ABSTRACT
Introduction:
Self-medication is the obtainment and consumption of drugs without a physician’s advice, in any stage of disease management. Indiscriminate practice of self-medication, which is common in developing countries like India, often leads to dangerous unwarranted adverse effects, ultimately increasing cost burden due to health care. The aim of this study was to assess self-medication practice and its reasons among study participants.
Methods:
Eligible residents of the urban field practice area of a Kolkata-based medical college were interviewed using a predesigned and pretested data collection schedule.
Results:
Among 170 participants, 98 (57.7%) were found to have practiced self-medication; 39.8% of them were aged between 28 and 37 years, the majority being females (57.1%). Lack of felt need to visit a registered medical practitioner was the most common reason (34.7%) cited behind practicing self-medication. All (100.0%) self-medicating participants checked expiry date before use; pain suppressing medications were the most commonly used (46.9%). Pharmacies were the commonest source of knowledge for medicinal use (64.3%). The less educated tended to self-medicate more than those with a higher level of education (P < 0.05).
Conclusion:
The study found the majority of its respondents to be practicing self-medication. Stringent implementation of law and increasing community awareness regarding the ill effects of self-medication is therefore necessary.
Keywords: Community-based, COVID-19, self-medication, urban, West Bengal
Introduction
Self-medication is the obtainment and consumption of drugs without a physician’s advice.[1] The World Health Organization defines self-medication as “use of pharmaceutical or medicinal products by the consumer to treat self-recognized disorders or symptoms, the intermittent or continued use of a medication previously prescribed by a physician for chronic or recurring disease or symptom, or the use of medication recommended by lay sources or health workers not entitled to prescribe medicine.”[2]
The problem of self-medication is felt across the world. While countries of the developed world such as Switzerland, Germany, the USA, and Australia report a low prevalence of 8%, 11%, 13%, and 11%, respectively, the prevalence of self-medication is higher in developing countries such as India, Pakistan, and Nigeria.[3,4] Though the sale of over-the-counter drugs without a doctor’s prescription is discouraged by the Indian Government, but due to the easy and unrestricted availability of medications over the counter without adequate supervision, the practice is rampant in India. A 2015 report stated that 52% of Indians self-medicate.[5,6] In the present scenario of the ongoing COVID-19 pandemic, there is a likely chance that these numbers might have gone up, considering that visiting a hospital during lockdown could have been a challenge, associated with the fact that many private clinics were shut or functioning at a lower capacity.[7] Some medicines have been advertised as beneficial without any proper scientific basis, and people might have also fallen for them.[7]
Self-medication is a cheaper and time-saving alternative to those who cannot afford clinical service for some reason or the other. In India, a few drugs do not require a prescription to be sold over the counter, but most other drugs do, which belong to either Schedule H, H1, or X of the Drug Schedule Classification.[8,9] Indiscriminate practice of self-medication often leads to dangerous unwarranted adverse effects like allergic reactions, poisoning due to overdosage, and life-threatening drug interactions. It may also result in a delay in health care seeking. All these factors ultimately increase the burden of morbidity and cost of health care seeking. Such indiscriminate use of medicines also results in drug resistance and dependence, frequently to the drugs that primary care physicians have to solely depend on, as they often have to work with limited resources and sometimes with a handful of drugs available to them for rendering disease management. This understandably results in increasing numbers of treatment failures, sometimes even resulting in violent forms of action targeted at the doctor from the patient and/or patient parties. With increasing incidences of such violence, primary care physicians are often the first ones to face the heat.[10]
With this background of the high prevalence of this important issue, this study assesses the pattern of self-medication and its practice among adults in an urban community of West Bengal and tries to find out the reasons behind such behavior. The association of socio-demographic factors with the practice of self-medication was also studied.
Materials and Methods
This descriptive, cross-sectional study was conducted in the field practice area of a Kolkata-based medical college, in August 2020. Efforts were made to incorporate all the resident families, however, 193 out of the total 213 families agreed to participate. The rest were either unwilling or were unreachable after three attempts, on three successive data collection days. Adult members (aged 18 years or more), with a history of taking allopathic medication in the last month among those 193 families were considered eligible for interview; those seriously ill were excluded. The data collection schedule used was predesigned and pretested. It had two parts. The first part of the study tool had questions on socio-demographic variables, and the second part had questions on self-medication practice. The second part of the schedule was administered only to those found to have practiced self-medication, in the last one month. The participants were interviewed after obtaining informed consent, with their identity undisclosed. For the purpose of the study, self-medication was considered to be present if, a study subject took any allopathic medication (which require doctor’s prescription as per Government rule) without consultation of a doctor or used an expired prescription for even one instance in the last one month to procure them and use. Medicines that do not require a prescription from a registered medical practitioner (RMP) to be used, as per government rule, were not considered as self-medication for the study.[8,9]
The study obtained clearance from the institutional ethics committee of the concerned medical college (Ref No.: MC/KOL/IEC/NON-SPON/756/08/20, dated 06.08.20).
The data were entered and analyzed in Statistical Packages for Social Science (SPSS)® (SPSS Inc, Chicago, IL, USA) version 16.0. The results were obtained based on the pre-defined objectives. Chi-square test was performed to check for any significant statistical association of self-medication practice with any socio-demographic variable (P < 0.05).
Results
Out of the 193 families who were approached, one or more members of 152 such families were found to have taken medication in the last one month, with individual participants amounting to 170. Out of these participants, 98 (57.7%) were found to have practiced self-medication. Among participants who had practiced self-medication, 39.8% (39/98) were aged between 28 and 37 years, the majority being females (57.1%; 56/98), with most being educated up to middle school level (36.7%; 36/98) and 46.9% (46/98) each belonging to socio-economic class III and IV of the Modified BG Prasad Scale.[11] [Table 1].
Table 1.
Socio-demographic characteristics of the study subjects (n=98)
| Variables | No. (%) | |
|---|---|---|
| Age (completed years) Mean: 38.6 years (SD: 10.7) | 18-27 | 13 (13.3) |
| 28-37 | 39 (39.8) | |
| 38-47 | 27 (27.6) | |
| 48-57 | 15 (15.3) | |
| 58 or more | 4 (4.1) | |
| Gender | Male | 42 (42.9) |
| Female | 56 (57.1) | |
| Educational status | Illiterate | 8 (8.2) |
| Primary | 33 (33.7) | |
| Middle School | 36 (36.7) | |
| Secondary | 15 (15.3) | |
| Higher Secondary or above | 6 (6.1) | |
| Marital status | Currently Married | 77 (78.6) |
| Never Married | 16 (16.3) | |
| Widowed/Separated | 5 (5.1) | |
| Socio-economic class* | Class I | 0 (0.0) |
| Class II | 6 (6.1) | |
| Class III | 46 (46.9) | |
| Class IV | 46 (46.9) | |
| Class V | 0 (0.0) | |
| Occupation | Home based | 42 (42.9) |
| Outdoor based | 56 (57.1) | |
*As per Modified BG Prasad Scale, July 2019.[11]
Among the 98 participants, who had practiced self-medication, the most commonly used medicines were for pain suppression (46.9%; 46/98), followed by antibiotics (43.9%; 43/98) and anti-acid medications (39.8%; 39/98). Fever and cough-cold were the commonest morbidities due to which the participants self-medicated (27.6%; 27/98 and 24.5%; 24/98, respectively). The most common reasons behind not seeking physician’s consultation were lack of felt-need (34.7%; 34/98), followed by satisfaction after using the concerned medicine in a previous instance (24.5%; 24/98), the same proportion (24.5%; 24/98) cited emergency reasons behind non-consultation. A total of 64.3% (63/98) of these participants stated that pharmacies suggested they take such medication after listening to their symptoms, whereas 46.9% (46/98) cases used their knowledge that was gained from a previous consultation with an RMP. Regarding the source of procurement, 76.5% (75/98) procured such medications from pharmacies without any prescription, whereas 34.7% (34/98) used expired prescriptions to buy the medicine (s) in one or more instances. All were found to have checked the expiry date of medicine (s) before consumption (100.0%; 98/98) [Figures 1, 2 and Table 2].
Figure 1.
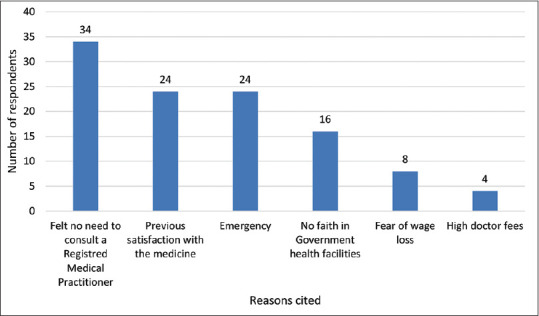
Distribution of the respondents practicing self-medication according to reasons cited in favor of such practice* (n = 98)
*(Multiple response)
Figure 2.
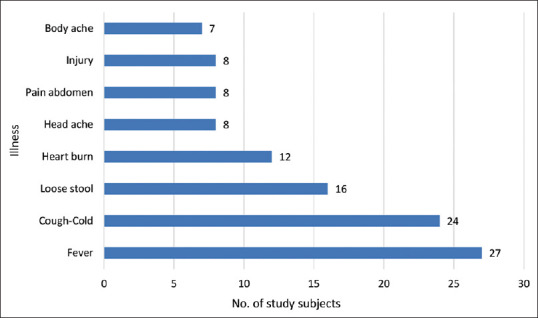
Illnesses for which the study subjects self-medicated* (n = 98)
*(Multiple response)
Table 2.
Distribution of study subjects practicing self-medication according to details of such practice* (n=98)
| Variable | No. (%) | ||
|---|---|---|---|
| Type of medicine (s) taken | Pain suppressor | 46 (46.9) | |
| Antibiotics | 43 (43.9) | ||
| Anti-acidity | 39 (39.8) | ||
| Anti-allergics (including cough suppressants) | 16 (16.3) | ||
| Source of knowledge regarding the medicine (s) used | Pharmacy | 63 (64.3) | |
| Previous consultation with an RMP for a similar illness | 46 (46.9) | ||
| Family members | 31 (31.6) | ||
| Friends | 12 (12.2) | ||
| Source of procurement of the medicine (s) used | Pharmacy | Without prescription | 75 (76.5) |
| Using old prescription | 34 (34.7) | ||
| Medicines kept with self or provided by other family members or friends | 16 (16.3) | ||
*Multiple responses
Level of education was significantly associated with self-medication tendency (P = 0.021), with the less educated tending to self-medicate more than those with higher education (Odds Ratio: 2.200 (1.116-4.336)). Females, subjects belonging to the higher socio-economic class, and those staying at home were found to be more prone to self-medicate than their counterparts, however, no significant statistical association was found [Table 3].
Table 3.
Association of self-medication practice with socio-demographic variables (n=170)
| Variable | Self-medication practice | Total | OR (95% C.I.) | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Practiced | Not practiced | |||||
| Age (completed years) | 38 or less | 55 | 42 | 97 | Ref 0.914 (0.494-1.691) |
0.774 |
| >38 | 43 | 30 | 73 | |||
| Gender | Female | 56 | 39 | 95 | Ref 1.128 (0.612-2.081) |
0.699 |
| Male | 42 | 33 | 75 | |||
| Occupation | Home based | 42 | 27 | 69 | Ref 1.250 (0.671-2.330) |
0.482 |
| Outdoor | 56 | 45 | 101 | |||
| Socioeconomic class | Class II & III | 52 | 34 | 86 | Ref 1.263 (0.687-2.324) |
0.452 |
| Class IV | 46 | 38 | 84 | |||
| Marital status | Currently Married | 69 | 52 | 121 | Ref 0.915 (0.467-1.795) |
0.796 |
| Others | 29 | 20 | 49 | |||
| Education | Up to middle school | 77 | 45 | 122 | Ref 2.220 (1.116-4.336) |
0.021 |
| Secondary or above | 21 | 27 | 48 | |||
Discussion
Self-medication practice is a dangerous predisposition that often puts its practitioners at health risks of various kinds, which often amount to further health complications as a result of side-effects, resulting in increased out-of-pocket expenditure and financial burden. A study from Telangana found the proportion of self-medicating respondents to be 73%, whereas another study from Karnataka noted this number to be 40.5%.[12,13] In a study from Delhi, 92.8% of the participants were reportedly practicing self-medication.[14] A high prevalence of such practice (73.8%) was also found by a study done in Rajasthan; self-medication was found to be practiced by 68% of the respondents of a Maharashtra-based study.[15,16] An Andhra Pradesh–based study showed self-medication to be prevalent in 68.1% of their study participants.[17] Studies from other developing countries have reported a high trend in self-medication practice. A Bangladeshi study done during the COVID-19 pandemic reported 71.40% of its participants to have self-medicated.[18] A recent study done among residents of Pokhara valley in Nepal found, 38.2% of their study subjects to be self-medicating.[19] The present study also reports a similar finding, with the majority of its participants practicing self-medication (57.7%) – not feeling the need to consult a registered medical practitioner before taking medications was found to be the most common reason cited by these participants (34.7%). Satisfaction after using the concerned medicine in a previous instance and emergency reasons were the excuses that followed (24.5% each). Along similar lines, a study from Hyderabad noted 42% of its participants found self-medication to be a time-saving option.[12] As per a study from Karnataka, 32.1% of its participants reasoned previous good experience with a specific medicine was the basis of them self-medicating; whereas a study from Delhi found 46.5% of its respondents had self-medicated based on their past experience.[13,14] A study based in Southern Rajasthan found a lack of felt need for doctor’s advice to be the most common excuse behind self-medication practice.[15] Not perceiving the illness serious enough for a doctor’s consultation was what the majority (58.8%) of the participants of a Maharashtra-based study had to say.[16]
Unregulated sale of medications in India including easy access to even those medications which ideally cannot be sold without a valid prescription as per the government regulations is often the most important factor behind such a preponderance of self-medication in the country. All forms of medicines are easily available over the counter, with none to be held accountable due to a lack of adequate legal enforcements.
As per our study, pain suppressors and antibiotics were used maximally by the participants (46.9% and 43.9%, respectively). All self-medicating participants were found to have checked for expiry dates before consuming such medications. Pharmacies (64.3%) were the commonest information source regarding medicine (s) for self-medication. Fever was the commonest morbidity, followed by cough-cold for which the participants self-medicated (27.6% and 24.5%, respectively), a finding which was also obtained by other similar studies.[12,14] A study done in Hyderabad reported 93% of its participants checking for expiry dates of the medications; information regarding such medicine (s) being obtained from pharmacies in 67% of the cases.[12] A Bengaluru-based study found a majority of its participants resorting to analgesics and checking for expiry date, with fever being the commonest issue (78.89%).[13] Fever and headache were the commonest causes behind self-medication, as reported by studies from Rajasthan and Andhra Pradesh.[15,17] Analgesics were the most common self-medicated drug, as per the study from Andhra Pradesh (85%).[17] A Nepalese study found most of their participants resorting to self-medication for aches (50%) and cough and cold (31%).[19] A Dhaka-based study conducted during the ongoing COVID-19 pandemic reported fever (37.61%), throat pain (28.79%), and dry cough (14.20%) to be the commonest symptoms for which self-medication was practiced; pharmacies were the source of knowledge for 24% of their respondents.[18] On similar lines, knowledge regarding self-medications was obtained mostly from pharmacies in studies from Puducherry and Vishakhapatnam (38.1% and 72.6%, respectively).[17,20] Pharmacists served as a source for medical information for 43.52% of the respondents, followed by a previous prescription (27.16%), in a study done in Udaipur, Rajasthan.[15]
Conclusion
This study found self-medication to be a common practice among the majority of its participants, with fever being the commonest cause and pain suppressors as the commonest class of medicines used. Most of those who practiced self-medication did so as they did not feel it to be necessary to consult a physician, coupled with the fact that in most cases, both suggestions about which medicine to use and the medicine itself was readily available from local pharmacies, without the need of a valid prescription.
Indians are found to easily predispose themselves to the harmful practice of self-medication, as is evident in media reports and research articles from all over the country as well.[5,12,13,14,15,16,20,21] There is an urgent need to curb such practice, as it ultimately leads to an unfavorable health scenario by resulting in an increased load of morbidity and financial loss.
The findings as mentioned above, emphasize the need to sensitize people regarding the danger posed by the indiscriminate use of medicines. Education played a significant role in determining the tendency of our study participants towards self-medication practice. Seminars in schools and colleges may be arranged to make the population aware of the evils of self-medication at a young age. This study also found that females and participants staying at home tended to self-medicate more. Means of mass communication such as television and radio can be made use of, to deliver the necessary messages to the people who mostly stay at home. Active campaigns designed to spread such awareness among other sections of the population must also be undertaken. Local motivators such as politicians, teachers, religious leaders may be sensitized first and asked to join the campaign. Film stars and sports personalities may be approached to become goodwill ambassadors in this fight against self-medication. Social media campaigns also have a great potential to reach most segments of the Indian population, especially those belonging to the higher socio-economic class. Stricter implementation of existing laws that limit the availability of medicines over the counter, along with the adaptation of the community education strategy is, therefore, the need of the hour. Regular and ongoing vigilance in the matter is also warranted to control this tendency.
The limitation of the present study could have been the fact that its findings rely upon the respondents recalling their medication use over the last month, and therefore recall bias cannot be ruled out. Being conducted on a population residing in a medical college’s field practice area, there could be a hindrance in generalizing the findings of the study on other communities, as the study population can be expected to behave differently than others, being exposed to regular health campaigns.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Montastruc JL, Bagheri H, Geraud T, Lapeyre MM. Pharmacovigilance of self-medication. Therapie. 1997;52:105–10. [PubMed] [Google Scholar]
- 2.WHO. Guidelines for the Regulatory Assessment of Medicinal Products For Use In Self-Medication. Geneva: World Health Organization; 2000. [Last accessed on 2019 Jan 28]. Available from: http://www.apps.who.int/medicinedocs/en/d/Js2218e/ [Google Scholar]
- 3.Limaye D, Limaye V, Krause G, Fortwengel G. A Systematic Review of the Literature to Assess Self-medication Practices. Annals of Medical and Health Sciences Research [Internet] 2017. [Last accessed on 2020 Jun 22]. Available from: https://www.amhsr.org/abstract/a-systematic-review-of-the-literature-to-assess-selfmedication-practices-3711.html .
- 4.Bennadi D. Self-medication:A current challenge. J Basic Clin Phar. 2013;5:19–23. doi: 10.4103/0976-0105.128253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jha DN. 52% Indians self-medicate [Internet]. The Times of India. 2015. [Last accessed on 2020 Jun 14]. Available from: https://timesofindia.indiatimes.com/city/delhi/52-Indians-self-medicate/articleshow/46844097.cms .
- 6.Narendranath KG. Govt says no to OTC sale of schedule H drugs [Internet] The Economic Times. 2004. [Last accessed on 2020 Jun 17]. Available from: https://economictimes.indiatimes.com/govt-says-no-to-otc-sale-of-schedule-h-drugs/articleshow/560289.cms .
- 7.Patil AD, Sharma H, Tetarbe T. COVID-19 and concerns related to self-medication. Int J Basic Clin Pharm. 2020;9:1475–6. [Google Scholar]
- 8.Drugs and Cosmetics Rules-Schedule H &Schedule H1 Drugs [Internet]. Medindia. [Last accessed on 2020 Jun 17]. Available from: https://www.medindia.net/patientinfo/drugs-and-cosmetics-rules-schedule-h-schedule-h1-drugs.htm .
- 9.Tandon P, Gupta V, Ranjan A, Gandhi P, Kotiyal A, Kapoor A. A review on the current classification and regulatory provisions for medicines in drug &cosmetic act, in the light of present day context. Int Arch BioMed Clin Res. 2017;3:I–VII. [Google Scholar]
- 10.Ghosh K. Violence against doctors:A wake-up call. Indian J Med Res. 2018;148:130–3. doi: 10.4103/ijmr.IJMR_1299_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.BG Prasad scale [Internet] Prasad Social Classification Scale Update. 2019. [Last accessed on 2019 Sep 03]. Available from: http://prasadscaleupdate.weebly.com/
- 12.Katkuri S, Chauhan P, Shridevi K, Kokiwar P, Gaiki V. Prevalence of self-medication practices among urban slum dwellers in Hyderabad, India. Int J Community Med Public Health. 2016;3:1816–9. [Google Scholar]
- 13.Hajira S, Shivananda K., Jayan M, Hussain CA. Prevalence of self-medication practices and its associated factors in rural Bengaluru, Karnataka, India. Int J Community Med Public Health. 2017;3:1481–6. [Google Scholar]
- 14.Kumar V, Mangal A, Yadav G, Raut D, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ. 2015;8:16–20. [Google Scholar]
- 15.Jain M, Prakash R, Bapna D, Jain R. Prevalence and pattern of self-medication practices in Urban area of Southern Rajasthan. Ntl J of Community Med. 2015;6:474–7. [Google Scholar]
- 16.Vargese SS, Durgawale PM, Mathew P. Prevalence of self medication in an urban slum area in Maharashtra. J Krishna Inst Med Sci Univ. 2013;2:108–10. [Google Scholar]
- 17.Rangari GM, Bhaisare RG, Korukonda V, Chaitanya YL, Hanumanth N. Prevalence of self-medication in rural area of Andhra Pradesh. J Family Med Prim Care. 2020;9:2891–9. doi: 10.4103/jfmpc.jfmpc_204_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nasir M, Chowdhury ASMS, Zahan T. Self-medication during COVID-19 outbreak:A cross sectional online survey in Dhaka city. Int J Basic Clin Pharm. 2020;9:1325–30. [Google Scholar]
- 19.Paudel S, Aryal B. Exploration of self-medication practice in Pokhara valley of Nepal. BMC Public Health. 2020;20:714. doi: 10.1186/s12889-020-08860-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selvaraj K, Kumar SG, Ramalingam A. Prevalence of self-medication practices and its associated factors in Urban Puducherry, India. Perspect Clin Res. 2014;5:32–6. doi: 10.4103/2229-3485.124569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wani WR. Self Medication –The New Epidemic [Internet] New Delhi Times. 2018. [Last accessed on 2020 Jun 22]. Available from: https://www.newdelhitimes.com/self-medication-the-new-epidemic/


