ABSTRACT
Background:
Trauma is a leading cause of morbidity and mortality in both developed and developing countries.
Methodology:
This retrospective observational study was done in the Emergency Department (ED) of a tertiary care trauma center in Southern India in 2018 (January to December).
Results:
During the study period of 1 year, the ED attended 74,466 patients which included 7675 (10.3%) trauma patients. The mean age was 35.3 (SD: 18.5) years with three-fourth (76.6%) being males. Pediatric/adolescents (age ≤18 years) and geriatric age groups (age ≥60 years) comprised 16.7% and 11.8% cases, respectively. Road traffic accidents (RTA) (66%) were the predominant mode of injury followed by falls (fall from height: 8.6% and fall on level ground: 7.8%). Among the RTAs, the majority were two-wheelers related (73.8%), followed by pedestrian injuries (9.4%) and four-wheelers injuries (7.2%). Bivariate and multivariate logistic regression analysis showed pedestrian injuries, low Glasgow Coma Scale (GCS), and hypotension at arrival as independent predictors of hospital mortality. The in-hospital mortality rate was 0.7%. A quarter (24%; n = 1841) of the patient’s population was solely managed by the ED team and discharged stable, while 2179 (28.4%) victims required hospital admission.
Conclusion:
Trauma is a major cause of mortality especially among the breadwinners of families in India with almost half being due to two-wheeler accidents. Efficient ED professionals and a multispecialty team of trauma surgeons, neurosurgeons, and orthopedics handle the major load of acute trauma. Pedestrian injuries, low GCS, and hypotension at arrival are independent predictors of in-hospital mortality.
Keywords: Accidents, emergency department, profile of trauma, road traffic accidents, trauma
Introduction
Trauma is a leading cause of morbidity and mortality in both developed and developing countries. In the Indian subcontinent, trauma is a major killer contributing to the majority of deaths mainly due to road traffic accidents (RTA).[1] The World Health Organization (WHO) reports that the global mortality due to RTA has plateaued at 1.25 million a year.[2] In India, trauma accounts for more than a third of unnatural causes of death, and the country loses 2% to 3% of its gross domestic product annually amounting to 7.2 billion dollars.[3,4,5] Hence, Emergency departments (EDs) and trauma centers across the length and breadth of the country must be well equipped and well resourced to efficiently handle the ever-increasing load of trauma.
In a developing country like India, there has been a significant improvement in the roads and highway infrastructure in addition to the rapid urbanization and motorization in the last few decades. These developments have precipitated an alarming increase in the incidence of RTAs. India is estimated to have 11% of the global automobile accidents despite having 1% of the motorized vehicles of the world.[6,7] According to a report by the World Bank, the country accounts for about 4.5 lakh road crashes per annum, in which 1.5 lakh people die.[6] The “golden hour” of trauma, wherein primary assessment and secondary survey are performed by the first responders and life-saving interventions are initiated, is extremely crucial in decreasing morbidity and mortality which would lead to a significant impact on Disability-Adjusted Life Years. Therefore, the clinical assessment of trauma in primary care medicine has become a central issue.
We conducted this retrospective study to understand the magnitude and impact of trauma, mechanism of injury, the severity of injuries, monthly pattern, and outcome of patients. Accidents cannot be avoided but can be prevented. With this study, we hoped to have a better understanding of patient load on each department involved in a trauma care center and to identify the predictors of mortality.
Methods
We conducted this retrospective cross-sectional study in the ED of a large tertiary care referral hospital in India. Our ED attends to approximately 75,000 emergency visits annually including trauma and non-trauma patients. All patients (pediatric and adult) presenting with various modes of trauma (RTA, fall on level ground or from height, occupational injuries and injuries caused by animals, sports, and assault) were included in the study. Brought dead patients following trauma and those with incomplete chart documentation and missing records were excluded from the study. Since we aimed to study the seasonal variation concerning the modes of injuries, we included all trauma victims presenting to ED over 1 year (January to December 2018).
Data were collected from the hospital’s electronic database (Clinical workstation) and documented in a standard extraction datasheet. The following were extracted: demographic characteristics, mode of trauma, time of the incident, vital signs at arrival, triage priority level, and outcome. Standard Canadian triaging criteria was used to determine the physiological severity at admission. Triage priority I, included patients those who required immediate attention with life-threatening emergencies like compromised airway, irregular breathing, circulatory compromise, or those with a severe head injury as determined by Glasgow Coma Scale (GCS) ≤8. Triage priority II patients include those with no airway/breathing/circulatory compromise and triage priority III patients were those with minor trauma and did not require ED admission. After performing the initial assessment, relevant radiological imaging was done to determine the extent of internal injuries. The outcome measures were the spectrum of injuries, the monthly pattern of trauma, and ED and hospital outcomes.
Software used
Statistical Package for the Social Sciences for Windows software released in 2015, version 23.0, Armonk, New York, USA. Mean and standard deviation was used for continuous variables and percentages for nominal variables. We used multivariate logistic regression analysis to correlate factors influencing mortality.
Ethical considerations
Approval was obtained from the Institution Review board (IRB) prior to commencement of study (IRB Min no: 12222 dated 22nd August 2019).
Results
During the study period of 1 year (1st January to 31st December 2018), our ED attended 74,466 patients of whom 7675 (10.3%) were trauma victims. Charts were not scanned for 6 patients and 8 of these victims were brought dead to ED, and therefore, the final cohort comprised 7661 (10.3%) patients [Figure 1].
Figure 1.
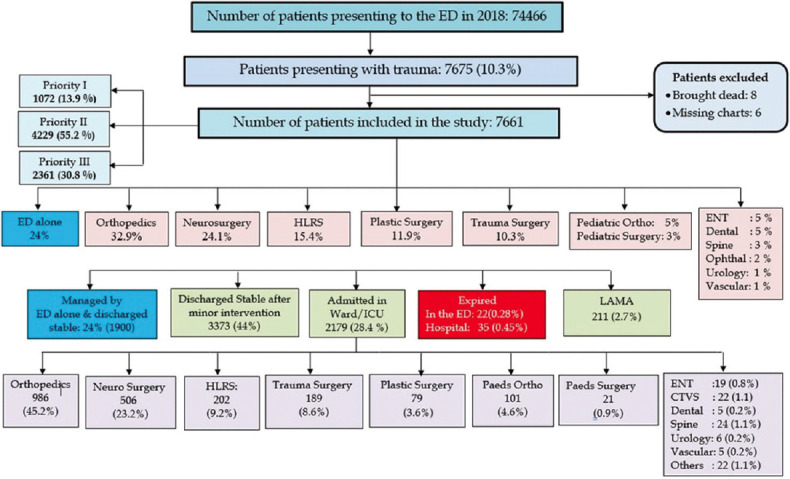
STROBE diagram
Demography
The mean age of the patients was 35.3 (SD: 18.5) years and ranged from 0 to 87 years. Male predominance was observed in 5884 (76.8%) victims. Most of the victims, that is, 5472 (71.5%) were from the middle-aged group (18 to 59 years), whereas pediatric/adolescents (age ≤18 years) and geriatric age groups (age ≥60 years) comprised 1284 (16.7%) and 905 (11.8%) cases, respectively [Table 1]. Triage priority I patients comprised 1071 (14%) victims, while the majority, that is, 4229 (55.2%) victims were triaged as priority II followed by 2361 (30.8%) victims as priority III [Figure 1].
Table 1.
Baseline characteristics (n=7661)
| Characteristics | Number (%) |
|---|---|
| Age, mean (SD), years | 35.3 (18.5) |
| Time of Incident | |
| 8 am - 5 pm | 3654 (47.7%) |
| 5 pm - 12 am | 2819 (36.8%) |
| 12 am - 8 am | 1188 (15.5%) |
| Sex ratio | |
| Male | 5884 (76.8%) |
| Female | 1777 (23.2%) |
| Age group | |
| Pediatric and adolescent trauma (≤18 years) | 1284 (16.7%) |
| Adult trauma (18-59 years) | 5472 (71.5%) |
| Geriatric trauma (≥60 years) | 905 (11.8%) |
Mode of injury
We noticed that RTAs were the most common mechanism of incidence 5049 (65.9%), followed by fall from height 657 (8.6%) and fall on level ground 596 (7.8%). The mode of other injuries is shown in Figure 2. Among the patients with RTAs, 3725 (73.8%) victims were either driving motorized two-wheeled vehicles or were pillion riders. Other modes of RTAs involving 4-wheeler were 366 (7.3%), motorized 3-wheeler was 145 (2.9%), other vehicles (bus, lorry, and van) were 145 (2.9%), and pedestrians getting hit by any vehicle were 473 (9.4%) patients.
Figure 2.
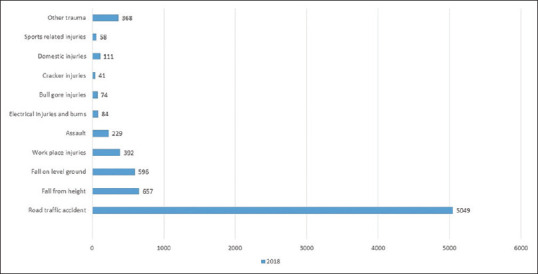
Modes of injury
Monthly variation of incidents
We noted that there was no significant peak in the incidences of RTAs in any given month. The mean incidence of RTAs was 638.4 (SD: 51.6) per month. The average monthly rainfall for Vellore city was obtained from the meteorological database and the trend was plotted against the number of traumas with a special focus on RTAs secondary to motorized 2-wheelers and fall on the ground level. The maximum rainfall was noted in June (1143 mm) and July (1335 mm). Therefore, a peak in the incidences of slip and fall on the ground were noted in these months [Figure 3].
Figure 3.
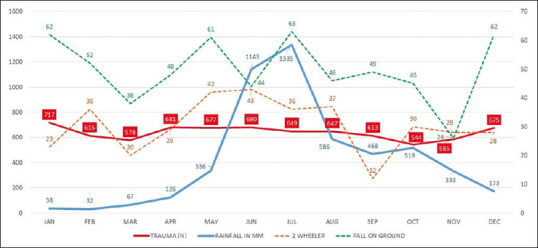
Month-wise distribution of trauma
Time and day of ED presentation
The number of trauma victims presenting between 8 am to 5 pm and 5 pm to 12 am were 3654 (47.7%) and 2819 (36.8%), respectively. As expected, the number of incidences were higher at the weekends [mean 23.85 (SD: 6.11)] than on the weekdays [mean 19.85 (SD: 5.50)]. We found no significant difference in the mean number of patients per day presenting on weekdays and weekends [Table 2].
Table 2.
Bivariate and multivariate logistic regression analysis for factors associated with in-hospital mortality among triage priority I and II trauma patients
| Variables | Died in hospital (n=59) | Discharged alive (n=5241) | P | Unadjusted odds ratio | P | Adjusted odds ratio |
|---|---|---|---|---|---|---|
| Male | 48 (81.4%) | 4086 (78.0%) | 0.53 | 1.23 (0.64-2.38) | - | - |
| Age ≤18 years | 1 (1.7%) | 771 (14.7%) | 0.005 | 0.10 (0.01-0.72) | 0.005 | 0.06 (0.01-0.42) |
| Age >60 years | 12 (20.3%) | 665 (12.7%) | 0.08 | 1.76 (0.93-3.33) | - | - |
| GCS! ≤8 | 37 (62.7%) | 340 (6.5%) | 0.000 | 24.24 (14.14-41.56) | <0.05 | 3.92 (1.99-7.74) |
| SBP# <90 mm Hg | 47 (79.7%) | 501 (9.6%) | 0.000 | 37.06 (19.53-70.32) | <0.05 | 26.88 (12.26-58.95) |
| RTA$ vs Others | 52 (88.1%) | 3709 (70.8%) | 0.003 | 3.07 (1.39-6.77) | 0.23 | 1.68 (0.72-3.88) |
| Pedestrian | 10 (16.9%) | 362 (6.9%) | 0.003 | 2.75 (1.38-5.48) | 0.02 | 2.48 (1.14-5.42) |
| Two-wheeler | 29 (49.2%) | 2814 (53.7%) | 0.48 | 0.83 (0.50-1.39) | - | - |
| Four-wheeler | 5 (8.5%) | 265 (5.1%) | 0.23 | 1.74 (0.69-4.38) | - | - |
| Weekend (Saturday, Sunday) | 16 (0.6%) | 2465 (99.4%) | 0.38 | 0.78 (0.44-1.38) | - | - |
| 12 AM - 8 AM | 9 (0.7%) | 1260 (99.3%) | 0.78 | 0.91 (0.44-1.85) | - | - |
GCS!: Glasgow Coma Scale; SBP#: Systolic blood pressure; RTA$: Road traffic accident
Predictors of in-hospital mortality among priority I and II patients
Multiple logistic regression analysis done to study factors related to in-hospital mortality among priority I and II patients between various indices are given in Table 2. Patients presenting to ED with low GCS (≤8) [Adjusted OR: 4.18 (2.13-8.21); P value: <0.001], hypotension (Systolic BP ≤90 mmHg) [Adjusted OR: 26.95 (12.27–59.19); P value: <0.001], and pedestrian injuries [Adjusted OR: 2.74 (1.27–5.93); P value: 0.01] were the independent risk factors associated with high in-hospital mortality.
Management, ED, and hospital outcome
A quarter of 1841 (24%) of the trauma victims were managed by the ED team alone. Trauma patients were referred to the concerned surgical specialties for further management if needed after early resuscitation. Orthopedics 2521 (32.9%), Neurosurgery 1847 (24.1%), Plastic Surgery 912 (11.9%), and Hand Surgery 1180 (15.4%) were the main units involved in the ED management of patients [Figure 1]. About half of the study population, that is, 3373 (44%) patients, were discharged stable after minor intervention in the ED by the specialty units. Among the total study population, 22 (0.3%) succumbed to the illness in the ED during resuscitation and 35 (0.5%) victims during their hospital stay [Figure 4].
Figure 4.
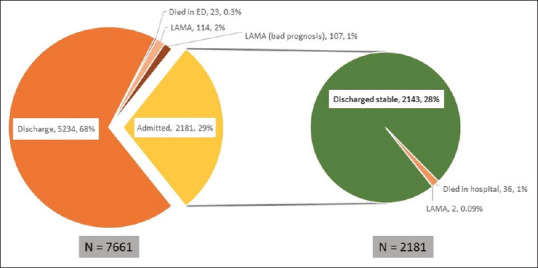
ED and hospital outcome
Discussion
Trauma is a common presentation in the ED across the globe leading to permanent disability, financial burden on society, and even death. Our study focused on the spectrum of trauma to determine the different modes of injury, monthly patterns of trauma, the proportion of patients managed by each department in the ED, and hospital mortality. Understanding the spectrum of trauma described in our study helps the ED to be better prepared in handling acute trauma. The proportion of trauma victims in our ED, during the study period, was found to be 10.3%. The young and productive mean age (35.3 years) of our cohort with male predominance (76.6%) involving the potential bread earner of the families is an alarming factor.
In our cohort, majority of the victims presented with RTA secondary to driving motorized two-wheeled vehicles or were pillion riders. According to WHO, RTAs are expected to account for almost half a million deaths in India by 2020 due to rapid socioeconomic growth and urbanization.[6,7,8] Primary and secondary level health centers in India lack certain vital facilities like a blood bank, advanced radiological imaging (computed tomography), and equipped surgical theaters for evaluation and treatment of severe trauma, thereby necessitating referral of these patients to higher centers of care. An underdeveloped and ill-equipped pre-hospital care system in India further compounds this problem, resulting in an increased number of deaths during the critical “Golden Hour” of trauma.[9,10,11,12]
Two-wheeler users and pedestrians are at higher risk than other vehicular occupants in an RTA. In developed countries, mortality rates due to RTA have decreased due to enforcement of laws against speed limits, use of helmets, and enforcing strong drink-driving laws.[13] However, low- and middle-income nations have the vast majority (93%) of the world’s road fatalities, despite having only 60% of the vehicles in the world.[14] In our study population, 59 victims, that is, 0.7% of all trauma cases and 1.1% of triage priority I and II cases succumbed to the cause. Triage priority III patients were excluded from the logistic analysis because of trivial trauma.
Given the pattern of injuries seen in this set of people, we expected a significant rise in incidences of slip and fall and two-wheeler-related accidents during the rainy season.[15] There was a peak noted among the slip and fall cases in July which corresponds to the maximum rainfall in our locality. On the contrary, there was no obvious peak of two-wheeler-related accidents during the rainy season. The total number of trauma patients not showing any significant variance in each month can be explained by the fact that ours is a tertiary care referral center that receives patients throughout the year to its maximum capacity.
Our study demonstrated no substantial increase in the average number of trauma patients during weekends, as seen in other studies done in the West.[16] Many studies have previously looked at the “weekend effect” on trauma, which assumes a worse hospital outcome of trauma victims at the weekends or night. However, the major regional centers of the West have proven this wrong and similar results were observed at our center.[17,18] There was no significant difference between the mortality of trauma victims who presented during weekends or at nighttime.
Understanding the mode of injury and injury patterns associated with mechanisms will help guide the examination and choice of radiologic studies. Patients with open wounds should be given a loading dose of a broad-spectrum antibiotic within 6 h after trauma to reduce the risk of infection.[19,20,21] Multiple logistic regression analysis showed that patients with severe head injury (GCS ≤ 8), circulatory shock, and pedestrian injuries were independent risk factors for in-hospital mortality. According to our analysis, pediatric age group victims have a lower (90%) chance of in-hospital mortality. This could be explained by the fact that the nature of injury among the pediatric age group of this study population was trivial and play related. In addition, it was noted that there was no increased risk of mortality associated with two-wheeler accidents, which was in contrast with previous studies that showed a higher risk of mortality among victims involved in two-wheeler related accidents.[22,23,24]
In our study population, wound wash was performed in most patients after initial workup by the ED registrars. Emergency procedures like suturing or debridement or minor surgical procedures in the ED were done by the concerned specialty doctors. More than half of the patients were discharged stable after performing first aid and minor surgical procedures in the ED. The in-hospital admitted patients were taken up for emergency operations in the theater or needed further evaluation and management. A few patients, that is, 211 (2.7%) patients, were discharged against medical advice or discharged at request to go to other hospitals due to probable poor prognosis or financial constraints. The current Corona Virus Disease 19 (COVID-19) pandemic lockdown restriction imposed in most countries have resulted in a significant reduction in trauma victims with a positive blood alcohol content which perhaps is the silver lining of the ongoing pandemic.[25-27]
Limitations: Our data are from a single tertiary care referral center, hence resulting in selection and referral pattern bias. Nonetheless, our study shows the current spectrum of trauma, departments involved in managing the active load of trauma, and the hospital outcome.
Key points
Trauma is a major cause of mortality, especially in the younger age group with almost half (48.6%) due to two-wheeler-related accidents.
Low GCS, hypotension, and pedestrian injuries are independent predictors of in-hospital mortality among priority I and II patients.
RTA, fall from height, and fall on level ground comprised majority of trauma cases.
Conclusion
Prevention of trauma should be focused on high-risk populations, which according to this data includes young adults and men. RTAs involving motorized two-wheeler are the most common mode injury. Low GCS, hypotension, and pedestrian injuries were independent risk factors associated with hospital mortality in priority I and II patients. There was no difference in hospital outcome based on the day and time of presentation. The trauma team of ED physicians, Orthopaedicians, and Neurosurgeons plays a pivotal role in managing these victims.
Highlights
This is a descriptive study to determine the magnitude and impact of a large cohort of patient’s population presenting to the ED with trauma.
Our study provides a detailed description of the mode of injury in relation to the seasonal pattern in a year.
Research quality and ethics statement
The authors of this manuscript declare that this scientific work complies with reporting quality, formatting, and reproducibility guidelines set forth by the EQUATOR Network. The authors also attest that this clinical investigation was determined to require Institutional Review Board/Ethics Committee review, and the corresponding protocol/approval number is IRB Min no: 12222 dated 22nd August 2019. We also certify that we have not plagiarized the contents in this submission and have done a Plagiarism Check.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Making a difference. The World Health Report 1999. Health Millions. 1999;25:3–5. [PubMed] [Google Scholar]
- 2.Weiss RJ, Montgomery SM, Al Dabbagh Z, Jansson KA. National data of 6409 Swedish in patients with femoral shaft fractures:Stable incidence between 1998 and 2004. Injury. 2009;40:304–8. doi: 10.1016/j.injury.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Gautam D, Hazra D, Nekkanti AC, Abhilash KP. Retrospective study on cost accounting of trauma patients presenting to the emergency department in a tertiary care hospital in South India. Curr Med Issues. 2020;18:14–8. [Google Scholar]
- 4.Abhilash KP, Chakraborthy N, Pandian GR, Dhanawade VS, Bhanu TK, Priya K. Profile of trauma patients in the emergency department of a tertiary care hospital in South India. J Family Med Prim Care. 2016;5:558–63. doi: 10.4103/2249-4863.197279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nantulya VM, Reich MR. Equity dimensions of road traffic injuries in low- and middle-income countries. Inj Control SafPromot. 2003;10:13–20. doi: 10.1076/icsp.10.1.13.14116. [DOI] [PubMed] [Google Scholar]
- 6.India tops the world with 11% of global death in road accidents:World Bank report-The Economic Times. [Last accessed on 2021 Jun 28]. Available from: https://economictimes.indiatimes.com/news/politics-and-nation/india-tops-the-world-with-11-of-global-death-in-road-accidents- world-bank- report/articleshow/80906857. cms?from=mdr .
- 7.Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European guideline on management of major bleeding and coagulopathy following trauma:Fifth edition. Crit Care. 2019;23:98. doi: 10.1186/s13054-019-2347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramanujam P, Aschkenasy M. Identifying the need for pre-hospital and emergency care in the developing world:A case study in Chennai, India. J Assoc Physicians India. 2007;55:491–5. [PubMed] [Google Scholar]
- 9.Abhilash KP, Sivanandan A. Early management of trauma:The golden hour. Curr Med Issues. 2020;18:36–9. [Google Scholar]
- 10.Divya B, Edacheril IG, Jacob M, Abhilash KP. Prospective observational study to assess the circulatory status of the patients presenting to resuscitation room in emergency department. Curr Med Issues. 2020;18:115–9. [Google Scholar]
- 11.Roy N, Murlidhar V, Chowdhury R, Patil SB, Supe PA, Vaishnav PD, et al. Where there are no emergency medical services-prehospital care for the injured in Mumbai, India. Prehosp Disaster Med. 2010;25:145–51. doi: 10.1017/s1049023x00007883. [DOI] [PubMed] [Google Scholar]
- 12.Joshipura MK. Trauma care in India:Current scenario. World J Surg. 2008;32:1613–7. doi: 10.1007/s00268-008-9634-5. [DOI] [PubMed] [Google Scholar]
- 13.The Global impact. [Last accessed on 2021 Jun 28]. Available from: https://www.who.int/violence_injury_prevention/publications/road_traffic/world_report/chapter 2.pdf .
- 14.Road traffic injuries. [Last accessed on 2021 Jun 28]. Available from: https://www.who.int/news-room/fact-sheets/detail/road-traffic-injuries .
- 15.Ali AM, Willett K. What is the effect of the weather on trauma workload?A systematic review of the literature. Injury. 2015;46:945–53. doi: 10.1016/j.injury.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 17.Metcalfe D, Perry DC, Bouamra O, Salim A, Lecky FE, Woodford M, et al. Is there a 'weekend effect'in major trauma? Emerg Med J. 2016;33:836–42. doi: 10.1136/emermed-2016-206049. [DOI] [PubMed] [Google Scholar]
- 18.Carr BG, Reilly PM, Schwab CW, Branas CC, Geiger J, Wiebe DJ. Weekend and night outcomes in a statewide trauma system. Arch Surg. 2011;146:810–7. doi: 10.1001/archsurg.2011.60. [DOI] [PubMed] [Google Scholar]
- 19.Hauser CJ, Adams CA, Jr, Eachempati SR. Council of the surgical infection society. Surgical infection society guideline:Prophylactic antibiotic use in open fractures:An evidence-based guideline. Surg Infect (Larchmt) 2006;7:379–405. doi: 10.1089/sur.2006.7.379. [DOI] [PubMed] [Google Scholar]
- 20.Hoff WS, Bonadies JA, Cachecho R, Dorlac WC. EAST practice managementguidelines update for prophylactic antibiotic use in open fractures. J Trauma. 2011;70:751–4. doi: 10.1097/TA.0b013e31820930e5. [DOI] [PubMed] [Google Scholar]
- 21.A new classification scheme for open fractures. Orthopaedic Trauma Association:Open Fracture Study Group. J Orthop Trauma. 2010;24:457–65. doi: 10.1097/BOT.0b013e3181c7cb6b. [DOI] [PubMed] [Google Scholar]
- 22.Jain A, Menezes RG, Kanchan T, Gagan S, Jain R. Two-wheeler accidents on Indian roads--A study from Mangalore, India. J Forensic Leg Med. 2009;16:130–3. doi: 10.1016/j.jflm.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Gupta A, Jaipuria J, Bagdia A, Kumar S, Sagar S, Misra MC. Motorised two-wheeler crash and helmets:Injury patterns, severity, mortality and the consequence of gender bias. World J Surg. 2014;38:215–21. doi: 10.1007/s00268-013-2230-3. [DOI] [PubMed] [Google Scholar]
- 24.Clement N, Regina DL, Abhilash KP. A retrospective study on the profile and outcome of polytrauma in the emergency department. Curr Med Issues. 2018;16:56–9. [Google Scholar]
- 25.Hazra D, Jindal A, Fernandes JP, Abhilash KP. Impact of the lockdown due to COVID-19 pandemic on the spectrum and outcome of trauma in India. Indian J Crit Care Med. 2021;25:273–8. doi: 10.5005/jp-journals-10071-23758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zsilavecz A, Wain H, Bruce JL, Smith MTD, Bekker W, Laing GL, et al. Trauma patterns during the COVID-19 lockdown in South Africa expose vulnerability of women. S Afr Med J. 2020;110:1110–2. doi: 10.7196/SAMJ.2020.v110i11.15124. [DOI] [PubMed] [Google Scholar]
- 27.Abhilash KPP, Paul AJ, Das S, Hazra D, Jain S, Dhinakar Arelly SP. Changing pattern of trauma during the COVID-19 Pandemic. Med J Armed Forces India. 2021 Jul;77((Suppl 2)):S338–S344. doi: 10.1016/j.mjafi.2021.05.010. doi:10.1016/j.mjafi.2021.05.010. PMID:34334902;PMCID:PMC8313048. [DOI] [PMC free article] [PubMed] [Google Scholar]


