOI] [PubMed] [Google Scholar]
- 127.Kudo M. Scientific Rationale for Combined Immunotherapy with PD-1/PD-L1 Antibodies and VEGF Inhibitors in Advanced Hepatocellular Carcinoma. Cancers (Basel) 2020. 12. [DOI] [PMC free article] [PubMed]
- 128.Faucher JL, Lacronique-Gazaille C, Frebet E, Trimoreau F, Donnard M, Bordessoule D. et al. "6 markers/5 colors" extended white blood cell differential by flow cytometry. Cytometry A. 2007;71:934–44. doi: 10.1002/cyto.a.20457. [DOI] [PubMed] [Google Scholar]
- 129.Ramlau R, Quoix E, Rolski J, Pless M, Lena H, Lévy E. et al. A phase II study of Tg4010 (Mva-Muc1-Il2) in association with chemotherapy in patients with stage III/IV Non-small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2008;3:735–44. doi: 10.1097/JTO.0b013e31817c6b4f. [DOI] [PubMed] [Google Scholar]
- 130.Lu Y, Xue J, Deng T, Zhou X, Yu K, Deng L. et al. Safety and feasibility of CRISPR-edited T cells in patients with refractory non-small-cell lung cancer. Nat Med. 2020;26:732–40. doi: 10.1038/s41591-020-0840-5. [DOI] [PubMed] [Google Scholar]
- 131.Qu J, Mei Q, Chen L, Zhou J. Chimeric antigen receptor (CAR)-T-cell therapy in non-small-cell lung cancer (NSCLC): current status and future perspectives. Cancer Immunol Immunother. 2021;70:619–31. doi: 10.1007/s00262-020-02735-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dammeijer F, Lievense LA, Veerman GDM, Hoogsteden HC, Hegmans JP, Arends LR. et al. Efficacy of Tumor Vaccines and Cellular Immunotherapies in Non-Small-Cell Lung Cancer: A Systematic Review and Meta-Analysis. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2016;34:3204–12. doi: 10.1200/JCO.2015.66.3955. [DOI] [PubMed] [Google Scholar]
- 133.Tao L, Huang G, Shi S, Chen L. Bevacizumab improves the antitumor efficacy of adoptive cytokine-induced killer cells therapy in non-small cell lung cancer models. Med Oncol. 2014;31:777. doi: 10.1007/s12032-013-0777-3. [DOI] [PubMed] [Google Scholar]
- 134.Shi S, Wang R, Chen Y, Song H, Chen L, Huang G. Combining antiangiogenic therapy with adoptive cell immunotherapy exerts better antitumor effects in non-small cell lung cancer models. PLoS One. 2013;8:e65757. doi: 10.1371/journal.pone.0065757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kwilas AR, Ardiani A, Donahue RN, Aftab DT, Hodge JW. Dual effects of a targeted small-molecule inhibitor (cabozantinib) on immune-mediated killing of tumor cells and immune tumor microenvironment permissiveness when combined with a cancer vaccine. J Transl Med. 2014;12:294. doi: 10.1186/s12967-014-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Huang Y, Yuan J, Righi E, Kamoun WS, Ancukiewicz M, Nezivar J. et al. Vascular normalizing doses of antiangiogenic treatment reprogram the immunosuppressive tumor microenvironment and enhance immunotherapy. Proc Natl Acad Sci U S A. 2012;109:17561–6. doi: 10.1073/pnas.1215397109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Pircher A, Wolf D, Heidenreich A, Hilbe W, Pichler R, Heidegger I. Synergies of Targeting Tumor Angiogenesis and Immune Checkpoints in Non-Small Cell Lung Cancer and Renal Cell Cancer: From Basic Concepts to Clinical Reality. Int J Mol Sci. 2017. 18. [DOI] [PMC free article] [PubMed]
- 138.Wang W, Ma Y, Li J, Shi HS, Wang LQ, Guo FC. et al. Specificity redirection by CAR with human VEGFR-1 affinity endows T lymphocytes with tumor-killing ability and anti-angiogenic potency. Gene Ther. 2013;20:970–8. doi: 10.1038/gt.2013.19. [DOI] [PubMed] [Google Scholar]
- 139.Ishikura N, Sugimoto M, Yorozu K, Kurasawa M, Kondoh O. Anti-VEGF antibody triggers the effect of anti-PD-L1 antibody in PD-L1 and immune desert-like mouse tumors. Oncology reports. 2022. 47. [DOI] [PMC free article] [PubMed]
- 140.Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N. et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med. 2018;378:2288–301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 141.Herbst RS, Arkenau HT, Bendell J, Arrowsmith E, Wermke M, Soriano A. et al. Phase 1 Expansion Cohort of Ramucirumab Plus Pembrolizumab in Advanced Treatment-Naive NSCLC. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2021;16:289–98. doi: 10.1016/j.jtho.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 142.Gadgeel SM, Stevenson JP, Langer CJ, Gandhi L, Borghaei H, Patnaik A. et al. Pembrolizumab and platinum-based chemotherapy as first-line therapy for advanced non-small-cell lung cancer: Phase 1 cohorts from the KEYNOTE-021 study. Lung Cancer. 2018;125:273–81. doi: 10.1016/j.lungcan.2018.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]