ABSTRACT
Introduction:
Mushroom poisoning occurs from consumption of the wild variants of mushroom containing varied forms of toxins. Among those toxins, amatoxin containing mushrooms are known for the significant morbidity and mortality from hepatic toxicity and delayed gastroenteritis. Although not a very common cause of poisoning, it is prevalent in the north-eastern region of India, especially during the rainy summer seasons when the wild variants are found abundantly and often confused with the edible variants.
Aims and Objectives:
To study the clinical and biochemical profiles and short term outcomes of patients with mushroom poisoning admitted to a tertiary care hospital.
Materials and Methods:
We analyzed the data of patients with mushroom poisoning admitted to a tertiary care institute in north-eastern India between January 2015 to December 2020 to study their clinical and biochemical profiles, and short-term outcomes. Their clinical features, biochemical parameters, management, and in-hospital outcomes were noted. All data was recorded in Microsoft MS Excel and analyses done using SPSS version 22.
Results:
Of the 44 patients with mushroom poisoning, 23 (52%) were male and 21 (47%) were female, with a mean age of 20.13 years. Seventeen patients (38%) had delayed liver failure and delayed gastroenteritis, 19 patients (43%) had acute gastroenteritis syndrome, 5 patients (11%) had cholinergic symptoms, one patient (2%) each had acute kidney injury and a disulfiram-type reaction with headache. The mean hospital stay of the patients was 5 days. In-hospital mortality occurred in 10 (58%) patients with delayed liver failure and none of the patients with the other complications died.
Conclusion:
This study revealed a high prevalence of mushroom poisoning that caused delayed liver toxicity and delayed gastroenteritis, probably amatoxin-induced, which is fatal, thus accounting for high mortality and poor outcomes in these patients.
Keywords: Amatoxin, mushroom, Northeast India, poisoning, syndromes
Introduction
Mushroom poisoning occurs with the consumption of poisonous mushrooms containing toxins responsible for different syndromic presentations and some having high mortality. The consumption of wild mushrooms in India is common among many ethnic tribes. However, some of the wild mushrooms are known to be poisonous especially those containing amatoxins which results in fulminant hepatitis. The exact prevalence of mushroom poisoning in our country has not been accounted for because such poisoning is uncommon or unreported. In recent years, mushroom poisoning and deaths have been reported in case reports and case series during the rainy summer seasons.[1,2,3,4,5,6,7,8,9,10] It is during these time of the year that wild poisonous mushrooms grow abundantly and they are often mistaken with the edible ones. In two separate studies by Goldfrank LR et al.[11] and Brent J et al.,[12] described 14 syndrome presentations caused by 12 groups of toxins. The presentation of mushroom poisoning as different syndromes can help us to identify the associated toxins and early medical therapy can prevent death from the lethal amatoxins which are commonly found in the Amanita, Lepiota and Galerina species of the mushroom.[12,13]
Although sporadic cases of death following mushroom consumption have been reported from various part of India[2,3,5] there is no data on the pattern and magnitude of complications and outcome from the north eastern part of the country. Therefore, we conducted this study to report the clinical and biochemical profiles and short term outcomes of patients with mushroom poisoning admitted to a tertiary care hospital.
Material and Methods
Study design and participants
An observational cross- sectional study of patients with mushroom poisoning presenting to our institute was conducted from 2015 to 2020 to describe their clinical and biochemical profiles, and short- term outcomes. All patients who presented with a history of mushroom poisoning were included in the study. Clinical syndromes were based on clinical presentations and biochemical results. However, specific toxin analyses and mushroom identification by mycologists could not be performed.
Statistical analysis
Data entry and analysis were performed using SPSS software (IBM SPSS 22.0, Armonk, New York, USA). The demographic profile was recorded retrospectively in terms of the time of onset of symptoms, presentation to the hospital, clinical presentation, and laboratory parameters. The means and standard deviations were analyzed for continuous data, while percentages/proportions were described for categorical data. Comparisons of continuous variables between the syndrome of “delayed liver toxicity and delayed gastroenteritis” and “acute gastroenteritis syndrome” groups were analyzed using t-test (independent sample t-tests). Statistical significance was set at P < 0.05.
Ethical approval
Ethical approval was obtained from the Institutional Board vide letter No. NEIGR/IEC/M3/F17/17 dated 7th December 2017.
Results
A total of 44 patients were admitted with mushroom poisoning between January 2015 and December 2020, comprising 23 males (52%) and 21 females (48%), with a mean age of 20.13 (SD ± 15.39). The age of those affected ranged from 2 to 60 years [Table 1]. The main source of wild mushrooms was self- picked by patients or relatives for consumption [Figures 1 and 2]. Six clinical syndromes were identified in our study [Table 2], with acute gastroenteritis (38%) being the commonest, followed by hepatic failure and delayed gastroenteritis (43%). Of the 17 patients with “delayed liver toxicity and delayed gastroenteritis syndrome” 10 patients (58%) expired due to complications of fulminant hepatitis. Most of these patients had late onset of presentation of symptoms (after 6 hours) and consequently delayed hospitalization. However none of the patients with the other syndromes died. A comparative analysis between the two syndromes “Delayed liver toxicity and delayed gastroenteritis” and “acute gastroenteritis” shows that the severity is more in the former in terms of complications bleeding, encephalopathy, hypoglycemia, acute kidney injury, requirement for mechanical ventilation. [Table 3] There were two seasonal peaks in the incidence of mushroom poisoning admission to our hospital occurring in two parts of the years, the rainy summer seasons (March, April, and May) and autumn (August, September, and October), where the rainfall and humidity are high [Figures3 and 4].
Table 1.
Demographic Profile of the patients with Mushroom Poisoning from January 2015 - June 2020 (n=44)
| Age distribution | ||
|---|---|---|
|
| ||
| Number of cases | Frequency (%) | |
| Age group (Years) | ||
| 2-12 | 15 | 34 |
| 13-18 | 12 | 27 |
| 19-60 | 17 | 38 |
| Mean Age (Years) | 20.13 (SD±15.39) | |
| Sex | ||
| Male | 23 | 52 |
| Female | 21 | 48 |
| Source of mushroom | ||
| Wild | 44 | 100 |
| Market | - | - |
Figure 1.

Mushrooms that grew at the site and were picked and consumed by the patients who showed delayed hepatitis and delayed gastroenteritis syndrome
Figure 2.

Basket of plucked mushrooms brought to the hospital by relatives of patients who died of delayed liver toxicity and delayed gastroenteritis
Table 2.
Clinical profile and outcome of the Syndromes with Mushroom Poisoning
| Syndrome (number) | Onset of symptoms (Hours) | Time of presentation to hospital (days) | Symptoms (number) | Complications (number) | ICU care | Death | Total hospital stay (days; Mean±SD) |
|---|---|---|---|---|---|---|---|
| Delayed liver toxicity and delayed gastroenteritis (17) | >6 h | 2.41±2.12 | Loose stool (13) Vomiting (15) Pain abdomen (9) Altered sensorium (5) Bleeding (2) |
Hepatitis (17) Pre-renal failure (6) Coagulopathy (17) Hypoglycemia (10) |
17 | 10 | 5.57±7.5 |
| Acute gastroenteritis (19) | <6 h (17) >6 h (2) |
3.36±2.24 | Loose stool (5) Vomiting (19) Abdominal pain (12) |
Pre-renal failure (2) | None | None | 3.32±2.16 |
| Cholinergic mushroom poisoning (5) | <6 h | 2 | Fever with increased salivation | None | None | None | 3 |
| Acute kidney injury (1) | >6 h | 2 | Vomiting with abdominal pain | Renal failure | None | None | 15 |
| Disulfram type of reaction (1) | >6 h | 1 | Vomiting, headache and flushing under alcohol influence | None | None | None | 2 |
| Headache (1) | >6 h | 1 | Headache | None | None | None | 2 |
Table 3.
Clinical, Biochemical profile and short outcome of mushroom poisoning with Delayed liver toxicity and delayed gastroenteritis syndrome and Acute gastroenteritis syndrome
| Syndrome | Delayed liver toxicity and delayed gastroenteritis | Syndrome | Delayed liver toxicity and delayed gastroenteritis |
|---|---|---|---|
| No of patients | 17 | 19 | |
| Time of presentation to the hospital (days) | 2.41±2.12 | 3.36±2.24 | P<0.199 |
| ALT (IU/L) | 3056±1695 | 32.94±2.80 | P<0.000 |
| AST (IU/L) | 1898±468 | 45.21±6.17 | P<0.000 |
| PT (sec) | 52.35±33.07 | 14.15±1.77 | P<0.000 |
| INR | 6.45±4.49 | 1.21±0.28 | P<0.000 |
| aPTT (sec) | 92.59±40.33 | 34.26±4.80 | P<0.000 |
| Creatinine (mg/dl) | 1.60±2.13 | 0.83±0.60 | P<0.139 |
| Urea (mg/dl) | 44.00±35.89 | 24.15±9.42964 | P<0.026 |
| RBS (mg/dl) | 68.31±34.22 | 111.68±12.83 | P<0.000 |
| ICU care | 17 | None | P<0.000 |
| Mechanical Ventilation | 11 | None | P<0.000 |
| Duration of hospital stay (in days) | 5.57±7.5 | 3.32±2.16 | P<0.199 |
| Death | 10 (58.82%) | Nil |
P<0.000=may be written as <0.001; ALT : Alanine Aminotransferase; AST : Aspartate aminotransferase; PT-Prothrombin time; INR- International normalized ratio; aPTT: Activated partial thromboplastin time; RBS: Random Blood Sugar; ICU=Intensive Care Unit
Figure 3.
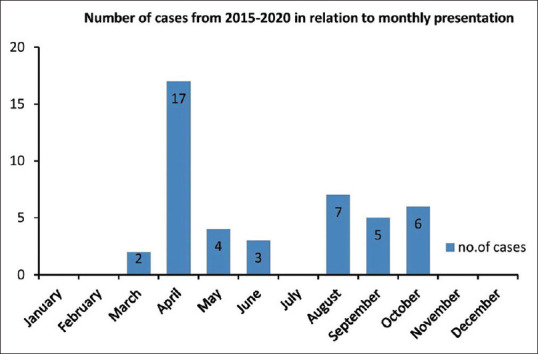
Cases based on a monthly distribution
Figure 4.
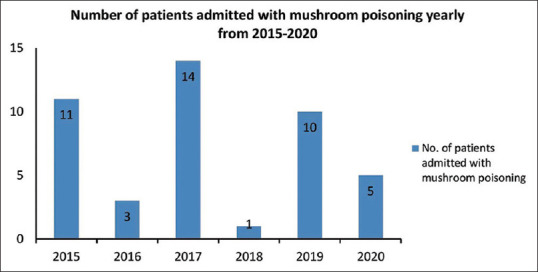
Cases based on an annual distribution
Discussion
From what is known from literature there are more than 10,000 species of mushroom worldwide. However, only a small percentage is known to be poisonous. Over 1200 species of mushrooms are known to be present in our country, and more than 500 species are toxic and contain lethal mycotoxins responsible for different types of clinical syndromes.[2] Delayed liver toxicity and delayed gastroenteritis caused by amatoxin and phyllotoxin found in the Amanita, Lepiota, and Galerina species of mushrooms accounts for up to 30% mortality. Seizures, delayed gastroenteritis and liver toxicity caused by gyromitrin found in the Gyromitra species, Sarcosphaera species and Cyathipodia species accounts for up to 10% mortality. Delayed rhabdomyolysis and delayed encephalopathy with renal failure caused by unknown toxin accounts for up to 25% and 27% of mortality respectively.[11] Early and aggressive management of such poisoning have shown to reduced mortality significantly.
In the recent literature the new syndrome classification has also been given by White et al.[14] where he classified the syndromes into 6 groups based on their cytotoxic, neurological, myotoxic, gastrointestinal, metabolic and other miscellaneous adverse effects. Compared to the old classification new mushroom species were identified like the Russula species causing rhabdomyolysis, polyporic acid containing mushroom, Morchella spp causing morel neurologic syndrome, Trogia venenat a inducing hypoglycemia, Boletussatanas resulting in hyperprocalcitoninemia mushroom poisoning. Pancytopenic mushroom poisoning caused by Ganoderma neojaponicum and Paxillus syndrome induced by Paxillus involutus has also been added to the new classification which was not described by Goldfrank.
In our study observation, our diagnosis was based also based on the presentation of clinical syndrome. The fatal cases of mushroom poisoning were associated with delayed liver toxicity and delayed gastroenteritis syndrome probably caused by liver toxins (amatoxins and phyllotoxin) found in the Amanita, Lepiota, and Galerina species of mushrooms. Younger age groups are affected more maybe because they unknowingly pick up and consume poisonous mushrooms as compared to the elderly subjects who have ancestral knowledge about the types of poisonous mushrooms. All the 17 cases had severe hepatitis with complications of bleeding and encephalopathy. The case fatality rate was as high as 58%, indicating that patients with the associated syndrome are at a higher risk of death and hence should be managed with utmost caution. We also noted the presence of other syndromes which are however not fatal and requires more of supportive therapy. Based on the classification provided by Goldfrank et al.[11] and Brent and Palmer.[11,13] the anticipated toxins and mushrooms responsible for these clinical syndrome caused by poisoning are given below [Table 4]. The clinical presentation of mushroom poisoning help in anticipating whether the mushroom consume d are poisonous and life threatening.[12,14] To date, cases of mushroom poisoning in India have been reported in case reports, and fatal cases have been observed more often in tropical belts of the country (Eastern Ghats, Western Ghat, Himalayan Belt and Northeast India, Kerela) that favor the growth of different mushroom species.[2,3,5,6,7,8] Most case reports were diagnosed from the clinical history and presentation because mushroom identification by an expert mycologist is not always available and toxin analysis is also not routinely performed.[15,16,17,18,19] A case series described by Verma et al. showed three cases of mushroom poisoning which was complicated with acute liver failure and multiorgan dysfuntion syndrome and death in all the three cases.[3] In Assam similar cases has been reported where mortality was observed more among those patients who presented late with liver failure.[5] A detailed study was also carried out by M Kumar et al.[2] in the Kolli Hills of South India where they found the presence of few poisonous species namely Omphalotus olevascens and Mycena pura causing cholinergic syndrome and gastrointestinal syndrome, and Chlorophyllum molybdites resulting in gastrointesitinal symptoms. Toxin analysis study was also carried out in Mysore by S. Sai Latha et al.[8] where they documented the presence of poisonous mushroom namely the Amanita angustilamellata, Agaricus endoxanthus, Clarkeinda trachodes, Chlorophyllum molybdites, Psilocybe subcubensis, Entoloma crissum. In Kerela cases of gastrointesitinal syndrome cause by the Chlorophyllum molybdites species are also encountered from time to time.[7] The poisonous mushroom species like the Amanita, Galerina, and Lepiota are known to contain two main groups of toxins, i.e., amatoxins and phallotoxins.[20] Amanitin is the chief component of the toxins, and - a b amanitin is responsible for the toxic effects. The lethal dose (LD50) of amanitin or alpha- amatoxin can be as low as 0.4- 0.8 mg/kg in humans, which corresponds to approximately two mushroom caps. A single mushroom contains 10 mg of the toxin, which is sufficient to cause mortality.[13,15] When it reaches the portal circulation after absorption from the gastrointestinal tract, it is actively transported by hepatocyte membrane proteins [organic anion transporting polypeptide (OATP)] and sodium taurocholate cotrans porter (NTCP), which facilitates the concentration of toxins inside hepatocytes. Amatoxins then bind to DNA-dependent RNA polymerase type II and prevent protein synthesis, which results in apoptosis and centrilobular necrosis of liver cells.[20] Extensive liver damage results in fulminant hepatitis, which accounts for the high mortality. Mortality in our cohort of patients is those with delayed onset of hepatitis presenting late to the hospital. Thus, hepatitis and late presentation are important prognostic factors to the outcome of mushroom poisoning. The specific tests for toxins in the serum include reversed- phase high-performance liquid chromatography, capillary electrophoresis coupled with mass spectrometry, and liquid chromatography coupled to mass spectrometry or tandem mass spectrometry. Toxins in the urine can be estimated by enzyme- linked immunosorbent assay (ELISA), radioimmunoassay, and high- performance light chromatography. However, these tests are limited and not easily available.[21,22,23]
Table 4.
Clinical Syndrome and the likely toxins and mushrooms causing the poisoning based on the symptoms
| Clinical Syndrome | Number of patients | Possible toxins | Mushrooms containing the toxins |
|---|---|---|---|
| Delayed liver toxicity and delayed gastroenteritis | 17 | Amatoxins | Amanita spp. |
| Phallotoxins | Lepiota spp. | ||
| Galerina marginata | |||
| Acute gastroenteritis | 19 | Gi irritants | Chlorophyllum molybdites spp. |
| Disulfiram like reaction | 1 | Coprine | Coprinopsis atramentaria |
| Cholinergic mushroom poisoning | 5 | Muscarine | Clitocybe cerussata |
| Citocybe dealbata | |||
| Inocybe fibrosa | |||
| Inocybe geophylla | |||
| Inocybe fastigiata/rimosa | |||
| Acute Kidney injury | 1 | Orellanine, orellinine, cortinarin | Orellani spp. |
| Allenic norleucine | Amanita smithiana | ||
| Headache | 1 | Unknown | - |
Management in our patients with suspected amatoxin- induced liver toxicity is mainly supportive, with few patients receiving silibinin and ceftazidime injections [Table 5]. In fulminant hepatitis cases, ultrasonography- guided biliary aspiration was performed in 5 patients to decrease the enterohepatic circulation; however, only three patients survived.[24,25] Some patients also received octreotide injection, as proposed in some observational studies, which reduced the release of toxins from the gall bladder to the enterohepatic circulation.[26] The use of supposed antidotes (amatoxin uptake inhibitors), silymarin, penicillin G, silibinin, and ceftazidime is still controversial. However, silibinin dihemisuccinate is an accepted d antidote in European n countries.[27] In the USA, the drug silibinin hemisuccinate was studied in an observational study by Mengs U et al.,[28] who showed that it led to a 10% reduction in mortality compared to other antidotes. The drug acts by blocking member an e transport receptors [(organic anion transporting polypeptide (OATP) 1b3 and sodium taurocholate cotrans porter (NTCP)], which diverts the amatoxin back into the general circulation for renal clearance. For other antioxidants, such as N-acetylcysteine (NAC), vitamin C has yet to be proven to be effective. In the recent systemic review carried out by Jiaming Liu et al.[29] showed the effectiveness of NAC treatment when combined with other therapies in patients with amatoxin poisoning. Other observational studies of Amanita poisoning with acute liver failure, liver transplantation has been the last resort for treatment.[30,31] With time other bridging therapies for fulminant hepatitis, such as the molecular absorbent recirculating system (MARS), fractionate d plasma separation and adsorption system (FPSA), or plasma exchange, have also been mentioned in a few case reports and observational studies.[32,33,34,35] Recent studies have also shown significant reduction in mortality among fulminant hepatitis patients based on early aggressive hydration therapy of 4 L over 24 h and administration of antioxidant N-acetyl cysteine with the continuation of supportive therapy compared to cohorts of older patients who did not receive such treatment.[36,37] We also noted that climate plays an important role in the growth of these wild poisonous mushrooms. Rainfall, temperature, and humidity are the factors influencing the growth of wild mushrooms, as shown in Figure 5. The variety of tree species and climatic factors in our state favors the presence of the ectomycorrhizal fungi, indicating that it is an endemic zone for such species. The wild mushrooms (Amanita, Lepiota and Galerina species) are ectomycorrhizal fungi growing in mixed deciduous and coniferous forests, with an average temperature of 23-24°C, relative humidity of >80%, and rainfall of >200 mm which thrive in the woods and are easily available for collection.[38] Hence, awareness of the existence of such wild poisonous mushrooms is important.
Table 5.
Management and Outcome of patients
| Clinical syndromes | Total no of patients | Management | ICU care | Mechanical ventilation | Death |
|---|---|---|---|---|---|
| Delayed liver toxicity and delayed gastroenteritis | 17 | Supportive therapy | 17 | 10 | 10 |
| IV fluids | |||||
| Vitamin K | |||||
| Fresh frozen plasma | |||||
| US guided gall bladder aspiration | |||||
| Octreotride infusion | |||||
| Antidote : silibilin/ceftazidime | |||||
| Acute gastroenteritis | 19 | Supportive therapy | None | None | None |
| IV fluids | |||||
| Proton pump inhibitors | |||||
| Antiemetic | |||||
| Cholinergic mushroom poisoning | 5 | Supportive therapy : Hydration therapy | None | None | None |
| Acute kidney injury | 1 | Hydration therapy and hemodialysis | None | None | None |
| Disulfram type of reaction | 1 | Supportive therapy | None | None | None |
| Headache | 1 | Supportive therapy | None | None | None |
Figure 5.
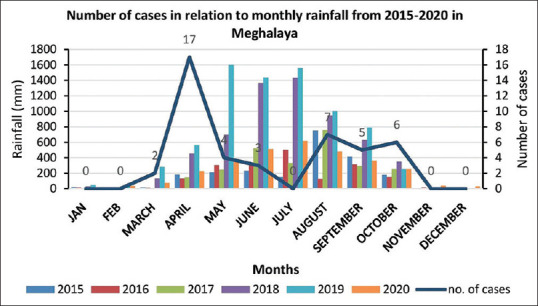
Number of cases in relation to rainfall
Mushroom poisoning is encountered in the peripheral areas where the only means of first aid is from peripheral health centers where medical officers are the first to encounter such cases. At the same time early medical intervention as mention in discussion which can easily be carried out at the peripheral health centers decreased mortality and organ failure as evidenced from the literature mention in the discussion part. Hence we feel that primary care physicians can play a big role in saving lives of patients with fatal mushroom poisoning at the right time.
The limitations of our study are as follows. First, this was a retrospective study. Second, specific diagnostic tests were not available, and toxin analyses of the patient’s urine and blood could not be perform ed. Third, the syndrome diagnosis was based on the patient’s history and clinical presentation. Finally, the number of mushroom poisoning cases is also low, which increases the difficulty of showing the significance of the clinical features in the outcomes of the patients.
Conclusion
Our study observed some wild mushrooms are edible and some are not. Delayed liver toxicity and delayed gastroenteritis lead to the highest number of fatalities among wild mushrooms. Climatic factors (temperature, rainfall, and humidity) are known to favor the growth of wild poisonous mushrooms. Unless proven, all late- presenting cases of mushroom poisoning with hepatitis should be considered amatoxin- induced poisoning which is fatal. Immediate resuscitative and aggressive therapy should be considered to prevent organ damage. The early spring, rainy season, and autumn are the anticipated times of such cases. Awareness about the existence of such mushrooms in this part of our country should be promoted to prevent the occurrence of death from mushroom poisoning.
Key messages and recommendation
Mushroom poisoning is the present era is not uncommon and if caused by the amatoxin accounts for high mortality as observed in our study and other studies as well.
With recent evidences early and aggressive medical therapy can reduced mortality
Diagnosis can be made by recognition of the clinical syndrome which can be made even bedside from proper history and examination with certain laboratory parameters even if toxin analysis is not available.
Antidotes and antioxidants for mushroom poisoning have a role in the treatment of mushroom poisoning
This study shows that late presentation of amatoxin induced poisoning accounts for high mortality
Some medical therapeutic intervention like gall bladder aspiration which decreases the enterohepatic circulation of the toxins seemed to have been effective for some of our patients but requires more studies to be conducted.
This observation study shows that treatment for lethal mushroom poisoning is still a grey area which need more RCT for certain ANTIDOTES to have stronger evidence and recommendation for their use.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Erden A, Esmeray K, Karagöz H, Karahan S, Gümüşçü HH, Başak M, et al. Acute liver failure caused by mushroom poisoning: A case report and review of the literature. Int Med Case Rep J. 2013;6:85–90. doi: 10.2147/IMCRJ.S53773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar M, Kaviyarasan V. Few common poisonous mushrooms of Kolli hills, South India. Mycotaxon. 1976;3:363. [Google Scholar]
- 3.Verma N, Bhalla A, Kumar S, Dhiman RK, Chawla YK. Wild mushroom poisoning in north India: Case series with review of literature. J Clin Exp Hepatol. 2014;4:361–5. doi: 10.1016/j.jceh.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.West PL, Lindgren J, Horowitz BZ. Amanita Smithiana mushroom ingestion: A case of delayed renal failure and literature review. J Med Toxicol. 2009;5:32–8. doi: 10.1007/BF03160979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dutta A, Kalita BC, Pegu AK. A study of clinical profile and treatment outcome of mushroom poisoning – A hospital- based study. Assam J Int Med. 2013;3:13–7. [Google Scholar]
- 6.Barman B, Warjri S, Lynrah KG, Phukan P, Mitchell ST. Amanita nephrotoxic syndrome: Presumptive first case report on the Indian subcontinent. Indian J Nephrol. 2018;28:170–2. doi: 10.4103/ijn.IJN_353_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bijeesh C, Vrinda KB, Pradeep CK. Mushroom poisoning by Chlorophyllum molybdites in Kerala. J Mycopathol Res. 2017;54:477–83. [Google Scholar]
- 8.Sai Latha S, Naveen S, Pradeep CK, Sivaraj C, Dinesh MG, Anilakumar KR. Toxicity assessment of wild mushrooms from the Western Ghats, India: An in vitro and sub-acute in vivo study. Front Pharmacol. 2018;9:90. doi: 10.3389/fphar.2018.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keller SA, Klukowska-Rötzler J, Schenk-Jaeger KM, Kupferschmidt H, Exadaktylos AK, Lehmann B, et al. Mushroom poisoning- A 17 year retrospective study at a level I University Emergency Department in Switzerland. Int J Environ Res Public Health. 2018;15:2855. doi: 10.3390/ijerph15122855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan CK, Lam HC, Chiu SW, Tse ML, Lau FL. Mushroom poisoning in Hong Kong: A ten- year review. Hong Kong Med J. 2016;22:124–30. doi: 10.12809/hkmj154706. [DOI] [PubMed] [Google Scholar]
- 11.Goldfrank LR, Nelson LS, Lewin NA, Howland MA, Hoffman RS. Goldfrank's Toxicologic Emergencies. 9th ed. New York: McGraw-Hill Medical; 2011. [Google Scholar]
- 12.Brent J, Palmer RB. Mushrooms. In: Shannon MW, Borron SW, Burns MJ, editors. Haddad and Winchester's Clinical Management of Poisoning and Drug Overdose. 4th ed. Philadelphia, PA: Saunders Elsevier; 2007. p. 455. [Google Scholar]
- 13.Vetter J. Toxins of Amanita phalloides. Toxicon. 1998;36:13–24. doi: 10.1016/s0041-0101(97)00074-3. [DOI] [PubMed] [Google Scholar]
- 14.White J, Weinstein SA, De Haro L, Bédry R, Schaper A, Rumack BH, et al. Mushroom poisoning: A proposed new clinical classification. Toxicon. 2019;157:53–65. doi: 10.1016/j.toxicon.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Yilmaz I, Ermis F, Akata I, Kaya E. A case study: What doses of Amanita phalloides and amatoxins are lethal to humans? Wilderness Environ Med. 2015;26:491–6. doi: 10.1016/j.wem.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Trakulsrichai S, Sriapha C, Tongpoo A, Udomsubpayakul U, Wongvisavakorn S, Srisuma S, et al. Clinical characteristics and outcome of toxicity from Amanita mushroom poisoning. Int J Gen Med. 2017;10:39–400. doi: 10.2147/IJGM.S141111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wennig R, Eyer F, Schaper A, Zilker T, Andresen-Streichert H. Mushroom poisoning. Dtsch Arztebl Int. 2020;117:701–8. doi: 10.3238/arztebl.2020.0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berger KJ, Guss DA. Mycotoxins revisited: Part I. J Emerg Med. 2005;28:53–62. doi: 10.1016/j.jemermed.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 19.Diaz JH. Syndromic diagnosis and management of confirmed mushroom poisonings. Crit Care Med. 2005;33:427–36. doi: 10.1097/01.ccm.0000153531.69448.49. [DOI] [PubMed] [Google Scholar]
- 20.Garcia J, Costa VM, Carvalho A, Baptista P, de Pinho PG, de Lourdes Bastos M, et al. Amanita phalloides poisoning: Mechanisms of toxicity and treatment. Food Chem Toxicol. 2015;86:41–55. doi: 10.1016/j.fct.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Horgen PA, Vaisius AC, Ammirati JF. The insensitivity of mushroom nuclear RNA polymerase activity to inhibition by amatoxins. Arch Microbiol. 1978;118:317–9. doi: 10.1007/BF00429124. [DOI] [PubMed] [Google Scholar]
- 22.Parant F, Peltier L, Lardet G, Pulce C, Descotes J, Moulsma M. Phalloidin syndrome: Role of Elisa- based assay for the detection of alpha- and gamma- amanitins in urine. Preliminary results. Acta Clin Belg. 2006;61(Suppl 1):11–7. doi: 10.1179/acb.2006.063. [DOI] [PubMed] [Google Scholar]
- 23.Butera R, Locatelli C, Coccini T, Manzo L. Diagnostic accuracy of urinary amanitin in suspected mushroom poisoning: A pilot study. J Toxicol Clin Toxicol. 2004;42:901–12. doi: 10.1081/clt-200035472. [DOI] [PubMed] [Google Scholar]
- 24.Frank IC, Cummins L. Amanita poisoning treated with endoscopic biliary diversion. J Emerg Nurs. 1987;13:132–6. [PubMed] [Google Scholar]
- 25.Sun J, Zhang YT, Niu YM, Li HJ, Yin Y, Zhang YZ, et al. Effect of Biliary drainage on the toxicity and toxicokinetics of amanita exitialis in beagles. Toxins (Basel) 2018;10:215. doi: 10.3390/toxins10060215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vo KT, Montgomery ME, Mitchell ST, Scheerlinck PH, Colby DK, Meier KH, et al. Amanita phalloides mushroom poisonings-Northern California, December 2016. MMWR Morb Mortal Wkly Rep. 2017;66:549–53. doi: 10.15585/mmwr.mm6621a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganzert M, Felgenhauer N, Schuster T, Eyer F, Gourdin C, Zilker T. Amanita poisoning- -comparison of silibinin with a combination of silibinin and penicillin. Dtsch Med Wochenschr. 2008;133:2261–7. doi: 10.1055/s-0028-1091268. [DOI] [PubMed] [Google Scholar]
- 28.Mengs U, Pohl RT, Mitchell T. Legalon Ò SIL: The antidote of choice in patients with acute hepatotoxicity from amatoxin poisoning. Curr Pharm Biotechnol. 2012;13:1964–70. doi: 10.2174/138920112802273353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu J, Chen Y, Gao Y, Walline JH, Lu X, Yu S, et al. N- acetylcysteine as a treatment for amatoxin poisoning: A systematic review. Clin Toxicol. 2020;58:1015–22. doi: 10.1080/15563650.2020.1784428. [DOI] [PubMed] [Google Scholar]
- 30.Enjalbert F, Rapior S, Nouguier-Soulé J, Guillon S, Amouroux N, Cabot C. Treatment of amatoxin poisoning: 20- year retrospective analysis. J Toxicol Clin Toxicol. 2002;40:715–57. doi: 10.1081/clt-120014646. [DOI] [PubMed] [Google Scholar]
- 31.Kim YJ, Lee HJ, Ryoo SM, Ahn S, Sohn CH, Seo DW, et al. Prognostic value of decision criteria for emergency liver transplantation in patients with wild mushroom induced acute liver injury. Hepatobiliary Pancreat Dis Int. 2018;17:210–3. doi: 10.1016/j.hbpd.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 32.Karvellas CJ, Tillman H, Leung AA, Lee WM, Schilsky ML, Hameed B, et al. Acute liver injury and acute liver failure from mushroom poisoning in North America. Liver Int. 2016;36:1043–50. doi: 10.1111/liv.13080. [DOI] [PubMed] [Google Scholar]
- 33.Bergis D, Friedrich- Rust M, Zeuzem S, Betz C, Sarrazin C, Bojunga J. Treatment of Amanita phalloides intoxication by fractionated plasma separation and adsorption (Prometheus Ò) J Gastrointest Liver Dis. 2012;21:171–6. [PubMed] [Google Scholar]
- 34.Shi Y, He J, Chen S, Zhang L, Yang X, Wang Z, et al. MARS: Optimistic therapy method in fulminant hepatic failure secondary to cytotoxic mushroom poisoning- -A case report. Liver. 2002;22(Suppl 2):78–80. doi: 10.1034/j.1600-0676.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- 35.Covic A, Goldsmith DJ, Gusbeth- Tatomir P, Volovat C, Dimitriu AG, Cristogel F, et al. Successful use of molecular absorbent regenerating system (MARS) dialysis for the treatment of fulminant hepatic failure in children accident ally poisoned by toxic mushroom ingestion. Liver Int. 2003;23(Suppl 3):21–7. doi: 10.1034/j.1478-3231.23.s.3.9.x. [DOI] [PubMed] [Google Scholar]
- 36.Dutta A, Das AK, Pegu AK, Kalita BC. Early hydration therapy in mushroom poisoning improves mortality and morbidity. J Indian Soc Toxicol. 2018;14:22–7. [Google Scholar]
- 37.Jongthun R, Hemachudha P, Wacharapluesadee S, Hemachudha T. Low-cost management of mushroom poisoning in a limited-resource area: A 12-year retrospective study. Trop Doct. 2020;50:135–8. doi: 10.1177/0049475519897704. [DOI] [PubMed] [Google Scholar]
- 38.Jang SK, Hur TC. Relationship between climatic factors and the distribution of higher fungi in Byeonsanbando National Park, Korea. Mycobiology. 2014;42:27–33. doi: 10.5941/MYCO.2014.42.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]


