Abstract
Background
Many adolescent girls in Ethiopia and elsewhere missed school during their monthly cycles due to a lack of affordable menstrual absorbent materials or money to buy sanitary pads. So far, few studies have looked into the relationship between earning pocket money and maintaining good menstrual hygiene. Hence, this systematic review and meta-analysis aimed to synthesize the best available evidence regarding the association between earning pocket money and menstrual hygiene management among adolescents in Ethiopia.
Methods
We systematically searched PubMed, Hinari, Science Direct, Cochrane Library, ProQuest, POPLINE, African Journal Online, Direct of Open Access Journals, and Google Scholar for studies examining the association between earning pocket money and menstrual hygiene management among adolescent girls in Ethiopia, without restriction in a publication year. The Joanna Briggs Institute quality assessment tool for the cross-sectional studies was used to assess the quality of included studies. A prefabricated checklist, including variables: first author, publication year, sample size, type of questionnaire, and the region was used to extract data from the selected articles. A random-effect meta-analysis model was used to estimate the pooled odds ratio (OR) of the association between earning pocket money and menstrual hygiene management. The heterogeneity and publication bias was assessed by using I2 test statistics and Egger’s test, respectively.
Results
Data from nine studies involving 4783 adolescent girls were extracted. The meta-analysis revealed that adolescent girls who earned pocket money from their parents or relative had 1.64 times higher odds of having good menstrual hygiene management than their counterparts [pooled OR = 1.64, 95% CI: 1.16–2.34, I2:66.7%, n = 7 (number of studies)]. Similarly, the likelihood of having good menstrual hygiene management was lower by 49% among adolescent girls who did not receive any pocket money from their parents compared to their counterparts (pooled OR = 0.51, 95% CI: 0.35–0.74, I2:48.4%, n = 2).
Conclusions
The findings revealed that adolescent girls who earned pocket money were more likely to practice good menstrual hygiene management. Progress toward better menstrual hygiene will necessitate consideration of this factor.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12905-022-01855-2.
Keywords: Menstrual hygiene, Adolescent girls, Pocket money, Sanitary pad, Ethiopia
Background
Menstruation is a normal part of a woman's sexual health during her childbearing years; however, girls are almost globally stigmatized and discriminated against for this natural process [1]. Menstrual hygiene management (MHM) refers to the use of clean menstrual management material to absorb or collect menstrual blood by women and adolescent girls. It is a part of overall sexual and reproductive health rights, based on all individuals' ability to decide over their bodies and live healthy and productive lives [2–4].
Lack of adequate water, sanitation, and hygiene (WASH) facilities, as well as limited access to affordable menstrual absorbent materials, cause adolescent girls' menstrual hygiene needs to go unmet in low-income settings [5]. In many cases, adolescent girls in low-income settings have developed their own menstrual hygiene practices to cope with menstruation [6]. These management techniques include the use of homemade clothes, old rags, underwear, sponges, and other poor materials for their periods [7–10]. These management techniques can be unsanitary and risky [6]. Poor menstrual hygiene can lead to a range of reproductive tract infections, such as urogenital infections [6, 11]. Torondel et al. suggested that lower reproductive tract infections were protected by changing absorbent pads more frequently [11]. According to UNICEF, girls should also change their menstrual absorbent materials three or four times a day [12].
The cost of commercial sanitary pads, a lack of water and latrine facilities, and poor knowledge of menstruation are important impediments to schoolgirls managing their periods [13–16]. Furthermore, girls in SSA miss school during menstruation due to a lack of menstrual products, physical pain, and fear of smelling or leaking blood on their school uniform [7, 17–19]. Sadly, in certain situations, girls engage in transactional sex to purchase sanitary pads and obtain pads from boyfriends to manage their menses [18–21]. According to a Kenyan qualitative study, girls' monthly struggle to buy sanitary pads can lead to sexual risk behaviors and raise the risk of STIs [21]. A cluster randomized controlled trial (RCT) in rural Kenya reported that providing menstrual hygiene management materials was associated with a lower risk of sexually transmitted infection (STI) [22].
For many adolescent girls in Ethiopia, the onset of menstruation could result in some amount of embarrassment and even fear due to poor family support [1, 23]. This is exacerbated further by society's negative attitudes, societal norms, and limited access to menstruation absorbent materials [1, 7, 10, 13]. Menstruation causes 32% of Ethiopian girls to miss one or more days of school each month [2]. Moreover, 48.9% of Ethiopian adolescent girls practiced poor menstruation hygiene [24]. There has been increasing evidence on the association between earning pocket money and good menstrual hygiene management [10, 23, 25–31]. However, existing studies have been small-scale or localized by area, and the conclusions made by those studies are inconsistent. For this reason, unequivocal evidence was not drawn at the national level. Therefore, we aimed to synthesize the best available evidence, and quantify the strength and direction of the association between earning pocket money and menstrual hygiene management among adolescents in Ethiopia. Evidence on the pooled estimate has the potential to move menstrual management forward.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [32] were used to prepare and present this systematic review and meta-analysis (Additional file 1).
We employed the PEO (Population, Exposure of interest, Outcome) technique to establish inclusion and exclusion criteria.
Eligibility criteria
Population Adolescent girls (age 10–19).
Exposure of interest Earning pocket money.
Outcome of interest Good menstrual hygiene management.
Study designs All observational study designs reporting the association between earning pocket money and menstrual hygiene were considered. In addition, studies that presented an adjusted odds ratio (OR) to assess the association between earning pocket money and menstrual hygiene management were considered for inclusion in the meta-analysis.
Study setting Only studies conducted in Ethiopia.
Publication status Both published and unpublished studies were considered.
Study period There was no restriction on the publication date.
Language Articles published in the English language were considered.
Year of publication All publications reported up to September 15, 2021, were considered.
Exclusion criteria
Study design: systematic reviews, commentaries, letters to editors, short communications, and qualitative studies were excluded. We also excluded articles, which were not fully accessed.
Information sources
The following databases were subjected to a thorough search with no time limit. PubMed/MEDLINE, Science Direct, Google Scholar, Hinari, ProQuest, Directory of Open Access Journals, POPLINE, and Cochrane Library from inception to September 15, 2021.
Searching strategy
The following key search terms and Medical Subject Headings [MeSH] were used ("Adolescent [MeSH Terms], OR Adolescents [Text Word], OR adolescence, OR puberty, OR peer, OR school”) AND (“Menstruation [MesH], OR menstrual, OR menses” AND “Hygiene [MesH], OR hygiene, OR hygienically, OR sanitation, OR sanitary, OR Feminine ‘’Hygiene Products’’ [MesH], OR ‘’Menstrual Hygiene Products’’ [MesH]”) AND (“Ethiopia”) separately or in combination with the Boolean operator’s terms “AND” and “OR” (Additional file 2). The electronic database search was supplemented with gray literature searches via Google scholar and Google searching. Some research centers, including the Addis Ababa Digital Library, were searched to find gray literature in the field of our systematic review and meta-analysis. A secondary search method is known as "footnote chasing" has been used to identify relevant articles.
This systematic review and meta-analysis include all articles published till September 15, 2021, and the search was conducted between August 15 and September 15, 2021.
Study selection process
Two investigators (BS and DA) independently screened and identified eligible articles by title, abstract, and full text against preset inclusion and exclusion criteria. The two authors (BS and DA) compiled the screened articles, and disagreements between them were resolved by discussion. In this review, all the searched articles were exported into the EndNote version X8 software, and subsequently, the duplicate articles were removed. Screening of retrieved article titles, abstracts, and full-text quality was conducted independently by two review authors (BS and DA) based on the eligibility criteria.
Data collection process
Microsoft Excel was used to extract the data. Two authors (BS and DA) retrieved all necessary data independently using a predefined data extraction form. Any disagreements that arose during the data abstraction process were settled through discussion. The primary author, publication year, study design, study area, sample size, response rate, the proportion of good menstrual hygiene management, and confounder adjusted OR were all included in the data extraction format. EndNote version 8 reference manager software was utilized to collect search outcomes and remove duplicate articles.
Risk of bias assessment of the studies
The Joanna Briggs Institute (JBI) quality evaluation method was used to assess the quality of the included studies [33]. The quality of the included studies was assessed independently by two reviewers (BS and DA). The evaluation tool has nine parameters. Failure to satisfy any of the parameters resulted in a 1, otherwise in a 0. We agreed to assign a 1 to an item when the information provided was insufficient to make a decision (a failure to satisfy a specific item or unclear). Bias risks were categorized as low (total score of 0 to 2), moderate (total score of 3 or 4), or high (total score of 5 or higher) [33].
Synthesis of results
For statistical analysis, the extracted data were imported into STATA version 14 software. First, we extracted the adjusted ORs from all studies that were included. The adjusted odds ratios (AOR) were then pooled using the generic inverse variance method, which involved converting the adjusted odds ratio to a logarithmic scale and then calculating standard error [SE] based on the 95% confidence intervals. The Cochran Q (Standard X2) test and Haggin I2 statistics were used to assess the presence and degree of heterogeneity among included studies. The tests indicate the presence of average heterogeneity among included studies [I2 = 66.7%, p-value = 0.006]. Thus, the ORs were pooled using random-effect meta-analysis techniques using the DerSimonian and Laird method, which accounts for the variation between studies [34]. The pooled ORs along with their 95% confidence intervals [CI] were presented using a forest plot.
Publication bias
In this meta-analysis, possible publication bias was visualized through funnel plots. A symmetrical large inverted funnel resembled the absence of publication biases. Also, the probability of publication biases was tested using Egger's weighted regression test.
Additional analyses
Subgroup analysis and meta-regression
We performed a subgroup analysis based on geographical regions, sampling methods, method of data collection, sample size, publication year, and the type of confounders adjusted in a primary study. Further statistical analyses such as univariate meta-regression were also performed to identify the possible sources of heterogeneity.
Sensitivity analysis
Sensitivity analysis using a random-effects model was performed to assess the influence of a single study on the overall pooled odds ratio estimate.
Operational definition
Good menstrual hygiene management
Adolescent girls use a clean menstrual management material to absorb or collect blood that can be changed in privacy as often as necessary for the duration of the menstruation period, using soap and water for washing the body as required, and having access to facilities to dispose of used menstrual management materials.
Earning pocket money
In this article, the term "pocket money" refers to any amount of money received by adolescent girls from family or relatives to purchase menstrual hygiene products.
Results
Study selection
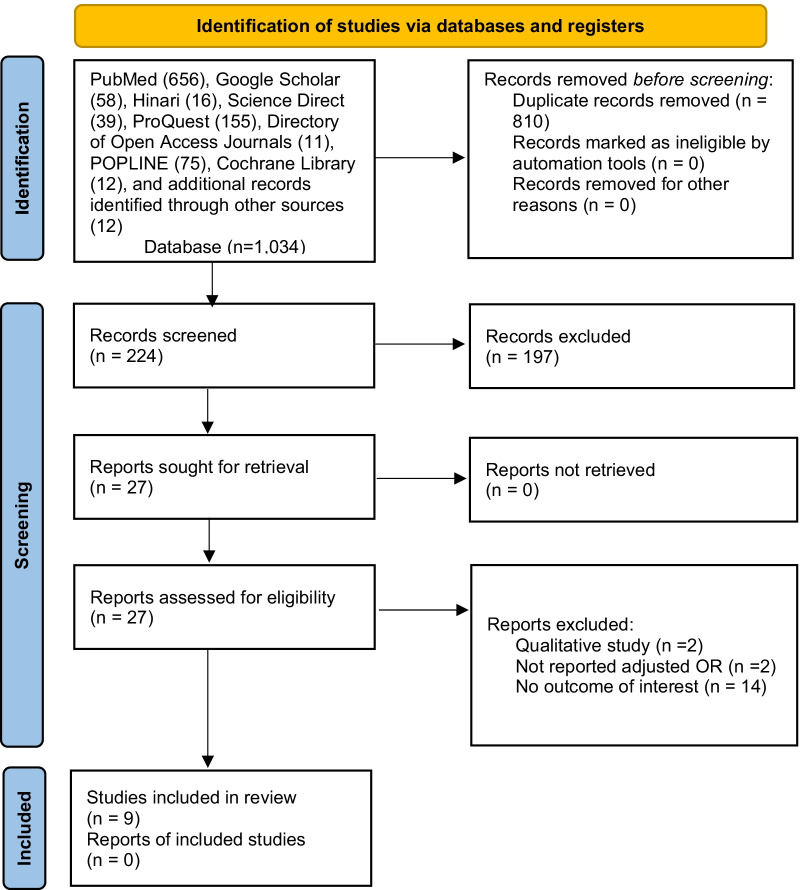
Through all database searches, a total of 1034 studies were found. A total of 810 duplicate records were removed. One hundred ninety-seven articles were excluded after screening 224 studies based on their title and abstract. Then, based on the eligibility criteria, 27 studies were assessed for eligibility. Finally, this systematic review and meta-analysis included 9 studies [10, 23, 25–31] (Fig. 1).
Fig. 1.
Flow chart of study selection for systematic review and meta-analysis of menstrual hygiene management and its association with earning pocket money among adolescent girls in Ethiopia, 2014–2021
Study characteristics
As seen in Table 1, the maximum and minimum sample sizes were found in studies conducted by Felleke A., et al. (n = 301) in Eastern Ethiopia [28] and Upashe SP., et al. (n = 828) in Western Ethiopia [25], respectively. This systematic review and meta-analysis comprised a total of 4783 participants. The confounder adjusted odds ratio for examining the link between earning pocket money and menstrual hygiene management was reported in nine of the studies [10, 23, 25–31] (Table 2).
Table 1.
List of included studies in the systematic review and meta-analysis of the association between earning pocket money and good menstrual hygiene management among adolescent girls in Ethiopia [2014–2021]
| Author’s name, year of publication | Study area | Region | Study design | Methods of data collection | Sampling | Included sample size | Response rate | Good MHM | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|
| Kitesa B et al., 2016 [10] | Shoa zone | Oromia | Cross-sectional | Interviewer administered questionnaire | Multistage sampling | 430 | 100 | 70.2 | Low |
| Habtegiorgis Y et al., 2021[23] | Dessie | Amhara | Cross-sectional | Interviewer administered questionnaire | Multistage sampling | 536 | 98.2 | 53.9 | Moderate |
| Upashe SP et al., 2015 [25] | Nekemte | Oromia | Cross-sectional | Self-administered structured questionnaire | Simple random sampling | 828 | 98 | 39.9 | Low |
| Abita Z et al.,2021 [26] | Finot selam | Amhara | Cross-sectional | Self-administered structured questionnaire | A stratified sampling technique | 442 | 99.1 | 68.8 | Low |
| Anchebi HT et al., 2017 [27] | Adama | Oromia | Cross-sectional | Self-administered structured questionnaire | Multistage stratified sampling | 398 | 94.3 | 57 | Low |
| Felleke AA et al., 2021 [28] | Harari | Harari | Cross-sectional | Self-administered structured questionnaire | Systematic sampling | 301 | 100 | 55.8 | Moderate |
| Hasan JH, 2021 [29] | Chelenko | Oromia | Cross-sectional | Self-administered structured questionnaire | Simple random sampling | 482 | 99 | 68 | Moderate |
| Kedir T, 2017 [30] | West Shoa | Oromia | Cross-sectional | Interviewer administered questionnaire | Multistage stratified sampling | 610 | 98.7 | 45.6 | Low |
| Biruk E et al., 2018 [31] | Addis Ababa | Addis Ababa | Cross-sectional | Self-administered structured questionnaire | Multistage sampling | 756 | 98 | 52.5 | Low |
SNNPR South Nations and Nationalities People of the Region; MHM Menstrual hygiene management
Table 2.
Primary studies with available odds ratios of the association between earning pocket money and good menstrual hygiene management among adolescent girls in Ethiopia [2014–2021]
| Author’s name, year of publication | Study design | COR [95%CI] | AOR [95%CI] | Reference category | Interpretations of a significant finding | Adjusted confounders |
|---|---|---|---|---|---|---|
| Kitesa B et al., 2016 [10] | Cross-sectional | 1.9[1.15–3.12] | 1.5[0.87–2.59] | A | Not significant | Educational status, religion, father's educational status, mother's educational status, and access to washing facilities |
| Habtegiorgis Y et al., 2021 [23] | Cross-sectional | 2.66[1.58–4.50] | 2.08 [1.15,3.78] | A | Girls who asked for money to purchase pads were two times more likely to practice good menstrual hygiene than those who did not ask [AOR = 2.08, 95% CI: [1.15–3.78] | Age, grade, marital status, live with, maternal education, paternal education, maternal occupation, paternal occupation, regular menses, duration of menses flow, knowledge status, discuss menstrual hygiene with friends, communicate about menstruation with family, and water source functionality in the school |
| Upashe SP et al., 2015 [25] | Cross-sectional | 2.65 [1.76–4.00] | 2.73 [1.76,4.26] | A | Girls who earn permanent pocket money from families were nearly three times more likely to have good practice about menstrual hygiene compared to those who don’t earn permanent pocket money from families [AOR = 2.73, 95% CI: 1.76 – 4.26] | Educational status of the mothers, educational status of the father, occupational status of the mother, and monthly income |
| Abita Z et al.,2021 [26] | Cross-sectional | 2.03 [1.35, 3.05] | 0.76[0.45,1.29] | A | Not significant | Residency, mother's educational status, father's educational status, father's occupation, wealth index, hearing about menstruation before menarche, discussion with parents about menstruation, learning about menstrual hygiene in the school, and know sanitary pads in the market |
| Anchebi HT et al., 201s7 [27] | Cross-sectional | 1.71[0.84,3.50] | 2.27[1.07,4.77] | A | Students whose source of money was their parents were 2.27 times more likely to have a good menstrual hygiene practices than students who earn money by themselves [AOR = 2.27;95% CI = 1.08, 4.77] | Age, mother's educational level, father's educational level, and school uncomfortable to keep hygiene |
| Felleke AA et al., 2021 [28] | Cross-sectional | 0.39[0.24,0.64] * | 0.36[0.19,0.65] | B | Adolescent girls who have no permanent pocket money from family [AOR: 0.36:95% CI, 0.31, 0.99] were 64% less likely to have good menstrual hygiene practices than students who have permanent pocket money from family | Grade level, types of school, place of residence, age at menarche, family monthly income, father's educational status, mother's educational status, heard about menstruation before menarche, know sanitary pad, and knowledge about menstrual hygiene practice |
| Hasan JH, 2021 [29] | Cross-sectional | 1.96[1.32,2.90] | 2.08[1.27, 3.40] | A | Schoolgirls who earned permanent pocket money from parents or relatives were two times 2.08 times higher odds of practicing good menstrual hygiene than those who have not earned permanent pocket money from parents or relatives [AOR: 2.08, 95%CI: 1.27, 3.40] | Grade level, religion, mother's educational status, knowledge level, residence, ethnicity, age at menarche, and fathers' education |
| Kedir T, 2017 [30] | Cross-sectional | 0.52[0.38, 0.72] | 0.62[0.39, 0.97] | B | Adolescent girls who did not receive pocket money were 38% less likely to behave in good menstrual hygiene practice [AOR = 0.62, 95%CI:0.39, 0.97] than adolescent girls who receive permanent pocket money | Age of respondents, residence, place for drying menstrual absorbent material in the household, going to school during menstruation, and taking advice on menstruation |
| Biruk E et al., 2018 [31] | Cross-sectional | 2.17[1.57–3.01] | 1.11[0.67,1.81] | A | Not significant | School type, age of the respondents, wealth index, grade, religion, living with, Mothers’ educational status, fathers’ educational status, fathers’ occupation, Mothers’ occupation, and age at first menarche |
NA Not Applicable; Reference category “A = NO” indicates: girls who did not receive permanent pocket money from their parents and “B = YES” indicates those girls who receive pocket money; *Crude Odds Ratio [COR] was calculated from a two-by-two table considering girls who did not receive permanent pocket money from their parents as a reference category to estimate the pooled COR [as these studies used different reference category from the rest of the included studies]. Accordingly, the COR [95%CI] for the authors Felleke AA et al., 2021 and Kedir T, 2017 were [COR: 2.54, 95%CI: 1.56,4.11] and [COR:1.91, 95%CI: 1.38, 2.64], respectively
Risk of bias within studies
When it came to the risk of bias in the studies that were included, the majority of them [99 percent] had a low risk of bias (Additional file 3).
Meta-analysis
Association between earning pocket money and good menstrual hygiene management
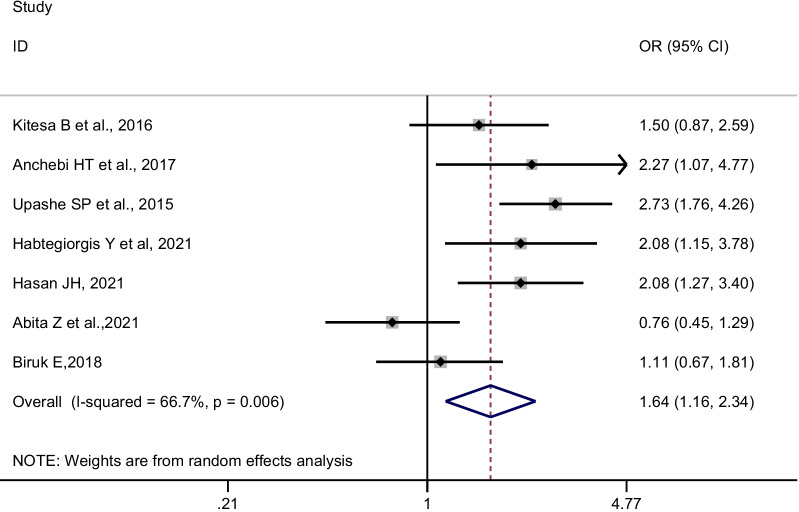
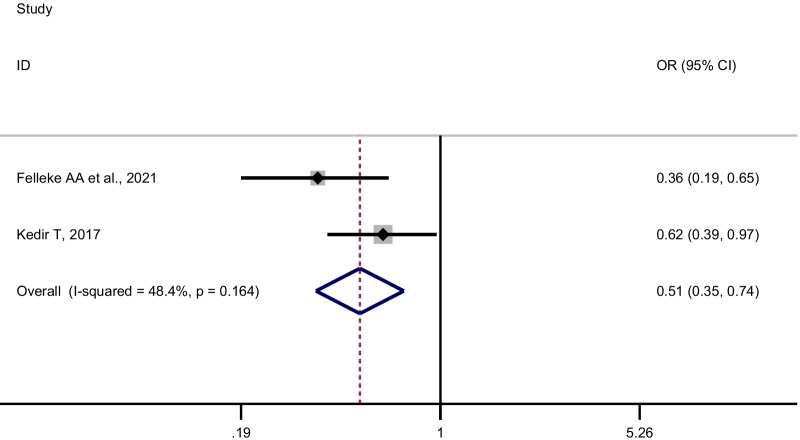
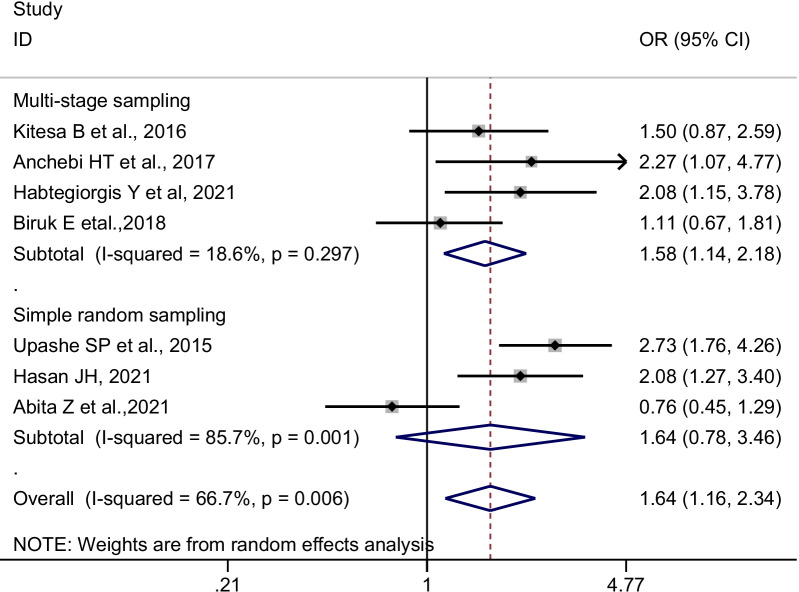
Adolescent girls who received pocket money from their parents or relatives had significantly higher odds of having good menstrual hygiene management than their counterparts (pooled OR [POR] = 1.64, 95%CI: 1.16–2.34, n = 7). We used a random-effects meta-analysis model to estimate POR because the included studies had moderate heterogeneity (I2 = 66.7%, p-value = 0.006) (Fig. 2). Since two studies [28, 30] used different reference categories, we pooled the confounder adjusted odds ratios separately (Table 2). Likewise, the odds of having good menstrual hygiene management were lower among adolescent girls who did not receive pocket money compared to their counterparts (POR = 0.51, 95% CI: 0.35–0.74; I2:48.4%, n = 2) (Fig. 3).
Fig. 2.
Forest plot of the individual and pooled odds ratios (POR) of the association between earning pocket money and good menstrual hygiene management, 2014–2021
Fig. 3.
Forest plot of two studies and pooled odds ratios (POR) of the association between earning pocket money and good menstrual hygiene management, 2014–2021
Additional analysis
Subgroup analysis
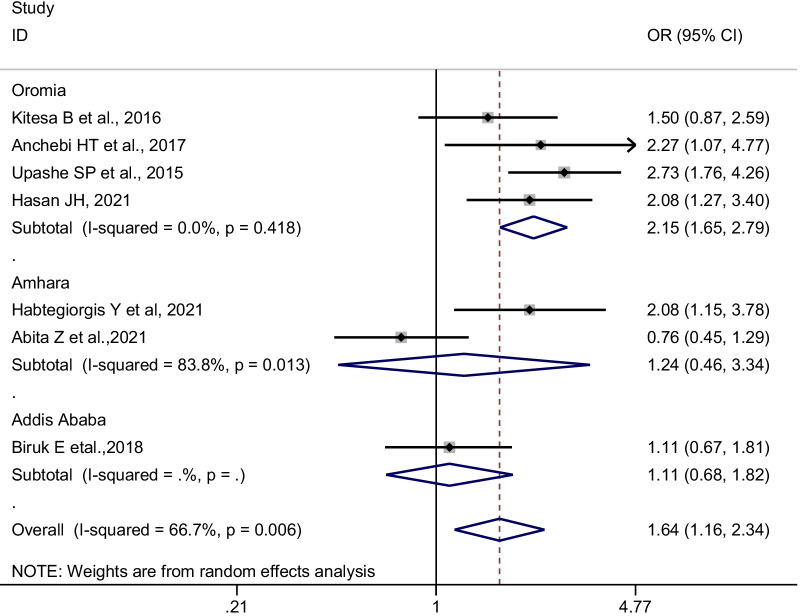
Subgroup analysis was conducted by geographical regions, sampling methods, method of data collection, sample size, publication year, and confounders adjusted in a multivariate model in primary studies. Accordingly, in the random-effects model, studies conducted in the Oromia region, studies used multistage sampling, and the interviewer-administered data collection technique was found to reveal a significant pooled odds ratio (Figs. 4 and 5). The present meta-analysis also revealed different effect sizes with different sample sizes, and the higher the sample size the more precise the effect size (Table 3).
Fig. 4.
Subgroup pooled odds ratios (POR) of the association between earning pocket money and good menstrual hygiene management among adolescent girls in Ethiopia, by region, 2014–2021
Fig. 5.
Subgroup pooled odds ratios (POR) of the association between earning pocket money and good menstrual hygiene management among adolescent girls in Ethiopia, by sampling technique, 2014–2021
Table 3.
Subgroup analysis of the association between earning pocket money is significantly associated with good menstrual hygiene management
| Variables | Sub-group | Number of studies | Pooled OR (95%CI) | Heterogeneity tests across the studies | |
|---|---|---|---|---|---|
| I2 (%) | p-value | ||||
| Region | Oromia | 4 | 2.14 [1.64–2.79] | 0.00 | 0.418 |
| Amhara | 2 | 1.24 [0.46–3.34] | 83.8 | 0.013 | |
| Addis Ababa | 1 | 1.11 [0.67–1.81] | - | - | |
| Sampling methods | Multistage sampling | 4 | 1.58 [1.14–2.18] | 18.6 | 0.297 |
| Simple random sampling | 3 | 1.64 [0.78–3.46] | 85.7 | 0.001 | |
| Method of data collection | Self-administered | 5 | 1.60 [0.98–2.62] | 76.9 | 0.002 |
| Interviewer administered | 2 | 1.74[1.16–2.60] | 0.00 | 0.427 | |
| Sample size | ≤ 500 | 4 | 1.49 [0.91–2.45] | 67.5 | 0.026 |
| > 500 | 3 | 1.85 [1.06–3.23] | 72.1 | 0.028 | |
| Publication year | 2015–2020 | 4 | 1.78 [1.15–2.76] | 61.8 | 0.049 |
| > 2020 | 3 | 1.48 [0.76–2.89] | 78.4 | 0.010 | |
| Confounders adjusted in a multivariable model | |||||
| Knowledge towards menstruation | Adjusted | 2 | 2.08 [1.42–3.04] | 0.00 | 1.00 |
| Not adjusted | 5 | 1.50 [0.92–2.42] | 75.1 | 0.003 | |
| Age | Adjusted | 3 | 1.65 [1.03–2.65] | 45.4 | 0.160 |
| Not adjusted | 4 | 1.61 [0.94–2.78] | 78.9 | 0.003 | |
| Age at menarche | Adjusted | 2 | 1.52 [0.82–2.81] | 67.7 | 0.078 |
| Not adjusted | 5 | 1.70 [1.06–2.74] | 72.6 | 0.006 | |
| Grade level | Adjusted | 2 | 2.08[1.42–3.04] | 0.00 | 1.00 |
| Not adjusted | 5 | 1.50 [0.92–2.42] | 75.1 | 0.003 | |
Meta-regression
A univariate meta-regression model with publication year and sample size as covariates was run to identify potential sources of heterogeneity across primary studies, but none of these variables were found to be statistically significant sources of heterogeneity (Table 4).
Table 4.
Meta-regression of factors associated with the heterogeneity of the studies included in estimating the pooled effect of earning pocket money on good menstrual hygiene management [based on univariate meta-regression]
| Variables | Coef | p-value |
|---|---|---|
| Sample size | 0.0006037 | 0.627 |
| Year of publication | − 0.0666867 | 0.408 |
Publication bias
Using funnel plots, potential publication bias was visualized. The publication bias was also assessed using Egger's tests. The absence of publication biases was represented by an asymmetrical large inverted funnel (Fig. 6). The statistics from Egger's test indicated that there was no statistically significant publication bias, with p-values of 0.813.
Fig. 6.
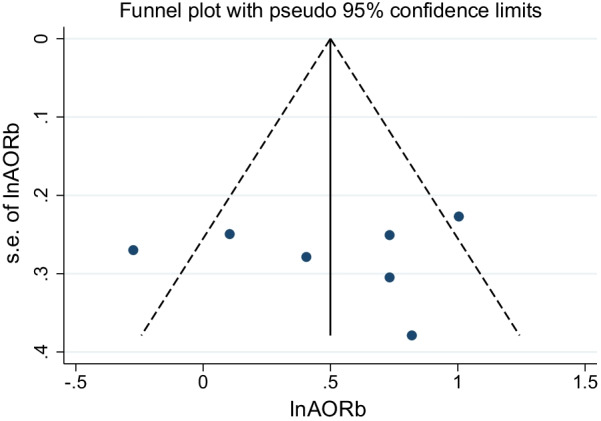
Funnel plot for the meta-analysis of the association between earning pocket money and good menstrual hygiene management, 2014–2021
Sensitivity analyses
In this review, the sensitivity of each study was checked to identify smaller or larger pooled estimates of the association between earning pocket money and good menstrual hygiene management, which could affect the pooled result by giving wider confidence intervals and variance instability. Based on the result of the random effect model, the sensitivity analyses suggested that the pooled odds ratio or the heterogeneity were somewhat modified after removing a study by Abita Z et al.,2021 [26] (Table 5).
Table 5.
Sensitivity analysis for the pooled estimates of the association between earning pocket money and good menstrual hygiene management
| Author’s name, year of publication | POR | 95%CI | I2 [%] | p-value |
|---|---|---|---|---|
| Kitesa B et al., 2016 [10] | 1.67 | 1.10–2.53 | 72.0 | 0.003 |
| Habtegiorgis Y et al., 2021 [23] | 1.58 | 1.06–2.37 | 71.2 | 0.004 |
| Upashe SP et al., 2015 [25] | 1.48 | 1.05–2.10 | 57.5 | 0.038 |
| Abita Z et al.,2021 [26] | 1.88 | 1.41–2.49 | 39.3 | 0.144 |
| Anchebi HT et al., 2017 [27] | 1.58 | 1.07–2.33 | 71.0 | 0.004 |
| Hasan JH, 2021 [29] | 1.58 | 1.04–2.38 | 70.6 | 0.005 |
| Biruk E et al., 2018 [31] | 1.76 | 1.20–2.60 | 66.8 | 0.010 |
Discussion
Menstrual hygiene practice is essential to adolescent schoolgirl empowerment. Improper menstrual hygiene puts girls at risk of infection and impacts students' academic confidence and self-esteem [6, 7, 15]. Menstrual hygiene management is still poorly discussed in Ethiopia, as it is in many developing countries. There has been an increase in evidence on the association between earning pocket money and good menstrual hygiene management [10, 23, 25, 26]. For the first time in Ethiopia, this study tries to assess the association. This meta-analysis found a significant positive relationship between receiving pocket money from parents or relatives and maintaining good menstrual hygiene among adolescent girls.
In this review, adolescent girls who earned pocket money from their families were nearly two times more likely to have good menstrual hygiene than those who don't earn permanent pocket money from their families. This study supported prior studies that show a link between good menstrual hygiene and obtaining pocket money from family members [10, 27, 35]. This might be because girls who earn money from their parents can easily purchase sanitary products for menstrual hygiene, which may lead girls to have good menstrual hygiene [16]. According to prior studies, girls from families with higher monthly household expenditures or belonging to the richest wealth quintile were also more likely to use sanitary napkins and have good menstrual hygiene management than their counterparts [7, 31, 36].
This study found pocket money to be a crucial component in addressing hygienic management of menstruation among schoolgirls. In this regard, recent literature has recognized pocket money as an important intervention to address girls' menstrual hygiene needs [37], as well as access to quality hygiene supplies to promote good menstrual hygiene [38].
Studies suggest that menstruation contributes to school absenteeism, possibly extending to school dropout. Lack of menstrual hygiene resources was reported to lead directly to drop out or school absence [18, 37, 39]. According to a review conducted in India, females miss school due to the fear and embarrassment of blood and body odor leaking [16]. In fact, poverty was a constant underlying attribute in the stories of the girls either directly or indirectly responsible for the higher proportion of absenteeism or dropout. A review discovered that limited financial resources to purchase supplies continue to be a barrier to improving menstrual hygiene management in many resource-limited settings [40]. As a result, poor menstrual hygiene remains a major impediment to girls' education and their self-esteem and personal development [41].
Our review demonstrated that adolescent girls who did not get pocket money were less likely than their peers to adopt proper menstrual hygiene management. According to studies conducted in Kenya [37] and Tanzania [42], girls frequently mention the need for sanitary pads, but their parents' funds rarely allow them to buy the high-quality or sufficient number of pads required, and girls' financial dependence on sanitary materials impacts their MHM, school attendance, and sexual behaviors. We believe that earning permanent pocket money from parents may, in turn, enhance girls' menstrual hygiene, which may lead to increased school attendance. Eliminating menstrual needs as a burden for schoolgirls will improve their dignity, school involvement, and possibly their menstrual hygiene management. Moreover, access to hygienic menstrual management methods for adolescent girls is critical from both public health and adolescent girls' perspectives. One strategy for this is to give schoolgirls pocket money to spend on their menstrual hygiene needs as needed.
Limitations
Our study has several limitations. First, all included studies were cross-sectional studies, so causality cannot be inferred. Second, our study could lack representativeness at a country level as we did not find a study from some regions of the country. Third, the included studies were not free of social desirability bias. Fourth, there was average heterogeneity between included studies as indicated by the I2 statistic. This might be explained by the methodological variation and/or difference in the study setting. Hence, we performed sub-group analysis, sensitivity analysis, and meta-regression to explore the variations within the studies. Finally, we did not examine the link between the amount of pocket money and the menstrual hygiene of girls. However, we believe that the amount of pocket money a girl has may affect her menstrual hygiene, and further research is necessary to address this topic in depth.
Conclusions
The evidence suggests that adolescent girls who earned pocket money were more likely to practice good menstrual hygiene management. Progress toward improving schoolgirl menstrual hygiene will necessitate consideration of this factor to enhance menstrual hygiene practice.
Supplementary Information
Additional file 2: Examples of searching strategy.
Additional file 3: Risk of bias for included studies.
Acknowledgements
We would like to acknowledge all public health department staff of Madda Walabu University for their cooperation and support.
Author contributions
BS: Conception of the research protocol, study design, searching, literature review, data extraction, quality assessment, data extraction and analysis, interpretation, and drafting of the manuscript. DA: searching, data extraction, quality assessment, and reviewing the manuscript. AK, GB, YT, DZ, DW, FD, TA, DB, FN and KEA: Data analysis, reviewing, and editing the manuscript. All authors read and approved the manuscript.
Funding
No organization funded this research.
Availability of supporting data
All data generated or analyzed during this study are included in this published article and its Additional files (Additional file 4).
Declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sarah Bumbarger. How menstrual hygiene management impacts girls in the ethiopian lowlands. Weblog. https://dt-global.com/company/blog/may-28th-2021/menstruation-health-ethiopia. Accessed 21 Sep 2021. [Online].
- 2.Sahiledengle B, Atlaw D, Kumie A, Tekalegn Y, Woldeyohannes D, Agho KE. Menstrual hygiene practice among adolescent girls in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2022;17(1):e0262295. doi: 10.1371/journal.pone.0262295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guidance on Menstrual Health and Hygiene. United Nations Children’s Fund [UNICEF]. New York, NY, USA. 2019. https://www.unicef.org/media/91341/file/UNICEF-Guidance-menstrual-health-hygiene-2019.pdf. Accessed 21 Sep 2021.
- 4.WHO/UNICEF. Consultation on draft long list of goal, target and indicator options for future global monitoring of water, sanitation and hygiene. 2012. https://washdata.org/sites/default/files/documents/reports/2017-06/JMP-2012-post2015-consultation.pdf. Accessed 21 Sep 2021.
- 5.World Bank. Menstrual hygiene management enables women and girls to reach their full potential NW Washington, USA. https://www.worldbank.org/en/news/feature/2018/05/25/menstrual-hygiene-management. Accessed 21 Sep 2021.
- 6.Das P, Baker KK, Dutta A, Swain T, Sahoo S, Das BS, et al. Menstrual hygiene practices, WASH access and the risk of urogenital infection in women from Odisha, India. PLoS ONE. 2015;10(6):e0130777. doi: 10.1371/journal.pone.0130777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tegegne TK, Sisay MM. Menstrual hygiene management and school absenteeism among female adolescent students in Northeast Ethiopia. BMC Public Health. 2014;14:1118. doi: 10.1186/1471-2458-14-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohammed S, Larsen-Reindorf RE, Awal I. Menstrual hygiene management and school absenteeism among adolescents in ghana: results from a school-based cross-sectional study in a rural community. Int J Reprod Med. 2020;2020:1–9. doi: 10.1155/2020/6872491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trinies V, Caruso B, Sogoré A, Toubkiss J, Freeman M. Uncovering the challenges to menstrual hygiene management in schools in Mali. Waterlines. 2015;34(1):31–40. doi: 10.3362/1756-3488.2015.004. [DOI] [Google Scholar]
- 10.Kitesa B. Assessment of knowledge and practice of adolescent in-school girls towards menstrual hygiene management and determinin, 2016. Int J Immunol. 2016;4(6):52. doi: 10.11648/j.iji.20160406.12. [DOI] [Google Scholar]
- 11.Torondel B, Sinha S, Mohanty JR, Swain T, Sahoo P, Panda B, et al. Association between unhygienic menstrual management practices and prevalence of lower reproductive tract infections: a hospital-based cross-sectional study in Odisha. India BMC Infect Dis. 2018;18:473. doi: 10.1186/s12879-018-3384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.UNICEF . Sharing simple facts: useful information about menstrual health and hygiene. New Delhi: UNICEF India; 2008. [Google Scholar]
- 13.Birhane AD, Serbessa MK, Degfie TT. Menstrual hygiene management: a study of adolescent schoolgirls in sebeta town, oromia region. Ethiopia Glob Drugs Ther. 2020;5:1–8. [Google Scholar]
- 14.Tamiru S, Mamo K, Acidria P, Mushi R, Ali CS, Ndebele L. Towards a sustainable solution for school menstrual hygiene management: cases of Ethiopia, Uganda, South-Sudan, Tanzania, and Zimbabwe. Waterlines. 2015;34(1):92–102. doi: 10.3362/1756-3488.2015.009. [DOI] [Google Scholar]
- 15.Davis J, Macintyre A, Odagiri M, Suriastini W, Cordova A, Huggett C, et al. Menstrual hygiene management and school absenteeism among adolescent students in Indonesia: evidence from a cross-sectional school-based survey. Trop Med Int Health. 2018;23(12):1350–1363. doi: 10.1111/tmi.13159. [DOI] [PubMed] [Google Scholar]
- 16.van Eijk AM, Sivakami M, Thakkar MB, Bauman A, Laserson KF, Coates S, et al. Menstrual hygiene management among adolescent girls in India: a systematic review and meta-analysis. BMJ Open. 2016;6(3):e010290. doi: 10.1136/bmjopen-2015-010290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miiro G, Rutakumwa R, Nakiyingi-Miiro J, Nakuya K, Musoke S, Namakula J, et al. Menstrual health and school absenteeism among adolescent girls in Uganda [MENISCUS]: a feasibility study. BMC Womens Health. 2018;18:4. doi: 10.1186/s12905-017-0502-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mason L, Nyothach E, Alexander K, Odhiambo FO, Eleveld A, Vulule J, et al. ‘We keep it secret so no one should know’ – a qualitative study to explore young schoolgirls attitudes and experiences with menstruation in Rural Western Kenya. PLoS ONE. 2013;8(11):e79132. doi: 10.1371/journal.pone.0079132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips-Howard PA, Otieno G, Burmen B, Otieno F, Odongo F, Odour C, et al. Menstrual needs and associations with sexual and reproductive risks in rural Kenyan females: a cross-sectional behavioral survey linked with HIV prevalence. J Women's Health. 2015;24(10):801–811. doi: 10.1089/jwh.2014.5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nobelius AM, Kalina B, Pool R, Whitworth J, Chesters J, Power R. “You still need to give her a token of appreciation”: the meaning of the exchange of money in the sexual relationships of out-of-school adolescents in rural Southwest Uganda. J Sex Res. 2010;47(5):490–503. doi: 10.1080/00224499.2010.494776. [DOI] [PubMed] [Google Scholar]
- 21.Forde S. Playing by their rules: coastal teenage girls in kenya on life, love and football createspace. 2009. p. 250
- 22.Phillips-Howard PA, Nyothach E, Ter Kuile FO. Menstrual cups and sanitary pads to reduce school attrition, and sexually transmitted and reproductive tract infections: a cluster randomised controlled feasibility study in rural Western Kenya. BMJ Open. 2016;6(11):e013229. doi: 10.1136/bmjopen-2016-013229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Habtegiorgis Y, Sisay T, Kloos H, Malede A, Yalew M, Arefaynie M, et al. Menstrual hygiene practices among high school girls in urban areas in Northeastern Ethiopia: a neglected issue in water, sanitation, and hygiene research. PLoS ONE. 2021;16(6):e0248825. doi: 10.1371/journal.pone.0248825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yalew M, Adane B, Arefaynie M, Kefale B, Damtie Y, Mitiku K, et al. Menstrual hygiene practice among female adolescents and its association with knowledge in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2021;16(8):e0254092. doi: 10.1371/journal.pone.0254092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Upashe SP, Tekelab T, Mekonnen J. Assessment of knowledge and practice of menstrual hygiene among high school girls in Western Ethiopia. BMC Womens Health. 2015;15:84. doi: 10.1186/s12905-015-0245-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abita Z, Ali R, Admassu B, Abita Z, Ali R, Admassu B. Menstrual hygiene management practice and associated factors among secondary school girls in finot selam town, northwest Ethiopia, 2019. Int J Sex Reprod Health Care. 2021;4(1):053–61. [Google Scholar]
- 27.Anchebi H, Shiferaw B, Fite R, Abeya S. Practice of menstrual hygiene and associated factors among female high school students in adama town. J Women’s Health Care. 2017;6(3):1–8. doi: 10.4172/2167-0420.1000370. [DOI] [Google Scholar]
- 28.Felleke AA, Gerada AA, Abibeker MA. Assessment of menstrual hygiene practice and associated factor among high school female students in Harar Eastern Ethiopia 2019. medRxiv. 2021. 10.1101/2020.03.16.20036913
- 29.Hasan JH. Practice of menstrual hygiene management and associated factors among secondary school girls in Chelenko town, East Hararghe zone, Eastern Ethiopia. MPH Thesis. March, 2021. Haramaya University. Harare. Ethiopia.
- 30.Kedir T. Knowledge and practice of menstrual hygiene and associated factors among adolescent girls in Weliso District,Southwest Shoa zone, Oromia, Ethiopia. MPH Thesis. April, 2021. Madda Walabu University. Bale-Goba. Ethiopia.
- 31.Biruk E, Tefera W, Tadesse N, Sisay A. Assessment of menstrual hygiene management and its determinants among adolescent girls: a cross-sectional study in-school adolescent girls in Addis Ababa, Ethiopia. BioRxiv. 2018. 10.1101/450007v2
- 32.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.JBI. Checklist for Analytical Cross-Sectional Studies. JBI critical appraisal tools for use in JBI systematic reviews. 2017. http://joannabriggs.org/research/critical-appraisal-tools.htmlwww.joannabriggs. [Internet]
- 34.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 35.Omidvar S, Begum K. Factors influencing hygienic practices during menses among girls from south India - a cross-sectional study. Int J Coll Res Inter Med Pub Hlth. 2010;2(12):411–423. [Google Scholar]
- 36.Chauhan S, Kumar P, Marbaniang SP, Srivastava S, Patel R, Dhillon P. Examining the predictors of use of sanitary napkins among adolescent girls: a multi-level approach. PLoS ONE. 2012;16(4):e0250788. doi: 10.1371/journal.pone.0250788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oruko K, Nyothach E, Zielinski-Gutierrez E, Mason L, Alexander K, Vulule J, et al. “He is the one who is providing you with everything so whatever he says is what you do”: a qualitative study on factors affecting secondary schoolgirls’ dropout in Rural Western Kenya. PLoS ONE. 2015;10(12):e0144321. doi: 10.1371/journal.pone.0144321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gopalan M. There are 3 barriers blocking good menstrual hygiene for all women. Here’s how we overcome them. World Econ Forum 2019. https://www.weforum.org/agenda/2019/11/menstruation-in-different-cultures-period-taboos/
- 39.Mason L, Laserson K, Oruko K, Nyothach E, Alexander K, Odhiambo F, et al. Adolescent schoolgirls’ experiences of menstrual cups and pads in rural western Kenya: a qualitative study. Waterlines. 2015;34:15–30. doi: 10.3362/1756-3488.2015.003. [DOI] [Google Scholar]
- 40.Kuhlmann AS, Henry K, Wall LL. Menstrual Hygiene management in resource-poor countries. Obstet Gynecol Surv. 2017;72(6):356–376. doi: 10.1097/OGX.0000000000000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chandra-Mouli V, Patel SV. Mapping the knowledge and understanding of menarche, menstrual hygiene and menstrual health among adolescent girls in low- and middle-income countries. Reprod Health. 2017;14(1):30. doi: 10.1186/s12978-017-0293-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maganja RK, Maman S, Groves A, Mbwambo JK. Skinning the goat and pulling the load: transactional sex among youth in Dar es Salaam. Tanzania AIDS Care. 2007;19(8):974–981. doi: 10.1080/09540120701294286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2: Examples of searching strategy.
Additional file 3: Risk of bias for included studies.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its Additional files (Additional file 4).