Abstract
Background
A randomized controlled study was conducted on the effects of laughter yoga in reducing the perceived stress and burnout levels in nurses during the pandemic and in increasing their life satisfaction.
Materials and methods
The study was conducted with 101 (51 in the experimental group, and 50 in the control group) nurses providing care for patients with COVID-19. A total of eight sessions of laughter yoga were applied to the nurses in the experimental group for four weeks, twice a week. The Introductory Information Form, Perceived Stress Scale, Maslach Burnout Inventory, and Life Satisfaction Scale were used during data collection.
Results
The difference between the pre- and posttest Perceived Stress Scale, Maslach Burnout Inventory, and Life Satisfaction Scale score averages of the nurses in the experimental group were found to be statistically significant (p < 0.05), whereas the difference between the pre- and posttest score averages of the nurses in the control group was not significant (p > 0.05).
Conclusion
Laughter yoga is an effective method to reduce perceived stress and burnout while also increasing life satisfaction.
Clinicaltrials.gov id
Keywords: Pandemic, Nurse, Stress, Burnout, Life satisfaction, Laughter yoga
1. Introduction
The new coronavirus disease (COVID-19), was first seen in Wuhan, China in 2019 [1,2]. As the virus spread to across the world in a short period of time, a pandemic was declared by the World Health Organization (WHO) [3]. In the fight against this disease, which inherently spreads very quickly and has high mortality rates, the healthcare industry has assumed significant responsibilities [4]. Since the beginning of the pandemic, healthcare providers have been among the most challenged institutions. Across the world, nurses constitute the majority of the healthcare workforce during this epidemic [5]. Nurses who have played an active role during the pandemic experience anxiety about being infected and transmitting the disease to their family, friends, and colleagues because of direct contact with COVID-19 patients [6,7]. Moreover, the suffering and death of patients increases the fear and anxiety of nurses [6]. The care of critical patients with COVID-19, increased workload, high risk of infection, uncertainty, and stigma, use of personal protective equipment, high number of patients, and ethical dilemmas cause psychological pressure on nurses [[8], [9], [10]]. Previous research has shown that pandemics increase the stress perceived by nurses trying to cope with intense emotional, physical, and cognitive demands [[11], [12], [13]]. In studies conducted during the COVID-19 pandemic, it was reported that nurses especially experienced physical symptoms such as depression, anxiety, insomnia, stress, fatigue, and burnout [[14], [15], [16], [17], [18]]. In Iran, half of the nurses working in the corona services of eight university hospitals were found to have burnout syndrome [19]. Janeway's study reported that the prevalence of burnout in nurses ranged from 35% to 45% [20]. Burnout in nurses manifests in physiological and emotional areas and occurs as a result of not being able to cope with the current situation, which is in line with the increase in perceived stress [21]. Prolonged stress and burnout cause nurses to feel tired, exhausted, and inadequate, hence reducing their performance [22,23]. In addition, this can lead to weakened decision making and increased medical errors, which adversely affect the quality of patient care [18,24,25].
It is critical to support the health team with evidence-based practices aimed at reducing stresses and fears [5], increasing the satisfaction and performance of nurses, who are one of the higher risk groups of contracting COVID-19 [18]. Mind–body-based complementary practices, such as yoga, meditation, breathing, and relaxation exercises, could be used to improve the level of well-being and facilitate adaptation to the changes experienced during this period [26,27]. Among these practices, laughter yoga is a new, cost-effective, and effective method [28,29]. As a nonpharmacological practice, laughter yoga is a set of exercises that combines unprovoked laughter with yoga breathing techniques (Pranayama). Stretching-relaxation techniques include laughter and deep-breathing exercises [20,30]. It has been reported that laughter yoga physiologically increases breathing in the body; relaxes muscles; strengthens mental function by reducing the level of stress hormones; reduces burnout, depression, and anxiety levels; positively affects quality of life; improves sleep quality; and provides psychological well-being by increasing interpersonal relationships and social interaction [28,31,32]. In addition, it has been emphasized that laughter yoga stimulates the immune system, increases endorphin levels, reduces the production of stress hormones, such as cortisol and epinephrine, accelerates the circulatory system, and has vasodilation effects in the veins [29,31,32].
In general during the pandemic especially, nurses need to feel good—both mentally and physically—to work more efficiently. Coping with stress related to the COVID-19 pandemic and creating a cheerful environment to laugh during a stressful period is perhaps more important than ever. Laughter yoga can improve mood, reduce stress, improve life saturation and quality of life, and reduce the negative emotions associated with current circumstances [31]. Looking at the literature, a limited number of international studies have evaluated the effect of laughter yoga on nurses [31,33], and no studies were found in Turkey on this subject. Thus, the present study aims to investigate the effect of laughter yoga on the perceived stress, burnout levels, and life satisfaction in nurses during the pandemic. For this purpose, the following hypotheses were tested:
H1
Laughter yoga reduces the stress perceived by nurses during the pandemic.
H2
Laughter yoga reduces nurses' burnout during the pandemic.
H3
Laughter yoga increases the life satisfaction of nurses during the pandemic.
2. Methods
2.1. Study design
This experimental randomized controlled study was conducted with nurses working in the COVID-19 clinics and providing care for COVID-19 patients at hospital in a city, which is located in the northeastern part of Turkey, between June 2021 and August 2021. The study was carried out with one experimental group (EG) and one control group (CG). This study was registered at the Clinical.Trials.gov Protocol Registration and Results System (Protocol ID Number NCT05317091)
2.2. Setting and samples
The study sample consisted of 120 nurses who were accessed by the snowball method, who met the criteria for inclusion in the study, and who volunteered to participate in the research. Nurses who did not have diagnosed psychiatric diseases; who provided care for patients with COVID-19; who had not had abdominal surgery in the last three months; who did not have uncontrollable hypertension, glaucoma, hernia, or epilepsy; and who had not done laughter yoga before were included. Nurses who left the study at any stage; nurses who did not participate regularly in the yoga sessions; nurses who used another relaxation method during this period; nurses who took antidepressants, were excluded from the research.
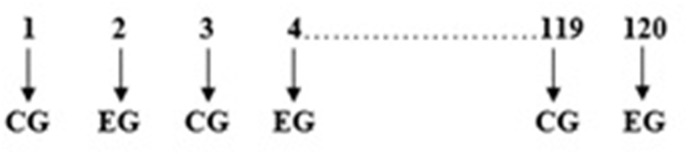
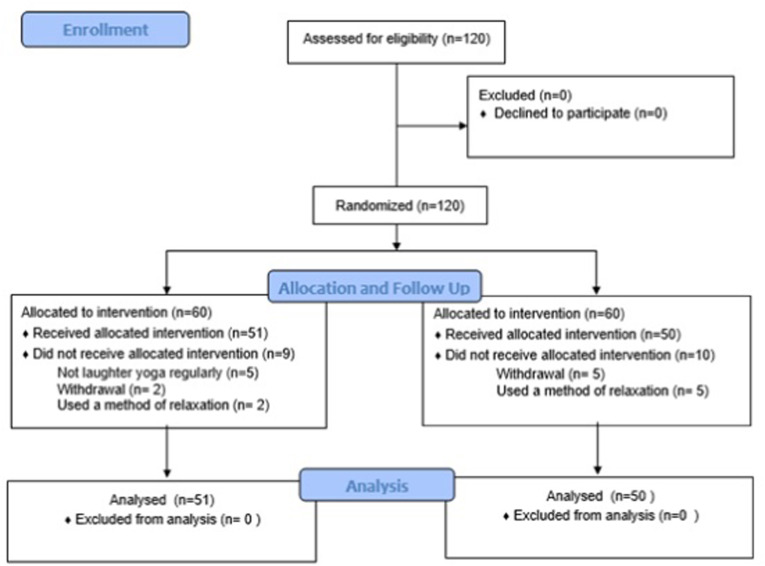
All nurses who met the inclusion criteria were randomly listed on a computer using the https://www.randomizer.org/ website. The participants were selected randomly; the odds were assigned to the CG, and the evens were assigned to the EG. The randomization scheme is presented in Fig. 1 . During the study, nine people in the EG (five people did not attend regular sessions, two people voluntarily left, two people used a different relaxation method), and 10 people in the CG (five people left voluntarily, five people used a relaxation method) were excluded from the research. The algorithm in the CONSORT flowchart (Fig. 2 ) shows those who left the study. Finally, the study was completed with 101 nurses, including 51 in the EG and 50 in the CG.
Fig. 1.
Randomization scheme.
Fig. 2.
CONSORT flow diagram.
In the current study, the power of the study sample was calculated using the “G Power-3.1.9.2” program with a margin of error of 0.05 after data collection. In the study, an independent samples t-test was used to determine whether the perceived stress levels of the nurses in the posttest differed between the EG (nurses who had laughter yoga) and CG. Accordingly, the effect size of the study was calculated as 2.07, the alpha value was 0.05, and the power was 0.99 (51 in the EG and 50 in the CG).
2.3. Data collection instruments
The Introductory Information Form, Perceived Stress Scale, Maslach Burnout Inventory, and Life Satisfaction Scale were used during data collection.
Introductory Information Form: This form was prepared by the researchers and contains a total of nine items on age, gender, education level, marital status, working year, frequent mode of shift, COVID-19 status, vaccination status, and previous information about laughter yoga.
Perceived Stress Scale (PSS): A Turkish reliability and validity study of the scale, which was developed by Cohen et al. (1983) [34] to reveal the perceived stress levels of individuals regarding certain events that they experienced was carried out by Eskin et al. (2013) [35]. The 5-point Likert-type scale consists of 14 items. Seven items containing positive statements are reverse scored on the scale. The score ranges from 0 to 56, with a high score indicating a high state of stress. The internal consistency coefficient of the scale is 0.84 [35]. In the current study, Cronbach's alpha internal consistency coefficient was 0.75.
Maslach Burnout Inventory (MBI): The scale has been developed by Maslach and Jackson [36]. Its Turkish validity and reliability study was conducted by Ergin [37]. The 5-point Likert-type scale consists of 22 items and three subscales. The subscales are emotional exhaustion, depersonalization, and personal achievement. Positive statements in the personal success subscale are reverse coded. Higher emotional exhaustion and depersonalization subscale score averages and lower personal achievement score averages indicate higher burnout. The lowest and highest scores on the scale are 0 and 88, respectively. The Cronbach's alpha values of the scale are 0.83 for emotional exhaustion, 0.65 for depersonalization, and 0.72 for personal achievement [37]. In the current study, Cronbach's alpha values of the subscales were 0.92 for the emotional exhaustion subscale, 0.80 for the depersonalization subscale, and 0.72 for the personal accomplishment subscale.
Life Satisfaction Scale: The scale was developed by Diener et al. [38] and adapted to Turkish by Dağlı et al. [39]. There are five items on the scale, and each item is organized according to a 7-point system. The scale is scored in a range from 5 to 35. An increase in the score indicates increased life satisfaction. The Cronbach's alpha value of the scale is 0.88 [39]. In the current study, Cronbach's alpha coefficient was found to be 0.87.
2.4. Data collection
The pretest data: Nurses who met the research inclusion criteria were contacted through social media tools such as WhatsApp, Instagram, and Facebook using the snowball method; nurses who volunteered to participate were informed about the research, and their contact numbers were obtained. Because of the pandemic, data were collected online. The online questionnaire link containing the measurement tools to be used for collecting the pretest data was shared with the nurses via the WhatsApp application, and then, the nurses were asked to respond to the questions on the Introductory Information Form, Perceived Stress Scale, MBI, and the Life Satisfaction Scale. The nurses were informed that they would be asked to fill in the relevant questionnaire again after one month and were asked to write a word that would be easy to remember to the nickname area included in the online questionnaire.
The posttest data: One month (four weeks) after collecting the pretest data, the online survey link with measurement tools to be used for the collection of the posttest data was shared with nurses via the WhatsApp application, and they were allowed to fill out the Perceived Stress Scale, MBI, and Life Satisfaction Scale included in the link. As previously reported, they were asked to type the word they had written earlier in the nickname item included in the questionnaire. According to the word written in the nickname area, the pretest and posttest data were matched in the online survey.
2.5. Intervention
In the current study, a total of eight sessions of laughter yoga were performed with nurses in the EG for four weeks, twice a week as an intervention. Because of the COVID-19 pandemic, laughter yoga sessions were held on the web through the Zoom program. Before starting laughter yoga, a WhatsApp group was established to provide faster and easier communication with the nurses in the EG, and communication about the sessions was handled in this group. Before starting the application, the Zoom program was downloaded to the phone or computer of the nurses in the EG.
The more participants there are in laughter yoga, the greater the spread of laughter, and the easier it is for participants to laugh. Therefore, it is recommended to make laughter yoga sessions in groups, and each group should consist of at least five people to ensure group dynamics [40]. Because nurses work in shifts, the most appropriate time intervals that they can connect to the online sessions were discussed, and three groups of approximately 20 people were formed. The sessions were planned according to the days and hours that the nurses could attend. The sessions were held between 12:00 and 13:00 on Mondays and Thursdays for the first group, between 17:00 and 18:00 on Tuesdays and Fridays for the second group, and between 20:00 and 21:00 on Wednesdays and Saturdays for the third group. The nurses were continuously contacted (using WhatsApp, and phone) to attend the sessions regularly and avoid interruptions in the sessions. No experiments were performed on the CG during the study time period. After the research, however, four weeks of laughter yoga was provided to those nurses in the control group who wanted.
2.6. Application of laughter yoga
Laughter yoga mainly includes stretching-relaxation techniques, laughter, and deep-breathing exercises. Laughter yoga sessions begin with light warm-up techniques consisting of stretching and stretching movements, songs, clapping, and body movements. These techniques aim at breaking down all kinds of barriers to laughter and developing feelings of childish play. Breathing exercises prepare the lungs for laughing and are combined with a set of laughing exercises that follow [30].
A laughter yoga session is about 40 min long and consists of four parts. These sections are deep-breathing exercises (5 min), warm-up exercises (10 min), childish games (10 min), and laughter exercises (15 min). In each laughter yoga session, the first three parts are the same, and the laughter exercises in the fourth part vary. The parts of a laughter yoga session are described below.
Section 1: Deep-breathing exercises: A deep breath is taken as far as possible by raising the arms up to the sky. Breathing is held for four to 5 s after deep inspiration. Breathing is performed rhythmically and slowly while the arms are placed in a normal position. After deep inspiration, one can exhale either by forming lips in the whistling position or by laughing. In each deep-breathing exercise technique, the expiration time of the exhalation process should be longer than the inspiration time.
Section 2: Warm-up exercises (10 min): Hands are clapped by holding them parallel to each other. The fingertips and palms touch each other, stimulating the acupuncture points on both hands, and the individual's energy level rises. To further raise the energy level and synchronize the movements of the group, a rhythm is added in the form of 1–2, 1–2–3. After several rhythmic hand-clapping movements, one more movement is added. Hands are clapped by swinging left and right. Then, an audible rhythm in the form of ho, ho, ha-ha-ha is added to the hand-clapping movement. People in the group look at each other and smile.
Section 3: Childish games (10 min): Childish games are used that will help the participants laugh for no reason, just like a child. Imagining these games and plays, the arms are raised upwards in the form of a “Y” with palms facing the sky, motivating the group by saying “excellent (clap), excellent (clap), yes.” The leader of laughter yoga speaks out “excellent (clap), excellent (clap), hey (arms to the right and left)” to keep the group's energy high and generate enthusiasm in the deep-breathing exercises and laughter exercises sections. According to the energy and desire of the group, this section is generally completed after about 10 min.
Section 4: Laughter exercises (15 min): This section contains a variety of laughter exercises that will bring about laughter, such as greetings, laughter cream, exploding balloon laughter, preparing and drinking strawberry milk, bonuses, hot soup, lion, aloha, bird, appreciation, elevator, and cream pie. A laugh is raised by doing only laughter exercises for no reason at all. At the end of this section, relaxation is achieved for about 3 min using deep-breathing exercises. The group is given verbal guidance: “Put your hand on your heart, feel your heartbeat, let's exhale with a smile, make a wish or pray, smile as if we had achieved our wish,” and the laughter yoga session ends.
In the first session for the current study, brief information was given about laughter yoga, its history, benefits, and breathing techniques before the exercises, and reminders were given in the following sessions.
2.7. Evaluation of data
The coding and evaluation of the data were carried out in the SPSS program. In the evaluation of the data, the mean, standard deviation, number, and percentage distributions were used. The Chi-square test and independent samples t-test were used to compare some descriptive variables of nurses in the EGs and CGs; an independent samples t-test was used for the intergroup comparison of PSS, MBI, and Life Satisfaction Scale pre- and posttest score averages; and a paired samples t-test was used in the intragroup comparisons. Cronbach's alpha coefficient was calculated to test the validity and reliability of the scale. The results were interpreted with a significance level of p < 0.05.
2.8. Ethical principles of the study
Before starting the research, approval (date:27/05/2021, no:4/13) was obtained from the Ethics Committee of Ataturk University Faculty of Medicine. An informative consent form and explanations that participation was voluntary and that they had the freedom to leave the study were added to the online questionnaire form for the target audience. After collecting the final test data, laughter yoga was applied to all nurses in the control group to fulfill the principle of “receiving adequate and appropriate care".
3. Results
Most of the nurses in the experimental and control groups of the study were female, had at least a bachelor's degree, were working in the profession for one to five years, had had COVID-19, had received the COVID-19 vaccine, and had no prior knowledge of laughter yoga.
In the comparison of the descriptive characteristics of the nurses in the experimental and control groups, the difference between the groups was found to not be statistically significant (p > 0.05, Table 1 ). In this regard, it can be stated that the descriptive characteristics of the nurses in the experimental and control groups were similar.
Table 1.
Distribution and intergroup comparison of the descriptive characteristics of the nurses in the experimental and control groups.
| Descriptive characteristics | Experimental group (n = 51) |
Control group (n = 50) |
Test and P values | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age avg. | 28.86 ± 6.79 | 28.86 ± 56.06 | t = 0.002 | ||
| p = 0.998 | |||||
| Age | |||||
| Between 18 and 29 | 36 | 70.6 | 34 | 68.0 | χ2 = 0.080 |
| 30 and over |
15 |
29.4 |
16 |
32.0 |
p = 0.778 |
| Gender | |||||
| Female | 40 | 78.4 | 42 | 84.0 | χ2 = 0.513 |
| Male |
11 |
21.6 |
8 |
16.0 |
p = 0.474 |
| Marital status | |||||
| Married | 18 | 35.3 | 19 | 38.0 | χ2 = 0.080 |
| Single |
33 |
64.7 |
31 |
62.0 |
p = 0.778 |
| Having children | |||||
| Yes | 11 | 21.6 | 14 | 28.0 | χ2 = 0.561 |
| No |
40 |
78.4 |
36 |
72.0 |
p = 0.454 |
| Education level | |||||
| Vocational school of health | 12 | 23.5 | 10 | 20.0 | χ2 = 0.185 |
| Bachelor's degree and over |
39 |
76.5 |
40 |
80.0 |
p = 0.667 |
| Total working time in the profession | |||||
| 1–5 years | 31 | 60.8 | 27 | 54.0 | |
| 6–10 years | 10 | 19.6 | 12 | 24.0 | χ2 = 0.495 |
| 11 years and over |
10 |
19.6 |
11 |
22.0 |
p = 0.781 |
| Working type | |||||
| Continuous nighttime | 8 | 15.7 | 8 | 16.0 | |
| Continuous daytime | 11 | 21.6 | 14 | 28.0 | χ2 = 0.617 |
| Day–night rotation |
32 |
62.7 |
28 |
56.0 |
p = 0.735 |
| Status of having had COVID-19 | |||||
| Yes | 32 | 62.7 | 33 | 66.0 | χ2 = 0.117 |
| No |
19 |
37.3 |
17 |
34.0 |
p = 0.733 |
| COVID-19 vaccination status | |||||
| Yes | 49 | 96.1 | 46 | 92.0 | χ2 = 0.752 |
| No |
2 |
3.9 |
4 |
8.0 |
p = 0.386 |
| Informed about the laughter yoga | |||||
| Yes | 10 | 19.6 | 12 | 24.0 | χ2 = 0.286 |
| No | 41 | 80.4 | 38 | 76.0 | p = 0.593 |
χ2 = Chi-squared test.
t = Independent samples t-test.
The pretest Perceived Stress Scale total score average was 32.47 ± 3.57 in nurses in the EG and 31.36 ± 5.03 in nurses in the CG; the difference between the groups was not statistically significant. Accordingly, the perceived stress levels of the nurses in the experimental and control groups were found to be similar in the pretest (t = 1.279, p > 0.05) (Table 2 ).
Table 2.
Intergroup and intragroup comparison of the pretest and posttest Perceived Stress Scale total score averages of the nurses in the experimental and control groups.
| Groups | First measurement Mean ± SD | Final measurement Mean ± SD | Test and p values |
||||
|---|---|---|---|---|---|---|---|
| ta | df | p value | |||||
| Experimental group | 32.47 ± 3.57 | 21.39 ± 4.65 | 16.794 | 50 | 0.000 | ||
| Control group | 31.36 ± 5.03 | 31.42 ± 5.03 | 0.171 | 49 | 0.865 | ||
| Test and p values | tb | 1.279 | 10.394 | ||||
| df | 99 | 99 | |||||
| p value | 0.204 | 0.000 | |||||
Paired samples t-test.
Independent samples t-test.
The posttest Perceived Stress Scale total score average was 21.39 ± 4.65 in the nurses in the EG and 31.42 ± 5.03 in the nurses in the CG, with a statistically significant difference. Accordingly, although the perceived stress levels of the nurses in the EG who had laughter yoga decreased after laughter yoga, there was no significant change in the perceived stress levels of the nurses in the CG (t = 10.394, p < 0.001) (Table 2).
The difference in the pretest Burnout Inventory total and subscale score averages of the nurses in the experimental and control groups was not statistically significant; accordingly, the nurses in the experimental and control groups were similar in terms of the pretest measurements of emotional exhaustion, depersonalization, personal accomplishment, and general burnout levels (p > 0.05) (Table 3 ).
Table 3.
Intergroup and intragroup comparison of the pretest and posttest Maslach Burnout Inventory total and subscale score averages of the nurses in the experimental and control groups.
| Groups | First measurement Mean ± SD | Final measurement Mean ± SD | Test and p values |
||||||
|---|---|---|---|---|---|---|---|---|---|
| ta | df | p value | |||||||
| Emotional exhaustion subscale | Experimental group | 22.45 ± 8.48 | 13.96 ± 5.90 | 13.662 | 50 | 0.000 | |||
| Control group | 21.96 ± 6.81 | 21.50 ± 7.11 | 1.798 | 49 | 0.078 | ||||
| Test and p values | tb | 0.320 | 5.802 | ||||||
| df | 99 | 99 | |||||||
|
p value |
0.749 |
0.000 |
|||||||
| Depersonalization subscale | Experimental group | 8.27 ± 3.99 | 5.47 ± 4.38 | 5.859 | 50 | 0.000 | |||
| Control group | 8.78 ± 4.54 | 8.68 ± 4.45 | 0.340 | 49 | 0.736 | ||||
| Test and p values | tb | 0.594 | 3.649 | ||||||
| df | 99 | 99 | |||||||
|
p value |
0.554 |
0.000 |
|||||||
| Personal accomplishment subscale | Experimental group | 22.74 ± 4.58 | 27.80 ± 3.58 | 11.578 | 50 | 0.000 | |||
| Control group | 23.12 ± 4.88 | 22.90 ± 4.91 | 1.065 | 49 | 0.292 | ||||
| Test and p values | tb | 0.398 | 5.737 | ||||||
| df | 99 | 99 | |||||||
|
p value |
0.692 |
0.000 |
|||||||
| Total | Experimental group | 53.47 ± 10.61 | 42.43 ± 9.57 | 22.246 | 50 | 0.000 | |||
| Control group | 53.86 ± 10.12 | 53.44 ± 10.27 | 1.382 | 49 | 0.173 | ||||
| Test and p values | tb | 0.189 | 5.574 | ||||||
| df | 99 | 99 | |||||||
| p value | 0.851 | 0.000 | |||||||
Paired samples t-test.
Independent samples t-test.
It was determined that the difference between the Burnout Inventory total and subscale posttest score averages of the nurses in the experimental and control groups was statistically significant. Accordingly, the levels of emotional exhaustion and depersonalization of the nurses in the EG who had laughter yoga decreased, their personal success levels increased, and their overall burnout levels decreased. Moreover, there was no significant change in the levels of emotional exhaustion, depersonalization, personal accomplishment, and overall burnout levels of the nurses in the CG (p < 0.001) (Table 3).
The pretest Life Satisfaction Scale total score average was 14.49 ± 3.90 in nurses in the EG and 14.06 ± 3.79 in nurses in the CG; the difference between the groups was not statistically significant. Accordingly, the life satisfaction levels of the nurses in the experimental and control groups were found to be similar in the pretest (t = 0.561, p > 0.05) (Table 4 ).
Table 4.
Intergroup and intragroup comparison of the pretest and posttest Life Satisfaction Scale total score averages of the nurses in the experimental and control groups.
| Groups | First measurement Mean ± SD | Final measurement Mean ± SD | Test and p values |
|||||
|---|---|---|---|---|---|---|---|---|
| ta | df | p value | ||||||
| Experimental group | 14.49 ± 3.90 | 23.39 ± 4.54 | 14.752 | 50 | 0.000 | |||
| Control group | 14.06 ± 3.79 | 14.12 ± 3.66 | 0.343 | 49 | 0.733 | |||
| Test and p values | tb | 0.561 | 11.271 | |||||
| df | 99 | 99 | ||||||
| p value | 0.576 | 0.000 | ||||||
Paired samples t-test.
Independent samples t-test.
The posttest Life Satisfaction Scale total score average was 23.39 ± 4.54 in the nurses in the EG and 14.12 ± 3.66 in the nurses in the CG, with a statistically significant difference. Accordingly, although the life satisfaction levels of the nurses in the EG who had laughter yoga increased after laughter yoga, there was no significant change in the life satisfaction levels of the nurses in the CG (t = 11.271, p < 0.001) (Table 4).
4. Discussion
In the current study, it was found that the stress levels perceived by the nurses in the EGs and CGs were similar and high at the first measurement (Table 2). At the end of the study, there was no significant change in the perceived stress levels of the nurses in the control group who did not undergo any intervention, but the perceived stress levels of the nurses in the EG who underwent laughter yoga were significantly decreased (Table 2). This finding supports hypothesis H1 “Laughter yoga reduces the stress perceived by nurses during the pandemic.” It has been emphasized in the literature that laughter has many positive physiological effects. The most important of these is to help individuals cope with stress and reduce their anxiety [41]. It has been noted that the body physically responds to laughter, such as through an increase in the level of beta-endorphins, a decrease in stress hormones such as adrenaline, noradrenaline, and cortisol, an improvement in mental processes, and a decrease in blood pressure and muscle tension [32,42]. In the literature, studies have reported that laughter yoga also provides a significant decrease in salivary cortisol, which is considered a biological marker of stress [[43], [44], [45], [46]]. In meta-analysis studies, it was found that laughter therapy is an effective complementary method and reduces anxiety levels [28,47]. Zhao et al. found that the humor intervention program they applied to older adults was effective in reducing anxiety symptoms and increasing subjective well-being [48]. According to the study by Deible et al. stress reduction methods such as yoga and meditation applied to nurses improve the coping mechanism and reduce perceived stress. Moreover, it was emphasized that the use of these methods by nurses would contribute to an improvement of their general health and the provision of better quality patient care [49]. Similar results were obtained in La Torre et al.’s study [50]. Another study has shown that repeated laughter yoga sessions have psychologically beneficial effects, especially on tension and anxiety; in the same study, it was reported that there was a significant decrease in adrenocorticotropic hormone and cortisol values related to the stress levels of the participants after the fourth laughter yoga session [51]. Researchers have argued that laughing minimizes existing psychological stress by reducing the release of neuroendocrine and stress-related hormones [52]. These results are in line with the current research's findings. The highly contagious nature of COVID-19, uncertainty about the end of the epidemic, one-on-one and long-term contact with infected patients during the provision of care, fear of infecting others their immediate environment with the virus, and an increasing number of cases of disease and death also increase the stress perceived by nurses. In line with this, the results from the current study have shown that laughter yoga can be an effective method that can be used to reduce the stress perceived by nurses, especially during intense and stressful periods, such as the pandemic.
In the present study, the emotional exhaustion and depersonalization pretest levels of the nurses in the EGs and CGs were similarly high, personal accomplishment levels were similarly low, and overall burnout levels were found to be similarly high (Table 3). At the end of the study, there was no significant change in the emotional exhaustion, depersonalization, personal accomplishment, and overall burnout levels of the nurses in the control group, who did not undergo any intervention, but it was found that the emotional exhaustion and depersonalization levels of the nurses in the EG who underwent laughter yoga decreased and their personal accomplishment levels increased; hence, their overall burnout levels decreased (Table 3). This finding supports hypothesis H2 “Laughter yoga reduced the burnout levels of nurses during the pandemic.” In their study comparing the burnout status of Iranian and Turkish nurses, Özlü et al. reported that Turkish nurses had high levels of emotional exhaustion and depersonalization, while Iranian nurses had higher levels of personal accomplishment; this was caused by the excessive burden caused by the excess number of patients in Turkey. In the same study, recommendations were made on various practices, including the use of “effective humor,” for the prevention of burnout [53]. This is because humor has many physical, emotional, social, and cognitive benefits. For example, during laughter, some physiological positive changes occur in the body (muscle tension decreases, pain tolerance, and immune globulin-A level increase, stress hormones decrease, burnout, depression, and anxiety levels decrease, interpersonal relationship and social interaction increase, providing psychological well-being). In addition, humor supports physical, emotional, social, and cognitive development, making it easier to cope with existing problems [28,54]. In the literature, it was emphasized that stress reduction methods improve both self-care and the care provided to others while reducing exhaustion and burnout [26]. In a study conducted by Shattla et al. with psychiatric nurses, after laughter therapy, there was a significant decrease in the burnout levels of nurses in the EG compared with the CG. It has been concluded that laughter therapy applied to psychiatric nurses has a positive effect on burnout [31]. The findings obtained from these studies support the current research results. In contrast to the research findings, Lynes et al. found that eight-week laughter yoga applied to nurses was not effective in reducing burnout [33]. This suggests that burnout may vary among cultures and based on the type of care being given. In addition, this result can also be attributed to the motivation and enthusiasm of nurses to know and successfully practice laughter yoga skills. Reducing stress and preventing burnout in nurses play a key role in improving mental and physical well-being. The application of laughter yoga, which is a complementary, simple, and reliable method for improving the health and well-being of nurses during the pandemic, can contribute to physical and psychological well-being.
In the current study, it was found that the life satisfaction levels of nurses in the EGs and CGs were similar and low at the first measurement (Table 4). At the end of the study, it was found that there was no significant change in the life satisfaction levels of the nurses in the CG who did not undergo any intervention, but the life satisfaction levels of the nurses in the EG who underwent laughter yoga were found to decrease significantly (Table 4). This finding supports hypothesis H3 “Laughter yoga increased the life satisfaction of nurses during the pandemic.” Ellis et al. applied laughter yoga to individuals living in an elderly care nursery once a week for six weeks. After the application (first, third, and sixth sessions), an increase in happiness levels and decrease in negative moods (third and sixth sessions) were recorded [55]. In another similar study, it was found that laughter therapy increases life satisfaction and health perception, increases the indicators that define positive well-being, and decreases the level of emotions that negatively affect well-being. It has been observed that laughter therapy also leads to an increase in the life expectancy of individuals [56]. These results support the present study's findings. It can be stated that working in a non-stressful environment has a significant impact on nurses' life satisfaction [57]. Some studies have shown that using humor to deal with stressful situations can help individuals make more positive assessments, which can increase happiness and life satisfaction [58]. In line with these results, laughter yoga is a noninvasive, nonpharmacological therapy with positive physiological, psychological, and social effects on health.
4.1. Strengths and limitations
The current research results was limited to the nurses who participated. The scales used are self-report tools, and the data are limited to the answers given by the nurses. Moreover, the lack of measurement of the persistence of laughter yoga after the four weeks is also a limitation. Due to the nature of the study, it could not be double-blind. It was done single-blindly to eliminate bias. Data were collected online. The researchers who practiced laughter yoga and did the analysis were different. The strength of the study is the limited number of studies on laughter yoga applied to nurses during the pandemic period and the fact that this study is a randomized controlled study.
5. Conclusion
In the current study, it was found that laughter yoga applied to nurses during the pandemic reduced perceived stress and burnout levels and increased life satisfaction. Accordingly, laughter yoga is a simple, safe, and effective method that can be used to control the negative emotions that emerge during intense and stressful periods. Self-care practices such as laughter yoga can improve nurses’ overall health and provide better quality patient care. In hospitals particularly, the units and authorities charged with ensuring employee safety should recommend the practice of laughter yoga to all healthcare professionals and inform them about its benefits.
In addition, the effectiveness of the practice of laughter yoga can also be associated with the frequency and number of practices; therefore, frequent and more sessions can ensure better results.
5.1. Safety of participants
The safety of participants in the study was ensured by following the Helsinki Declaration principles. After the participants were informed about the study, verbal consent was obtained from the people who wanted to participate. During the collection of research data, the following principles were fulfilled: “Informed Consent” by informing the participants about the research, “Respect for Autonomy” by stating that participants are free to participate in the research, and “Protection of Confidentiality and Confidentiality” by assuring research participants that their information would be kept confidential. The participants were informed that the research would be conducted purely for scientific purposes and that they would not encounter any risks during the application. They were also advised of their right to leave the study at any stage.
Funding
We confirm that we have not taken any funding support.
CRediT authorship contribution statement
Aslı SİS ÇELİK: Conceptualization, Conception and design of study, acquisition of data, Writing - original draft, Writing - review & editing. Tülay KILINÇ: Writing - original draft, acquisition of data, Analysis and interpretation of data, Writing - review & editing. All the authors critically read the initial manuscript, commented on all parts of the text, and approved the final version of the manuscript.
Declaration of conflict of interest
There is no conflict of interest between any relevant persons or institutions.
Acknowledgements
We are grateful to our participants.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Phil D., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aydın T., Ağaçdiken Alkan S. In nurses colleague solidarity in Covıd-19 pandemia process and burnout status. J. Samsun Health Sci. 2021;6(1):11–22. doi: 10.47115/jshs.955279. [DOI] [Google Scholar]
- 3.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arpacıoğlu S.M., Baltacı Z., Ünübol B. Burnout, fear of Covid, depression, occupational satisfaction levels and related factors in healthcare professionals in the COVID-19 pandemic. Cukurova Med J. 2021;46(1):88–100. doi: 10.17826/cumj.785609. [DOI] [Google Scholar]
- 5.Yeşil Bayülgen M., Bayülgen A., Yeşil F.H., Akcan Türksever H. Determination of anxiety and hopelessness levels of nurses working during the covıd-19 pandemic process. University Health Sci. J. Nurse. 2021;3(1):1–6. doi: 10.48071/sbuhemsirelik.83922. [DOI] [Google Scholar]
- 6.Labrague L.J., De los Santos J.A.A. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020;28:1653–1661. doi: 10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khasne R.W., Dhakulkar B.S., Mahajan H.C., Kulkarni A.P. Burnout among healthcare workers during covıd-19 pandemic ın India: results of a questionnaire-based survey. Indian J. Crit. Care Med. 2020;24(8):664–671. doi: 10.5005/jp-journals-10071-23518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Çevik Aktura S., Özden G. Psychologıcal effects of the epıdemıc: nurses of Covıd-19. The. J. Int. Soc. Res. 2020;13(73):1146–1151. [Google Scholar]
- 9.Hiçdurmaz D., Üzar Özçetin Y.S. Protection of COVID-19 frontline nurses' mental health and prevention of psychological trauma. J. Hacettepe University Faculty Nurse. 2020;7:1–7. doi: 10.31125/hunhemsire.775531. [DOI] [Google Scholar]
- 10.Franza F., Basta Rpellegrino F., Solamita B., Fasano V. The role of fatigue of compassion, burnout and hopelessness in healthcare:Experience in the time of Covid-19 outbreak. Psychiatr. Danub. 2020;32(1):10–14. [PubMed] [Google Scholar]
- 11.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Hunter J.J. Long term psychological and occupational effects of providing hospital health care during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheong D., Lee C. Impact of Severe Acute Respiratory Syndrome on anxiety levels of front-line health care workers. Hong Kong Med. J. 2004;10(5):325–330. [PubMed] [Google Scholar]
- 13.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological ımpact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y., Wang C., Pan W., Zheng J., Gao J., Huang X., Zhu C. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in Wuhan and Shanghai, China. Front. Psychiatr. 2020;11:1154. doi: 10.3389/fpsyt.2020.565520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aksoy Y.E., Koçak V. Psychological effects of nurses and midwives due to COVID-19 outbreak: the case of Turkey. Arch. Psychiatr. Nurs. 2020;34(5):427–433. doi: 10.1016/j.apnu.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., Huang H. Work stress among Chinese nurses to support Wuhan in fighting against COVID‐19 epidemic. J. Nurs. Manag. 2020;28:1002–1009. doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiong H., Yi S., Lin Y. The psychological status and self-efficacy of nurses during COVID-19 outbreak: a cross-sectional survey. Inquiry: J. Health Care Org. Provision. Finance. 2020;57:1–6. doi: 10.1177/0046958020957114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shen Y., Zhan Y., Zheng H., Liu H., Wan Y., Zhou W. Anxiety and its association with perceived stress and insomnia among nurses fighting against COVID-19 in Wuhan: a cross-sectional survey. J. Clin. Nurs. 2021;30:2654–2664. doi: 10.1111/jocn.15678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jalili M., Niroomand M., Hadavand F., Zeinali K., Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int. Arch. Occup. Environ. Health. 2021;94:1345–1352. doi: 10.1007/s00420-021-01695-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janeway D. The role of psychiatry in treating burnout among nurses during the COVID-19 pandemic. J. Radiol. Nurs. 2020;39(3):176–178. doi: 10.1016/j.jradnu.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ersezgin R., Sevi Tok E.S. The predictive effects of perceived work stress, psychological resilience, coping styles and self-compassion on burnout level. Uludağ University Faculty of Arts and Sciences Journal of Social Sciences. 2019;20(36) doi: 10.21550/sosbilder.457245. [DOI] [Google Scholar]
- 22.Kamışlı S., Yüce D., Karakilic B., Kilickap S., Hayran M. Cancer patients and oncology nursing: perspectives of oncology nurses in Turkey. Niger. J. Clin. Pract. 2017;20(9):1065–1073. doi: 10.4103/njcp.njcp_108_16. [DOI] [PubMed] [Google Scholar]
- 23.Kaya N., Kaya H., Erdoğan A.S., Uygur E. Burnout of nurses who work in a government hospital. Int. J. Hum. Sci. 2010;7(1):401–419. [Google Scholar]
- 24.Aryankehesal A., Mohammadibakhsh R., Hamidi Y., Alidoost S., Behzadifar M., Sohrabi R., Farhadi Z. Interventions on reducing burnout in physicians and nurses: a systematic review. Med. J. Islam. Repub. Iran. 2019;33:77. doi: 10.34171/mjiri.33.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kantek F., Kabukcuoğlu K. Burnout in nurses: a meta analysis of related factors. J. Human Sci. 2017;14(2):1242–1254. doi: 10.14687/jhs.v14i2.4431. [DOI] [Google Scholar]
- 26.Tarantino B., Earley M., Audia D., D'Adamo C., Berman B. Qualitative and quantitative evaluation of a pilot integrative coping and resiliency program for healthcare professionals. Explore. 2013;9(1):44–47. doi: 10.1016/j.explore.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Suleiman-Martos N., Gomez-Urquiza J.L., Aguayo-Estremera R., Cañadas-De La Fuente G.A., De La Fuente-Solana E.I., Albendín-García L. The effect of mindfulness training on burnout syndrome in nursing: a systematic review and meta-analysis. J. Adv. Nurs. 2020;76:1124–1140. doi: 10.1111/jan.14318. [DOI] [PubMed] [Google Scholar]
- 28.Doğan M.D. The effect of laughter therapy on anxiety: a meta-analysis. Holist. Nurs. Pract. 2020;34(1):35–39. doi: 10.1097/HNP.0000000000000363. [DOI] [PubMed] [Google Scholar]
- 29.Meiera M., Wirzb L., Dickinsonc P., Pruessner J.C. Laughter yoga reduces the cortisol response to acute stress in healthy individuals. Int. J. Biol. Stress. 2021;24(1):44–52. doi: 10.1080/10253890.2020.1766018. [DOI] [PubMed] [Google Scholar]
- 30.Kataria M. Madhuri International; Mumbai (India): 2011. Laugh for No Reason. [Google Scholar]
- 31.Shattla S.I., Mabrouk S.M., Abed G.A. Effectiveness of laughter yoga therapy on job burnout syndromes among psychiatric nurses. Int. J. Nurs. 2019;6(1):33–47. doi: 10.15640/ijn.v6n1a5. [DOI] [Google Scholar]
- 32.Yim J. Therapeutic benefits of laughter in mental health: a theoretical review. Tohoku J. Exp. Med. 2016;239(3):243–249. doi: 10.1620/tjem.239.243. [DOI] [PubMed] [Google Scholar]
- 33.Lynes L., Kawar L., Valdez R.M. Can laughter yoga provide stress relief for clinical nurses? Nurs. Manag. 2019;50(6):30–37. doi: 10.1097/01.NUMA.0000558481.00191.78. [DOI] [PubMed] [Google Scholar]
- 34.Cohen S., Kamarck T., Mermelstein S. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 35.Eskin M., Harlak H., Demirkıran F., Dereboy Ç. Vol. 5. 2013. The adaptation of the perceived stress scale into Turkish: a reliability and validity analysis; pp. 132–140. (New Symposium Journal). 3. [Google Scholar]
- 36.Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2:99–113. [Google Scholar]
- 37.Ergin C. Adaptation of burnout and maslach burnout scale in doctors and nurses. VII. Nat. Psychiatry Congress Book Turkish Pysychol. Assoc. Pub. 1992 [Google Scholar]
- 38.Diener E., Emmons R.A., Larsen R.J., Griffin S. The satisfaction with life scale. J. Pers. Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 39.Dağlı A., Baysal N. Daptatıon of the satısfactıon wıth lıfe scale ınto Turkısh: the study of valıdıty and relıabılıty. Electronic. J. Soc. Sci. 2016;15:1250–1262. doi: 10.17755/esosder.263229. [DOI] [Google Scholar]
- 40.Öztürk F.Ö., Tezel A. Laughter yoga and nursing. J. Continue. Med. Edu. 2021;30(2):144–151. doi: 10.17942/sted.863483. [DOI] [Google Scholar]
- 41.Bast E.S., Berry E.M. Laugh away the fat? Therapeutic humor in the control of stress-induced emotional eating. Rambam Maimonide. Med. J. 2014;5(1) doi: 10.5041/RMMJ.10141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ripoll R. The therapeutic value of laughter in medicine. Alternative Ther. Health Med. 2010;16(6):56–64. [PubMed] [Google Scholar]
- 43.Öztürk F.O., Tezel A. Effect of laughter yoga on mental symptoms and salivary cortisol levels in first-year nursing students: a randomized controlled trial. Int. J. Nurs. Pract. 2021;27 doi: 10.1111/ijn.12924. [DOI] [PubMed] [Google Scholar]
- 44.Cha M.Y., Hong H.S. Effects on the laughter score, cortisol and ımmunoglobulin of laughter therapy in middle aged women. J. Korea Biol. Nurse. Sci. 2013;15(4):230–236. doi: 10.7586/jkbns.2013.15.4.230. [DOI] [Google Scholar]
- 45.Chang C., Tsai G., Hsieh C. J. Psychological, immunological and physiological effects of a Laughing Qigong Program (LQP) on adolescents. Compl. Ther. Med. 2013;21(6):660–668. doi: 10.1016/j.ctim.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 46.Pandey P.T., Sıngh V., Haıder J. Effect of yoga on salivary cortisol in medical student. Int. J. Res. Med. Sci. 2016;4(11):4995–4998. [Google Scholar]
- 47.Zhao J., Yin H., Zhang G., Li G., Shang B., Wang C., Chen L. A meta‐analysis of randomized controlled trials of laughter and humour interventions on depression, anxiety and sleep quality in adults. J. Adv. Nurs. 2019;75:2435–2448. doi: 10.1111/jan.14000. [DOI] [PubMed] [Google Scholar]
- 48.Zhao J., Yin H., Wang X., Zhang G., Jia Y., Shang B., Zhao J., Wang C., Chen L. Effect of humour intervention programme on depression, anxiety, subjective well-being, cognitive function and sleep quality in Chinese nursing home residents. J. Adv. Nurs. 2020;76:2709–2718. doi: 10.1111/jan.14472. [DOI] [PubMed] [Google Scholar]
- 49.Deible S., Fioravanti M., Tarantino B., Cohen S. Implementation of an ıntegrative coping and resiliency program for nurses. Global. Adv. Health Med. 2015;4(1):28–33. doi: 10.7453/gahmj.2014.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.La Torre G., Raffone A., Peruzzo M., Calabrese L., Cocchiara R.A., D'Egidio V., Leggieri P.F., Dorelli B., Zaffina S., Mannocci A. Yoga and mindfulness as a tool for ınfluencing affectivity, anxiety, mental health, and stress among healthcare workers: results of a single-arm clinical trial. J. Clin. Med. 2020;9:1037. doi: 10.3390/jcm9041037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tanaka A., Tokuda N., Ichihara K. Psychological and physiological effects of laughter yoga sessions in Japan: a pilot study. Nurs. Health Sci. 2018;20:304–312. doi: 10.1111/nhs.12562. [DOI] [PubMed] [Google Scholar]
- 52.Kim S.H., Kim Y.H., Kim H.J. Laughter and stress relief in cancer patients: a pilot study. Evid. base Compl. Alternative Med. 2015 doi: 10.1155/2015/864739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Özlü Z.K., Yayla A., Gümüs K., Khaghanyrad E. Comparison of nurses in two different cultures: who experiences more burnout. J. Perianesth. Nurs. 2017;32(3):238–244. doi: 10.1016/j.jopan.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 54.Tuğut N., Kaya D. Relation between therapeutic humor usage of nurses and their problem solving skills. Dokuz Eylul University Facul. Nurs. Electronic J. 2017;10(3):131–136. [Google Scholar]
- 55.Ellis J.M., Ben-Moshe R., Teshuva K. Laughter yoga activities for older people living in residential aged care homes: a feasibility study. Australas. J. Ageing. 2017;36(3):28–31. doi: 10.1111/ajag.12447. [DOI] [PubMed] [Google Scholar]
- 56.Brown A., Jeffrey C., Moyle D. Laughter yoga therapy in haemodialysis: one unit's experience. Renal Soc. Australia J. 2019;15:38–46. [Google Scholar]
- 57.Camci G.B., Kavuran E. Determination of the correlation of job stress and burnout levels of nurses with their job and life satisfaction levels. J. Anatolia Nurse Health Sci. 2021;24(2):274–283. doi: 10.17049/ataunihem.930846. [DOI] [Google Scholar]
- 58.Cann A., Stilwell K., Taku K. Humor styles, positive personality and health. Eur. J. Psychol. 2010;6(3):213–235. doi: 10.5964/ejop.v6i3.214. [DOI] [Google Scholar]