ABSTRACT
Objectives:
To find the prevalence of COVID vaccine hesitancy amongst people of Odisha and reasons for the same
Design:
Observational Study
Setting:
Outpatients, inpatients, and attenders in tertiary health centers in Khorda, Tangi, and Mendhasal, Odisha, India; online data via google forms from people across the state.
Duration of Study:
April to June 2021
Participants:
Convenience sampling of 450 adults aged between 18 and 60
Main Outcome Measure:
Willingness to get vaccinated against COVID-19
Results:
Hesitancy rate stands at 12.7%, with 5.7% in the urban setting and 20.9% in rural (CI 95%, P = 0.000), 3.1% amongst males and 25.4% females (CI 95% P = 0.000), and 42.6% amongst the homemakers. Main reasons for vaccine hesitancy include lack of knowledge about efficacy,fear of side effects, and testing positive despite taking the vaccine
Conclusions:
The near tripling of the hesitancy rates indicates a probable hindrance in stopping the spread of the infection. Family physicians have a significant role in alleviating the myths, counseling people, and managing adverse events.
Keywords: Attitude, COVID-19, hesitancy, vaccine
Introduction
Vaccination has been viewed skeptically since its inception.[1] The World Health Organisation (WHO) defines vaccine hesitancy as a delay in acceptance or refusal of vaccines despite the availability of vaccine services.[2]
A study in the USA showed around 48% of the sample was hesitant towards the COVID vaccine.[3] The hesitancy stood at 41.4% in January 2021 in India.[4]
The prevaccination drive surveys indicated significant vaccine hesitancy. The study had the primary objective of finding the prevalence of COVID-19 vaccine hesitancy amongst the people of Odisha, post initiation of the vaccination drive and secondary objectives of finding the general attitude with regard to the COVID-19 vaccines.
Materials and Methods
This cross-sectional study was conducted in and around tertiary level health centers in Tangi, Mendhasal, and Khorda, Odisha between 25th May and 15th June 2021. Taking the vaccine hesitancy prevalence at 50%, a confidence interval of 95%, a precision of 5%, and a non-response rate of 10%, the sample size was calculated to be 440. A convenience sampling of total of 460 participants was done, ensuring equitable distribution amongst male-female and rural-urban groups The inclusion criteria included being a resident of India, between the ages of 18 to 60, and being able to comprehend the objectives and give informed consent.
The remaining 450 participants, [Table 1] once provided an information sheet and consented, were administered a structured questionnaire-based interview by a single trained interviewer. The questionnaire covered various sociodemographic factors such as the interviewee’s age, education and economic status, religion, and place of residence, and information such as awareness about the start of the vaccination drive, the types and number of vaccines available in our country; interest in getting vaccinated; the major source of information regarding the vaccines; knowledge about common side effects and centers for vaccination; the belief of family members regarding the vaccines and importance of COVID-19 appropriate behavior post vaccination as well.
Table 1.
Demographic details of the interviewees
| Demographic parameter | No. of participants (n=450) |
|---|---|
| Age (in years) | |
| 18-30 | 246 (54.67) |
| 31-44 | 126 (28.00) |
| 45-60 | 78 (17.33) |
| Gender | |
| Male | 257 (57.11) |
| Female | 193 (42.89) |
| Residence | |
| Rural | 206 (45.78) |
| Urban | 244 (54.22) |
| Education status | |
| Illiterate | 10 (2.22) |
| Primary school | 63 (14.00) |
| Secondary school | 148 (32.89) |
| Graduate | 200 (44.44) |
| Postgraduate | 29 (6.45) |
| Occupation | |
| Student | 194 (43.11) |
| Government job | 33 (7.33) |
| Private job | 79 (17.55) |
| Daily wager | 58 (12.88) |
| Homemaker | 68 (15.13) |
| Unemployed | 18 (4.00) |
| Religion | |
| Hindu | 392 (87.11) |
| Muslim | 14 (3.11) |
| Christian | 42 (9.34) |
| Others | 2 (0.44) |
| Marital status | |
| Married | 227 (50.44) |
| Unmarried | 223 (49.56) |
| Socio-economic status (Kuppuswamy) | |
| Lower class | 170 (37.78) |
| Upper lower class | 82 (18.22) |
| Lower middle class | 106 (23.55) |
| Upper middle class | 44 (9.78) |
| Upper class | 48 (10.67) |
Institutional ethics committee approval was taken before the start of this study vide letter no. T/IM-NF/CM&FM/20/223 dated May 20th 2021. Confidentiality of the data was maintained in the department.
Statistics
The data collected was double-checked for completeness, coded, and analyzed using appropriate statistical methods with staatistical package for social sciences (SPSS) software version 25. Association between categorical variables was analyzed using the Chi-square test and those with P- value < 0.05 was considered significant.
Results
Nearly 90% of the sample was aware that the vaccination drive had begun in the country, however, the distribution remained unequal, with almost one-third of the homemakers having no idea about the drive [Figure 1]. The number was also alarmingly low amongst the illiterate. Only 53.4% females and 57.2% males were aware that there were currently two vaccines being rolled out, with the awareness standing at 74.2% in urban areas and 33.5% in rural areas [Table 2]. Nearly 83% of those individuals aged between 18 and 25 were aware, whereas the percentage was below 30 amongst those aged between 26 and 60 [Table 2]. Half the rural population didn’t t know either Covaxin or Covishield, whereas nearly 85% of the urban people were familiar with both the vaccines. Literacy played a role here with almost all illiterates and primary schooled people not aware of either vaccine [Table 3]. A total of 79.1% of the rural population and 94.3% of urban were willing to take the vaccine if given a choice [Table 4]. A total of 96.9% of the males were interested, whereas the number stood at 74.6% among the females, and the number was grossly lower in homemakers at 57.4% [Table 3]. A total of 44.2% of the interviewed preferred Covaxin, whereas nearly 30% did not have any particular preference or did not know about the two vaccines (P = 0.000). More than 70% had heard about the side effects of the vaccines but less than a fourth of them were apprehensive about them (P = 0.000). The most common side effects reported included fever, body pains, headache, and nausea, but around 18 people reported severe allergic reactions and death, more so, after being given Covishield. Around 1/3rd of the interviewees had searched around information about the vaccines, whereas nearly 40% were totally unaware. Almost 75% were willing to definitely take time out to get vaccinated. Around 20% thought that the vaccine may had been developed too fast, but nearly 50% were confident that it is possible to develop vaccines at a fast pace in today’s world. Around 1/3rd thought that the elderly should be prioritized for vaccination, whereas around 25% thought adults with co-morbidities should be given priority, around 12% suggested pregnant women to be vaccinated first. The major source of information remained news followed by social media and word of mouth by relatives and colleagues [Figure 2].
Figure 1.
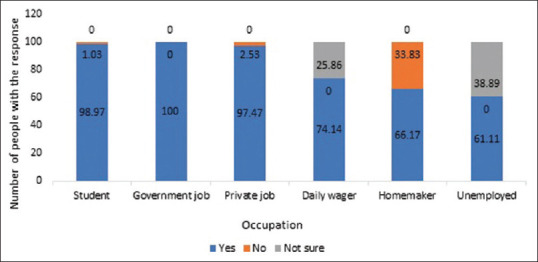
Knowledge regarding COVID-19 vaccination among respondents (N = 450) X-axis: Occupation, Y-axis: Number of people with the response
Table 2.
Knowledge about the number of vaccines available
| How many vaccines do you think are currently available for COVID-19 in our country? | 1 | 2 | 3 | >3 | Don’t know | Total (n=450) | P |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 7 (2.7) | 147 (57.2) | 2 (0.8) | 8 (3.1) | 93 (36.2) | 257 | 0.019 |
| Female | 2 (1.0) | 103 (53.4) | 0 (0.0) | 0 (0.0) | 88 (45.6) | 193 | |
| Age | |||||||
| 18-30 | 9 (3.7) | 204 (82.9) | 2 (0.8) | 4 (1.6) | 27 (11.0) | 246 | 0.000 |
| 31-44 | 0 (0) | 30 (23.8) | 0 (0) | 3 (2.4) | 93 (37.8) | 126 | |
| 45-60 | 0 (0) | 16 (20.5) | 0 (0) | 1 (1.3) | 61 (78.2) | 78 | |
| Residence | |||||||
| Rural | 7 (3.4) | 69 (33.5) | 0 (0.0) | 2 (1.0) | 128 (62.1) | 206 | 0.000 |
| Urban | 2 (0.8) | 181 (74.2) | 2 (0.8) | 6 (2.5) | 53 (21.7) | 244 |
Table 3.
Knowledge about the types of vaccines
| Know the currently available vaccines | Covaxin | Covishield | Both | Don’t know either | Total (n=450) | P |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18-30 | 16 (6.5) | 0 (0.0) | 222 (90.2) | 8 (3.3) | 246 | 0.000 |
| 31-44 | 8 (6.3) | 9 (7.1) | 41 (32.5) | 68 (54.0) | 126 | |
| 45-60 | 1 (1.3) | 2 (2.6) | 24 (30.8) | 51 (65.4) | 78 | |
| Gender | ||||||
| Male | 23 (8.9) | 2 (0.8) | 175 (68.1) | 57 (22.2) | 257 | 0.000 |
| Female | 2 (1.0) | 9 (4.7) | 112 (58.0) | 70 (36.3) | 193 | |
| Occupation | ||||||
| Student | 0 (0.0) | 0 (0.0) | 190 (97.9) | 4 (2.1) | 194 | 0.000 |
| Government job | 9 (27.3) | 2 (6.1) | 20 (60.6) | 2 (6.1) | 33 | |
| Private job | 14 (17.7) | 9 (11.4) | 38 (48.1) | 18 (22.8) | 79 | |
| Dailywager | 0 (0.0) | 0 (0.0) | 14 (24.1) | 44 (75.9) | 58 | |
| Homemaker | 0 (0.0) | 0 (0.0) | 16 (23.5) | 52 (76.5) | 68 | |
| Unemployed | 2 (11.1) | 0 (0.0) | 9 (50.0) | 7 (38.9) | 18 | |
| Residence | ||||||
| Rural | 18 (8.7) | 0 (0.0) | 81 (39.3) | 107 (51.7) | 206 | 0.000 |
| Urban | 7 (2.9) | 11 (4.5) | 206 (84.4) | 20 (8.2) | 244 | |
| Education status | ||||||
| Illiterate | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (100.0) | 10 | 0.000 |
| Primary school | 0 (0.0) | 0 (0.0) | 2 (3.2) | 61 (96.8) | 63 | |
| Secondary school | 14 (9.5) | 2 (1.4) | 98 (66.2) | 34 (23.0) | 148 | |
| Graduate | 11 (5.5) | 9 (4.5) | 167 (83.5) | 13 (6.5) | 200 | |
| Post-graduate | 0 (0.0) | 0 (0.0) | 20 (69.0) | 9 (31.0) | 29 |
Table 4.
Interest in getting vaccinated
| If given a choice, would you take the vaccine once the drive rolls out to public? | Yes | No | Maybe | Not right away, maybe later | Total (n=450) | P |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18-30 | 230 (93.5) | 0 (0.0) | 6 (2.4) | 10 (4.1) | 246 | |
| 31-44 | 107 (84.9) | 19 (15.1) | 0 (0.0) | 0 (0.0) | 126 | |
| 45-60 | 56 (71.8) | 2 (2.6) | 16 (20.5) | 4 (5.1) | 78 | |
| Socioeconomic status | ||||||
| Lower class | 140 (82.4) | 12 (7.1) | 14 (8.2) | 4 (2.4) | 170 | 0.01 |
| Upper lower class | 75 (91.5) | 0 (0.0) | 3 (3.7) | 4 (4.9) | 82 | |
| Lower middle class | 97 (91.5) | 2 (1.9) | 4 (3.8) | 3 (2.8) | 106 | |
| Upper middle class | 36 (81.8) | 5 (11.4) | 0 (0.0) | 3 (6.8) | 44 | |
| Upper class | 45 (93.8) | 2 (4.2) | 1 (2.1) | 0 (0.0) | 48 | |
| Gender | ||||||
| Male | 249 (96.9) | 0 (0.0) | 0 (0.0) | 8 (3.1) | 257 | 0.000 |
| Female | 144 (74.6) | 21 (10.9) | 22 (11.4) | 6 (3.1) | 193 | |
| Residence | ||||||
| Rural | 163 (79.1) | 21 (10.2) | 18 (8.7) | 4 (1.9) | 206 | 0.000 |
| Urban | 230 (94.3) | 0 (0.0) | 4 (1.6) | 10 (4.1) | 244 | |
| Occupation | ||||||
| Student | 184 (94.8) | 0 (0.0.) | 2 (1.1) | 8 (4.1) | 194 | 0.000 |
| Government job | 31 (93.9) | 0 (0.0) | 2 (6.1) | 0 (0.0) | 33 | |
| Private job | 73 (92.4) | 0 (0.0) | 2 (2.2) | 4 (5.1) | 79 | |
| Daily wager | 50 (86.2) | 0 (0.0) | 8 (13.8) | 0 (0.0) | 58 | |
| Homemaker | 39 (57.4) | 21 (30.9) | 8 (11.8) | 0 (0.0) | 68 | |
| Unemployed | 16 (88.9) | 0 (0.0) | 0 (0.0) | 2 (11.1) | 18 |
Figure 2.
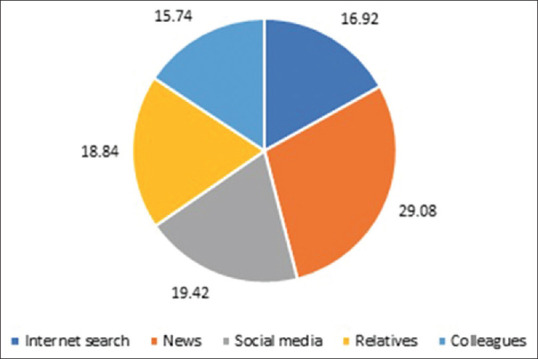
Major source of information about COVID-19 vaccines among respondents (%) (N = 450)
Discussion
The COVID-19 vaccination hesitancy stands at 12.7% (with 4.7% refusing outright and 8% in a dilemma whether to take or not), in the state of Odisha according to our study. This number stood at 4.70% amongst the health care workers interviewed across the country in December 2020 before the initiation of the vaccination drive.[5] The nearly tripling value of hesitancy amongst the rising COVID-19 cases, and related deaths were alarming as vaccination is one of the most successful and cost-effective health interventions known.[6] Though we stand far ahead of France, the United States, and Italy with hesitancy rates of 41.1%, 43.9%, and 46.3%, respectively, we are still behind the 3% of Ecuador and 5.7% of our neighboring country Malaysia.[7] The hesitancy could be a major limiting step in preventing the further spread and deaths associated with COVID-19 as studies estimate a range of 60%–75% population immunity necessary to prevent further forward transmission and spread in the community.[7] Our study showed lower interest of females towards the vaccine, similar to the results obtained in the United States, Canada, Israel, and other countries.[8,9,10,11] This is probably due to lower awareness and literacy amongst Indian women as well as constitutional risk-taking behavior in men.
The main reasons for the hesitancy as obtained from our study were, lack of knowledge about efficiency, second-hand experience with and fear of side effects, some quoted testing positive despite taking the vaccine, pretty much as the reasons obtained by studies worldwide [Figure 3]. In the case of women, the husband’s influence played a major role as well. Concerns about the speedy development of the vaccines, lack of trust in the pharmaceuticals manufacturing the vaccines, and disbelief in the concept of vaccination per se had not really been stated by the study group in contrast to being amongst the major reasons in the developed countries.[9]
Figure 3.
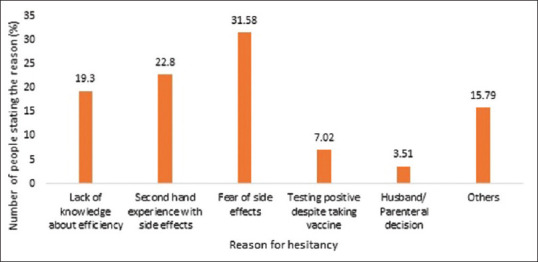
Reasons for vaccine hesitancy among those who are not willing to get vaccinated immediately (N = 57) X-axis: Reason for hesitancy, Y-axis: Number of people stating the reason (%)
Those willing to get vaccinated believed that the vaccines were safe, and side effects were mild, had had second-hand experience with family members getting vaccinated, had fear of contracting the infection, and trust the government, health care workers as well as the vaccine manufacturers. This is similar to the results obtained in the United states, where people with the fear of contracting the infection were one and a half times more likely to get themselves as well as their families vaccinated[12] and in Libya, a positive association was found between interest in getting vaccinated and a family member having been infected; and a negative association with COVID-related death of an acquaintance.[13] Of particular concern is the alarming fact that 50.33% of the interviewees said they would get influenced by family, friends, religious leaders, and celebrities about their decision of getting vaccinated. A study amongst university students in China showed an odds of nearly 18 times when asked if they would urge their family to get vaccinated or not.[14] This kind of affirmative influence may aid in the promotion of the vaccination drive. However, the scenario might be quite different in our country, considering the fact that most religious gurus have spoken against vaccination, and many participants in our study admitted to visiting one of these self-proclaimed godmen when a family member was infected with COVID-19, before going to the hospital. One such result was obtained by Umakanthan S in January in our country, who found the hesitancy to be higher amongst the religious people.[4]
Less than a fourth of the interviewed were apprehensive about the side effects that the vaccines may have. This stands much better compared to Libya where nearly 37% agreed to be concerned about serious adverse reactions the vaccines may have.[13]
The news was the major source of information, followed closely by social media and relatives and colleagues. Health information orientation i.e., “the extent to which the individual is willing to look for health information,”[15] is a key factor influencing health information seeking and exposure. News and mass media seem to be the most credible and effective ways to communicate with the general public, and it is relieving to know that they form the major source of information. Similar results were obtained in Germany, with mass media and interpersonal communication being the primary sources of information and health authorities, the most trusted source.[16]
Around 65% of the interviewed were aware of both the vaccines available under the government program i.e., Covaxin and Covishield. Amongst them, 63.7% preferred Covaxin, showing trust in the population in the indigenous vaccine. It shows the trust people have in the scientific methods and governance of our country and is comparable to the results obtained in China, where 64.2% preferred the domestically manufactured vaccine.[17]
Nearly 76% felt that the protection offered by the vaccine would be short-lasting but it is frightening to see that around 6% thought that masks, social distancing, and sanitization would not be essential after getting vaccinated. This is something of grave importance, given that COVID-appropriate behavior and individual measures have been advocated in every nook and corner of the world for more than a year. Almost 80% requested further official information about the efficacy and side effects profile of the vaccines before getting vaccinated, but nearly all of the interviewed trust that the government will help them make the right choice.
Interpretations and implications: Our study shows that despite the rising number of COVID cases and related deaths, there still exists hesitancy amongst people towards the vaccination. It is the need of the hour to combat any stigma that exists around the vaccines and deal with the concerns people have towards them.
We propose some strategies to combat this. We can have authorized government-run programs via mass media regarding the vaccines, efficacy data and side effect profile, availability at different centers, etc., One such initiative that has already been taken by the government is the “Har Ghar Dastak,” the door-to-door COVID-19 vaccine campaign, launched by the Government of India in early November.
Role of the primary care and family physicians: In a country like India, family physicians, who form an integral part of the first tier health system, can play a crucial role in “health information orientation,” i.e., make people understand the importance of health and seek information regarding the various health issues. They can act as a direct link between the public and the health care system vide effective counseling, clearing doubts of the public, explaining the various myths around vaccination with a special focus on the adverse effects following vaccination. They can also train the grass root level workers in order to speed up and make the process more effective.
Future research directions: Our current focus should be on the vaccination of children, the next phase of the vaccination program. A study in Turkey among the parents showed a gross 66% hesitancy among the parents towards foreign vaccines and a not so insignificant 37.4% towards indigenous vaccines for their kids.[18] As most adults are now vaccinated with at least one dose, there will be a paradigm shift in the incidence of the infection among children hence making it a crucial area to work on immediately.
The limitations of the study include the fact that the sample has been collected from one state only, extrapolation of the data to the entire country may not be very accurate, and hesitancy with respect to different expected efficacies of the vaccines has not been sought for.
Key points: The COVID-19 vaccination hesitancy stands at 12.7%. The main reasons for the hesitancy are lack of knowledge about efficiency, second-hand experience with and the fear of side effects.
Take home message: Primary care physicians can play a major role in counseling people, managing adverse events following vaccination, and bursting all myths around the subject.
Novelty from the study: Hesitancy in Odisha was sought for, after the initiation of the vaccination drive, when people had gained certain second-hand knowledge on the subject.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.A brief history of vaccination [Internet Immunisation Advisory Centre 2020] [Last accessed on 2021 Feb 14]. Available from: https://www.immune.org.nz/vaccines/vaccine-development/brief-history-vaccination#:~:text=Edward%20Jenner%20is%20 considered%20the,first%20smallpox%20vaccine%20was%20developed .
- 2.MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036. doi: 10.1016/j.vaccine.2015.04.036. Epub 2015 Apr 17. PMID: 25896383. [DOI] [PubMed] [Google Scholar]
- 3.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J Community Health. 2021;46:270–7. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umakanthan S, Patil S, Subramaniam N, Sharma R. COVID-19 vaccine hesitancy and resistance in India explored through a population-based longitudinal survey. Vaccines (Basel) 2021;9:1064. doi: 10.3390/vaccines9101064. doi: 10.3390/vaccines9101064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chew NWS, Cheong C, Kong G, Phua K, Ngiam JN, Tan BYQ, et al. An Asia-Pacific study on healthcare workers' perceptions of, and willingness to receive, the COVID-19 vaccination. Int J Infect Dis. 2021;106:52–60. doi: 10.1016/j.ijid.2021.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO Global vaccine action plan 2011. 2020 ISBN 978 92 4 150498 0 (NLM classification: WA 115) © World Health Organization 2013. [Google Scholar]
- 7.Sallam M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38:6500–7. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Razai MS, Chaudhry UAR, Doerholt K, Bauld L, Majeed A. Covid-19 vaccination hesitancy. BMJ. 2021;373:1138. doi: 10.1136/bmj.n1138. doi: 10.1136/bmj.n1138. [DOI] [PubMed] [Google Scholar]
- 10.Shacham M, Greenblatt-Kimron L, Hamama-Raz Y, Martin LR, Peleg O, Ben-Ezra M, et al. Increased COVID-19 vaccination hesitancy and health awareness amid COVID-19 vaccinations programs in Israel. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph18073804. 183804. doi: 10.3390/ijerph 18073804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogilvie GS, Gordon S, Smith LW, Albert A, Racey CS, Booth A, et al. Intention to receive a COVID-19 vaccine: Results from a population-based survey in Canada. BMC Public Health. 2021;21:1017. doi: 10.1186/s12889-021-11098-9. doi: 10.1186/s12889-021-11098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21:818. doi: 10.1186/s12889-021-10862-1. doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elhadi M, Alsoufi A, Alhadi A, Hmeida A, Alshareea E, Dokali M, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: A cross-sectional study. BMC Public Health. 2021;21:955. doi: 10.1186/s12889-021-10987-3. doi: 10.1186/s12889-021-10987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward the COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17:1469–75. doi: 10.7150/ijbs.58835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dutta-Bergman MJ. Primary sources of health information: Comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004;16:273–88. doi: 10.1207/S15327027HC1603_1. [DOI] [PubMed] [Google Scholar]
- 16.Gehrau V, Fujarski S, Lorenz H, Schieb C, Blöbaum B. The impact of health information exposure and source credibility on COVID-19 vaccination intention in Germany. Int J Environ. Res Public Health. 2021;18:4678. doi: 10.3390/ijerph18094678. doi: 10.3390/ijerph18094678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020;14:e0008961. doi: 10.1371/journal.pntd.0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40:e134–36. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]


