Abstract
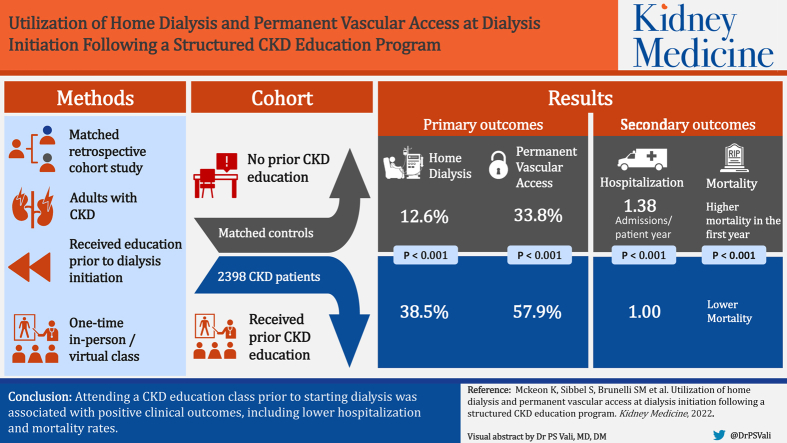
Rationale & Objective
Treatment options for kidney failure are complex, and the majority of patients transitioning to dialysis lack important information about treatment options and are not prepared to make informed decisions about their care. Correspondingly, the majority of patients who start dialysis default to in-center hemodialysis using a central venous catheter for vascular access as the initial modality; furthermore, hospital admissions, mortality, and infections are exceedingly common over the first few months.
Study Design
Matched retrospective cohort study.
Setting & Patients
2,398 adult patients with chronic kidney disease (CKD) who attended a structured CKD education program and pair-matched control patients who did not receive education before starting dialysis between January 2018 and June 2019.
Exposure
CKD education attendance documented from 2 months (60 days)-3 years before dialysis initiation. CKD education consisted of a 1-time, 90-minute, inperson or virtual class.
Outcome
Primary outcomes were dialysis modality and vascular access type on the first day of dialysis (day 0) and at day 90 after dialysis initiation. Secondary outcomes included hospitalizations and deaths during the first year of receiving dialysis.
Analytical Approach
Generalized linear models were used to compare outcomes between patients receiving CKD education and controls.
Results
Compared with controls, CKD education patients were more frequently receiving home dialysis (38.5% vs 12.6%, P < 0.001) and used a permanent vascular access (57.9% vs 33.8%, P < 0.001) at dialysis initiation; differences were minimally attenuated and remained statistically significant at day 90. Hospitalization rates were lower among CKD education patients than among controls during the first year of receiving dialysis (1.00 vs 1.38 admissions per patient-year; P < 0.001). CKD education patients also had lower mortality over the first year of receiving dialysis (P < 0.001).
Limitations
Bias and confounding cannot fully be accounted for in an observational study. Analyses only included patients with commercial and Medicare insurance who received CKD care before dialysis initiation and may not be generalizable to other patient populations.
Conclusions
Our findings indicate that attending a CKD education class before starting dialysis resulted in positive clinical outcomes, including reduction in hospitalization and mortality rates. Broad implementation of structured CKD education may result in more patients choosing home dialysis as their first treatment option and reduce the risk of adverse outcomes in the crucial early period after dialysis initiation.
Plain-Language Summary.
Treatment options for kidney failure are complex, and the majority of patients who develop kidney failure lack important information about treatment options and are not prepared to make informed decisions about their care. In the current study, we leveraged the experience from a structured CKD education program implemented across the United States to test the association of CKD education with clinical outcomes among patients starting dialysis, with emphasis placed on minimizing biases and confounding. In this analysis, CKD education patients were more likely to choose home dialysis, use a permanent vascular access at dialysis initiation, and experience lower hospitalization and mortality rates during the first year of dialysis.
The Centers for Disease Control and Prevention estimates that 1 in 7 Americans has chronic kidney disease (CKD), and each year, over 100,000 patients in the United States develop kidney failure.1,2 Patients transitioning to dialysis often experience adverse clinical outcomes in the first few months of dialysis, including frequent hospital admissions and high mortality rates.3 Despite current guidance supporting prioritization of transplantation and home dialysis, the vast majority of patients with kidney failure in the United States initiate dialysis in a clinic setting rather than at home.4, 5, 6 In addition, high rates of central venous catheter vascular access for dialysis contribute to higher infection rates and hospitalizations and, therefore, drive increased costs of care.7,8
Given the complexity of kidney disease and available treatment options, it is important that patients receive appropriate education before kidney failure to enable them to make informed decisions about their continued care. Unfortunately, the majority of patients currently starting dialysis have not received adequate CKD education.9 Previous studies have shown that structured implementation of educational programs for patients with advanced CKD is anticipated to have a positive impact on patient outcomes after dialysis initiation.10,11 Still, whether and to what degree this is the case remains unknown because prior studies failed to adequately account for the fact that patients who attend CKD education programs may be “healthier” overall and more engaged in their medical care than those who do not (“healthy-user bias”).12 If CKD education before kidney failure demonstrates a positive impact on patient outcomes, relevant policies should be developed to support broad availability and access to these programs. In the current study, we leveraged the experience from Kidney Smart (DaVita Inc), a structured CKD education class implemented across the United States, to test the association of CKD education with clinical outcomes among patients starting dialysis, with emphasis placed on minimizing biases and confounding.
Methods
This retrospective study included adult patients (aged 18 years or older) who started dialysis at a dialysis organization (DaVita Inc) between January 2018 and June 2019.
CKD Education Program
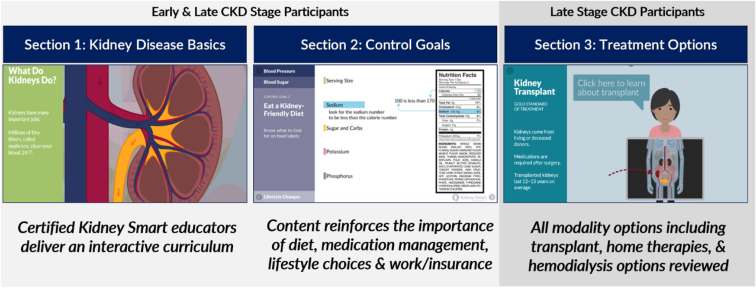
Kidney Smart seeks to help patients make informed decisions on lifestyle choices, kidney replacement modality, and other aspects of CKD and dialysis care. The education content includes an overview of CKD, diet, lifestyle, comorbid conditions management, and treatment options, including transplant, peritoneal dialysis, home hemodialysis, and in-center hemodialysis.13 The program is available as a no-cost resource to any person with kidney disease or their care-partners and family. Most patients (∼90%) who attend the program are referred by a treating physician, typically a nephrologist; other patients find the resource independently online. The program, which consists of a 90-minute class, uses adult learning principles of experience and internal motivation to increase comprehension and retention.14,15 The Kidney Smart curriculum consists of 3 sections: My Kidneys, My Choices, and My Treatment Options. In “Part 1: My Kidneys,” participants learn about kidney function, causes of kidney disease, and the stages of CKD. Participants are also invited to fill out an Action Plan to take back to their physicians for review. In “Part 2: My Choices,” participants learn about the importance of diet and adherence to medication prescription in managing their kidney disease. “Part 3: My Treatment Options” focuses on potential treatment options for kidney failure. This section reviews transplant, peritoneal dialysis, hemodialysis (home and in-center), as well as conservative management. In this section, educators reiterate the importance of a patient speaking to their physician about what modality option works best for them and their lifestyle.
The content is designed with simplified illustrations, interactive animation, and text at acceptable reading-level standards to break down complicated health concepts (Fig 1).16 The program is built with adult and neuro-learning techniques, including multimodal presentations (hands-on, where possible), memory devices including strategic repetition and alliteration, emotion-linking through character-based storytelling, and blended instruction and motivation techniques to inspire action. Classes are led in person (at dialysis clinics, nephrology offices, and community centers) or virtually (via webinar or telephone) by a clinically licensed caregiver (eg, nurse or social worker). Educators are trained to use the curriculum as a guide but to show flexibility in meeting patients’ unique needs and responsiveness to questions. Additional resources are available to patients online after the class. Since its launch in 2013, the program has educated more than 200,000 CKD patients across 49 states.
Figure 1.
Examples of Kidney Smart content.16 ©2022 DaVita Inc. Reprinted with Permission. KIDNEY SMART is a registered trademark of DaVita Inc. Abbreviation: CKD, chronic kidney disease.
Inclusion/Exclusion Criteria
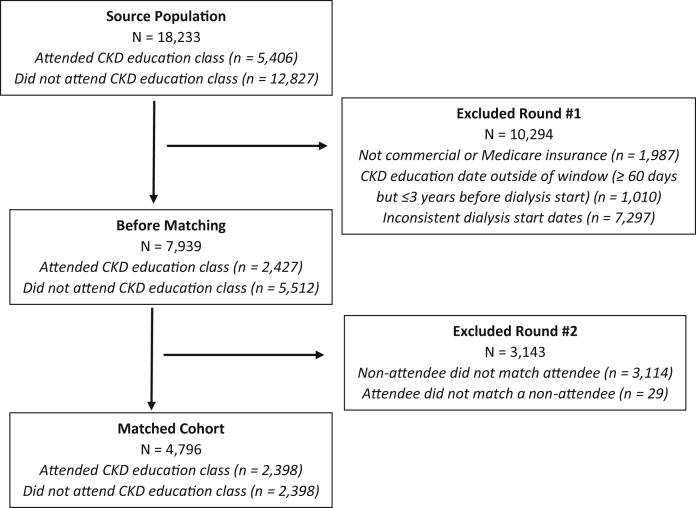
This study included patients who had either Medicare or commercial insurance as their primary insurance type; patients who had Medicaid or other types of insurance and those who were uninsured were excluded from the study because they represented a small patient population (Fig 2). Given the key role of nephrologists in referring patients to CKD education, the program is more accessible to individuals who receive CKD care before starting dialysis. Our dataset did not contain any information on whether or not a person received CKD care before dialysis. Therefore, given the low likelihood that they would have the opportunity to be referred to CKD education before dialysis initiation, the following types of patients were excluded: (1) patients with acute kidney injury; (2) patients with a prior kidney transplant; and (3) patients without an established physician relationship at the start of outpatient dialysis.
Figure 2.
Patient flow diagram. Abbreviation: CKD, chronic kidney disease.
Exposure and Outcomes
The primary exposure for our study was the attendance of the CKD education class. Patients were classified as having attended CKD education classes (yes/no) if attendance was documented from 2 months (60 days)-3 years before dialysis initiation. This time period was chosen to ensure enough time between CKD education and dialysis initiation, which would allow for patients’ preferences and choices to be reflected in clinical practice. Patients who received education outside of this time window were excluded from analysis.
Given the goals of the educational program, emphasis was placed on outcomes relevant during the period after dialysis initiation. Primary outcomes were prespecified as dialysis modality (peritoneal dialysis/home hemodialysis vs in-center hemodialysis) and vascular access type (arteriovenous graft/fistula vs central venous catheter) on the first day of dialysis (day 0) and at day 90 after dialysis initiation. In addition, we assessed annualized hospitalization events and mortality over the first year of receiving dialysis.
Analyses and Matching
In an effort to equilibrate access to the educational program, we leveraged multiple statistical techniques, including restriction and matching. We selected individuals who were likely to have had CKD care before dialysis (see Inclusion/Exclusion Criteria). Those who had attended the CKD education class were identified as eligible treatment group patients; those who did not attend the CKD education class were identified as eligible controls. For each CKD education patient, we identified a control using a hard 1:1 match with replacement, using exact matching for geographic region, patient race, and insurance type and a near match within 2 years of age. Matching was performed through a procedure available in the SAS software (surveyselect), with a 1-to-1 match ratio specified.17 In the absence of individual-level data on socioeconomic status, we linked each patient’s zip code with 2010 Census Bureau data on income, poverty, education, and unemployment and compared them between CKD education patients and controls.18
Statistical Approach
Baseline patient characteristics were described as means and standard deviations for continuous variables and counts and proportions for categorical variables and quantified as standardized mean differences. To estimate the proportion of patients receiving each dialysis modality and access type, we employed generalized linear models with a binomial distributional assumption to estimate the association of CKD education with dialysis modality (peritoneal dialysis/home hemodialysis vs in-center hemodialysis) and vascular access type (arteriovenous graft/fistula vs central venous catheter). To estimate annualized hospitalization rates between matched groups, generalized linear models with Poisson distributional assumptions were used to estimate the annualized hospitalization rate. First-year survival was estimated through time to event analyses with a Kaplan-Meier model.
According to 45 C.F.R. part 46 from the US Department of Health and Human Services, this study was exempt from institutional review board or ethics committee approval. We adhered to the Declaration of Helsinki, and informed consent was not required because we used deidentified information. The study was deemed exempt by Quorum Institutional Review Board (Seattle, Washington). Exposure data were obtained from the CKD education database; clinical outcomes were derived from the dialysis organization electronic health records. After linkage, statistical analysis files were provided to researchers in deidentified form for analysis. All analyses were performed using SAS software version 9.4.
Results
Among the 18,233 patients starting dialysis with the dialysis organization during the study period, 29% had received CKD education before kidney failure. Of the 2,427 eligible patients with CKD education attendance and the 5,512 eligible controls, 2,398 CKD education patients were successfully pair-matched (Fig 2; Table 1).19,20 After matching, demographic and clinical characteristics were well balanced between CKD education patients and control groups (Table 1).19,20 No meaningful differences were observed in zip code–level socioeconomic status factors between CKD education patients and controls (Table 2).18
Table 1.
Demographic and Clinical Characteristics Among CKD Education Patients and Controls Before and After Matching
| Before Matching |
After Matching |
|||||
|---|---|---|---|---|---|---|
| CKD Education Patients N = 2,427 |
Controls N = 5,512 |
Std Diffa % |
CKD Education Patients N = 2,398 |
Controls N = 2,398 |
Std Diffa % |
|
| Age, y, mean ± SD | 65.2 ± 13.0 | 65.9 ± 13.9 | −5.1 | 65.4 ± 12.6 | 65.4 ± 12.6 | 0.0 |
| Female, n (%) | 983 (40.5%) | 2,316 (42.0%) | −3.0 | 975 (40.7%) | 964 (40.2%) | 1.0 |
| Race, n (%) | ||||||
| Black | 503 (20.7%) | 1,207 (21.9%) | −2.9 | 502 (20.9%) | 502 (20.9%) | 0.0 |
| White | 1,282 (52.8%) | 2,526 (45.8%) | 14 | 1,273 (53.1%) | 1,273 (53.1%) | 0.0 |
| Hispanic | 311 (12.8%) | 703 (12.8%) | 0 | 303 (12.6%) | 303 (12.6%) | 0.0 |
| Asian | 226 (9.3%) | 712 (12.9%) | −11.2 | 100 (4.2%) | 100 (4.2%) | 0.0 |
| Other | 105 (4.3%) | 364 (6.6%) | −9.8 | 220 (9.2%) | 220 (9.2%) | 0.0 |
| Primary insurance, n (%) | ||||||
| Commercial | 752 (31.0%) | 1,509 (27.4%) | 8 | 733 (30.6%) | 733 (30.6%) | 0.0 |
| Medicare | 1,675 (69.0%) | 4,003 (72.6%) | −8 | 1,665 (69.4%) | 1,665 (69.4%) | 0.0 |
| US regionb, n (%) | ||||||
| West | 588 (24.2%) | 1,816 (32.9%) | −19.2 | 584 (24.4%) | 584 (24.4%) | 0.0 |
| Midwest | 550 (22.7%) | 1,002 (18.2%) | 11.4 | 540 (22.5%) | 540 (22.5%) | 0.0 |
| Northeast | 458 (18.9%) | 990 (18.0%) | 2.3 | 447 (18.6%) | 447 (18.6%) | 0.0 |
| South | 831 (34.2%) | 1,704 (30.9%) | 7.1 | 827 (34.5%) | 827 (34.5%) | 0.0 |
| BMI, kg/m2, mean ± SD | 29.9 ± 7.1 | 29.2 ± 7.6 | 9.4 | 29.9 ± 7.1 | 29.6 ± 7.5 | 0.0 |
| Diabetes, n (%) | 807 (33.3) | 1,893 (34.3) | −2.1 | 789 (32.9) | 787 (32.8%) | 0.2 |
Table 2.
2010 Census Zip Code–Level Indicators of Socioeconomic Status for CKD Education Patients and Controls18
| CKD Education Patients N = 2183 |
Controls N = 2148 |
|
|---|---|---|
| Household income, US$ | ||
| Mean ± SD | 55,639 ± 20,046 | 56,998 ± 21,451 |
| Median (IQR) | 51,721 (41,650-67,355) | 52,583 (41,089-70,041) |
| Aged 25 years or older with a Bachelor degree, % | ||
| Mean ± SD | 32.53 ± 15.13 | 32.44 ± 16.01 |
| Median (IQR) | 30.10 (20.10-41.60) | 29.60 (19.30-43.10) |
| Residents below poverty line, % | ||
| Mean ± SD | 14.13 ± 8.20 | 13.91 ± 8.53 |
| Median (IQR) | 12.20 (7.80-18.60) | 11.90 (7.40-18.90) |
| Unemployment, % | ||
| Mean ± SD | 5.79 ± 2.67 | 5.72 ± 2.74 |
| Median (IQR) | 5.30 (3.90-7.00) | 5.20 (3.90-6.80) |
Abbreviations: CKD, chronic kidney disease; IQR, interquartile range; SD, standard deviation.
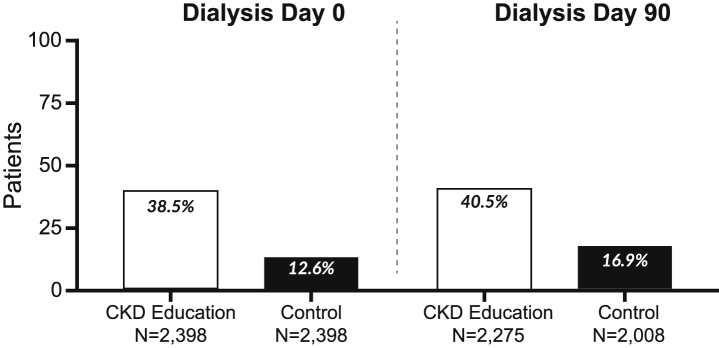
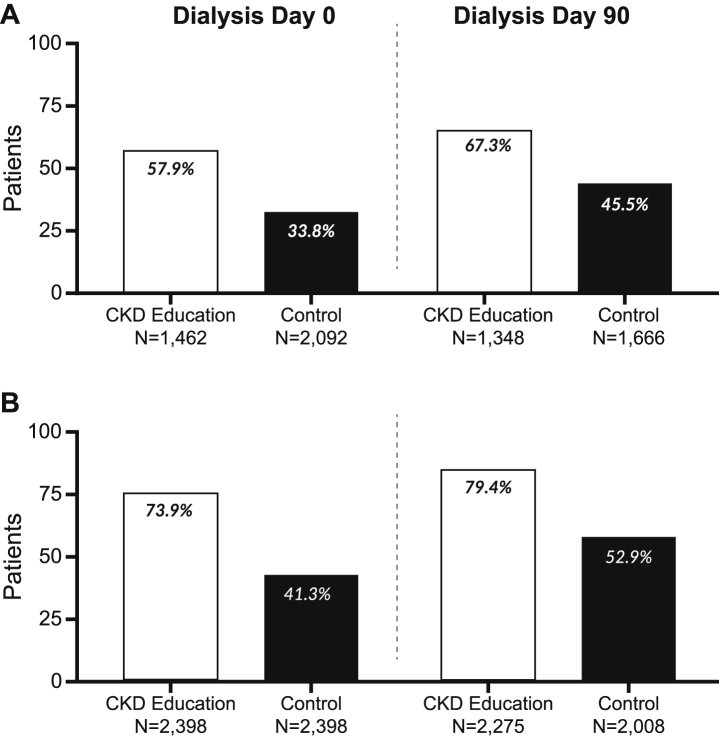
Home dialysis (peritoneal dialysis/home hemodialysis) was more common in patients who received CKD education than in controls both at day 0 (38.5% vs 12.6%, P < 0.001) and day 90 (40.5% vs 16.9%, P < 0.001) (Fig 3). Among hemodialysis patients treated at a dialysis center, the use of a permanent vascular access was more frequent in patients who received CKD education than in controls on both day 0 (57.9% vs 33.8%, P < 0.001) and day 90 (67.3% vs 45.5%, P < 0.001) (Fig 4A). The overall proportion of patients receiving hemodialysis (in-center or at home) via a permanent vascular access was higher among patients who received CKD education than among controls both at day 0 (73.9% vs 41.3%, P < 0.001) and day 90 of dialysis (79.4% vs 52.9%, P < 0.001) (Fig 4B).
Figure 3.
Home dialysis use among matched chronic kidney disease (CKD) education patients and controls at dialysis day 0 and dialysis day 90. Home dialysis was defined as peritoneal dialysis or home hemodialysis.
Figure 4.
Permanent vascular access use among matched chronic kidney disease (CKD) education patients and controls at dialysis day 0 and dialysis day 90. (A) Among patients receiving in-center hemodialysis. (B) Among patients receiving either in-center or home hemodialysis. Permanent vascular access was defined as either arteriovenous fistula or arteriovenous graft.
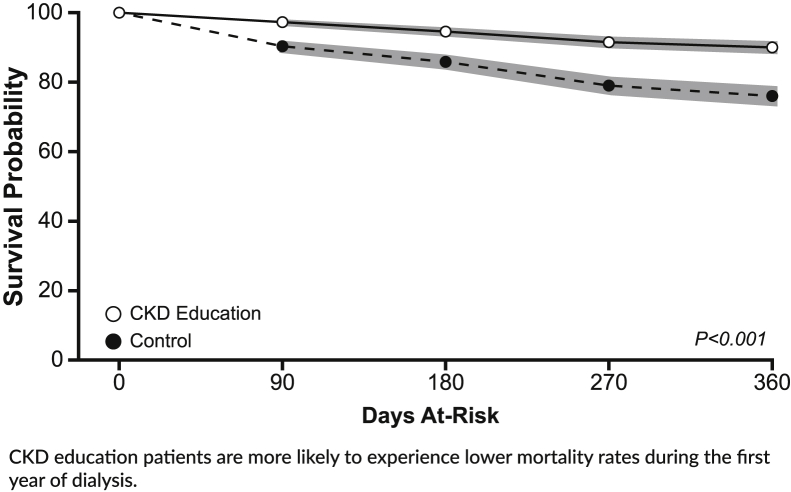
Over the first year of dialysis, patients who received CKD education contributed 2,625 patient-years at risk, during which time they experienced 2,617 hospitalizations, corresponding to an incidence rate of 1.00 admission per patient-year. Matched controls contributed 2,252 patient-years at risk, during which there were 3,106 hospitalizations, corresponding to an incidence rate of 1.38 admissions per patient-year. The corresponding incidence rate ratio (95% confidence interval) was 0.71 (0.68-0.75), favoring CKD education (P < 0.001) (Fig 5). In addition, CKD education patients also had lower mortality over the first year of receiving dialysis (P < 0.001) (Fig 6).
Figure 5.
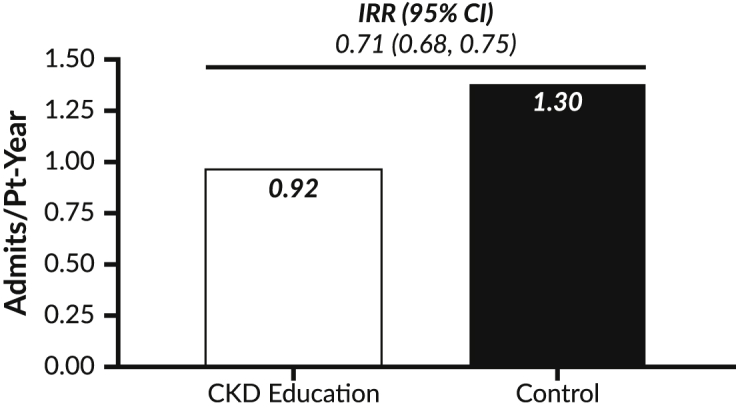
Hospitalization rates among matched chronic kidney disease (CKD) education patients and controls. Abbreviations: CI, confidence interval; IRR, incidence rate ratio; Pt, patient.
Figure 6.
Survival among matched chronic kidney disease (CKD) education patients and controls.
Discussion
In this analysis, a structured CKD education program was associated with improved clinical outcomes in the critical early period after dialysis initiation among patients who received CKD care before dialysis initiation. CKD education patients were more likely to choose home dialysis and use a permanent vascular access at dialysis initiation and experienced lower hospitalization and mortality rates during the first year of dialysis.
The positive effects of structured education on health outcomes are well recognized in a variety of settings, both in dialysis patients and the general population.21, 22, 23 Published literature suggests that structured CKD education programs may improve quality of life and clinical outcomes.10 However, prior studies failed to adequately account for confounding related to self-selection of patients attending education programs.10 To address this issue, in the present study, we placed particular emphasis on isolating the independent association of CKD education by applying restriction, matching, and modeling techniques. Reassuringly, our results are consistent with other studies reporting that CKD education is independently and strongly associated with better clinical outcomes and appears to be additive to the benefits of CKD care alone. Another strength of our study is the large sample size—one of the largest assessments to date—and from the inclusion of a contemporary study sample with broad geographic and demographic representation, thus supporting generalizability of these results to the broad population of patients starting dialysis in the United States.
The intervention we evaluated is a structured education that is implemented consistently for each patient and leverages adult learning techniques, visualizations, and plain language to accommodate a broad range of health literacy among program attendees.14,16 CKD education informs patients through instruction on self-management techniques (eg, blood pressure control and dietary recommendations) and by providing knowledge of available treatment options (ie, permanent vascular access vs a catheter, home dialysis vs in-center hemodialysis) and their impact on quality of life. Together, these steps contribute to empowering patients in their own care, promoting shared decision making, and choosing treatment options that best fit their lives—all of which can lead to better health outcomes.15,21,24
Despite the potential benefits of a CKD education program, a large proportion of patients (30%-89%) receive very little or no information before dialysis initiation.12,25, 26, 27 The rate of CKD education attendance in this study is comparable with that in previous studies, with roughly one-third of the qualifying patients attending a class. This could be because of many factors, including urgent dialysis initiation, patients’ lack of interest or unwillingness to attend an educational class, or lack of CKD education opportunities.26, 27, 28 Policies that support a broader implementation of structured CKD education programs are urgently needed in light of the ambitious goals for home dialysis and preemptive transplantation at the early stages of kidney failure recently set forth by the US Health and Human Services4 along with broader implementation a standardized platform that could enable more widespread CKD education in the United States. Prior studies have acknowledged this need; however, to date, no large scale studies on CKD platforms have been performed.29
This study has several limitations. First, despite our extensive efforts to minimize bias and confounding, such effects can never be completely eliminated in an observational setting, and healthy-user bias is still likely to play a role in these findings. Second, although there was no imbalance observed in zip code–level income, poverty, education, and unemployment status, the lack of data on patient health care engagement precluded us from accounting for potential confounding on the basis of other “self-care behaviors” (eg, adherence to pharmacological therapy and medical appointments, compliance with dietary recommendations, etc). A better understanding of how patients with advanced CKD seek access to and engage in kidney education programs is a potential future direction of this research. Given these considerations, our results represent the upper bound (largest effect) of the true impact of CKD education because we were unable to fully account for self-selection of patients who choose to participate in CKD education. Only a randomized controlled study would fully address this issue. Additionally, caution should be exercised in extrapolating these findings to patients who were excluded from this study to minimize confounding, such as those who did not have insurance coverage or those who did not receive predialysis nephrology care. Moreover, given data availability, we were only able to study patients who went on to initiate dialysis. Therefore, the effect of CKD education on health outcomes in the predialysis phase, including on preemptive transplantation and delaying the clinical progression of CKD, could not be examined.
Our results provide additional evidence that CKD education plays a key role in optimizing outcomes for patients with kidney failure starting dialysis. Novel approaches are needed to ensure that all patients with advanced CKD have access to predialysis education and ensure broad implementation of structured programs.
Article Information
Authors’ Full Names and Academic Degrees
Katherine Mckeon, MSPH, Scott Sibbel, MPH, PhD, Steven M. Brunelli, MSCE, MD, Erin Matheson, BA, Nick Lefeber, MBA, Meghan Epps, BS, and Francesca Tentori, MS, MD
Authors’ Contributions
Research idea and study design: SS, EM, NL, ME, SMB, FT; data acquisition: KM; data analysis/interpretation: KM, SMB, FT; statistical analysis: KM, SS; supervision or mentorship: SS, FT. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
None.
Financial Disclosure
Author Mckeon was an employee of DaVita Clinical Research at the time of manuscript preparation. Drs Sibbel, Brunelli, and Tentori are current employees of DaVita Clinical Research. Dr Brunelli’s spouse is an employee of AstraZeneca. Authors Matheson, Lefeber, and Epps are current employees of DaVita, Inc.
Peer Review
Received January 7, 2022 as a submission to the expedited consideration track with 3 external peer reviews. Direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form April 1, 2022.
Footnotes
Complete author and article information provided before references.
References
- 1.Chronic kidney disease basics. Centers for Disease Control and Prevention. February 7, 2020. https://www.cdc.gov/kidneydisease/basics.html
- 2.US Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2020. USRDS 2020 Annual Data Report: Epidemiology of kidney disease in the United States. [Google Scholar]
- 3.Chang C.H., Fan P.C., Kuo G., et al. Infection in advanced chronic kidney disease and subsequent adverse outcomes after dialysis initiation: a nationwide cohort study. Sci Rep. 2020;10(1):2938. doi: 10.1038/s41598-020-59794-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United States, Centers for Medicare and Medicaid, Health and Human Services, and Executive Order of the President (Donald Trump). Medicare program; end-stage renal disease prospective payment system, payment for renal dialysis services furnished to individuals with acute kidney injury, and end-stage renal disease quality incentive program. Executive Order 42 CFR Part 413, Federal Register, vol 85, no. 217; 2020:71398-71487.
- 5.Center for Medicare and Medicaid Services . 2021. ESRD Treatment Choices (ETC) Model.https://innovation.cms.gov/innovation-models/esrd-treatment-choices-model [Google Scholar]
- 6.Flanagin E.P., Chivate Y., Weiner D.E. Home dialysis in the United States: a roadmap for increasing peritoneal dialysis utilization. Am J Kidney Dis. 2020;75(3):413–416. doi: 10.1053/j.ajkd.2019.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad M., Wallace E.L., Jain G. Setting up and expanding a home dialysis program: is there a recipe for success? Kidney360. 2020;1(6):569–579. doi: 10.34067/KID.0000662019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Himmelfarb J., Vanholder R., Mehrotra R., Tonelli M. The current and future landscape of dialysis. Nat Rev Nephrol. 2020;16(10):573–585. doi: 10.1038/s41581-020-0315-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nicholas S.B., Kalantar-Zadeh K., Norris K.C. Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis. 2015;22(1):6–15. doi: 10.1053/j.ackd.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez-Vargas P.A., Tong A., Howell M., Craig J.C. Educational interventions for patients with CKD: a systematic review. Am J Kidney Dis. 2016;68(3):353–370. doi: 10.1053/j.ajkd.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Narva A.S., Norton J.M., Boulware L.E. Educating patients about CKD: the path to self-management and patient-centered care. Clin J Am Soc Nephrol. 2016;11(4):694–703. doi: 10.2215/CJN.07680715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lacson E., Jr., Wang W., DeVries C., et al. Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis. 2011;58(2):235–242. doi: 10.1053/j.ajkd.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Kidney smart FAQs DaVita. 2021. https://www.davita.com/education/kidney-smart-classes/kidney-smart-faqs
- 14.Knowles M.S. Cambridge Adult Education; 1980. The Modern Practice of Adult Education: From Pedagogy to Andragogy. [Google Scholar]
- 15.Lomen L.D. Nova University; 1974. To Develop the Learning Theory and Curriculum for a Health Class for Elderly Adults; p. 23. [Google Scholar]
- 16.2019 HERMES - Platinum Interactive Media: Web-based Training 2019 AVA Digital Awards - Platinum Web-based Element: Training/E-Learning2019 Digital Health Awards - Bronze Web-based Digital Health.
- 17.PROC SURVEYSELECT Statement. SAS Institute, Inc. https://go.documentation.sas.com/doc/en/pgmsascdc/9.4_3.3/statug/statug_surveyselect_syntax01.htm
- 18.US Census Bureau . American Community Survey; 2010. Educational attainment–5 year estimates.https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2014/5-year.html [Google Scholar]
- 19.Austin P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.2010 census regions and divisions of the United States. United Sttates Census Bureau. https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html
- 21.Adams R.J. Improving health outcomes with better patient understanding and education. Risk Manag Healthc Policy. 2010;3:61–72. doi: 10.2147/RMHP.S7500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gadola L., Poggi C., Poggio M., et al. Using a multidisciplinary training program to reduce peritonitis in peritoneal dialysis patients. Perit Dial Int. 2013;33(1):38–45. doi: 10.3747/pdi.2011.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klang B., Björvell H., Clyne N. Predialysis education helps patients choose dialysis modality and increases disease-specific knowledge. J Adv Nurs. 1999;29(4):869–876. doi: 10.1046/j.1365-2648.1999.00957.x. [DOI] [PubMed] [Google Scholar]
- 24.Subramanian L., Zhao J., Zee J., et al. Use of a decision aid for patients considering peritoneal dialysis and in-center hemodialysis: a randomized controlled trial. Am J Kidney Dis. 2019;74(3):351–360. doi: 10.1053/j.ajkd.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 25.Marrón B., Martínez Ocaña J.C., Salgueira M., et al. Analysis of patient flow into dialysis: role of education in choice of dialysis modality. Perit Dial Int. 2005;25(Suppl 3):S56–S59. [PubMed] [Google Scholar]
- 26.Yeoh H.H., Tiquia H.S., Abcar A.C., Rasgon S.A., Idroos M.L., Daneshvari S.F. Impact of predialysis care on clinical outcomes. Hemodial Int. 2003;7(4):338–341. doi: 10.1046/j.1492-7535.2003.00059.x. [DOI] [PubMed] [Google Scholar]
- 27.Ribitsch W., Haditsch B., Otto R., et al. Effects of a pre-dialysis patient education program on the relative frequencies of dialysis modalities. Perit Dial Int. 2013;33(4):367–371. doi: 10.3747/pdi.2011.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehrotra R., Marsh D., Vonesh E., Peters V., Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 2005;68(1):378–390. doi: 10.1111/j.1523-1755.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- 29.Van den Bosch J., Warren D.S., Rutherford P.A. Review of predialysis education programs: a need for standardization. Patient Prefer Adherence. 2015;9:1279–1291. doi: 10.2147/PPA.S81284. [DOI] [PMC free article] [PubMed] [Google Scholar]