ABSTRACT
Background:
The COVID-19 disease caused by the SARS-CoV-2 virus, has toppled the world since first case noted in 2019, and the cases have been increasing there after. This grave effect is caused by the cytokine storm induced inflammation produced by the noxious virus. As it is an inflammatory state, various acute phase reactants are expected to raise; thus serum ferritin is contemplated to increase. Here we aim to anchor serum ferritin as a way marker for diagnosis and management of COVID-19 patients and study its role as a prognostic marker. Another aspect is the association of COVID-19 with the N: L ratio; observation has stated that higher N: L ratio results in more severe outcome. The study aimed to establish a correlation of COVID-19 severity with serum ferritin in the form of HRCT Score, N: L Ratio and Clinical Outcome in the patients admitted in Intensive Care Unit
Result:
Out of 200 patients who were admitted in the intensive care unit with COVID-19, the association of serum ferritin with N: L Ratio and HRCT Score was significant, and the association of serum ferritin with clinical outcome in terms of discharged and expired was found to be statistically significant
Conclusion:
Serum ferritin was found to be a potent marker for clinical outcome in intensive care unit patients in terms of death versus treated. HRCT Score and N:L ratio were found to be correlated with serum ferritin. Therefore, we conclude that serum ferritin may determine the severity of COVID-19 infection and it can be used as a marker for Clinical Outcome thereby making it an often neglected biomarker for predicting prognosis in COVID-19 with most of the physicians focusing mostly on interleukin 6, C Reactive protein and d dimer as a marker of severe COVID infection.
Keywords: COVID-19, HRCT score, N:L ratio, serum ferritin
Introduction
Since the commencement of the pandemic, COVID-19 has been creating an intense burden on the health care system.[1] It has been noticed that these gruelling complications of COVID-19 is associated with the cytokine storm produced by the virus, hence anticipation of the cytokine storm can evaluate the necessity of intensive care management in the patients and aid in efficient management of the patient. The rise in Interleukin 1, 2, 6, 7 and Tumour necrosis factor (TNF) upshots the storm produced in COVID-19. As it is an inflammatory condition, the various acute phase reactants have been expected to rise in the inflammatory state of the disease.[2] Hence, an eagle s eye on serum ferritin, ESR, CRP could possibly enable to foretell the cytokine storm and aid in reduction of mortality caused by COVID-19.
Along with its aggressive spread, it has a great impact of morbidity and mortality. The virus is studied to evoke severe inflammatory response that leads to production of cytokine storm which results in significant irreversible multi organ damage and thus increase the rates of morbidity and mortality. The embarkment of cytokine storm also results in respiratory compromise resulting in development of hypoxia.[3] Thus, by analysing this cytokine storm before its appearance, a good amount of death rates could be brought to a standstill. As cytokine storm is an inflammatory response, various acute phase reactants like serum ferritin will be altered. A constant check on the serum ferritin level will help us anticipate the cytokine storm and aid in prompt management and thereafter assist in optimum care of these patients. Serum ferritin is generally used as a marker for anaemia, but in severe inflammatory state, hepcidin levels raise in the body.[4] Hepcidin plays a pivotal role in iron metabolism. Hepcidin inhibits the uptake of iron for haematopoiesis, as the level of hepcidin raises, iron cannot be utilised for haematopoiesis as a result serum ferritin levels raise in the body since it is the storage form of iron in body. This raised serum ferritin levels hence can be used as a prognostic tool for the patients.[5]
In a rural setting, due to monetary limitation, it is difficult to carry out expensive investigations for the diagnosis and prognosis of COVID-19 infection. As a result, a substantial amount of individuals with symptoms of COVID-19 do not visit the hospital and attain medical intervention. Availability of a cheaper alternative that can be easily accessible in the rural hospital and will provide effective results will prove beneficial to the medical fraternity and the patients too. Serum ferritin could serve this purpose in the rural settings and help to curb COVID-19 associated mortality.
In this study an attempt is being made to correlate serum ferritin levels with HRCT score, Neutrophil: lymphocyte ratio, anticipate the cytokine storm and analyse the prognosis of the patient. It will serve as an ideal tool for the management of these critically ill patients and thus reduce the mortality and morbidity associated.
The global pandemic SARS- COV-2 is distinguished by a diverse clinical course. Although the mass patients experience only mild symptoms, a major share advances to severe disease progression. Such that they may present with hypoxia initially or even respiratory distress. The considerable number of patients that presented with severe symptoms have worn out intensive care capacities to an unmatched range. Due to its unpredictable course and lack of sufficient predictors of the severity of COVID-19, parameters that enable to ensure the severity is essential Patients with PCR proven symptomatic COVID-19 infection hospitalized at our institution from 10th may 2020 10th may 2021 were analysed for baseline clinical and laboratory findings.
Study population, setting and data collection
Aim
Serum Ferritin and it’s correlation with severity of COVID-19 in terms of HRCT score, N: L Ratio and its Outcome.
Objectives
To access serum ferritin levels in COVID-19 patients having moderate to severe disease.
To correlate serum ferritin level with oxygen saturation, HRCT Score and need for oxygen- nasal versus NIV.
To correlate serum ferritin with other acute phase reactants.
To study the outcome of COVID-19 such as requirement of ventilator, mortality and ICU Stay.
Methods
Study population, Setting and Data Collection: -
Patients having symptoms of COVID-19 infection and were tested positive with Reverse Transcriptase Polymerase Chain Reaction, admitted in the ICU settings of Acharya Vinobha Bhave Rural Hospital, Sawangi, Wardha were enrolled in this study.
200 patients were ultimately identified and included in our study after receiving ethical clearance – IEC/2021/337.
Inclusion criteria
As per AIMS Criteria moderate/severe criteria.
Moderate criteria
Any one of the following
Respiratory rate >24 breaths per minute
Spo2 less than 94 percent on room air
Severe criteria
Any one of the following
Respiratory rate more than 30 breaths per minute
Saturation less than 90 percent on room air
Serum ferritin, HRCT, Serum neutrophil: lymphocyte ratio was done for all the enrolled patients on admission and all patients were admitted in the intensive care unit.
Exclusion criteria
Asymptomatic COVID infection.
Mild COVID infection
<18 years age excluded
Patients who were on steroids previously for any illness as it might affect the N: L Ratio.
Demographic Data, comorbidities, information, laboratory results and outcome was followed for all these 200 patients.
Laboratory measurements
Reverse Transcriptase Polymerase Chain Reaction (RTPCR) for SARS-CoV 2, collected from the 200 patients admitted in Acharya Vinoba Bhave hospital and testing carried out by The Clinical Laboratory of Jawaharlal Nehru Medical College, Sawangi has been included.
RTPCR detection of COVID-19 in the throat and nasal swabs was done. The laboratory has been authorized by the ICMR for conduction testing for COVID-19. RTPCR was done by Quant Studio 5 using meril COVID-19 onestep RTPCR kit.
The kit comprised of COVID-19 enzyme mix (lyophilized), COVID-19 primer probe mix, enzyme mix buffer, COVID-19 PCR positive control and COVID-19 negative control (DEPC treated H2O).
Serum ferritin was detected using the VITROS 5600 integrated system, that is aimed on the principle of electrochemiluminescence immunoassay. This kit consists of elecsys ferritin, ferritin reagent, and calset.
Study definition
Only Severe and Critical Patients were enrolled in the study who were admitted in intensive care unit.
Severe was defined as a patient who had shortness of breath with respiratory rate greater than 30 breaths/minute or had less than 93 percent oxygen saturation at room air on rest or pao2/fio2 less than 300 mm of hg.
The critical Patients were defined as the patients that had respiratory failure or shock or had any organ failure.
Statistics
To summarize the demographic data, we applied Descriptive statistics. Medians and interquartile ranges or counts and frequency or means with standard deviations were used to interpret the results. To detect the significant differences among stratifications One-way ANOVA was used and Software SPSS v23 was used to analyse the statistical data
One-way ANOVA was applied to detect significant differences among stratifications. Software SPSS v23 was used to scrutinize the statistical data.
Results
A total of 200 patients who were COVID-19 Positive by RT-PCR report of the Nasopharyngeal Swab and Admitted in ICU were enrolled in our cross sectional study.
HRCT Score, N:L Ratio and Outcome were significantly associated (p < 0.05) with Serum Ferritin (ng/mL) as shown in Figure 1 and Table 1.
Figure 1.
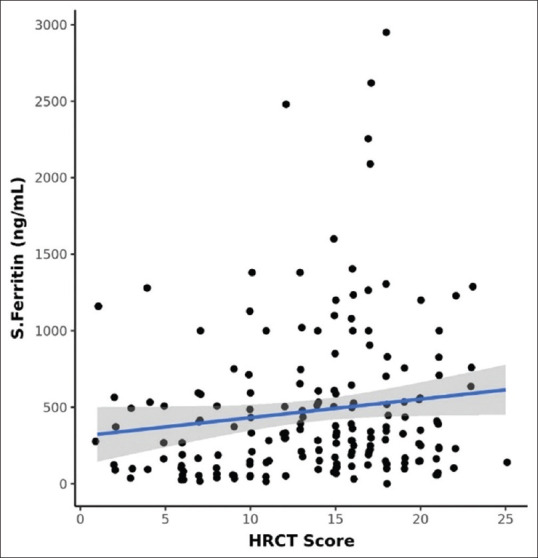
Scatter graph showing association of serum ferritin with HRCT score
Table 1.
Association between Serum Ferritin (ng/mL) and Parameters
| Parameters | Serum Ferritin (ng/mL) | P |
|---|---|---|
| HRCT Score*** | Correlation Coefficient (rho)=0.17 | 0.0181 |
| N: L Ratio*** | Correlation Coefficient (rho)=0.23 | 0.0021 |
| Outcome*** | 0.0072 | |
| Discharged | 438.43±490.23 | |
| Expired | 616.98±484.72 |
***Significant at P<0.05, 1Spearman Correlation, 2Wilcoxon-Mann-Whitney U Test
Table 2 depicts the association of serum ferritin with HRCT score suggesting that it is significantly associated.
Table 2.
Correlation between HRCT Score and Serum Ferritin (ng/mL) (n=200)
| Correlation | Spearman Correlation Coefficient | P |
|---|---|---|
| HRCT Score vs Serum Ferritin (ng/mL) | 0.2 | 0.018 |
The above scatterplot depicts the correlation between HRCT Score and Serum Ferritin [Figure 1].
Each Individual point represents individual cases. The general trend of the correlation between those two variables is represented by blue trendline and 95% confidence interval is shown by the shaded grey area.
To establish the correlation between the two variables Non-parametric tests (Spearman Correlation) were used as the variables were not distributed informally.
Also, a statistically significant (rho = 0.17, P = 0.018), weakly positive correlation was marked between HRCT Score and Serum ferritin (ng/mL).
For each 1 unit rise in HRCT Score, the Serum Ferritin (ng/mL) increases by 12.13 units.
Relatively, for each 1 unit increase in S. Ferritin (ng/mL), the HRCT Score increases by 0.00 units.
The above scatterplot establishes the correlation between N: L Ratio and Serum Ferritin [Figure 2].
Figure 2.
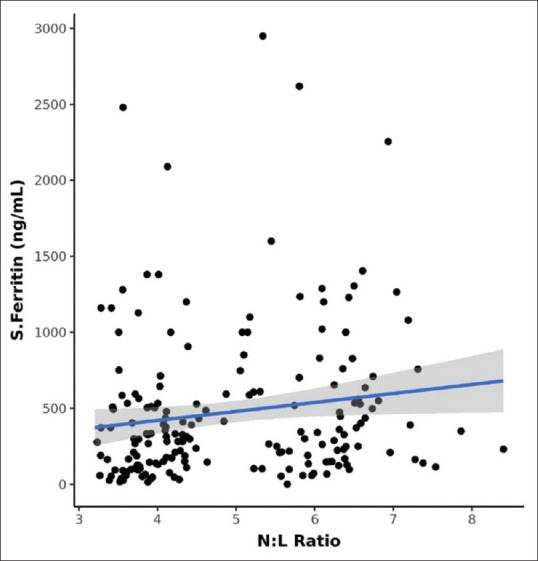
Scatter graph showing association of N: L ratio with serum ferritin
Each Individual point constitutes individual cases. The general trend of correlation between the two variables is marked by the blue trendline and 95% confidence interval of this trendline is indicated by the shaded grey area.
In order to explore the correlation between the two variables, Non-parametric tests (Spearman Correlation) were used, As they were not normally distributed.
A statistically significant (rho = 0.23, P = 0.002), weakly positive correlation between N: L Ratio and S. Ferritin (ng/mL) is demonstrated As shown in Table 3.
Table 3.
Correlation of N:L Ratio with Serum Ferritin
| Correlation | Spearman Correlation Coefficient | P |
|---|---|---|
| N: L Ratio vs Serum Ferritin (ng/mL) | 0.2 | 0.002 |
For every 1 unit increase in N: L Ratio, the S. Ferritin (ng/mL) increases by 59.10 units.
Conversely, for every 1 unit increase in S. Ferritin (ng/mL), the N: L Ratio increases by 0.00 units.
The graph [Figures 3 and 4] suggests association of serum ferritin and the outcome of these affected COVID-19 patients. The graph confirms the direct relation of serum ferritin levels with the outcome- discharge and mortality.
Figure 3.
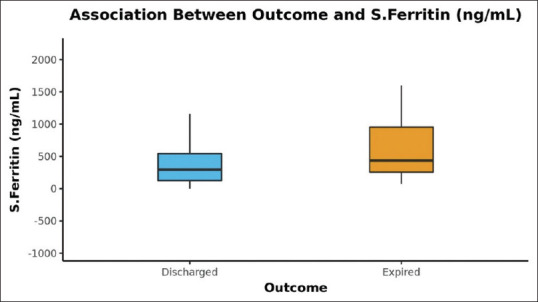
The bar graph in Figure 3 depicts the means of Serum Ferritin (ng/mL) in the 2 different groups (Discharged and Expired)
Figure 4.
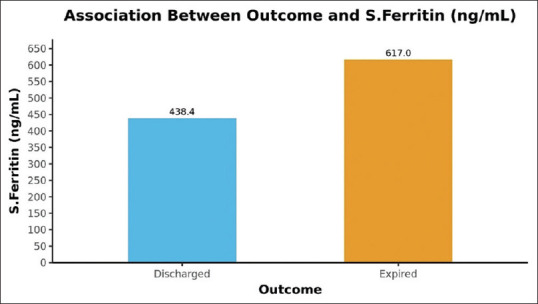
Bar Graph showing association of serum ferritin with outcome in Figure 4
Discussion
This single centre cross sectional study describes 200 patients with COVID-19 infection who were admitted in the ICU and had severe or critical condition. Serum ferritin levels were tested in all patients at admission. It is postulated that a multifactorial immune response might be related to the severity of COVID-19. The result of our study supports this postulate by indication of increasing serum ferritin levels with increase in severity of the disease. Thus we have established a connection between serum ferritin and the severity of COVID-19 disease in terms of increased HRCT Score, High N: L Ratio as well as clinical outcomes.
It was observed that higher serum ferritin were related to Higher N: L Ratio and higher CT severity score on HRCT Thorax. Our findings were different from a study done in Italy where ferritin was a predictor of severity but not mortality in a two centre study.[6] In various studies conducted throughout the world it was found that serum ferritin was one of the important markers out of inflammatory markers that can be used to determine the severity of COVID-19 however our study not only shows the association of serum ferritin with severity but also with morality in COVID-19 patients admitted in an intensive care unit.[7]
Through the study, it was observed that COVID-19 positive patients with low serum ferritin had mild symptoms and gradually recovered with symptomatic treatment alone, whereas patients who had raised serum ferritin level on admission eventually were hit by the cytokine storm and had to be treated as moderate to severe category patients with very high suspicion of morbidity and mortality which was consistent with other studies.[8]
Thus it could have been evidently stated that estimation of serum ferritin could have enabled us to anticipate this cytokine storm and administration of immunomodulators and anti- inflammatory medication in the right time, would have reduced the rate of development of associated mortality which needs further studies and trials to confirm.[9]
In a study conducted by Kumar S et al.[10] it was seen serum ferritin corelated with the severity of COVID-19 infection by a scoring system- PIRO scoring.
In a study conducted by Talwar et al.[11] it was established that interluelkin 6 was not correlated significantly with the outcome of intensive care unit patients who were COVID-19 positive. In the light of these findings and the findings of our study,serum ferritin can be an underrated marker which may be used in assessing outcome in COVID-19 although it’s utilization has been reduced in recent times with other inflammatory markers like interleukin 6 marking the pathway for treatment and prediction of outcome.However,further studies are required in order to fully establish potent markers of COVID-19.
We have established a linear association between serum ferritin and severity of COVID-19 patients therefore serum ferritin can be a forgotten biomarker which can be focused upon in intensive care units of COVID-19 while most clinicians only focus on biomarkers like C Reactive protein, interleukin 6 and D-dimer.
In a rural primary health care system many times due to lack of recent resources, investigations such as interleukin 6, d- dimer and CRP is not possible. During such times, carrying out simple serum ferritin test could help us understand the severity of COVID-19, its probable association with HRCT score and the related morbidity and mortality.[10] Hence, ferritin can prove pivotal in a rural setting.
Limitations
We have conducted that a cross sectional study only involving severe and critically ill patients of the intensive care unit. We have not included the treatment strategies in this study hence we cannot comment on the efficacy of various treatment regimens in COVID-19. Lastly, serum ferritin was not repeated serially hence we couldn’t report the serial ferritin levels during the recovery of COVID-19 patients.
Conclusion
Through our study we have concluded that serum ferritin is a good marker of severity for COVID-19 in an intensive care unit and can be correlated with HRCT Chest CT severity score N: L Ratio as well as clinical outcome. This is beneficial as by adding a simple test for serum ferritin analysis we can predict the course of disease in COVID-19 and design a tailored management approach.
Summary
COVID-19 has been a socio-economic burden in current times. Due to the associated mortality and morbidity it has become an important health concern.
Serum ferritin is an inexpensive and easily available biochemical investigation.
Due to its easy accessibility, serum ferritin can be used as an ideal prognostic marker for COVID-19 patients.
Through the study, it has been emphasized that ferritin not only suggests the patients to be positive for COVID-19 infection but the range of ferritin also allows to grade the severity of the cytokine storm associated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kappert K, Jahić A, Tauber R. Assessment of serum ferritin as a biomarker in COVID-19: Bystander or participant? Insights by comparison with other infectious and non-infectious diseases. Biomarkers. 2020:25616–25. doi: 10.1080/1354750X.2020.1797880. [DOI] [PubMed] [Google Scholar]
- 2.Vargas- Vargas M, Cortés-Rojo C. Ferritin levels and COVID-19. Rev Panam Salud Publica. 2020;44:e72. doi: 10.26633/RPSP.2020.72. doi: 10.26633/RPSP 2020.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin Z, Long F, Yang Y, Chen X, Xu L, Yang M. Serum ferritin as an independent risk factor for severity in COVID-19 patients. J Infect. 2020;81:647–79. doi: 10.1016/j.jinf.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomez- Pastora J, Weigand M, Kim J, Wu X, Strayer J, Palmer AF, et al. Hyperferritinemia in critically ill COVID-19 patients-Is ferritin the product of inflammation or a pathogenic mediator? Clin Chim Acta. 2020;509:249–51. doi: 10.1016/j.cca.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeng F, Huang Y, Guo Y, Yin M, Chen X, Xiao L, et al. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis. 2020;96:467–74. doi: 10.1016/j.ijid.2020.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carubbi F, Salvati L, Alunno A, Maggi F, Borghi E, Mariani R, et al. Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: Data from two Italian COVID-19 units. Sci Rep. 2021;11:4863. doi: 10.1038/s41598-021-83831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahat RK, Panda S, Rathore V, Swain S, Yadav L, Sah SP. The dynamics of inflammatory markers in coronavirus disease-2019 (COVID-19) patients: A systematic review and meta-analysis. Clin Epidemiol Glob Health. 2021;11:100727. doi: 10.1016/j.cegh.2021.100727. doi: 10.1016/j.cegh2021.100727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banchini F, Cattaneo GM, Capelli P. Serum ferritin levels in inflammation: A retrospective comparative analysis between COVID-19 and emergency surgical non-COVID-19 patients. World J Emerg Surg. 2021;16:9. doi: 10.1186/s13017-021-00354-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar S, Dronamraju S, Acharya S, Jaiswal P, Hulkoti V, Talwar D, et al. COVID-PIRO (predisposition, insult, response, organ dysfunction) score: A reliable predictor of outcomes in COVID-19 patients admitted in intensive care unit. Cureus. 2021;13:e18960. doi: 10.7759/cureus.18960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talwar D, Kumar S, Acharya S, Raisinghani N, Madaan S, Hulkoti V, et al. Interleukin 6 and Its Correlation with COVID-19 in Terms of Outcomes in an Intensive Care Unit of a Rural Hospital: A Cross-sectional Study. Indian J Crit Care Med. 2022;261:39–42. doi: 10.5005/jp-journals-10071-24075. [DOI] [PMC free article] [PubMed] [Google Scholar]


