Abstract
Background
Many transgender women and men undergo gender-affirming surgeries. Existing work shows that early surgery outcomes are generally positive, suggesting high surgical satisfaction and positive quality of life outcomes. Less work, however, examines these outcomes in the longer-term.
Aims
To conduct a systematic literature review into the longer-term (i.e., ≥ 1 year) surgical satisfaction and quality of outcomes following various forms of gender-affirming surgery in transgender populations. Specifically, we aim to examine research on such outcomes at least one-year post gender-affirming chest, genital, facial, vocal cord, and Adam’s apple removal surgeries.
Methods
Studies were identified through Google Scholar, PsycINFO, Scopus, and PubMed databases, as well as through Google Scholar search alerts. We considered all studies published until October 2021. Two reviewers extracted data from suitable studies using Covidence. Both reviewers also independently assessed the identified studies’ risk of bias and strength of evidence.
Results
Seventy-nine low quality (e.g., small sample sizes, lack of control/comparison groups) studies suggest that most transgender patients are satisfied with surgical outcomes when assessed at least one-year post-surgery. Low quality research also indicates that transgender women and men typically report positive psychological and sexual wellbeing post-surgery, and similar wellbeing outcomes as those who have not had surgery.
Discussion
To the best of our knowledge, this literature review is the first to critically summarize and evaluate all published studies on the longer-term quality of life outcomes following chest, genital, facial, voice and Adam’s apple removal surgeries for transgender women and men. While the results suggest promising surgical satisfaction and quality of life outcomes following surgery, many studies only draw on small samples, and most studies do not allow for causal conclusions. Further, few studies have compared surgical outcomes between transgender women and men. We conclude by offering concrete suggestions for future research.
Keywords: Long-term outcomes, quality of life; systematic, review, surgery, surgical satisfaction, transgender
Introduction
Many transgender men and women undergo surgeries to affirm their gender identities, many of which permanently alter their physical characteristics (Heath and Wynne, 2019). Studies examining surgical satisfaction suggest that surgery may be immediately beneficial for transgender men and women’s quality of life (Satterwhite et al., 2017; van de Grift et al., 2017). However, the literature concerning the longer-term effects of surgery on transgender people’s quality of life is still in its infancy, and often scattered across multiple disciplines. Thus, such a systematic literature review is needed to determine whether transgender men and women continue to report satisfaction and positive quality of life in the longer-term (i.e., at least one year post-surgery).
Many transgender women and men undergo surgeries that affirm their gender identities by altering physical characteristics, including secondary sex characteristics and in some cases, genitalia. Transgender men may undergo reduction mammaplasty or chest reconstructive surgery to alter their chests, and may undergo phalloplasty or metoidioplasty (with perhaps additional erectile prosthesis surgery) to alter their genitalia (Heath and Wynne, 2019). In contrast, transgender women may undergo augmentation mammaplasty to enhance their breasts, and/or may undergo vaginoplasty, clitoroplasty, labioplasty, orchiectomy, or vulvoplasty to alter their genitalia (or a combination of two or three). Transgender men and women may also undergo facial masculinization and feminization surgeries, respectively. Furthermore, if voices are not satisfactorily affirmed through hormone treatment, transgender women and men may undergo vocal cord surgeries, such as type III thyroplasty for transgender men, or glottoplasty and cricothyroid approximation for transgender women. Some transgender women choose to undergo chondrolaryngoplasty to reduce their laryngeal prominence (i.e., their Adam’s apple). It should be noted, however, that not all transgender men and women undergo surgery (or hormone treatment), and that the need or desire for gender-affirming medical treatment differs from person to person (Nieder et al., 2020).
To date, there are few reviews (e.g., Ardebili et al., 2020; Defreyne et al., 2017; Murad et al., 2010; Passos et al., 2020) that summarize quality of life outcomes following gender-affirming surgeries. There are, however, a handful of informative reviews focusing on specific types of gender-affirming surgery, including phalloplasty (Morrison et al., 2015; Remington et al., 2018)and vaginoplasty (Horbach et al., 2015; Manrique et al., 2018). Furthermore, a recent review by Oles et al. (2022) examined outcomes on chest, facial, and vocal cord surgeries. The general consensus across reviews is that surgery improves transgender men and women’s quality of life. These reviews do not explicitly delve into the longer-term quality of life outcomes following gender-affirming surgery, however, or simultaneously consider and compare outcomes for each gender-affirming surgery type in transgender men and women.
To the best of our knowledge, there are no current articles that summarize the literature solely on the longer-term (i.e., ≥ 1 year) quality of life outcomes following various types of gender-affirming surgery. In order to determine what timeframe best represented the “longer-term” we looked to the literature and established that the one year time point was significant. Patients tend to report positive transitioning outcomes within the first 12 months post-surgery, regardless of whether they have adverse transitioning outcomes in the longer-term (De Cuypere et al., 2006; Wierckx et al., 2012). In a longer-term evaluation of transgender women’s health and wellbeing, Lindqvist et al. (2017) found that transgender women reported increased health-related quality of life postoperatively, but that their health-related quality of life subsequently declined in the following years. Hence, early evaluations (i.e., < 1 year), while informative, need to be supplemented with information about longer-term functioning.
In the current article, then, we aim to examine and synthesize the literature on the longer-term quality of life outcomes for transgender women and men following each type of gender-affirming surgery. Cella (1994) defined quality of life as a subjective and multidimensional construct reflecting physical, emotional, and social wellbeing, as well as functional ability. Thus, we define quality of life outcomes as any outcomes reported by transgender men and women themselves in the physical (including physical wellbeing and functional ability; i.e., surgical satisfaction, regret and health-related quality of life), psychological (including emotional and social wellbeing; i.e., psychosocial wellbeing, gender dysphoria, life satisfaction, body image satisfaction, depression and anxiety, happiness, emotional stability, and self-esteem), and sexual (i.e., sexual function and wellbeing) domains. We chose to look at these three domains as they fit within Cella’s (1994) definition of quality of life, and because they are the most common areas investigated in the literature. Studies/outcomes focusing on non-binary people will not be discussed, as non-binary people face unique obstacles to treatment (Clark et al., 2018), and the effect of surgery on non-binary people’s quality of life warrants a separate review.
Methods
The present review’s writing was guided by the Preferred Reported Items for Systematic reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021). We did not register our review in the International Prospective Register of Systematic Reviews (PROSPERO), as it is a literature review (and therefore is not eligible for registration; Center for Reviews and Dissemination at the University of York, 2016).
Search strategy and eligibility criteria
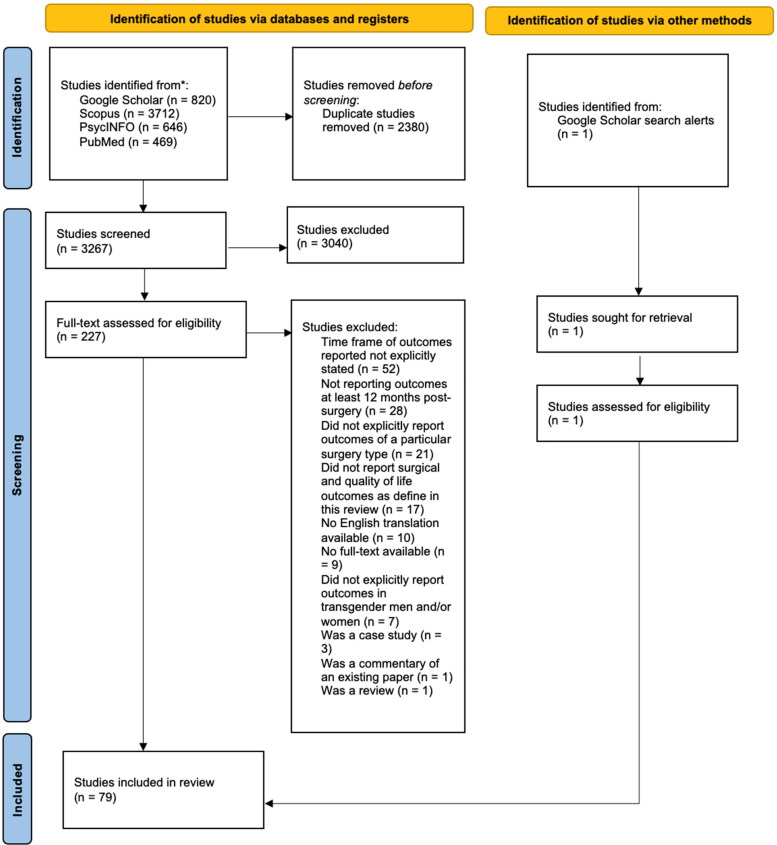
A two-step search strategy was employed to identify peer-reviewed articles for inclusion in this review (see Figure 1). First, two reviewers (CJ and FKB) conducted literature searches on Google Scholar, PsycINFO, Scopus, and PubMed to select English language articles that reported quality of life outcomes (measured at least one-year post-surgery) for transgender women and men who had previously undergone chest, genital, facial, vocal cord and/or Adam’s apple removal surgeries. The latest literature search was conducted in August 2021. Then, from August to October 2021, additional eligible articles were attained from Google Scholar search alerts (based upon the following search terms: “transgender”, “transgender surgery”, or “transgender transitioning outcomes”). As such, studies published until October 2021 were considered for this review (except for case studies which were excluded from consideration). Any synonyms of the term, “transgender” (e.g., “trans”, “transsexual1”) were employed in the literature search to maximize search results (see Table 1). Both British and American spellings of search terms (e.g., “feminisation” and “feminization”, respectively) were employed in our literature search (see Table 1).
Figure 1.
Flowchart of the literature search process.
Table 1.
Search terms employed in the literature search.
| Search group | Search terms |
|---|---|
| Population | “transgender”, “trans”, “transsexual”, “trans male”, “trans female”, “trans women”, “trans men”, “transgender male”, “transgender female” |
| Outcomes |
“long-term outcomes”, “quality of life”, “psychological outcomes”, “outcomes”, “satisfaction”, “psychosocial outcomes”, “depression”, “anxiety”, “mental health”, “gender dysphoria”, “gender identity disorder”, “suicidal ideation”, “body image”, “wellbeing”, “well-being”, “sexual function”, “happiness”, “emotional stability”, “self-esteem”, “regret” |
| Surgical procedures | “chest surgery”, “genital surgery”, “chest masculinizing surgery”, “chest masculinizing surgery”, “chest feminization surgery”, “chest feminization surgery”, “mammoplasty”, “mammaplasty”, “vaginoplasty”, “vulvoplasty”, “phalloplasty”, “penile prosthesis surgery”, “facial surgery”, “facial feminization surgery” “facial feminization surgery”, “facial masculinization surgery”, “facial masculinization surgery”, “facial surgery transgender”, “facial surgery trans”, “genital reassignment surgery”, “voice feminisation surgery”, “voice masculinisation surgery”, “voice feminization surgery”, “voice masculinization surgery”, “glottoplasty”, “orchiectomy” |
Study selection and data extraction
A four-step strategy was employed to select and extract study data for inclusion in this review (see Figure 1). First, all search results were imported onto Covidence to screen for duplicates (note that one reviewer (CJ) also manually screened for additional duplicates not already captured by the software). Next, two reviewers (CJ and a research assistant (RA)) independently screened both titles and abstracts of the remaining studies on Covidence. Both reviewers then independently screened the full text of all eligible articles to ensure that they reported quality of life outcomes at least 12 months after surgery. Any discrepancies were resolved through discussion between both reviewers. One reviewer (CJ) also searched the reference list of all eligible articles was for any additional relevant studies. Two reviewers (CJ and RA) extracted the data from each suitable study (these data are shown in the Appendix, Supplementary material).
Study quality assessment
All studies we reviewed were non-randomized (i.e., were not clinical randomized control trials) – likely because of the nature of the phenomenon under investigation, where there may be feasibility and ethical concerns about assigning people to control vs surgical conditions. As such, two reviewers (CJ and RA) independently analyzed the risk of bias from the studies retrieved using the Risk Of Bias In Non-randomized Studies - of Interventions (ROBINS-I) tool (Sterne et al., 2016). Risk of bias was graded using one of the following five classifications: no information (whereby there is insufficient evidence to classify a study’s risk of bias), then low, moderate, serious, and critical risk of bias. Sample size and whether a control/comparison group was included were both considered when grading the studies’ risk of bias. Studies that employed less than 10 participants with a pre-measure were automatically graded as having a critical risk of bias. Studies that employed a sample size of over 50 participants, but did not have a control/comparison group; or a sample size of less than 50 participants, but employed a control/comparison group, were classified as having a moderate risk of bias. Additionally, both reviewers analyzed the strength of evidence from the studies reviewed using the grading scheme recommended by the United States Agency for Healthcare Research (Berkman et al., 2015). We graded the strength of the evidence for each quality of life outcome using one of the following four classifications: insufficient (whereby there is insufficient evidence to classify the strength of evidence for an outcome), low, moderate, and high. Higher classifications indicate higher confidence that the estimated effect lies close to the true effect. Like the grading involved for the risk of bias, sample size and whether a control/comparison group was included were both considered when grading the studies’ risk of bias. Findings for a certain quality of life outcome that came from only one study that had a sample size of less than 100 participants were automatically classified as having low strength of evidence with high study limitations. Findings for an outcome construct that were only classified as having high strength of evidence if they came from both retrospective and prospective studies that have a combined sample size of over 1000 participants.
Results
Our literature search yielded 79 unique studies on quality of life outcomes for transgender people following gender-affirming surgeries. The latest study we found was made available online in October 2021 (Day et al., 2021). At the time of writing, there were no studies identified (meeting our criteria) that investigated the longer-term quality of life outcomes of either facial masculinization surgery or vocal cord surgery in transgender men (e.g., type III thyroplasty). Additionally, we did not identify any studies that examined the longer-term quality of life outcomes of transgender women who underwent orchiectomy.
Of the 79 studies found, two investigated outcomes of multiple surgery types (De Cuypere et al., 2005; Selvaggi et al., 2007). Additionally, only nine studies employed prospective research methods (Aires et al., 2020; Aires et al., 2021; et al., 2017; Casado et al., 2017; Kelly et al., 2019; La Padula et al., 2019; Mora et al., 2018; van de Grift et al., 2017; Weigert et al., 2013). A further six studies compared their outcomes to transgender men and women who did not undergo surgery, and/or a cisgender population who completed the same measures (Ainsworth and Spiegel, 2010; Fleming et al., 1982; Küenzlen et al., 2020; Meister et al., 2017; Papadopulos et al., 2021; van de Grift et al., 2018). Thus, given the remaining large number of retrospective studies that did not employ control/comparison groups, only two studies (Mora et al., 2018; Robinson et al., 2021) were classified as having a mild risk of bias (this will be further elaborated on in the Discussion section; see Appendix for full breakdown).
Chest surgery
In transgender men (mastectomy or reduction mammoplasty)
We identified four small studies (Antoszewski et al., 2012; Day et al., 2021; De Cuypere et al., 2005; van de Grift et al., 2018) meeting our criteria. These looked at: satisfaction with surgery, surgical regret, and health-related quality of life.
Satisfaction with surgery. The results from two retrospective quantitative studies (Antoszewski et al., 2012; Day et al., 2021) suggested that most transgender men were satisfied with the surgical outcomes of their chest surgeries. Another retrospective quantitative study by De Cuypere et al. (2005) revealed that no participant (in their 21 participant sample) reported dissatisfaction with their mastectomy. van de Grift et al. (2018) study reported that postoperative 36 participants (i.e., transgender men who underwent mastectomy) reported greater satisfaction with their genitalia than their preoperative counterparts (i.e., transgender men who did not underwent mastectomy at the time of study).
Surgical regret. Antoszewski et al. (2012) and Day et al. (2021) found that none (out of 98 participants) and two (out of 84 participants) transgender men regretted undergoing chest-affirming surgery, respectively.
Psychological and social functioning. Contrary to the surgical satisfaction findings reported by van de Grift et al. (2018), psychological and social functioning did not differ between preoperative and postoperative transgender men; they were moderately high in both cases.
In transgender women (augmentation mammoplasty)
Five retrospective quantitative studies (Balakrishnan et al., 2020; De Cuypere et al., 2005; Fakin et al., 2019; Kanhai et al., 2000; Tirrell et al., 2021) and one prospective quantitative study (Weigert et al., 2013) were identified. These examined: satisfaction with surgery, psychosocial wellbeing, and sexual wellbeing.
Satisfaction with surgery. Across all studies transgender women were largely satisfied with the surgical outcomes of their chest surgeries. Fakin et al. (2019) also found that women who underwent augmentation mammaplasty more (relative to less) recently were more likely to report higher satisfaction rates. These results potentially reflect improved surgical procedures over time (Fakin et al., 2019). The most common reason for any dissatisfaction (we note that dissatisfaction was rare) was that breasts were too small or big (Fakin et al., 2019; Kanhai et al., 2000).
Psychosocial and sexual wellbeing. A single study (Weigert et al., 2013) investigated the longer-term effects of augmentation mammoplasty on psychosocial wellbeing and sexual wellbeing. Transgender women reported improvements in both their psychosocial and sexual wellbeing from pre- to four and 12 months + post-surgery (Weigert et al., 2013).
Genital surgery
In transgender men (scrotoplasty, hysterectomy, phalloplasty, metoidioplasty, and penile prosthesis surgery). We identified twenty-eight studies that met our criteria. These examined: satisfaction with surgery, surgical regret, sexual wellbeing, body image, self-esteem, life satisfaction, levels of depression and anxiety, happiness, and emotional stability.
Satisfaction with surgery. Twenty-two retrospective quantitative studies (Akhoondinasab et al., 2020; Dabernig et al., 2006; De Cuypere et al., 2005; de Rooij et al., 2021; Djordjevic and Bizic, 2013; Djordjevic et al., 2009; Djordjevic et al., 2019; Falcone et al., 2018; Fleming et al., 1982; Garaffa et al., 2010; Leriche et al., 2008; Neuville et al., 2021; Papadopulos et al., 2021; Perovic and Djordjevic, 2003; Pigot et al., 2020; Schaff and Papadopulos, 2009; Song et al., 2011; Staud et al., 2021; Timsit et al., 2005; Van Caenegem et al., 2013; van de Grift et al., 2017; van de Grift et al., 2019) found that the majority of transgender men (if not, all) were satisfied with the outcomes of their genital surgeries. A further retrospective qualitative study (and the only study on scrotoplasty we identified to date) revealed that all 240 transgender men were satisfied with outcomes of their scrotoplasty (Selvaggi et al., 2009).
Surgical regret. Out of four studies examining surgical regret (Garcia et al., 2014; Neuville et al., 2021; Pigot et al., 2020; Song et al., 2011), only one participant in one study (total N = 13; Neuville et al., 2021) reported regret due to dissatisfaction with surgical outcomes.
Sexual wellbeing. The results of 11 studies suggest that transgender men experience positive sexual wellbeing outcomes after undergoing genital surgery. Eight studies (De Cuypere et al., 2005; Falcone et al., 2018, Garcia et al., 2014, Leriche et al., 2008, Pigot et al., 2020, Schaff and Papadopulos 2009; Selvaggi et al., 2007; Song et al., 2011) reported that at least half of their respective transgender male participant samples were satisfied with their sexual functioning (e.g., with orgasm, and during sex and masturbation). Dabernig et al. (2006) and Küenzlen et al. (2020) found that no participant (Ns = 5 and 20, respectively) reported difficulties engaging in sexual intercourse. Similar outcomes were observed in Djordjevic and Bizic (2013) and Djordjevic et al. (2019) studies on metoidioplasty and penile prosthesis surgery, respectively. Only de Rooij et al. (2021) and van de Grift et al. (2019) reported relatively low rates of satisfaction with sexual functioning post genital surgery (34 and 36%, respectively). Despite this, both studies revealed participants who underwent metoidioplasty reported greater rates of satisfaction with sexual functioning than those who underwent phalloplasty.
Furthermore, five studies (Fleming et al., 1982; Papadopulos et al., 2021; Robinson et al., 2021; Song et al., 2011; van de Grift et al., 2017) demonstrated that transgender men were predominantly reported positive genital self-image post-surgery.
Self-esteem. To date, three retrospective quantitative studies suggest that transgender men typically report positive self-esteem outcomes following genital surgery (hysterectomy, metoidioplasty, and phalloplasty). Specifically, Fleming et al. (1982) and Papadopulos et al. (2021) both found that all transgender men in their studies (Ns = 22 and 32, respectively) reported high levels of self-esteem following genital surgery. Pigot et al. (2020) found that most of their 40 participants reported that their levels of self-esteem improved post-surgery.
Life satisfaction. van de Grift et al. (2017) found that 21 transgender men did not report a decrease in life satisfaction from pre- to post-surgery (rather, their levels of life satisfaction remained relatively high from pre to post-surgery). Further, both Küenzlen et al. (2020) and Papadopulos et al. (2021) found that the post-surgery transgender men reported moderate levels of life satisfaction, similar to those found in the German general cisgender population (i.e., those whose gender identity matches their biological sex; Henrich and Herschbach, 2000).
Levels of depression and anxiety. van de Grift et al. (2017) found that participants’ depression and anxiety levels remained low from pre to post-surgery. Additionally, both van de Grift et al. (2017) and Papadopulos et al. (2021) found that their participants levels of depression and anxiety similar to transgender men in previous studies (Löwe et al., 2010; van de Grift et al., 2017, van de Grift et al., 2018), and the German general cisgender population used in van de Grift et al.’s (2017) study above.
Happiness. The study by van de Grift et al. (2017) is the only one we found to have examined transgender men’s happiness levels after one year of undergoing genital surgery. Results revealed that transgender men’s happiness levels significantly improved from pre to post-surgery.
Emotional stability. In one study (Papadopulos et al., 2021) transgender men reported moderate emotional stability post-surgery, similar to levels reported by the German general cisgender population (Fahrenberg et al., 2001).
In transgender women (clitoroplasty, labioplasty, orchiectomy, vaginoplasty, and vulvoplasty)
We identified twenty retrospective quantitative studies and one retrospective qualitative study (Rehman et al., 1999) that examined longer-term outcomes following genital surgery in transgender women: satisfaction with surgery, surgical regret, sexual wellbeing, life satisfaction, happiness, depression, and gender dysphoria.
Satisfaction with surgery. The results of twenty-four studies indicate that transgender women are generally satisfied with the surgical outcomes of their genital surgeries (Bouman et al., 2016; di Summa et al., 2019; De Cuypere et al., 2005; Hess et al., 2018; Imbimbo et al., 2009; Loree et al., 2020; Massie et al., 2018; Perovic et al., 2000; Sigurjónsson et al., 2017; Small, 1987; Tavakkoli Tabassi et al., 2015; van Noort and Nicolai, 1993; Wagner et al., 2010; Wei et al., 2018). In six studies, all participants were satisfied with outcomes of the genital surgeries (Amend et al., 2013; Dessy et al., 2014; Eldh 1993; Kim et al., 2009; Özkan et al., 2018; van der Sluis et al., 2020). Other studies found that transgender women were satisfied with the esthetic and functional outcomes of their vaginoplasty (Buncamper et al., 2015; Kaushik et al., 2019; Thalaivirithan et al., 2018; van der Sluis et al., 2016). Finally, Bouman et al. (2016), Manrique et al. (2018), Morrison et al. (2015), and van der Sluis et al. (2016) all found that transgender women were generally satisfied with the appearance of their genitals after vaginoplasty.
Surgical regret. Regret was measured in four studies. Rates of regret were extremely small: Amend et al. (2013) and Imbimbo et al. (2009) found that only one (four percent) and eight (six percent) participants regretted undergoing genital surgery, respectively. In two other studies, there were no reports of regret (Tavakkoli Tabassi et al., 2015; van Noort and Nicolai, 1993).
Sexual wellbeing. We found 24 studies providing positive findings about whether transgender women report positive or negative sexual wellbeing post genital surgery. Seven studies demonstrated that transgender women reported good sexual functioning post-surgery (Dessy et al., 2014; di Summa et al., 2019; Eldh, 1993; Hess et al., 2018; Rehman et al., 1999; van Noort and Nicolai, 1993; Wei et al., 2018). Thalaivirithan et al. (2018) and Wei et al. (2018) found that transgender women reported high satisfaction with their sex lives overall. Three studies demonstrated that no transgender woman reported experiencing pain or discomfort during sex (Amend et al., 2013; Blanchard et al., 1987; Sigurjónsson et al., 2017), with an additional ten studies indicating that most transgender women were able to orgasm post-surgery (di Summa et al., 2019; Kim et al., 2009; Loree et al., 2020; Massie et al., 2018; Perovic et al., 2000; Selvaggi et al., 2007; Seyed-Forootan et al., 2018; Sigurjónsson et al., 2017; Wei et al. 2018). Hess et al. (2018) found that their 119 transgender women sample reported experiencing more frequent orgasms after undergoing vaginoplasty.
Life satisfaction. We found three studies (that together suggest that most transgender women reported high levels of life satisfaction following vaginoplasty (Bouman et al., 2016; Rehman et al., 1999; van der Sluis et al., 2016; Ns = 31, 28, and 9, respectively).
Happiness. Three studies showed that transgender women did not report low levels of happiness following genital surgery. That is, Rehman et al. (1999) in their sample that all bar one transgender woman who underwent various types of female-affirming genital surgery (vaginoplasty, clitoroplasty, labioplasty) reported having high satisfaction with their lives. Further, later studies by Bouman et al. (2016) and van der Sluis et al. (2016) revealed that transgender women who underwent vaginoplasty reported moderately high levels of happiness (Ns = 31 and 9, respectively)
Depression. To date, one study showed that 30 transgender women reported generally reported low levels of depression 18 months (on average) after undergoing vaginoplasty and clitoroplasty (Thalaivirithan et al., 2018).
Gender dysphoria. A single study by Massie et al. (2018) found that the majority of 66 transgender women surveyed reported that their gender dysphoria was resolved following genital surgery.
Facial surgery
In transgender women (facial feminization surgery, including rhinoplasty)
Five retrospective quantitative studies (Ainsworth and Spiegel, 2010; Bellinga et al., 2017; Raffaini et al., 2016, Raffaini et al., 2019; Telang, 2020) and one prospective quantitative study (La Padula et al., 2019) examined transgender women’s: satisfaction with surgery, health-related quality of life, life satisfaction, happiness, gender incongruence, and experiences of misgendering.
Satisfaction with surgery. Three studies suggest that transgender women were generally satisfied with their facial surgical outcomes (Ainsworth and Spiegel, 2010; Raffaini et al., 2019; Telang 2020). Ainsworth and Spiegel, (2010) found, in their sample of 75 women, that women who had undergone facial feminization surgery reported higher satisfaction with their facial features than those who had not undergone facial surgery. Another study by Bellinga et al. (2017) on the longer-term outcomes following rhinoplasty revealed that their sample of 200 transgender women were satisfied with surgical outcomes on average, and perceived their noses as more feminine than they were prior to surgery.
Health-related quality of life. Three studies suggest positive longer-term health-related quality of life outcomes of facial feminization surgery (Ainsworth and Spiegel 2010; Raffaini et al., 2016, Raffaini et al., 2019). Ainsworth and Spiegel, (2010) found that transgender women who had undergone facial feminization surgery, other gender-affirming surgeries, or both, reported better health-related quality of life outcomes than those who had not undergone any gender-affirming surgery. There were no significant differences in health-related quality of life, however, between women who had undergone different surgery types (facial and/or other gender-affirming surgeries; Ainsworth and Spiegel 2010). Raffaini et al. (2016, 2019) also found that transgender women reported improvements in their quality of life when asked so post-surgery (Ns = 49 and 28, respectively).
Life satisfaction and happiness. Only one study has examined transgender women’s life satisfaction and happiness in the longer-term following facial feminization surgery. La Padula et al. (2019) found that their sample of 25 transgender women reported improvements in their levels of life satisfaction and happiness from pre- to post-surgery.
Gender incongruence and misgendering. Telang (2020) found that their sample of 220 transgender women reported that felt less gender incongruent following facial feminization surgery, and reported that more people referred to them by their correct she/her pronouns (i.e., participants reported less misgendering).
Vocal cord surgery
In transgender women (glottoplasty or cricothyroid approximation)
Three retrospective quantitative (Matai et al., 2003; Meister et al., 2017; Yang et al., 2002) and five prospective quantitative studies (Aires et al., 2021; Casado et al., 2017; Kelly et al., 2019; Mora et al., 2018; Yılmaz et al., 2021) examined longer-term outcomes of vocal cord surgery. Outcomes included: satisfaction with surgery, self-perceived voice femininity, life satisfaction, and voice-related quality of life.
Satisfaction with surgery. Seven studies found that transgender women were generally satisfied with the outcomes of their vocal cord surgeries (Casado et al., 2017; Kelly et al., 2019; Matai, et al., 2003; Meister et al., 2017; Mora et al., 2018; Yang et al., 2002; Yılmaz et al., 2021).
Five studies examined whether transgender women perceived their voices as feminine (vs masculine) following voice surgery. Yang et al. (2002) and Yılmaz et al. (2021) found that more than half of participants perceived their voices as feminine post-surgery (Ns = 20 and 28, respectively). Aires et al. (2021), Casado et al. (2017), and Kelly et al. (2019) report that their samples of 15, 18, and 24 transgender women, respectively, perceived their voices as more feminine post-surgery (compared to pre surgery).
Life satisfaction. Meister et al. (2017) is the only study that explored transgender women’s longer-term quality of life following vocal cord surgery. In contrast to the positive outcomes reported in the other studies in this section, Meister et al. (2017) found that the 21 women in their sample reported that they were generally dissatisfied with their relationships with their friends, acquaintances, and relatives after undergoing vocal cord surgery (Meister et al., 2017).
Voice-related quality of life. Both Aires et al. (2021) and Mora et al. (2018; N = 51) found that transgender women reported improvements in their voice-related quality of life from pre- to post-surgery.
Adam’s apple removal surgery (chondrolaryngoplasty) in transgender women
At present, Aires et al. (2020) prospective quantitative study was the only study we identified that investigated the longer-term outcomes of transgender women who had undergone Adam’s apple removal surgery. This study’s results revealed that a sample of seven transgender women who underwent chondrolaryngoplasty were more satisfied with the esthetic appearance of their laryngeal prominence after surgery than before (i.e., the surgery was successful in reducing the prominence of their Adam’s apples), and that undergoing the surgery did not cause any damage to their vocals.
Discussion
Summary of findings
It is widely claimed that gender-affirming surgeries can help establish positive quality of life outcomes in transgender men and women (Heath and Wynne, 2019). The present review aimed to critically examine the literature on outcomes reported by transgender women and men at least 12 months post-surgery to establish whether this claim is borne out by the data. In particular, we aimed to investigate whether undergoing gender-affirming surgeries affects transgender men and women’s quality of life and whether any effects are dependent on the type of surgery undertaken. This review considered all research found in four scholarly databases (Google Scholar, PsycINFO, Scopus, and PubMed) and Google Scholar search alerts published until October 2021. The studies examined in the present review converge around the conclusion that transgender patients who undergo gender-affirming surgeries generally report positive surgical satisfaction and quality of life outcomes in the longer-term (see Table 2 for summary of findings). Yet, not all longer-term outcomes following gender-affirming surgery reported in this review were positive. A small minority of transgender men and women among the studies reviewed reported low levels of surgical satisfaction (e.g., Ainsworth and Spiegel, 2010; Bouman et al., 2016; Fakin et al., 2019; Leriche et al., 2008). A small minority of transgender women and men also reported regretting having surgery (e.g., Amend et al., 2013; Antoszewski et al., 2012; Garcia et al., 2014; Neuville et al., 2021). In terms of specific surgeries, Meister et al. (2017) found that transgender women who underwent vocal cord surgery reported lower vocal and life satisfaction levels than cisgender controls. This result, however, can be contrasted with work by Kelly et al. (2019) and Mora et al. (2018) who found that transgender women reported improvements in their vocal satisfaction from pre to post vocal cord surgery. Overall, then, our review presents findings that are concordant with previous reviews on the shorter term outcomes (i.e., < 12 months) of gender-affirming surgeries (see Murad et al., 2010; Passos et al., 2020; Oles et al., 2022); transgender men and women typically report positive outcomes following surgery, and at worst, report a quality of life no different from those who have not had surgery, or cisgender comparator groups. Our findings therefore suggest that most transgender men and women continue to report positive wellbeing outcomes 12 months after undergoing surgery (in contrast so some past work; see Lindqvist et al., 2017). Multiple studies within this review, however, were rated as having serious or critical risk of bias (see Appendix for further information). Further, the strength of their evidence from all but two outcomes (i.e., surgical satisfaction and sexual wellbeing) were low or moderate (see Table 2 and the Limitations section below).
Table 2.
Summary of findings.
| Outcome | Number of studies (n)1 | Summary of findings1 | Strength of Evidence |
|---|---|---|---|
| Surgical satisfaction |
|
Direct evidence with medium study limitations suggests that most transgender men and women report satisfaction with their chest and genital surgeries. Similar outcomes were reported in transgender women who underwent facial, vocal cord, and Adam’s apple removal surgeries. | High |
| Surgical regret |
|
Direct evidence with medium study limitations suggests that the vast majority of transgender women and men do not regret undergoing chest/genital surgery. | Medium |
| Psychological and social functioning |
|
Direct evidence with high study limitations suggests that transgender men who underwent chest surgery reported moderately high levels of psychological and social functioning comparable to transgender men who did not undergo chest surgery | Low |
| Psychosocial wellbeing |
|
Direct evidence with high study limitations suggests transgender women overall reported improvements in their psychosocial wellbeing from pre- to post-surgery | Low |
| Sexual wellbeing |
|
Direct evidence with medium study limitations suggests that most transgender women report positive sexual wellbeing outcomes following chest and genital surgeries. Similar inferences also apply to transgender men who underwent genital surgery | High |
| Self-esteem |
|
Direct evidence with medium study limitations suggests transgender men who undergo genital surgery report high and/or improved self-esteem levels. | Medium |
| Life satisfaction |
|
Direct evidence with medium study limitations suggests that most transgender men and women do not report having poor life satisfaction following genital surgery. Similar inferences also apply to transgender women who underwent facial and/or voice surgeries | Medium |
| Depression and anxiety |
|
Direct evidence with medium study limitations suggests transgender men who underwent genital surgery do not report having high levels of depression and anxiety. Additionally, these levels were comparable with normative data (e.g., the German general population). Further, transgender women who underwent genital surgery report low levels of depression |
Medium |
| Happiness |
|
Direct evidence with medium study limitations suggests transgender men women report having positive happiness levels following genital surgery. Similar results were observed in transgender women who underwent facial surgery. | Medium |
| Gender dysphoria | One retrospective quantitative study on transgender women who underwent genital surgery (66) | Direct evidence with high study limitations suggests that most transgender women who undergo chest surgery reported that their gender dysphoria was resolved. | Low |
| Gender incongruence and misgendering | One retrospective quantitative study on transgender women who underwent facial surgery (220) | Direct evidence with medium study limitations suggests that most transgender women who undergo facial surgery report feeling less incongruent with their gender identity, as well as fewer instances of misgendering. | Medium |
| Emotional stability | One retrospective quantitative study on transgender men who underwent genital surgery (32) | Direct evidence with high study limitations suggests transgender men who undergo genital surgery have a “well-balanced” emotional stability comparable to that of the German general population. | Low |
| Health-related quality of life | Three retrospective quantitative studies on transgender women who underwent facial surgery (157) | Direct evidence with medium study limitations suggests that transgender women who undergo facial surgery report positive and/or improved health-related quality of life outcomes | Medium |
| Voice-related quality of life | Two prospective quantitative studies on transgender women who underwent vocal cord surgery (58) | Direct evidence with medium study limitations suggests that transgender women reported that their voice-related quality life improving after undergoing voice surgery | Medium |
1. Due to the similarity of study designs and findings across all studies reviewed, the summary of findings combines findings from both transgender men and women.
Practical implications
Transgender people in the United States report poorer mental health outcomes (e.g., depression, anxiety, suicide ideation) than their cisgender counterparts (Downing and Przedworski, 2018). The same is true in many other areas of the world (e.g., Australia; Leonard et al., 2012). El-Hadi et al. (2018) found that 91% of transgender people in their study reported gender affirmation through surgery was necessary for their quality of life. Our results suggest that transgender women and men who undergo surgery are largely satisfied with results, and report improvements in their psychological wellbeing (e.g., Weigert et al., 2013; van de Grift et al., 2017). There is limited evidence, however, that surgery reduces depression and anxiety, although more work is needed. The literature outlined in this review may help practitioners talk to transgender clients about their expectations surrounding surgery. Further to the practical implication outlined above, media coverage of people “detransitioning” (i.e., returning to a cisgender identity) has seen a recent spike (e.g., Knox, 2019). The core implication in such popular articles is that many people who undergo gender-affirming surgical treatments will come to regret their (sometimes irreversible) operations, and therefore may report diminished quality of life outcomes relative to those not accessed surgery. Our findings provide a counterpoint to these concerns, suggesting that while regrets exist (and should be acknowledged), they are rare (e.g., Amend et al., 2013; Antoszewski et al., 2012; Garcia et al., 2014; Neuville et al., 2021).
Limitations of the research reviewed and recommendations for future research
We identified four major limitations of our review, and present these alongside recommendations for future research. The first limitation of our findings is that most of the studies examined in this review were retrospective (i.e., involving participants reflecting upon outcomes of their surgeries; see Appendix for more detail). That is, while many participants claimed that surgeries improved their quality of life, there is little high quality data testing whether scores on quality of life measures actually improve from pre- to post- surgery and into the longer-term. As discussed above, it is possible that many benefits associated with undergoing gender-affirming surgeries may have already been achieved through gender-affirming hormone treatment (e.g., physical changes), social support (e.g., using transgender people’s correct pronouns), and/or wish to undergo further treatment. Consequently, surgery may represent one of the core factors, rather than the sole factor, that predicts their quality of life outcomes. These findings underscore the need for a long term, continuous assessment of the quality of life of transgender men and women both pre- and post-transition, ideally supplemented by data from control/comparison groups, to determine whether it is gender-affirming surgery that primarily predicts transgender patients’ longer-term quality of life outcomes.
The second limitation is that most studies analyzed in this review employed very small sample sizes, with findings for several quality of life outcome constructs being classified as having low strength of evidence due to its studies sampling fewer than 100 participants in total (see Table 2). Given these sample sizes it is difficult to draw firm conclusions from potentially small or null effects. We recognize that it is difficult to obtain data from transgender women and men who undergo gender-affirming surgery, particularly in the longer-term, given they are a small population who also face barriers when accessing treatment (see Sineath et al., 2016; Zhang et al., 2020). At the time of writing, however, studies drawing on larger samples are underway (see Kreukels et al., 2012; Lunn et al., 2019). Hence, we are optimistic that high quality data will be available soon.
The third limitation is that most studies cited in this review employed non-validated self-report measures when measuring transgender men and women’s quality of life (e.g., Ainsworth and Spiegel, 2010). Hence, it may be difficult to directly compare study findings across samples based on outcome measures that have yet to be validated. Hence, we recommend that future research should employ validated measures to assess transgender women and men’s quality of life post-surgery, such as the BREAST-Q in Weigert et al.’s (2013) study. Alternatively, new validated measures (or adaptations of existing measures for transgender men and women) could be developed to measure quality of life specifically in transgender populations. However, as noted with our first limitation, it is important that any future studies that utilize these validated measures to also utilize control/comparison groups, as well as pre- post-surgical data, in order to fully capitalize on the benefits of using validated measures to compare study findings across samples.
The fourth limitation is that our findings generally come from countries that are Westernized, and generally accepting of transgender people (issues compounded by the fact that we only included English language articles in our search). For example, 12 of the 79 (29.6%) studies included in this review were conducted in the Netherlands, a country noted for being socially accepting of transgender people (Flores, 2019). It is possible that surgery has different impacts in different contexts; for example, surgery may be vitally important for those living in countries where markers of being transgender result in physical risk. Sincere attempts at cross-cultural work are necessary, but we recognize that these may be limited by the social and legal factors that make public investigation of transgender issues difficult or dangerous.
Conclusions
Overall, the findings in this literature review suggest both transgender men and women who undergo gender-affirming surgery report being satisfied with their surgery in the longer-term, with very few reporting regret (e.g., Amend et al., 2013; Antoszewski et al., 2012; Garcia et al., 2014; Neuville et al., 2021). Additionally, our findings suggest no consistent declines (but some improvements) in psychological and sexual wellbeing following surgery relative to either transgender men and women who have not undergone surgery, or members of the general public. Such conclusions, however, warrant future investigation. We evaluated most of the studies we reviewed to have a moderate to serious risk of bias, and the strength of their evidence to be low or moderate. Thus, we have suggested several recommendations for future research, including extensive longitudinal studies, larger sample sizes, and accessing participants from countries with low social acceptance of the transgender community. Employing these recommendations may allow for firmer conclusions that assist transgender men and women, and health professionals working with transgender men and women, to make informed decisions that ultimately contribute to their quality of life and wellbeing.
Supplementary Material
Acknowledgments
The authors would like to thank Samantha Bulowski for assistance with screening articles for inclusion in the present review.
Glossary
- List of abbreviationsPRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ROBINS-I
Risk Of Bias In Non-randomized Studies - of Interventions
- RA
Research assistant
- LGBT
lesbian, gay, bisexual, and transgender
Funding Statement
This review was supported by Dr. Javier’s Australian Government Research Training Scholarship and 2019/2020 University of Queensland Summer Research Scholarships. Neither funding source did not contribute to the writing of the manuscript nor the decision to submit it for publication.
Footnotes
The authors (who are themselves gender diverse) note that the term “transsexual” is offensive to many transgender people.
Declaration of interest
The authors have no other conflict of interest to declare.
References
- Ainsworth, T. A., & Spiegel, J. H. (2010). Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Quality of Life Research, 19(7), 1019–1024. 10.1007/s11136-010-9668-7 [DOI] [PubMed] [Google Scholar]
- Aires, M. M., de Vasconcelos, D., Lucena, J. A., Gomes, A., de, O. C., & Moraes, B. T. (2021). Effect of Wendler glottoplasty on voice and quality of life of transgender women. Brazilian Journal of Otorhinolaryngology. 10.1016/j.bjorl.2021.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aires, M. M., de Vasconcelos, D., & Moraes, B. T. D. (2020). Chondrolaryngoplasty in transgender women: Prospective analysis of voice and aesthetic satisfaction. International Journal of Transgender Health, 22(4), 394–402. 10.1080/26895269.2020.1848690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhoondinasab, M. R., Saboury, M., Shafaeei, Y., Forghani, S., & Fatemi, M. J. (2020). The comparison of a new durable coronaplasty technique with Norfolk method for glans reconstruction after phalloplasty. World Journal of Plastic Surgery, 9(1), 39–43. 10.29252/wjps.9.1.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amend, B., Seibold, J., Toomey, P., Stenzl, A., & Sievert, K.-D. (2013). Surgical reconstruction for male-to-female sex reassignment. European Urology, 64(1), 141–149. 10.1016/j.eururo.2012.12.030 [DOI] [PubMed] [Google Scholar]
- Antoszewski, B., Bratoś, R., Sitek, A., & Fijałkowska, M. (2012). Long-term results of breast reduction in female-to-male transsexuals. Polski Przeglad Chirurgiczny, 84(3), 144–151. 10.1007/s11136-010-9668-7 [DOI] [PubMed] [Google Scholar]
- Ardebili, M. E., Janani, L., Khazaei, Z., Moradi, Y., & Baradaran, H. R. (2020). Quality of life in people with transsexuality after surgery: a systematic review and meta-analysis. Health and Quality of Life Outcomes, 18(1), 1–11. 10.1186/s12955-020-01510-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balakrishnan, T. M., Nagarajan, S., & Jaganmohan, J. (2020). Retrospective study of prosthetic augmentation mammoplasty in transwomen. Indian Journal of Plastic Surgery: Official Publication of the Association of Plastic Surgeons of India, 53(1), 42–050. 10.1055/s-0040-1709427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellinga, R. J., Capitán, L., Simon, D., & Tenório, T. (2017). Technical and clinical considerations for facial feminization surgery with rhinoplasty and related procedures. JAMA Facial Plastic Surgery, 19(3), 175–181. 10.1001/jamafacial.2016.1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman, N. D., Lohr, K. N., Ansari, M. T., Balk, E. M., Kane, R., McDonagh, M., Morton, S. C., Viswanathan, M., Bass, E. B., Butler, M., Gartlehner, G., Hartling, L., McPheeters, M., Morgan, L. C., Reston, J., Sista, P., Whitlock, E., & Chang, S. (2015). Grading the strength of a body of evidence when assessing health care interventions: An EPC update. Journal of Clinical Epidemiology, 68(11), 1312–1324. 10.1016/j.jclinepi.2014.11.023 [DOI] [PubMed] [Google Scholar]
- Blanchard, R., Legault, S., & Lindsay, W. R. N. (1987). Vaginoplasty outcome in male-to-female transsexuals. Journal of Sex & Marital Therapy, 13(4), 265–275. 10.1080/00926238708403899 [DOI] [PubMed] [Google Scholar]
- Bouman, M.-B., van der Sluis, W. B., van Woudenberg Hamstra, L. E., Buncamper, M. E., Kreukels, B. P., Meijerink, W. J., & Mullender, M. G. (2016). Patient-reported esthetic and functional outcomes of primary total laparoscopic intestinal vaginoplasty in transgender women with penoscrotal hypoplasia. The Journal of Sexual Medicine, 13(9), 1438–1444. 10.1016/j.jsxm.2016.06.009 [DOI] [PubMed] [Google Scholar]
- Buncamper, M. E., Honselaar, J. S., Bouman, M. B., Özer, M., Kreukels, B. P., & Mullender, M. G. (2015). Aesthetic and functional outcomes of neovaginoplasty using penile skin in male-to-female transsexuals. The Journal of Sexual Medicine, 12(7), 1626–1634. 10.1111/jsm.12914 [DOI] [PubMed] [Google Scholar]
- Casado, J. C., Rodríguez-Parra, M. J., & Adrián, J. A. (2017). Voice feminization in male-to-female transgendered clients after Wendler’s glottoplasty with vs. without voice therapy support. European Archives of Oto-Rhino-Laryngology, 274(4), 2049–2058. 10.1007/s00405-016-4420-8 [DOI] [PubMed] [Google Scholar]
- Cella, D. F. (1994). Quality of life: Concepts and definition. Journal of Pain and Symptom Management, 9(3), 186–192. 10.1016/0885-3924(94)90129-5 [DOI] [PubMed] [Google Scholar]
- Center for Reviews and Dissemination at the University of York. (2016). Guidance notes for registering a systematic review protocol with PROSPERO. https://www.crd.york.ac.uk/prospero/documents/Registering%20a%20review%20on%20PROSPERO.pdf.
- Clark, B. A., Veale, J. F., Townsend, M., Frohard-Dourlent, H., & Saewyc, E. (2018). Non-binary youth: Access to gender-affirming primary health care. International Journal of Transgender Health, 19(2), 158–169. 10.1080/15532739.2017.1394954 [DOI] [Google Scholar]
- Dabernig, J., Chan, L. K. W., & Schaff, J. (2006). Phalloplasty with free (septocutaneous) fibular flap sine fibula. The Journal of Urology, 176(5), 2085–2088. 10.1016/j.juro.2006.07.036 [DOI] [PubMed] [Google Scholar]
- Day, D.-L., Klit, A., Lang, C. L., Mejdahl, M. K., & Holmgaard, R. (2021). High self-reported satisfaction after top surgery in gender-affirming surgery: A single-center study. Transgender Health, 10.1089/trgh.2021.0091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Cuypere, G., Elaut, E., Heylens, G., Van Maele, G., Selvaggi, G., T’Sjoen, G., Rubens, R., Hoebeke, P., & Monstrey, S. (2006). Long-term follow-up: Psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies, 15(2), 126–133. 10.1016/j.sexol.2006.04.002 [DOI] [Google Scholar]
- De Cuypere, G., T’Sjoen, G., Beerten, R., Selvaggi, G., De Sutter, P., Hoebeke, P., Monstrey, S., Vansteenwegen, A., & Rubens, R. (2005). Sexual and physical health after sex reassignment surgery. Archives of Sexual Behavior, 34(6), 679–690. 10.1007/s10508-005-7926-5 [DOI] [PubMed] [Google Scholar]
- de Rooij, F. P., van de Grift, T. C., Veerman, H., Al-Tamimi, M., van der Sluis, W. B., Ronkes, B. L., Özer, M., Mullender, M. G., Bouman, M.-B., & Pigot, G. L. (2021). Patient-reported outcomes after genital gender-affirming surgery with versus without urethral lengthening in transgender men. The Journal of Sexual Medicine, 18(5), 974–981. 10.1016/j.jsxm.2021.03.002 [DOI] [PubMed] [Google Scholar]
- Defreyne, J., Motmans, J., & T’sjoen, G. (2017). Healthcare costs and quality of life outcomes following gender affirming surgery in trans men: A review. Expert Review of Pharmacoeconomics & Outcomes Research, 17(6), 543–556. 10.1080/14737167.2017.1388164 [DOI] [PubMed] [Google Scholar]
- Dessy, L. A., Mazzocchi, M., Corrias, F., Ceccarelli, S., Marchese, C., & Scuderi, N. (2014). The use of cultured autologous oral epithelial cells for vaginoplasty in male-to-female transsexuals: A feasibility, safety, and advantageousness clinical pilot study. Plastic and Reconstructive Surgery, 133(1), 158–161. 10.1097/01.prs.0000435844.95551.35 [DOI] [PubMed] [Google Scholar]
- di Summa, P. G., Watfa, W., Krähenbühl, S., Schaffer, C., Raffoul, W., & Bauquis, O. (2019). Colic-based transplant in sexual reassignment surgery: Functional outcomes and complications in 43 consecutive patients. The Journal of Sexual Medicine, 16(12), 2030–2037. 10.1016/j.jsxm.2019.09.007 [DOI] [PubMed] [Google Scholar]
- Djordjevic, M. L., Bencic, M., Kojovic, V., Stojanovic, B., Bizic, M., Kojic, S., Krstic, Z., & Korac, G. (2019). Musculocutaneous latissimus Dorsi flap for phalloplasty in female to male gender affirmation surgery. World Journal of Urology, 37(4), 631–637. 10.1007/s00345-019-02641-w [DOI] [PubMed] [Google Scholar]
- Djordjevic, M. L., & Bizic, M. R. (2013). Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. The Journal of Sexual Medicine, 10(5), 1431–1438. 10.1111/jsm.12108 [DOI] [PubMed] [Google Scholar]
- Djordjevic, M. L., Stanojevic, D., Bizic, M., Kojovic, V., Majstorovic, M., Vujovic, S., Milosevic, A., Korac, G., & Perovic, S. V. (2009). Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. The Journal of Sexual Medicine, 6(5), 1306–1313. 10.1111/j.1743-6109.2008.01065.x [DOI] [PubMed] [Google Scholar]
- Downing, J. M., & Przedworski, J. M. (2018). Health of transgender adults in the U.S., 2014–2016. American Journal of Preventive Medicine, 55(3), 336–344. 10.1016/j.amepre.2018.04.045 [DOI] [PubMed] [Google Scholar]
- Eldh, J. (1993). Construction of a neovagina with preservation of the glans penis as a clitoris in male transsexuals. Plastic and Reconstructive Surgery, 91(5), 895–900. [PubMed] [Google Scholar]
- El-Hadi, H., Stone, J., Temple-Oberle, C., & Harrop, A. R. (2018). Gender-affirming surgery for transgender individuals: Perceived satisfaction and barriers to care. Plastic Surgery (Oakville, ON), 26(4), 263–268. 10.1177/2292550318767437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahrenberg, J., Hamepel, R., & Selg, H. (2001). Freiburger Persönlichkeitsinventar (FPI). Revidierte Fassung (FPI-R) und teilweise geänderte Fassung (FPI-A1). Göttingen, Germany: Hogrefe Verlag. [Google Scholar]
- Fakin, R. M., Zimmermann, S., Kaye, K., Lunger, L., Weinforth, G., & Giovanoli, P. (2019). Long-term outcomes in breast augmentation in trans-women: A 20-year experience. Aesthetic Surgery Journal, 39(4), 381–390. 10.1093/asj/sjy143 [DOI] [PubMed] [Google Scholar]
- Falcone, M., Garaffa, G., Gillo, A., Dente, D., Christopher, A. N., & Ralph, D. J. (2018). Outcomes of inflatable penile prosthesis insertion in 247 patients completing female to male gender reassignment surgery. BJU International, 121(1), 139–144. 10.1111/bju.14027 [DOI] [PubMed] [Google Scholar]
- Fleming, M. Z., MacGowan, B. R., Robinson, L., Spitz, J., & Salt, P. (1982). The body image of the postoperative female-to-male transsexual. Journal of Consulting and Clinical Psychology, 50(3), 461–462. 10.1037/0022-006X.50.3.461 [DOI] [PubMed] [Google Scholar]
- Flores, A. R. (2019). Social Acceptance of LGBT People in 174 Countries: 1981 to 2017. https://escholarship.org/content/qt5qs218xd/qt5qs218xd.pdf.
- Garaffa, G., Christopher, N. A., & Ralph, D. J. (2010). Total phallic reconstruction in female-to-male transsexuals. European Urology, 57(4), 715–722. 10.1016/j.eururo.2009.05.018 [DOI] [PubMed] [Google Scholar]
- Garcia, M. M., Christopher, N. A., De Luca, F., Spilotros, M., & Ralph, D. J. (2014). Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: The Institute of Urology, London U.K. Experience. Translational Andrology and Urology, 3(2), 156–162. 10.3978/j.issn.2223-4683.2014.04.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath, R. A., & Wynne, K. (2019). A guide to transgender health: state-of-the-art information for gender-affirming people and their supporters. Santa Barbara, CA: ABC-CLIO LLC. [Google Scholar]
- Henrich, G., & Herschbach, P. (2000). Questions on Life Satisfaction (FLZM): A short questionnaire for assessing subjective quality of life. European Journal of Psychological Assessment, 16(3), 150–159. 10.1027//1015-5759.16.3.150 [DOI] [Google Scholar]
- Hess, J., Henkel, A., Bohr, J., Rehme, C., Panic, A., Panic, L., Rossi Neto, R., Hadaschik, B., & Hess, Y. (2018). Sexuality after male-to-female gender affirmation surgery. BioMed Research International, 2018, 9037977–9037979. 10.1155/2018/9037979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horbach, S. E. R., Bouman, M. B., Smit, J. M., Özer, M., Buncamper, M. E., & Mullender, M. G. (2015). Outcome of vaginoplasty in male-to-female transgenders: A systematic review of surgical techniques. Journal of Sexual Medicine 12(6), 1499–1512. 10.1111/jsm.12868 [DOI] [PubMed] [Google Scholar]
- Imbimbo, C., Verze, P., Palmieri, A., Longo, N., Fusco, F., Arcaniolo, D., & Mirone, V. (2009). Intersex and gender identity disorders: A report from a single institute’s 14-year experience in treatment of male-to-female transsexuals. The Journal of Sexual Medicine, 6(10), 2736–2745. 10.1111/j.1743-6109.2009.01379.x [DOI] [PubMed] [Google Scholar]
- Kanhai, R. C. J., Hage, J. J., & Mulder, J. W. (2000). Long-term outcome of augmentation mammaplasty in male-to-female transsexuals: A questionnaire survey of 107 patients. British Journal of Plastic Surgery, 53(3), 209–211. 10.1054/bjps.1999.3298 [DOI] [PubMed] [Google Scholar]
- Kaushik, N., Jindal, O., & Bhardwaj, D. K. (2019). Sigma-lead male-to-female gender affirmation surgery: Blending cosmesis with functionality. Plastic and Reconstructive Surgery. Global Open, 7(4), e2169. 10.1097/GOX.0000000000002169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, V., Hertegård, S., Eriksson, J., Nygren, U., & Södersten, M. (2019). Effects of gender-confirming pitch-raising surgery in transgender women a long-term follow-up study of acoustic and patient-reported data. Journal of Voice, 33(5), 781–791. 10.1016/j.jvoice.2018.03.005 [DOI] [PubMed] [Google Scholar]
- Kim, S.-K., Lee, K.-C., Kwon, Y.-S., & Cha, B.-H. (2009). Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 62(3), 309–317. 10.1016/j.bjps.2007.11.011 [DOI] [PubMed] [Google Scholar]
- Knox, L. (2019, December 19). Media’s ‘detransition’ narrative is fueling misconceptions, trans advocates say. NBC News. https://www.nbcnews.com/feature/nbc-out/media-s-detransition-narrative-fueling-misconceptions-trans-advocates-say-n1102686.
- Kreukels, B., Haraldsen, I., De Cuypere, G., Richter-Appelt, H., Gijs, L., & Cohen-Kettenis, P. (2012). A European network for the investigation of gender incongruence: The ENIGI initiative. European Psychiatry: The Journal of the Association of European Psychiatrists, 27(6), 445–450. 10.1016/j.eurpsy.2010.04.009 [DOI] [PubMed] [Google Scholar]
- Küenzlen, L., Nasim, S., van Neerven, S., Kühn, S., Burger, A. E., Sohn, M., Rieger, U. M., & Bozkurt, A. (2020). Multimodal evaluation of functional nerve regeneration in transgender individuals after phalloplasty with a free radial forearm flap. The Journal of Sexual Medicine, 17(5), 1012–1024. 10.1016/j.jsxm.2020.02.014 [DOI] [PubMed] [Google Scholar]
- La Padula, S., Hersant, B., Chatel, H., Aguilar, P., Bosc, R., Roccaro, G., Ruiz, R., & Meningaud, J. P. (2019). One-step facial feminization surgery: The importance of a custom-made preoperative planning and patient satisfaction assessment. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 72(10), 1694–1699. 10.1016/j.bjps.2019.06.014 [DOI] [PubMed] [Google Scholar]
- Leonard, W., Pitts, M., Mitchell, A., Lyons, A., Smith, A., Patel, S., & Couch, M. (2012). Private lives 2: The second national survey on the health and wellbeing of gay, lesbian, bisexual, transgender. GLBT. https://melbourneinstitute.unimelb.edu.au/assets/documents/hilda-bibliography/other-publications/2012/Leonard_etal_Private_Lives_2_Report.pdf [Google Scholar]
- Leriche, A., Timsit, M. O., Morel, ‐Journel, N., Bouillot, A., Dembele, D., & Ruffion, A. (2008). Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU International, 101(10), 1297–1300. 10.1111/j.1464-410X.2007.07362.x [DOI] [PubMed] [Google Scholar]
- Lindqvist, E. K., Sigurjonsson, H., Möllermark, C., Rinder, J., Farnebo, F., & Lundgren, T. K. (2017). Quality of life improves early after gender reassignment surgery in transgender women. European Journal of Plastic Surgery, 40(3), 223–226. 10.1007/s00238-016-1252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loree, J. T., Burke, M. S., Rippe, B., Clarke, S., Moore, S. H., & Loree, T. R. (2020). Transfeminine gender confirmation surgery with penile inversion vaginoplasty: An initial experience. Plastic and Reconstructive Surgery. Global Open, 8(5), e2873. 10.1097/GOX.0000000000002873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe, W. I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., Schneider, A., & Brähler, E. (2009). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders., 122(1), 86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- Lunn, M. R., Lubensky, M., Hunt, C., Flentje, A., Capriotti, M. R., Sooksaman, C., Harnett, T., Currie, D., Neal, C., & Obedin-Maliver, J. (2019). A digital health research platform for community engagement, recruitment, and retention of sexual and gender minority adults in a national longitudinal cohort study-The PRIDE Study. Journal of the American Medical Informatics Association: JAMIA, 26(8–9), 737–748. 10.1093/jamia/ocz082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manrique, O. J., Sabbagh, M. D., Ciudad, P., Martinez-Jorge, J., Kiranantawat, K., Sitpahul, N., Nippoldt, T. B., Charafeddine, A., & Chen, H.-C. (2018). Gender-confirmation surgery using the pedicle transverse colon flap for vaginal reconstruction: A clinical outcome and sexual function evaluation study. Plastic and Reconstructive Surgery, 141(3), 767–771. 10.1097/PRS.0000000000004122 [DOI] [PubMed] [Google Scholar]
- Massie, J. P., Morrison, S. D., Van Maasdam, J., & Satterwhite, T. (2018). Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plastic and Reconstructive Surgery, 141(6), 911e–921e. 10.1097/PRS.0000000000004427 [DOI] [PubMed] [Google Scholar]
- Matai, V., Cheesman, A. D., & Clarke, P. M. (2003). Cricothyroid approximation and thyroid chondroplasty: A patient survey. Otolaryngology-Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery, 128(6), 841–847. 10.1016/S0194-5998(03)00462-5 [DOI] [PubMed] [Google Scholar]
- Meister, J., Hagen, R., Shehata-Dieler, W., Kühn, H., Kraus, F., & Kleinsasser, N. (2017). Pitch elevation in male-to-female transgender persons—The Würzburg approach. Journal of Voice: Voice, 31(2), 244.e7. 10.1016/j.jvoice.2016.07.018 [DOI] [PubMed] [Google Scholar]
- Mora, E., Cobeta, I., Becerra, A., & Lucio, M. J. (2018). Comparison of cricothyroid approximation and glottoplasty for surgical voice feminization in male-to-female transsexuals. The Laryngoscope, 128(9), 2101–2109. 10.1002/lary.27172 [DOI] [PubMed] [Google Scholar]
- Morrison, S. D., Satterwhite, T., Grant, D. W., Kirby, J., Laub, D. R., Sr., & VanMaasdam, J. (2015). Long-term outcomes of rectosigmoid neocolporrhaphy in male-to-female gender reassignment surgery. Plastic and Reconstructive Surgery, 136(2), 386–394. 10.1097/PRS.0000000000001459 [DOI] [PubMed] [Google Scholar]
- Murad, M. H., Elamin, M. B., Garcia, M. Z., Mullan, R. J., Murad, A., Erwin, P. J., & Montori, V. M. (2010). Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clinical Endocrinology, 72(2), 214–231. 10.1111/j.1365-2265.2009.03625.x [DOI] [PubMed] [Google Scholar]
- Neuville, P., Carnicelli, D., Paparel, P., Ruffion, A., & Morel-Journel, N. (2021). Metoidioplasty with implantation of a specific semirigid prosthesis. The Journal of Sexual Medicine, 18(4), 830–836. 10.1016/j.jsxm.2021.01.177 [DOI] [PubMed] [Google Scholar]
- Nieder, T. O., Eyssel, J., & Köhler, A. (2020). Being trans without medical transition: Exploring characteristics of trans individuals from germany not seeking gender-affirmative medical interventions. Archives of Sexual Behavior, 49(7), 2661–2672. 10.1007/s10508-019-01559-z [DOI] [PubMed] [Google Scholar]
- Oles, N., Darrach, H., Landford, W., Garza, M., Twose, C., Park, C. S., Tran, P., Schechter, L. S., Lau, B., & Coon, D. (2022). Gender affirming surgery: A comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (Part 1: Breast/chest, face, and voice). Annals of Surgery, 275(1), e52–e66. 10.1097/SLA.0000000000004728 [DOI] [PubMed] [Google Scholar]
- Özkan, Ö., Özkan, Ö., Çinpolat, A., Doğan, N. U., Bektaş, G., Dolay, K., Gürkan, A., Arıcı, C., & Doğan, S. (2018). Vaginal reconstruction with the modified rectosigmoid colon: Surgical technique, long-term results and sexual outcomes. Journal of Plastic Surgery and Hand Surgery, 52(4), 210–216. 10.1080/2000656X.2018.1444616 [DOI] [PubMed] [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research Ed.), 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopulos, N. A., Ehrenberger, B., Zavlin, D., Lellé, J.-D., Henrich, G., Kovacs, L., Herschbach, P., Machens, H.-G., & Schaff, J. (2021). Quality of life and satisfaction in transgender men after phalloplasty in a retrospective study. Annals of Plastic Surgery, 87(1), 91–97. 10.1097/SAP.0000000000002693 [DOI] [PubMed] [Google Scholar]
- Passos, T. S., Teixeira, M. S., & Almeida-Santos, M. A. (2020). Quality of life after gender affirmation surgery: A systematic review and network meta-analysis. Sexuality Research and Social Policy, 17(2), 252–262. 10.1007/s13178-019-00394-0 [DOI] [Google Scholar]
- Perovic, S. V., & Djordjevic, M. (2003). Metoidioplasty: A variant of phalloplasty in female transsexuals. BJU International, 92(9), 981–985. 10.1111/j.1464-410x.2003.04524.x [DOI] [PubMed] [Google Scholar]
- Perovic, S. V., Stanojevic, D., & Djordjevic, M. L. (2000). Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU International, 86(7), 843–850. 10.1046/j.1464-410x.2000.00934.x [DOI] [PubMed] [Google Scholar]
- Pigot, G. L. S., Al-Tamimi, M., Nieuwenhuijzen, J. A., van der Sluis, W. B., Moorselaar, R. J. A. v., Mullender, M. G., van de Grift, T. C., & Bouman, M.-B. (2020). Genital gender-affirming surgery without urethral lengthening in transgender men: A clinical follow-up study on the surgical and urological outcomes and patient satisfaction. The Journal of Sexual Medicine, 17(12), 2478–2487. 10.1016/j.jsxm.2020.08.004 [DOI] [PubMed] [Google Scholar]
- Raffaini, M., Magri, A. S., & Agostini, T. (2016). Full facial feminization surgery: Patient satisfaction assessment based on 180 procedures involving 33 consecutive patients. Plastic and Reconstructive Surgery, 137(2), 438–448. 10.1097/01.prs.0000475754.71333.f6 [DOI] [PubMed] [Google Scholar]
- Raffaini, M., Perello, R., Tremolada, C., & Agostini, T. (2019). Evolution of full facial feminization surgery: Creating the gendered face with an all-in-one procedure. The Journal of Craniofacial Surgery, 30(5), 1419–1424. 10.1097/SCS.0000000000005221 [DOI] [PubMed] [Google Scholar]
- Rehman, J., Lazer, S., Benet, A. E., Schaefer, L. C., & Melman, A. (1999). The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Archives of Sexual Behavior, 28(1), 71–89. 10.1023/A:1018745706354 [DOI] [PubMed] [Google Scholar]
- Robinson, I. S., Blasdel, G., Cohen, O., Zhao, L. C., & Bluebond-Langner, R. (2021). Surgical outcomes following gender affirming penile reconstruction: Patient-reported outcomes from a multi-center, international survey of 129 transmasculine patients. The Journal of Sexual Medicine, 18(4), 800–811. 10.1016/j.jsxm.2021.01.183 [DOI] [PubMed] [Google Scholar]
- Remington, A. C., Morrison, S. D., Massie, J. P., Crowe, C. S., Shakir, A., Wilson, S. C., Vyas, K. S., Lee, G. K., & Friedrich, J. B, (2018). Outcomes after phalloplasty: Do transgender patients and multiple urethral procedures carry a higher rate of complication?. Plastic and Reconstructive Surgery, 141(2), 220e–229e. 10.1097/PRS.0000000000004061 [DOI] [PubMed] [Google Scholar]
- Satterwhite, T., Morrison, S. D., Ludwig, D. C., Massie, J. P., Sorkin, M., Friedrich, J., & Cederna, P. S. (2017). Prospective quality of life outcomes after facial feminization surgery. Plastic and Reconstructive Surgery - Global Open, 5(9S), 204–205. 10.1097/01.GOX.0000526461.64463.c [DOI] [Google Scholar]
- Schaff, J., & Papadopulos, N. A. (2009). A new protocol for complete phalloplasty with free sensate and prelaminated osteofasciocutaneous flaps: Experience in 37 patients. Microsurgery, 29(5), 413–419. 10.1002/micr.20647 [DOI] [PubMed] [Google Scholar]
- Selvaggi, G., Monstrey, S., Ceulemans, P., T’Sjoen, G., De Cuypere, G., & Hoebeke, P. (2007). Genital sensitivity after sex reassignment surgery in transsexual patients. Annals of Plastic Surgery, 58(4), 427–433. 10.1097/01.sap.0000238428.91834.be [DOI] [PubMed] [Google Scholar]
- Selvaggi, G., Hoebeke, P., Ceulemans, P., Hamdi, M., Van Landuyt, K., Blondeel, P., De Cuypere, G., & Monstrey, S. (2009). Scrotal reconstruction in female-to-male transsexuals: A novel scrotoplasty. Plastic Reconstructive Surgery, 123(6), 1710–1718. 10.1097/PRS.0b013e3181a659fe [DOI] [PubMed] [Google Scholar]
- Seyed-Forootan, K., Karimi, H., & Seyed-Forootan, N.-S. (2018). Autologous fibroblast-seeded amnion for reconstruction of neo-vagina in male-to-female reassignment surgery. Aesthetic Plastic Surgery, 42(2), 491–497. 10.1007/s00266-018-1088-z [DOI] [PubMed] [Google Scholar]
- Sigurjónsson, H., Möllermark, C., Rinder, J., Farnebo, F., & Lundgren, T. K. (2017). Long-term sensitivity and patient-reported functionality of the neoclitoris after gender reassignment surgery. The Journal of Sexual Medicine, 14(2), 269–273. 10.1016/j.jsxm.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Sineath, R. C., Woodyatt, C., Sanchez, T., Giammattei, S., Gillespie, T., Hunkeler, E., Owen-Smith, A., Quinn, V. P., Roblin, D., Stephenson, R., Sullivan, P. S., Tangpricha, V., & Goodman, M. (2016). Determinants of and barriers to hormonal and surgical treatment receipt among transgender people. Transgender Health, 1(1), 129–136. 10.1089/trgh.2016.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small, M. R. (1987). Penile and scrotal inversion vaginoplasty for male to female transsexuals. Urology, 29(6), 593–597. 10.1016/0090-4295(87)90098-7 [DOI] [PubMed] [Google Scholar]
- Song, C., Wong, M., Wong, C.-H., & Ong, Y.-S. (2011). Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. Journal of Reconstructive Microsurgery, 27(2), 115–120. 10.1055/s-0030-1268210 [DOI] [PubMed] [Google Scholar]
- Staud, C. J., Zaussinger, M., Duscher, D., Radtke, C., Wenny, R., Schmidt, M., & Huemer, G. M. (2021). A modified microvascular “Tube-in-Tube” concept for penile construction in female-to-male transsexuals: Combined radial forearm free flap with anterolateral thigh flap. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 74(9), 2364–2371. 10.1016/j.bjps.2021.01.016 [DOI] [PubMed] [Google Scholar]
- Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A.-W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical Research ed.), 355, i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavakkoli Tabassi, K., Djavan, B., Hosseini, J., Ghoreifi, A., Ershadi, M., & Hosseini, E. (2015). Fold-back perineoscrotal flap plus penile inversion vaginoplasty for male-to-female gender reassignment surgery in circumcised subjects. European Journal of Plastic Surgery, 38(1), 43–48. 10.1007/s00238-014-1038-1 [DOI] [Google Scholar]
- Telang, P. S. (2020). Facial feminization surgery: A review of 220 consecutive patients. Indian Journal of Plastic Surgery, 53(2), 244–253. 10.1055/s-0040-1716440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thalaivirithan, B. M., Sethu, M., Ramachandran, D. K., Kandasamy, M., & Janardhanam, J. (2018). Application of embryonic equivalents in male-to-female sex reassignment surgery. Indian Journal of Plastic Surgery: Official Publication of the Association of Plastic Surgeons of India, 51(2), 155–166. 10.4103/ijps.IJPS_62_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timsit, M., Ruffian, A., Morel-Journel, N., Dembele, D., Bouillot, A., & Leriche, A. (2005). 130: Long term follow up of phalloplasty with forearm free flap in 56 female-to-male transsexuals. Journal of Urology, 173(4S), 35–35. 10.1016/S0022-5347(18)34395-7 [DOI] [Google Scholar]
- Tirrell, A. R., Abu El Hawa, A., Bekeny, J. C., & Del Corral, G. (2021). Outcomes in chest feminization patients with a history of illicit hormone use and silicone injections. The Breast Journal, 27(4), 352–358. 10.1111/tbj.14178 [DOI] [PubMed] [Google Scholar]
- Van Caenegem, E., Verhaeghe, E., Taes, Y., Wierckx, K., Toye, K., Goemaere, S., Zmierczak, H.-G., Hoebeke, P., Monstrey, S., & T’Sjoen, G. (2013). Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. The Journal of Sexual Medicine, 10(6), 1644–1651. 10.1111/jsm.12121 [DOI] [PubMed] [Google Scholar]
- van de Grift, T. C., Elfering, L., Greijdanus, M., Smit, J. M., Bouman, M.-B., Klassen, A. F., & Mullender, M. G. (2018). Subcutaneous mastectomy improves satisfaction with the body and psychosocial function in trans men: Findings of a cross-sectional study using the BODY-Q chest module. Plastic and Reconstructive Surgery, 142(5), 1125–1132. 10.1097/PRS.0000000000004827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Grift, T. C., Pigot, G. L. S., Boudhan, S., Elfering, L., Kreukels, B. P. C., Gijs, L. A. C. L., Buncamper, M. E., Özer, M., van der Sluis, W., Meuleman, E. J. H., Bouman, M.-B., & Mullender, M. G. (2017). A longitudinal study of motivations before and psychosexual outcomes after genital gender-confirming surgery in transmen. The Journal of Sexual Medicine, 14(12), 1621–1628. 10.1016/j.jsxm.2017.10.064 [DOI] [PubMed] [Google Scholar]
- van de Grift, T. C., Pigot, G. L. S., Kreukels, B. P. C., Bouman, M.-B., & Mullender, M. G. (2019). Transmen’s experienced sexuality and genital gender-affirming surgery: Findings from a clinical follow-up study. Journal of Sex & Marital Therapy, 45(3), 201–205. 10.1080/0092623X.2018.1500405 [DOI] [PubMed] [Google Scholar]
- van der Sluis, W. B., Bouman, M.-B., de Boer, N. K. H., Buncamper, M. E., van Bodegraven, A. A., Neefjes-Borst, E. A., Kreukels, B. P. C., Meijerink, W. J. H. J., & Mullender, M. G. (2016). Long-term follow-up of transgender women after secondary intestinal vaginoplasty. The Journal of Sexual Medicine, 13(4), 702–710. 10.1016/j.jsxm.2016.01.008 [DOI] [PubMed] [Google Scholar]
- van der Sluis, W., Steensma, T., Timmermans, F., Smit, J., de Haseth, K., Özer, M., & Bouman, M. (2020). Gender-confirming vulvoplasty in transgender women in the netherlands: Incidence, motivation analysis, and surgical outcomes. The Journal of Sexual Medicine, 17(8), 1566–1573. 10.1016/j.jsxm.2020.04.007 [DOI] [PubMed] [Google Scholar]
- van Noort, D. E., & Nicolai, J.-P. (1993). Comparison of two methods of vagina construction in transsexuals. Plastic and Reconstructive Surgery, 91(7), 1308–1315. 10.1097/00006534-199306000-00018 [DOI] [PubMed] [Google Scholar]
- Wagner, S., Greco, F., Hoda, M., Inferrera, A., Lupo, A., Hamza, A., & Fornara, P. (2010). Male-to-female transsexualism: Technique, results and 3-year follow-up in 50 patients. Urologia Internationalis, 84(3), 330–333. 10.1159/000288238 [DOI] [PubMed] [Google Scholar]
- Wei, S.-Y., Li, F.-Y., Li, Q., Li, S.-K., Zhou, C.-D., Zhou, Y., Cao, Y.-J., Zhang, S.-Y., & Zhao, Y. (2018). Autologous buccal micro-mucosa free graft combined with posterior scrotal flap transfer for vaginoplasty in male-to-female transsexuals: A pilot study. Aesthetic Plastic Surgery, 42(1), 188–196. 10.1007/s00266-017-0977-x [DOI] [PubMed] [Google Scholar]
- Weigert, R., Frison, E., Sessiecq, Q., Al Mutairi, K., & Casoli, V. (2013). Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plastic and Reconstructive Surgery, 132(6), 1421–1429. 10.1097/01.prs.0000434415.70711.49 [DOI] [PubMed] [Google Scholar]
- Wierckx, K., Mueller, S., Weyers, S., Van Caenegem, E., Roef, G., Heylens, G., & T’sjoen, G. (2012). Long-term evaluation of cross-sex hormone treatment in transsexual persons. The Journal of Sexual Medicine, 9(10), 2641–2651. 10.1111/j.1743-6109.2012.02876.x [DOI] [PubMed] [Google Scholar]
- Yang, C. Y., Palmer, A. D., Meltzer, T. R., Murray, K. D., & Cohen, J. I. (2002). Cricothyroid approximation to elevate vocal pitch in male-to-female transsexuals: Results of surgery. The Annals of Otology, Rhinology, and Laryngology, 111(6), 477–485. 10.1177/000348940211100602 [DOI] [PubMed] [Google Scholar]
- Yılmaz, T., Ozer, F., & Aydinli, F. E. (2021). Laser reduction glottoplasty for voice feminization: Experience on 28 patients. The Annals of Otology, Rhinology, and Laryngology, 130(9), 1057–1063. 10.1177/0003489421993728 [DOI] [PubMed] [Google Scholar]
- Zhang, Q., Goodman, M., Adams, N., Corneil, T., Hashemi, L., Kreukels, B., Motmans, J., Snyder, R., & Coleman, E. (2020). Epidemiological considerations in transgender health: A systematic review with focus on higher quality data. International Journal of Transgender Health, 21(2), 113–125. 10.1080/26895269.2020.1753136 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.