Abstract
Breast cancer (BC) is the second most common cause of cancer-related deaths and the most frequently diagnosed cancer in females. Among breast cancer types, HER2-positive breast cancer occurs in nearly 20% of human breast cancers and is associated with increased aggressiveness, poor prognosis, and shortened overall survival. HER2+ breast cancer is currently managed with multidisciplinary treatment strategies including surgery, radiation, chemotherapy, and targeted therapy. Drug resistance remains a continuing challenge, especially to targeted therapy utilizing monoclonal antibodies and tyrosine kinase inhibitors. This review discusses some of the recent molecular mechanisms that are involved in the development of resistance to Her2-targeted therapies including the PI3K/Akt/mTOR pathway, IGF-IR, Src, c-MET, the PP2A family, CD36, p27kip1, and miRNAs.
Keywords: HER2+, Targeted therapy resistance, IGF-IR, Src, c-MET, PP2A, CD36, miRNA
INTRODUCTION
Breast cancer (BC) is the most frequently diagnosed cancer in females and the second most common cause of cancer-related deaths, accounting for 30% of malignancies in women[1]. In the U.S, it is estimated that approximately 40,000 women die from breast cancer each year[2]. Moreover, in 2020, 2.3 million women were diagnosed with BC worldwide, with the number of deaths reaching 685,000. Near the end of 2020, 7.8 million women diagnosed with BC in the previous five years were alive, making it the most prevalent cancer globally[3].
Breast cancers prognosis and classification rely not only on tumor morphology but also on the expression levels of three proteins, specifically the estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 (HER2). Tumors that do not express any of these proteins are classified as triple-negative breast cancers, a form of the disease that is particularly difficult to treat[4].
HER2 (ERBB2) belongs to the ERBB family, which includes epidermal growth factor receptor 1 (EGFR) (ERBB1/HER1), HER3 (ERBB3), and HER4 (ERBB4)[5]. HER2 shares structural and sequence similarities with the other family members consisting of three regions: an extracellular N-terminal domain, a single transmembrane α-helix domain, and a tyrosine kinase intracellular domain[6,7].
Extracellular ligands have a conserved EGF motif bind with ERBB receptors, causing homo- and heterodimeric interactions between the ERBB receptors in various combinations[7]. HER2 has lacks a ligand binding domain and does not require a ligand for activation and may be found in an activated state via homo-dimerization or hetero-dimerization with other members of the ERBB family. Homo- or hetero-dimerization causes autophosphorylation of the tyrosine kinase domains, resulting in the subsequent activation of different signaling pathways, primarily the phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin (PI3K/Akt/mTOR) and Ras/Raf/mitogen-activated protein kinase (MAPK) pathways, promoting cell survival, proliferation, differentiation, angiogenesis, and invasion[8-11]. Although ERBB receptors are vital regulators for different cellular processes, their dysregulation, as a result of mutations, could lead to the development of cancers[7].
Amplification or overexpression of the human epidermal growth factor receptor-2 occurs in nearly 20% of human breast cancers and is associated with increased aggressiveness, poor prognosis, and short overall survival[11].
HER2+ breast cancer is currently managed with multidisciplinary treatments that include surgery, radiation, chemotherapy, and targeted therapy[12]. Targeted therapy includes monoclonal antibodies such as trastuzumab and tyrosine kinase inhibitors. Although these drugs markedly improve the prognosis of HER2+ breast cancer patients[13,14], a substantial fraction of these patients still suffer from relapse due to intrinsic or acquired resistance to the treatment, particularly in the case of trastuzumab. The majority of patients who achieve an initial response to trastuzumab-based therapy develop resistance within one year[15-17]. In fact, 70% of patients with HER2+ BC show intrinsic or acquired resistance to trastuzumab[18].
In this review, we will shed light on some of the molecular mechanisms that are involved in resistance to anti-HER2 therapies, which significantly hinder their efficacy.
SPECIFIC MECHANISMS OF RESISTANCE
Dysregulation of the PI3K/Akt/mTOR pathway
Targeted therapy resistance may occur as a result of the sustained activation of signaling pathways such as the PI3K/Akt/mTOR pathway, despite HER2 blockage, priming a drug escape mechanism[19-21].
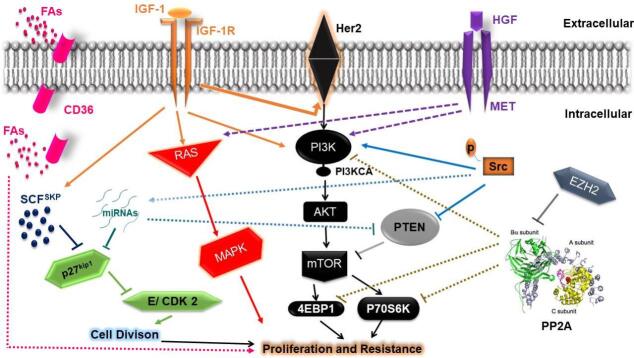
PI3K/Akt signaling dysregulation results in mTOR pathway upregulation and increased mRNA translation leading to enhanced cellular proliferation[22,23], which is mediated by the overexpression of growth factor receptors and loss of the phosphatase and tensin homolog (PTEN) [Figure 1][24]. Breast cancer models of hyperactive PI3K/Akt/mTOR pathway have shown resistance to targeted therapy[25].
Figure 1.
Signaling pathways involved in the development of resistance to Human epidermal growth factor receptor 2 (Her2)-targeted therapy. A central element of resistance appears to be PI3K/AKT/mTOR signaling, which may demonstrate persistent activation through c-MET, IGF-1, p-Src, or interference with PTEN and PP2A mediated suppression of mTOR and downstream signaling at the level of p70S6K and 4EBP1. PP2A activity could also be inhibited by EZH2-mediated slicing of the PP2A regulatory B-subunit. miRNAs and p-Src can also promote the loss of PTEN activity. Resistance could also be mediated through c-MET or IGF1 activation of the RAS/MAPK signaling pathway well as IGF-1; IGF1 can also induce Her2 receptor phosphorylation. p27Kip1 expression is reduced via SCFSKP E3 ubiquitin-mediated degradation, which can be augmented by IGF-1 or via miRNAs which are overexpressed through p-Src, causing loss of cyclin E/CDK2 control and promoting cell cycle progression. CD36 contributed to tumor growth and resistance to Her 2 targeted therapies by providing FAs as a critical energy source for tumorigenesis. PTEN: Phosphatase and tensin homolog; IGF: insulin-like growth factor; MAPK: mitogen-activated protein kinase; FAs: fatty acids.
The persistent activation of this pathway may result from mutations in genes such as PIK3CA, AKT1, AKT2 amplification, and PTEN loss[26]. PTEN loss or PIK3CA mutations are common oncogenic events in HER2+ breast cancer, occurring in approximately 19% and 42% of patients, respectively[27].
PTEN, an mTOR negative regulator, is a tumor suppressor gene whose suppression leds to trastuzumab resistance and shorter survival[20,28]. Nagata et al.[29] provided compelling evidence supporting the role of PTEN loss in trastuzumab resistance. They showed that PI3K/Akt signaling increased via PTEN downregulation [Figure 1], which resulted in blockage of the growth arrest mediated by trastuzumab. Furthermore, they demonstrated that the absence of PTEN expression was associated with a significantly poorer response to trastuzumab-based therapy in HER2+ BC patients than in those with normal PTEN expression. Moreover, in PTEN-deficient cells, PI3K inhibitors decrease trastuzumab resistance both in vitro and in vivo[29].
PIK3CA is a gene that encodes the PI3K catalytic subunit. PIK3CA mutations acquired during disease progression are suggested to reflect increased activation of the PI3K pathway [Figure 1][19]. In vitro data show that PI3KCA gene mutations and HER2 gene amplification are accompanied by resistance to HER2-targeted therapy[21,30,31]. In addition, biomarker analysis from the CLEOPATRA trial showed that PIK3CA mutations were associated with worse survival outcomes in patients with advanced HER2+ breast cancer[32]. Moreover, in the EMILIA trial, PTEN loss or PIK3CA mutations were associated with shorter survival and lower overall response rates in patients receiving capecitabine and lapatinib[33].
These data support a role of the dysregulated PI3K/Akt/mTOR signaling pathway in the development of resistance to HER2 targeted agents.
c-MET
c-MET (mesenchymal-epithelial transition factor) is a tyrosine kinase receptor encoded by the proto-oncogene MET. Along with RON, c-MET belongs to the MET family, which is widely expressed in epithelial and endothelial cells[34-36]. c-MET controls a number of different cellular processes, including replication, survival, and motility[37].
c-MET becomes activated upon binding with its ligand, the hepatocyte growth factor (HGF), triggering a variety of downstream signaling pathways, including PI3K/AKT, Ras/MAPK [Figure 1], Src, signal transducer, and transcription activator[38-41].
Aberrant c-MET activation can contribute to both tumor growth and metastasis[37]. For example, c-MET was reported to be highly expressed in HER2+ BC cell lines and in 25% of HER2+ BC patients’ tissues[42,43]. Poorly differentiated and invasive cell lines also showed an elevated level of c-MET[44]. Clinically, a number of trials demonstrated that c-MET hyperactivity in breast tumors is associated with a lower survival rate[43,45].
Several experimental findings suggest a role for c-MET in targeted-therapy resistance. Engelman et al. showed that c-MET amplification causes HER3-mediated activation of PI3K, and results in gefitinib resistance in lung cancer[46]. In addition, c-MET hyperactivity has been reported as a potential contributor to trastuzumab resistance that may be mediated through sustained Akt activation [Figure 1][42,43]. Additionally, c-MET/HGF axis amplification was reported in a cohort of HER2+ BC patients who failed to respond to trastuzumab-based therapies[42].
Upon treatment with trastuzumab, HER2-overexpressing BC cells may upregulate c-MET, which then protects cells against trastuzumab[42]. Moreover, loss of c-MET function is reported to improve the response of these cell lines to trastuzumab[47].
In studies to demonstrate the significance of c-Met inhibition, Yue et al.[48] reported that miR-182 directly targets the c-MET gene in BC cells and that miR-182 downregulation is associated with trastuzumab resistance in BC cells. They utilized miR-182 to reverse the trastuzumab resistance of BC cells in part via targeting c-MET and its downstream PI3K/AKT/mTOR pathway. Their studies showed that c-MET downregulation restored sensitivity to trastuzumab in vitro using SKBR3 and BT474 BC cell lines, as well as in xenografted models[48].
Cell lines that have upregulated the c-MET/HGF axis have also demonstrated reduced lapatinib sensitivity, indicating that c-MET activation may decrease the effectiveness of the EGFR/HER2 inhibitors. Conversely, lapatinib or erlotinib combined with foretinib, a c-MET inhibitor, suppressed the growth of these cell lines[49,50].
Many selective c-MET inhibitors are currently under clinical development. Cabozantinib, for example, an inhibitor of c-MET and VEGFR2, is being evaluated, in combination with trastuzumab, in HER2 positive BC patients who suffer from brain metastasis[50] [Table 1].
Table 1.
A summary of different targets that promote the development of Human epidermal growth factor receptor 2 (Her2)-targeted therapy resistance and drugs to potentially overcome resistance
| Factors | Mechanism | Drugs | Ref. |
| PTEN loss | PTEN loss causes loss of PI3K/Akt/mTOR pathway control and its sustained activation | BEZ235 | [29,127] |
| PIK3CA mutations | PIK3CA mutations increase activation of the PI3K/Akt/mTOR pathway | BEZ235 | [19,127] |
| c-MET | Upon activation with its ligand HGF, c-MET triggers a variety of downstream signaling pathways, including PI3K/AKT, Ras/MAPK, and Src | Cabozantinib | [38-41,50] |
| IGF-IR | Upon ligand binding, IGF-IR initiates signaling through the Ras/MAPK and PI3K/ AKT pathways. IGF1 signaling also elevates the expression of the p27Kip1 ubiquitin ligase, SKP2, resulting in the degradation of p27Kip1 IGF1 signaling induces the phosphorylation of the HER2 receptor |
BMS-754807 | [52,53,54,127] |
| p27kip1 |
Alteration in its cellular localization or reduced expression is permissive for the activation of cyclin E/ CDK 2, causing cell cycle progression | MG132 | [63,64,65,56] |
| Src |
pSrc promotes activation of the PI3K/Akt/mTOR pathway, EGFR, HER2, and HER3 receptors. Src has been found to inhibit PTEN activity and interfere with its membrane localization |
Dasatinib Saracatinib |
[29,78,80,81,82] |
| PPP2R2B | PPP2R2B downregulation or its silencing by EZH2 causes persistent PI3K/Akt/mTOR pathway activation | EPZ-6438 | [94,95,96-101,102] |
| CD36 |
The CD36-mediated pathway is activated and becomes the major source of FAs uptake rather than FASN-mediated FAs de novo biosynthesis, and provides the cell with needed energy sources, promoting tumor growth and survival | -------- | [111] |
| MicroRNAs | MicroRNAs upregulation targets cell cycle regulators such as p57 and p27. miR-221 directly inhibits PTEN |
--------- | [69-71,72,118] |
PTEN: phosphatase and tensin homolog; MAPK: mitogen-activated protein kinase; PIK3CA: PIK3 catalytic subunit; HGF: hepatocyte growth factor; IGF-IR: insulin-like growth factor-I receptor; PPP2R2B: regulatory B-subunit of PP2A; pSrc: phosphorylated Src; FAs: fatty acids.
Insulin-like growth factor 1 receptor signaling
Another pathway involved in targeted therapy resistance is mediated via the Insulin-like growth factor-I receptor (IGF-IR)[51]. IGF-IR is a tyrosine kinase receptor that plays a critical role in tumor progression. Upon ligand binding, IGF-IR initiates signaling through the Ras/MAPK and PI3K/ AKT pathways [Figure 1], resulting in cell proliferation and the inhibition of apoptosis[52].
A number of studies support a role of IGF-IR in the development of HER2+ breast cancer resistance. One study demonstrated that IGF1R interacts with and induces phosphorylation of HER2 in trastuzumab-resistant cells [Figure 1], but not in the sensitive parental cells. Moreover, the resistant cells showed more-rapid IGF1 stimulation of PI3K/Akt and Ras/MAPK pathways compared with the parental cells[53]. Furthermore, in the in vitro model of resistance, IGF1R signaling inhibition either by IGF1R tyrosine kinase suppression or antibody blockade restored sensitivity to trastuzumab[53].
In a study by Lu et al.[51], the link between trastuzumab resistance and IGF1R signaling was confirmed. These investigators demonstrated that the growth inhibition mediated by trastuzumab was lost in breast cancer cells having high HER2 and IGF1R levels. Moreover, growth arrest was restored when IGF1- mediated activation of IGF1R was inhibited by IGF-binding protein 3 (IGFBP3)[51]. IGF1 signaling was also demonstrated to elevate the expression of the p27Kip1 ubiquitin ligase, SKP2, resulting in degradation of the cyclin-dependent kinase inhibitor p27Kip1 and loss of growth arrest [Figure 1][54]. p27Kip1 belongs to the family of cyclin-dependent kinase inhibitors (CDKIs), which have inhibitory activity towards different CDKs and may function as a tumor suppressor gene by inducing cell cycle arrest[55].
In another study, cyclin-dependent kinase 2 activity was found to be increased in trastuzumab-resistant HER2+ BC cells, accompanied by a reduction in p27Kip1 levels. The addition of exogenous p27Kip1 increased sensitivity to trastuzumab. Thus, these data suggest that p27Kip1 reduction is associated with trastuzumab resistance, which may be mediated by HER2 and IGF-IR heterodimerization[56,57].
p27kip1
p27kip1 (p27) is a member of the CDKI family[58] that functions as an inhibitor of cell cycle transition from the G1 to S phase by suppressing cyclin E/CDK 2 [Figure 1][59]. The p27kip1 expression level serves as a prognostic marker for BC patients[60]. p27kip1 level can be decreased at post-transcriptional levels during G1/S phase progression via ubiquitination and proteasomal degradation after its phosphorylation[61].
Several studies have investigated the role of p27 in targeted-therapy resistance, particularly to trastuzumab and lapatinib in Her2-positive breast cancer.
Trastuzumab-mediated growth arrest appears to depend, in large part, on p27 activity. Trastuzumab causes G1 cell-cycle arrest through increasing the formation of p27-CDK2 complexes[62]. Moreover, trastuzumab increases p27 half-life via decreasing its phosphorylation by cyclin E/CDK2, as well as by suppressing the subsequent ubiquitin-mediated degradation[63].
Yakes et al. and Le et al. demonstrated that the reduction of p27 levels in SKBR3 HER2+ BC cells by antisense oligonucleotides[64] or by small interfering RNA[63] blocked the growth arrest mediated by trastuzumab. Nahta et al. also reported that the trastuzumab-resistant SKBR3 cells showed reduced p27 levels and increased CDK2 activity[56].
Furthermore, Nahta et al. showed that transfection-mediated expression of p27 in the resistant cells increased trastuzumab sensitivity[56,57]. This is consistent with the findings of Kute et al.[65] in which p27 induction by MG132 (a proteasome inhibitor) [Table 1] restored trastuzumab sensitivity, suggesting that downregulation of p27 is likely to result from increased protein degradation. They also reported that the p27 cellular localization might be important for the response to trastuzumab, as trastuzumab-resistant BT474 HER2+ BC cells showed a loss in the nuclear expression of p27[65].
These data are consistent with earlier results in which trastuzumab exposure caused an elevation in p27 levels and nuclear localization in the sensitive cells[64].
In addition, studies by Kute et al.[65], Shattuck et al.[42], and Lu et al.[51,54] suggested that the IGF1R and MET signaling could contribute to p27 downregulation and the development of trastuzumab-resistance, indicating that p27 appears to be a common endpoint for various resistance pathways [42,51,53,54].
Several studies also showed that Src overexpression activated the proteolysis of p27, which may confer lapatinib-resistance in Her2 + breast cancer[66]. It was reported that Src phosphorylates p27 at Tyr74 and Tyr88 to reduce its stability and reduce p27-cyclin E-CDK2 complex formation during G1 phase[67]. Moreover, p27 phosphorylation by Src further promotes the phosphorylation of p27 by cyclin E/ CDK 2, resulting in p27 degradation by SCFSKP E3 ubiquitin[68].
miR-221 upregulation has been reported in different tumors and may be involved in tumor progression by affecting expression levels of the cell cycle regulators such as p57 and p27 [Figure 1][69-71]. Interestingly, Huynh et al.[72] reported that Src-activated NF-κB may result in miR-221 upregulation in lapatinib-resistant cells [Figure 1]. In addition, the findings of Huynh et al. indicated miR-221 involvement, and not the ubiquitination-proteasomal degradation pathway, in p27 downregulation in the lapatinib - resistant cells[72].
These data demonstrated the crosstalk of p27 with the different signaling pathways as well as its role in the development of targeted therapy resistance.
Src
The cellular proto-oncogene Src is a non-receptor tyrosine kinase that regulates varied biological processes such as cellular replication, differentiation, and survival[73,74]. Aberrant Src activation is considered to be a marked oncogenic event[75]. Src is normally found inactivated by the intramolecular binding of its phosphotyrosine (Tyr530) with the Src homology 2 domain[73]. The involvement of receptor tyrosine kinases (RTKs) with growth factors such as EGF and PDGF causes Y530 dephosphorylation and consequent Src activation[76,77]. The activated Src then autophosphorylates tyrosine 416 residue (Tyr416) in its kinase domain, enabling it to interact with a variety of targets[73].
In terms of the relationship between Src activation and the response to targeted therapy, one study which involved 57 BC patients showed that tumors with a high level of phosphorylated Src (pSrc) had a poor clinical response and more aggressive disease after trastuzumab therapy. As might have been anticipated, the overall survival was significantly lower than for patients with pSrc-low tumors[78].
Peiró et al.[79] demonstrated that Src activation resulted in trastuzumab resistance and poor prognosis in HER2+ breast cancer patients. Moreover, the in vitro inhibition of Src restored trastuzumab sensitivity in the resistant cells, with the ability to suppress tumor growth in several preclinical models of resistance. These data are consistent with findings by Zhang et al.[78], where expression of the activated SRC in a trastuzumab-sensitive BC cell line, BT474, caused trastuzumab resistance both in vitro and in xenografted mouse models. Conversely, sensitivity was restored by Src inhibition[78]. In a related finding, in a phase 2 trial of 23 patients with metastatic HER2+ BC, the combination of paclitaxel, trastuzumab, and dasatinib (Src inhibitor) showed high efficacy and success rate[80] [Table 1].
Lapatinib resistance has also been reported in cell lines showing a high level of the activated Src. Lapatinib combined with Saracatinib (Src inhibitor) significantly prolonged the xenografted-mice survival[81] [Table 1].
In efforts to understand the mechanistic relationships between the HER family, IGF-1R, PTEN, and Src, the work of Zhang et al.[78] showed that overexpression of EGFR or IGF-1R or PTEN loss caused Src hyperactivation that is monitored by Tyr416 phosphorylation. The activated Src then promoted trastuzumab resistance in BC cell lines via a PI3K/Akt-dependent [Figure 1] or via independent manner[78]. These cell lines also showed sensitivity to Src inhibitors[78]. Moreover, Src inhibition led to a reduction in EGFR, HER2, and HER3 activation, suggesting that the Src hyperactivity in trastuzumab-resistant cells induces a feedback loop where the active Src causes receptor activation, which, then activate Src.
Studies by Nagata et al.[29] and Lu et al.[82] also suggest a linkage between Src and PTEN, wherein PTEN can use its protein phosphatase activity to regulate Src phosphorylation. Src has been found to inhibit PTEN activity through tyrosine phosphorylation as well as by blocking the membrane localization of PTEN[29,82] [Figure 1], indicating that Src and PTEN may regulate each other to produce trastuzumab resistance.
These results suggest that Src activation is a common event during the development of targeted therapy resistance and that Src inhibition may be a novel therapeutic strategy.
The Protein Phosphatase 2A (PP2A) Family
PP2A is a serine/threonine phosphatase family that regulates a variety of cellular processes including growth, metabolism, and apoptosis[83]. PP2A family members are also well known for their role as tumor suppressors[84,85], suppressing several oncogenic pathways in carcinogenesis including Wnt, Myc, and PI3K/AKT/mTOR[86-88].
Structurally, the PP2A family is found as a heterotrimeric complex that consists of scaffolding A-subunit (PPP2R1A), regulatory B-subunit (PPP2R2B), and catalytic C-subunit (PPP2R2C)[89]. The PPP2R1A subunit often carries inactivating mutations[90,91], while the PPP2R2C and PPP2R2B subunits may be subjected to epigenetic repression or deletions[88,92,93]. These mutations suppress the PP2A tumor suppressor activity, leading to cancer development.
One critical pathway that PP2A controls is the PI3K/AKT/mTOR pathway. The ribosomal protein S6 kinase beta-1 (p70S6K) and eukaryotic translation initiation factor 4E binding protein 1 (4EBP1) regulate two downstream pathways of AKT and mTOR that are vital for cellular proliferation and tumorigenesis[94,95]. PP2A can directly dephosphorylate p70S6K and 4EBP1 to maintain the PI3K/AKT/mTOR pathway equilibrium [Figure 1][96-101]. Consequently, PP2A may be linked to targeted-therapy sensitivity in cancer, including monoclonal antibodies and tyrosine kinase inhibitors[88,90].
In a study by Tan et al.[88], the silencing of PPP2R2B by DNA hypermethylation was found to be accompanied by mTOR inhibitor resistance, while Bao et al.[102] demonstrated that PPP2R2B downregulation is associated with poor prognosis in HER2+ BC and resistance to HER2-targeted therapy, including both lapatinib and trastuzumab. Additionally, these authors suggest that the persistent activation of both p70S6K and 4EBP1 following HER2-targeted therapy in low PPP2R2B-expressing tumor cells might result in therapy failure.
EZH2 is the catalytic subunit of the polycomb repressive complex 2, which suppresses gene expression via mediating the lysine 27 methylation of histone 3[103]. In this study by Tan et al.[103], PPP2R2B silencing mediated by EZH2 was shown to be required for both drug tolerance and HER2-targeted therapy resistance [Figure 1]. Moreover, HER2-targeted therapies combined with EZH2 inhibitors in anti-HER2 resistant cell lines and mouse models engrafted with trastuzumab-resistant cells showed significant tumor growth arrest in both cases. These studies suggest that the combination of EPZ-6438 (EZH2 inhibitor) with HER2-targeted therapy might prevent tumor recurrence and metastasis[102].
Taken together, these data indicate the involvement of the PP2A family in the development of HER2-targeted therapy resistance with the potential use of the PPP2R2B expression levels as a predictive marker for the response.
CD36
Fatty acids (FAs) play a vital role in various biological processes, including cellular signaling, membrane phospholipids synthesis, and energy production[104,105]. Generally, two FAs sources are available for cells to meet their energy requirements: exogenously via specialized transporters and/or endogenously via FA synthase (FASN)-mediated de novo biosynthesis[106]. In contrast to normal cells (except liver and adipose tissues), which preferentially acquire FAs from exogenous sources, more than 90% of FAs in cancer cells are normally derived from de novo FAs synthesis[105]. Tumor cells depend on these two sources not only to sustain their proliferative capacity but also to secure a critical energy source under stress conditions[107].
In terms of exogenous FAs uptake, specific transporters are needed to facilitate FAs movement across the plasma membrane. The most commonly identified transporter is CD36[108], an 88-kDa glycosylated membrane protein that is well-known as a member of the type B scavenger receptor family. CD36 binds several ligands including anionic phospholipids, thrombospondin, and fatty acids[109].
Vazquez-Martin et al.[110] reported that the FASN-mediated FAs de novo biosynthesis is inhibited in response to HER2 inhibition and cancer cells undergo apoptosis, indicating crosstalk between FASN and HER2. However, a recent study found that lapatinib-resistant cells are unresponsive to (-)-C75, which is well-established to suppress FASN[111]. Furthermore, the lapatinib-resistant cells showed a significantly higher level of CD36 with an enhanced rate of FAs uptake, as well as an increase in the presence of lipid droplets compared to their sensitive counterparts[112]. CD36 expression has also been reported to be increased after anti-HER2 therapy, including lapatinib and trastuzumab, which significantly correlates with a poor prognosis in HER2+ BC patients[111]. These data suggest that there is a shift in the metabolic dependence toward CD36-mediated FAs uptake in these cells for maintaining the cellular FAs requirements[111].
CD36 knockdown via siRNA or the small molecule inhibitor, sulfosuccinimidyl oleate (SSO), re-sensitizes lapatinib-resistant cells and induces apoptotic cell death[111]. The role of CD36 in lapatinib resistance was also supported by a tumor xenograft study in mice, in which an anti-CD36 antibody markedly sensitized the resistant tumors to lapatinib. Moreover, CD36 knockdown repressed the tumor growth and extended the survival in a HER2+ BC model[111].
Illustrating the mechanistic aspects of how FAs source alteration in response to targeted therapy ultimately leads to resistance, Feng et al.[111] suggested that HER2 activates FASN via phosphorylation, as well as via transcriptional induction. Therefore, HER2 inhibition mediated by trastuzumab or lapatinib causes the suppression of FASN activity. The CD36-mediated pathway is then activated to become the major source of FAs uptake, promoting tumor growth and survival [Figure 1][111].
These reports indicated the possible role of CD36 in resistance to anti-Her2 targeted therapy.
MicroRNAs
MicroRNAs (miRNAs) are a class of 22-25 nucleotide RNA molecules that downregulate gene expression[113]. miRNAs also play a vital role in the post-transcriptional regulation of mRNA stability and translation efficiency through base-pairing with the complementary locations in the 3’untranslated region of the mRNA[113,114].
miRNAs have been shown to be significantly deregulated in many types of cancer, especially breast cancer, in which deregulated miRNAs are associated with breast cancer metastasis and poor prognosis in some cases, highlighting their critical roles in carcinogenesis, tumor growth, and metastasis[114-116].
The oncogenic miRNA, miR-221, is one of the few miRNAs that are persistently elevated in malignancies of different tissue including breast cancer[117], and has been suggested to accelerate cancer progression by targeting cell cycle regulators such as p57 and p27 [Figure 1][69-71].
Several studies suggest the role of miRNA in the development of targeted therapy resistance. Xingming et al.[118] reported that miR-221 is upregulated in breast cancer cells resistant to trastuzumab. In addition, miR-221 directly inhibits PTEN [Figure 1], causing an elevation in motility and invasiveness of HER2+ BC cells. Moreover, miR-221 suppression or the restoration of PTEN expression reversed the malignant phenotypes of HER2+ BC, indicating the critical role of miRNAs in regulating the progression of HER2+ breast cancer[118].
Huynh et al.[72] discovered that miR-221 upregulation by the Src/NF-κB pathway contributed to the development of lapatinib resistance by targeting p27 [Figure 1]. Furthermore, miR-221 inhibition by Src inhibitors may serve as a novel therapeutic strategy to overcome targeted-therapy resistance[72]. Interestingly, miR-16 has been reported to be involved in regulation of the NF-κB pathway[119]. In addition, miR-630 and miR-16 have been shown to play a role in HER2+ BC sensitivity to lapatinib[120-121]. The interplay among miR-16, miR-630, and miR-221 in regulating the cellular response to targeted-therapy needs to be further investigated.
CONCLUSIONS
Her2-targeted therapies are safe and effective drugs for Her2-positive breast cancer; however, de novo or acquired resistance to these agents has limited their clinical efficacy, which ultimately leads to disease relapse and tumor progression. Many molecular mechanisms are incorporated in targeted-therapy resistance including signaling through alternative RTKs[122,123], altered immune response[122], altered antibody-receptor interaction[123], Her2 TK domain mutations[124], HER3 or HER4 overexpression[125,126] and p95HER2 overexpression[50]. In this review, we have focused on recent mechanisms that play a role in resistance development and the crosstalk between different signaling pathways that contribute to disease progression and resistance. Current and future strategies for overcoming resistance include switching or combining different Her2-targeted agents and the development of small molecule inhibitors such as BEZ235 (Dual PI3K/mTOR inhibitor)[127] [Table 1], BMS-754807 (IGF1R inhibitor)[127] [Table 1], and EPZ-6438 (EZH2 inhibitor)[102] [Table 1]. These strategies show promise towards improving survival in Her2 positive BC patients.
DECLARATIONS
Authors’ contributions
Made substantial contributions in terms of the organization, presentation, writing and editing of this article: Elshazly AM, Gewirtz DA
Availability of data and materials
Not applicable.
Financial support and sponsorship
Work in Dr. Gewirtz’s laboratory relating to breast cancer is supported by NIH/NCI Grant # CA260819 and Grant #W81XWH19-1-0490 from the Department of Defense Breast Cancer Research Program. The funding agencies had no role in the development of this article.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2022.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Kohler BA, Sherman RL, Howlader N, et al. Annual report to the nation on the status of cancer, 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107:djv048. doi: 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO. Breast cancer. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer. [Last accessed on 2 Apr 2022]
- 4.Kalimutho M, Parsons K, Mittal D, et al. Targeted therapies for triple-negative breast cancer: combating a stubborn disease. Trends Pharmacol Sci. 2015;36:822–46. doi: 10.1016/j.tips.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2:127–37. doi: 10.1038/35052073. [DOI] [PubMed] [Google Scholar]
- 6.Lax I, Burgess WH, Bellot F, et al. Localization of a major receptor-binding domain for epidermal growth factor by affinity labeling. Mol Cell Biol. 1988;8:1831–4. doi: 10.1128/mcb.8.4.1831-1834.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu JL, Hung MC. The role of HER2, EGFR, and other receptor tyrosine kinases in breast cancer. Cancer Metastasis Rev. 2016;35:575–88. doi: 10.1007/s10555-016-9649-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olayioye MA. Update on HER-2 as a target for cancer therapy: intracellular signaling pathways of ErbB2/HER-2 and family members. Breast Cancer Res. 2001;3:385–9. doi: 10.1186/bcr327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Citri A, Yarden Y. EGF-ERBB signalling: towards the systems level. Nat Rev Mol Cell Biol. 2006;7:505–16. doi: 10.1038/nrm1962. [DOI] [PubMed] [Google Scholar]
- 10.Moasser MM. The oncogene HER2: its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene. 2007;26:6469–87. doi: 10.1038/sj.onc.1210477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slamon DJ, Clark GM, Wong SG, et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–82. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 12.Lyerly HK. The breast: comprehensive management of benign and malignant diseases. Ann Surg. 1992;215:192. doi: 10.1001/jama.281.2.192-jbk0113-3-1. [DOI] [Google Scholar]
- 13.Dawood S, Broglio K, Buzdar AU, Hortobagyi GN, Giordano SH. Prognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based review. J Clin Oncol. 2010;28:92–8. doi: 10.1200/JCO.2008.19.9844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perez EA, Romond EH, Suman VJ, et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2-positive breast cancer: planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. JCO. 2014;32:3744–52. doi: 10.1200/JCO.2014.55.5730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slamon DJ, Leyland-jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 16.Baselga J, Cortés J, Kim SB, et al. CLEOPATRA Study Group. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366:109–19. doi: 10.1056/NEJMoa1113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen DL, Andersson M, Kamby C. HER2-targeted therapy in breast cancer. Monoclonal antibodies and tyrosine kinase inhibitors. Cancer Treat Rev. 2009;35:121–36. doi: 10.1016/j.ctrv.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Wong AL, Lee SC. Mechanisms of resistance to trastuzumab and novel therapeutic strategies in HER2-positive breast cancer. Int J Breast Cancer. 2012;2012:415170. doi: 10.1155/2012/415170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurvitz SA, Hu Y, O'Brien N, Finn RS. Current approaches and future directions in the treatment of HER2-positive breast cancer. Cancer Treat Rev. 2013;39:219–29. doi: 10.1016/j.ctrv.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berns K, Horlings HM, Hennessy BT, et al. A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell. 2007;12:395–402. doi: 10.1016/j.ccr.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 21.Eichhorn PJ, Gili M, Scaltriti M, et al. Phosphatidylinositol 3-kinase hyperactivation results in lapatinib resistance that is reversed by the mTOR/phosphatidylinositol 3-kinase inhibitor NVP-BEZ235. Cancer Res. 2008;68:9221–30. doi: 10.1158/0008-5472.CAN-08-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Margariti N, Fox SB, Bottini A, Generali D. “Overcoming breast cancer drug resistance with mTOR inhibitors”. Could it be a myth or a real possibility in the short-term future? Breast Cancer Res Treat. 2011;128:599–606. doi: 10.1007/s10549-010-0986-9. [DOI] [PubMed] [Google Scholar]
- 23.Yuan R, Kay A, Berg WJ, Lebwohl D. Targeting tumorigenesis: development and use of mTOR inhibitors in cancer therapy. J Hematol Oncol. 2009;2:45. doi: 10.1186/1756-8722-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martino MC, van Koetsveld PM, Pivonello R, Hofland LJ. Role of the mTOR pathway in normal and tumoral adrenal cells. Neuroendocrinology. 2010;92 Suppl 1:28–34. doi: 10.1159/000314280. [DOI] [PubMed] [Google Scholar]
- 25.Keck S, Glencer AC, Rugo HS. Everolimus and its role in hormone-resistant and trastuzumab-resistant metastatic breast cancer. Future Oncol. 2012;8:1383–96. doi: 10.2217/fon.12.143. [DOI] [PubMed] [Google Scholar]
- 26.Mayer I. Role of mTOR inhibition in preventing resistance and restoring sensitivity to hormone-targeted and HER2-targeted therapies in breast cancer. Clin Adv Hematol Oncol. 2013;11:217–24. [PMC free article] [PubMed] [Google Scholar]
- 27.Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Esteva FJ, Guo H, Zhang S, et al. PTEN, PIK3CA, p-AKT, and p-p70S6K status: association with trastuzumab response and survival in patients with HER2-positive metastatic breast cancer. Am J Pathol. 2010;177:1647–56. doi: 10.2353/ajpath.2010.090885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagata Y, Lan KH, Zhou X, et al. PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell. 2004;6:117–27. doi: 10.1016/j.ccr.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 30.O'Brien NA, Browne BC, Chow L, et al. Activated phosphoinositide 3-kinase/AKT signaling confers resistance to trastuzumab but not lapatinib. Mol Cancer Ther. 2010;9:1489–502. doi: 10.1158/1535-7163.mct-09-1171. [DOI] [PubMed] [Google Scholar]
- 31.Rexer BN, Chanthaphaychith S, Dahlman K, Arteaga CL. Direct inhibition of PI3K in combination with dual HER2 inhibitors is required for optimal antitumor activity in HER2+ breast cancer cells. Breast Cancer Res. 2014;16:R9. doi: 10.1186/bcr3601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baselga J, Cortés J, Im SA, et al. Biomarker analyses in CLEOPATRA: a phase III, placebo-controlled study of pertuzumab in human epidermal growth factor receptor 2-positive, first-line metastatic breast cancer. J Clin Oncol. 2014;32:3753–61. doi: 10.1200/JCO.2013.54.5384. [DOI] [PubMed] [Google Scholar]
- 33.Baselga J, Lewis Phillips GD, Verma S, et al. Relationship between tumor biomarkers and efficacy in EMILIA, a phase III study of trastuzumab emtansine in HER2-positive metastatic breast cancer. Clin Cancer Res. 2016;22:3755–63. doi: 10.1158/1078-0432.CCR-15-2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salgia R. MET in Lung cancer: biomarker selection based on scientific rationale. Mol Cancer Ther. 2017;16:555–65. doi: 10.1158/1535-7163.MCT-16-0472. [DOI] [PubMed] [Google Scholar]
- 35.Fu YT, Zheng HB, Zhou L, et al. Valproic acid, targets papillary thyroid cancer through inhibition of c-Met signalling pathway. Am J Transl Res 2017;9:3138-47. [PMC free article] [PubMed] [Google Scholar]
- 36.Bottaro DP, Rubin JS, Faletto DL, et al. Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product. Science. 1991;251:802–4. doi: 10.1126/science.1846706. [DOI] [PubMed] [Google Scholar]
- 37.Organ SL, Tsao MS. An overview of the c-MET signaling pathway. Ther Adv Med Oncol. 2011;3:S7–S19. doi: 10.1177/1758834011422556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boccaccio C, Comoglio PM. Invasive growth: a MET-driven genetic programme for cancer and stem cells. Nat Rev Cancer. 2006;6:637–45. doi: 10.1038/nrc1912. [DOI] [PubMed] [Google Scholar]
- 39.Blumenschein GR Jr, Mills GB, Gonzalez-Angulo AM. Targeting the hepatocyte growth factor-cMET axis in cancer therapy. J Clin Oncol. 2012;30:3287–96. doi: 10.1200/JCO.2011.40.3774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pilotto S, Carbognin L, Karachaliou N, et al. Tracking MET de-addiction in lung cancer: a road towards the oncogenic target. Cancer Treat Rev. 2017;60:1–11. doi: 10.1016/j.ctrv.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Zhang Y, Xia M, Jin K, et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol Cancer. 2018;17:45. doi: 10.1186/s12943-018-0796-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shattuck DL, Miller JK, Carraway KL 3rd, Sweeney C. Met receptor contributes to trastuzumab resistance of Her2-overexpressing breast cancer cells. Cancer Res. 2008;68:1471–7. doi: 10.1158/0008-5472.CAN-07-5962. [DOI] [PubMed] [Google Scholar]
- 43.Gastaldi S, Comoglio PM, Trusolino L. The Met oncogene and basal-like breast cancer: another culprit to watch out for? Breast Cancer Res. 2010;12:208. doi: 10.1186/bcr2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beviglia L, Matsumoto K, Lin C, Ziober BL, Kramer RH. Expression of the C-Met/HGF receptor in human breast carcinoma: correlation with tumor progression. Int J Cancer. 1997;74:301–9. doi: 10.1002/(sici)1097-0215(19970620)74:3<301::aid-ijc12>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 45.Raghav KP, Wang W, Liu S, et al. cMET and phospho-cMET protein levels in breast cancers and survival outcomes. Clin Cancer Res. 2012;18:2269–77. doi: 10.1158/1078-0432.CCR-11-2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–43. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 47.Pohlmann PR, Mayer IA, Mernaugh R. Resistance to trastuzumab in breast cancer. Clin Cancer Res. 2009;15:7479–91. doi: 10.1158/1078-0432.CCR-09-0636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yue D, Qin X. miR-182 regulates trastuzumab resistance by targeting Met in breast cancer cells. Cancer Gene Ther. 2019;26:1–10. doi: 10.1038/s41417-018-0031-4. [DOI] [PubMed] [Google Scholar]
- 49.Liu L, Shi H, Liu Y, et al. Synergistic effects of foretinib with HER-targeted agents in MET and HER1- or HER2-coactivated tumor cells. Mol Cancer Ther. 2011;10:518–30. doi: 10.1158/1535-7163.MCT-10-0698. [DOI] [PubMed] [Google Scholar]
- 50.Melo Gagliato D, Jardim DL, Marchesi MS, Hortobagyi GN. Mechanisms of resistance and sensitivity to anti-HER2 therapies in HER2+ breast cancer. Oncotarget. 2016;7:64431–46. doi: 10.18632/oncotarget.7043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu Y, Zi X, Zhao Y, Mascarenhas D, Pollak M. Insulin-like growth factor-I receptor signaling and resistance to trastuzumab (Herceptin) J Natl Cancer Inst. 2001;93:1852–7. doi: 10.1093/jnci/93.24.1852. [DOI] [PubMed] [Google Scholar]
- 52.Wang Y, Hailey J, Williams D, et al. Inhibition of insulin-like growth factor-I receptor (IGF-IR) signaling and tumor cell growth by a fully human neutralizing anti-IGF-IR antibody. Mol Cancer Ther. 2005;4:1214–21. doi: 10.1158/1535-7163.MCT-05-0048. [DOI] [PubMed] [Google Scholar]
- 53.Nahta R, Yuan LX, Zhang B, Kobayashi R, Esteva FJ. Insulin-like growth factor-I receptor/human epidermal growth factor receptor 2 heterodimerization contributes to trastuzumab resistance of breast cancer cells. Cancer Res. 2005;65:11118–28. doi: 10.1158/0008-5472.CAN-04-3841. [DOI] [PubMed] [Google Scholar]
- 54.Lu Y, Zi X, Pollak M. Molecular mechanisms underlying IGF-I-induced attenuation of the growth-inhibitory activity of trastuzumab (Herceptin) on SKBR3 breast cancer cells. Int J Cancer. 2004;108:334–41. doi: 10.1002/ijc.11445. [DOI] [PubMed] [Google Scholar]
- 55.Agnantis N, Goussia A, Zagorianakou P, Bai M. Alterations of the cell cycle regulating proteins in invasive breast cancer. Molecular Genetics; Lung and Breast Carcinomas. 2002;1:425–38. doi: 10.1016/s1874-5784(04)80053-9. [DOI] [Google Scholar]
- 56.Nahta R, Takahashi T, Ueno NT, Hung MC, Esteva FJ. P27(kip1) down-regulation is associated with trastuzumab resistance in breast cancer cells. Cancer Res. 2004;64:3981–6. doi: 10.1158/0008-5472.CAN-03-3900. [DOI] [PubMed] [Google Scholar]
- 57.Hubalek M, Brunner C, Matthä K, Marth C. Resistance to HER2-targeted therapy: mechanisms of trastuzumab resistance and possible strategies to overcome unresponsiveness to treatment. Wien Med Wochenschr. 2010;160:506–12. doi: 10.1007/s10354-010-0838-6. [DOI] [PubMed] [Google Scholar]
- 58.Lloyd RV, Erickson LA, Jin L, et al. p27kip1: a multifunctional cyclin-dependent kinase inhibitor with prognostic significance in human cancers. The American Journal of Pathology. 1999;154:313–23. doi: 10.1016/S0002-9440(10)65277-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sherr CJ, Roberts JM. CDK inhibitors: positive and negative regulators of G1-phase progression. Genes Dev. 1999;13:1501–12. doi: 10.1101/gad.13.12.1501. [DOI] [PubMed] [Google Scholar]
- 60.Guan X, Wang Y, Xie R, et al. p27(Kip1) as a prognostic factor in breast cancer: a systematic review and meta-analysis. J Cell Mol Med. 2010;14:944–53. doi: 10.1111/j.1582-4934.2009.00730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nakayama KI, Nakayama K. Ubiquitin ligases: cell-cycle control and cancer. Nat Rev Cancer. 2006;6:369–81. doi: 10.1038/nrc1881. [DOI] [PubMed] [Google Scholar]
- 62.Lane HA, Motoyama AB, Beuvink I, Hynes NE. Modulation of p27/Cdk2 complex formation through 4D5-mediated inhibition of HER2 receptor signaling. Ann Oncol. 2001;12 Suppl 1:S21–2. doi: 10.1093/annonc/12.suppl_1.s21. [DOI] [PubMed] [Google Scholar]
- 63.Le XF, Claret FX, Lammayot A, et al. The role of cyclin-dependent kinase inhibitor p27Kip1 in anti-HER2 antibody-induced G1 cell cycle arrest and tumor growth inhibition. J Biol Chem. 2003;278:23441–50. doi: 10.1074/jbc.M300848200. [DOI] [PubMed] [Google Scholar]
- 64.Yakes FM, Chinratanalab W, Ritter CA, et al. Herceptin-induced inhibition of phosphatidylinositol-3 kinase and Akt Is required for antibody-mediated effects on p27, cyclin D1, and antitumor action. Cancer Res 2002;62:4132-41. [PubMed] [Google Scholar]
- 65.Kute T, Lack CM, Willingham M, et al. Development of herceptin resistance in breast cancer cells. Cytometry A. 2004;57:86–93. doi: 10.1002/cyto.a.10095. [DOI] [PubMed] [Google Scholar]
- 66.Ishizawar R, Parsons SJ. c-Src and cooperating partners in human cancer. Cancer Cell. 2004;6:209–14. doi: 10.1016/j.ccr.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 67.Chu I, Sun J, Arnaout A, et al. p27 phosphorylation by Src regulates inhibition of cyclin E-Cdk2. Cell. 2007;128:281–94. doi: 10.1016/j.cell.2006.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bloom J, Pagano M. Deregulated degradation of the cdk inhibitor p27 and malignant transformation. Seminars in Cancer Biology. 2003;13:41–7. doi: 10.1016/s1044-579x(02)00098-6. [DOI] [PubMed] [Google Scholar]
- 69.Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857–66. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 70.Galardi S, Mercatelli N, Giorda E, et al. miR-221 and miR-222 expression affects the proliferation potential of human prostate carcinoma cell lines by targeting p27Kip1. J Biol Chem. 2007;282:23716–24. doi: 10.1074/jbc.M701805200. [DOI] [PubMed] [Google Scholar]
- 71.Fornari F, Gramantieri L, Ferracin M, et al. MiR-221 controls CDKN1C/p57 and CDKN1B/p27 expression in human hepatocellular carcinoma. Oncogene. 2008;27:5651–61. doi: 10.1038/onc.2008.178. [DOI] [PubMed] [Google Scholar]
- 72.Huynh TK, Huang CH, Chen JY, et al. miR-221 confers lapatinib resistance by negatively regulating p27kip1 in HER2-positive breast cancer. Cancer Sci. 2021;112:4234–45. doi: 10.1111/cas.15107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yeatman TJ. A renaissance for SRC. Nat Rev Cancer. 2004;4:470–80. doi: 10.1038/nrc1366. [DOI] [PubMed] [Google Scholar]
- 74.Thomas SM, Brugge JS. Cellular functions regulated by Src family kinases. Annu Rev Cell Dev Biol. 1997;13:513–609. doi: 10.1146/annurev.cellbio.13.1.513. [DOI] [PubMed] [Google Scholar]
- 75.Kim LC, Song L, Haura EB. Src kinases as therapeutic targets for cancer. Nat Rev Clin Oncol. 2009;6:587–95. doi: 10.1038/nrclinonc.2009.129. [DOI] [PubMed] [Google Scholar]
- 76.Ralston R, Bishop JM. The product of the protooncogene c-Src is modified during the cellular response to platelet-derived growth factor. Proc Natl Acad Sci U S A. 1985;82:7845–9. doi: 10.1073/pnas.82.23.7845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Weernink PA, Rijksen G. Activation and translocation of c-Src to the cytoskeleton by both platelet-derived growth factor and epidermal growth factor. J Biol Chem. 1995;270:2264–7. doi: 10.1074/jbc.270.5.2264. [DOI] [PubMed] [Google Scholar]
- 78.Zhang S, Huang WC, Li P, et al. Combating trastuzumab resistance by targeting SRC, a common node downstream of multiple resistance pathways. Nat Med. 2011;17:461–9. doi: 10.1038/nm.2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Peiró G, Ortiz-Martínez F, Gallardo A, et al. Src, a potential target for overcoming trastuzumab resistance in HER2-positive breast carcinoma. Br J Cancer. 2014;111:689–95. doi: 10.1038/bjc.2014.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ocana A, Gil-Martin M, Antolín S, et al. Efficacy and safety of dasatinib with trastuzumab and paclitaxel in first line HER2-positive metastatic breast cancer: results from the phase II GEICAM/2010-04 study. Breast Cancer Res Treat. 2019;174:693–701. doi: 10.1007/s10549-018-05100-z. [DOI] [PubMed] [Google Scholar]
- 81.Formisano L, Nappi L, Rosa R, et al. Epidermal growth factor-receptor activation modulates Src-dependent resistance to lapatinib in breast cancer models. Breast Cancer Res. 2014;16:R45. doi: 10.1186/bcr3650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lu Y, Yu Q, Liu JH, et al. Src family protein-tyrosine kinases alter the function of PTEN to regulate phosphatidylinositol 3-kinase/AKT cascades. J Biol Chem. 2003;278:40057–66. doi: 10.1074/jbc.M303621200. [DOI] [PubMed] [Google Scholar]
- 83.O'Connor CM, Perl A, Leonard D, Sangodkar J, Narla G. Therapeutic targeting of PP2A. Int J Biochem Cell Biol. 2018;96:182–93. doi: 10.1016/j.biocel.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pallas DC, Shahrik LK, Martin BL, et al. Polyoma small and middle T antigens and SV40 small t antigen form stable complexes with protein phosphatase 2A. Cell. 1990;60:167–76. doi: 10.1016/0092-8674(90)90726-u. [DOI] [PubMed] [Google Scholar]
- 85.Chen W, Possemato R, Campbell K, et al. Identification of specific PP2A complexes involved in human cell transformation. Cancer Cell. 2004;5:127–36. doi: 10.1016/s1535-6108(04)00026-1. [DOI] [PubMed] [Google Scholar]
- 86.Wandzioch E, Pusey M, Werda A, et al. PME-1 modulates protein phosphatase 2A activity to promote the malignant phenotype of endometrial cancer cells. Cancer Res. 2014;74:4295–305. doi: 10.1158/0008-5472.CAN-13-3130. [DOI] [PubMed] [Google Scholar]
- 87.Sablina AA, Hector M, Colpaert N, Hahn WC. Identification of PP2A complexes and pathways involved in cell transformation. Cancer Res. 2010;70:10474–84. doi: 10.1158/0008-5472.CAN-10-2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tan J, Lee PL, Li Z, et al. B55β-associated PP2A complex controls PDK1-directed myc signaling and modulates rapamycin sensitivity in colorectal cancer. Cancer Cell. 2010;18:459–71. doi: 10.1016/j.ccr.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 89.Virshup DM, Shenolikar S. From promiscuity to precision: protein phosphatases get a makeover. Mol Cell. 2009;33:537–45. doi: 10.1016/j.molcel.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 90.Schmoldt A, Benthe HF, Haberland G. Digitoxin metabolism by rat liver microsomes. Biochem Pharmacol. 1975;24:1639–41. [PubMed] [Google Scholar]
- 91.Haesen D, Abbasi Asbagh L, Derua R, et al. Recurrent PPP2R1A mutations in uterine cancer act through a dominant-negative mechanism to promote malignant cell growth. Cancer Res. 2016;76:5719–31. doi: 10.1158/0008-5472.CAN-15-3342. [DOI] [PubMed] [Google Scholar]
- 92.Curtis C, Shah SP, Chin SF, et al. METABRIC Group. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature. 2012;486:346–52. doi: 10.1038/nature10983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cheng AS, Lau SS, Chen Y, et al. EZH2-mediated concordant repression of Wnt antagonists promotes β-catenin-dependent hepatocarcinogenesis. Cancer Res. 2011;71:4028–39. doi: 10.1158/0008-5472.CAN-10-3342. [DOI] [PubMed] [Google Scholar]
- 94.Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes Dev. 2004;18:1926–45. doi: 10.1101/gad.1212704. [DOI] [PubMed] [Google Scholar]
- 95.Fingar DC, Richardson CJ, Tee AR, et al. mTOR controls cell cycle progression through its cell growth effectors S6K1 and 4E-BP1/eukaryotic translation initiation factor 4E. Mol Cell Biol. 2004;24:200–16. doi: 10.1128/MCB.24.1.200-216.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rodgers JT, Vogel RO, Puigserver P. Clk2 and B56β mediate insulin-regulated assembly of the PP2A phosphatase holoenzyme complex on Akt. Mol Cell. 2011;41:471–9. doi: 10.1016/j.molcel.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hui L, Rodrik V, Pielak RM, et al. mTOR-dependent suppression of protein phosphatase 2A is critical for phospholipase D survival signals in human breast cancer cells. J Biol Chem. 2005;280:35829–35. doi: 10.1074/jbc.M504192200. [DOI] [PubMed] [Google Scholar]
- 98.Peterson RT, Desai BN, Hardwick JS, Schreiber SL. Protein phosphatase 2A interacts with the 70-kDa S6 kinase and is activated by inhibition of FKBP12-rapamycinassociated protein. Proc Natl Acad Sci U S A. 1999;96:4438–42. doi: 10.1073/pnas.96.8.4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hahn K, Miranda M, Francis VA, et al. PP2A regulatory subunit PP2A-B’ counteracts S6K phosphorylation. Cell Metab. 2010;11:438–44. doi: 10.1016/j.cmet.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 100.Padmanabhan S, Mukhopadhyay A, Narasimhan SD, et al. A PP2A regulatory subunit regulates C. elegans insulin/IGF-1 signaling by modulating AKT-1 phosphorylation. Cell. 2009;136:939–51. doi: 10.1016/j.cell.2009.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kuo YC, Huang KY, Yang CH, et al. Regulation of phosphorylation of Thr-308 of Akt, cell proliferation, and survival by the B55alpha regulatory subunit targeting of the protein phosphatase 2A holoenzyme to Akt. J Biol Chem. 2008;283:1882–92. doi: 10.1074/jbc.M709585200. [DOI] [PubMed] [Google Scholar]
- 102.Bao Y, Oguz G, Lee WC, et al. EZH2-mediated PP2A inactivation confers resistance to HER2-targeted breast cancer therapy. Nat Commun. 2020;11:5878. doi: 10.1038/s41467-020-19704-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tan JZ, Yan Y, Wang XX, Jiang Y, Xu HE. EZH2: biology, disease, and structure-based drug discovery. Acta Pharmacol Sin. 2014;35:161–74. doi: 10.1038/aps.2013.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ookhtens M, Kannan R, Lyon I, Baker N. Liver and adipose tissue contributions to newly formed fatty acids in an ascites tumor. Am J Physiol. 1984;247:R146–53. doi: 10.1152/ajpregu.1984.247.1.R146. [DOI] [PubMed] [Google Scholar]
- 105.Kamphorst JJ, Cross JR, Fan J, et al. Hypoxic and Ras-transformed cells support growth by scavenging unsaturated fatty acids from lysophospholipids. Proc Natl Acad Sci U S A. 2013;110:8882–7. doi: 10.1073/pnas.1307237110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer. 2007;7:763–77. doi: 10.1038/nrc2222. [DOI] [PubMed] [Google Scholar]
- 107.Röhrig F, Schulze A. The multifaceted roles of fatty acid synthesis in cancer. Nat Rev Cancer. 2016;16:732–49. doi: 10.1038/nrc.2016.89. [DOI] [PubMed] [Google Scholar]
- 108.Su X, Abumrad NA. Cellular fatty acid uptake: a pathway under construction. Trends Endocrinol Metab. 2009;20:72–7. doi: 10.1016/j.tem.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Febbraio M, Hajjar DP, Silverstein RL. CD36: a class B scavenger receptor involved in angiogenesis, atherosclerosis, inflammation, and lipid metabolism. J Clin Invest. 2001;108:785–91. doi: 10.1172/JCI14006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Vazquez-Martin A, Colomer R, Brunet J, Menendez JA. Pharmacological blockade of fatty acid synthase (FASN) reverses acquired autoresistance to trastuzumab (Herceptin by transcriptionally inhibiting ‘HER2 super-expression’ occurring in high-dose trastuzumab-conditioned SKBR3/Tzb100 breast cancer cells. Int J Oncol. 2007;31:769–76. [PubMed] [Google Scholar]
- 111.Feng WW, Bang S, Kurokawa M. CD36: a key mediator of resistance to HER2 inhibitors in breast cancer. Mol Cell Oncol. 2020;7:1715766. doi: 10.1080/23723556.2020.1715766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2:re3. doi: 10.1126/scisignal.272re3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–97. doi: 10.1016/s0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 114.Syeda Z, Langden SSS, Munkhzul C, Lee M, Song SJ. Regulatory mechanism of MicroRNA expression in cancer. Int J Mol Sci. 2020;21:1723. doi: 10.3390/ijms21051723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ahmad A, Aboukameel A, Kong D, et al. Phosphoglucose isomerase/autocrine motility factor mediates epithelial-mesenchymal transition regulated by miR-200 in breast cancer cells. Cancer Res. 2011;71:3400–9. doi: 10.1158/0008-5472.CAN-10-0965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Adams BD, Guttilla IK, White BA. Involvement of microRNAs in breast cancer. Semin Reprod Med. 2008;26:522–36. doi: 10.1055/s-0028-1096132. [DOI] [PubMed] [Google Scholar]
- 117.Rao X, Di Leva G, Li M, et al. MicroRNA-221/222 confers breast cancer fulvestrant resistance by regulating multiple signaling pathways. Oncogene. 2011;30:1082–97. doi: 10.1038/onc.2010.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ye X, Bai W, Zhu H, et al. MiR-221 promotes trastuzumab-resistance and metastasis in HER2-positive breast cancers by targeting PTEN. BMB Rep. 2014;47:268–73. doi: 10.5483/bmbrep.2014.47.5.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tian T, Zhou Y, Feng X, et al. MicroRNA-16 is putatively involved in the NF-κB pathway regulation in ulcerative colitis through adenosine A2a receptor (A2aAR) mRNA targeting. Sci Rep. 2016;6:30824. doi: 10.1038/srep30824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Venturutti L, Cordo Russo RI, Rivas MA, et al. MiR-16 mediates trastuzumab and lapatinib response in ErbB-2-positive breast and gastric cancer via its novel targets CCNJ and FUBP1. Oncogene. 2016;35:6189–202. doi: 10.1038/onc.2016.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Corcoran C, Rani S, Breslin S, et al. miR-630 targets IGF1R to regulate response to HER-targeting drugs and overall cancer cell progression in HER2 over-expressing breast cancer. Mol Cancer. 2014;13:71. doi: 10.1186/1476-4598-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hunter FW, Barker HR, Lipert B, et al. Mechanisms of resistance to trastuzumab emtansine (T-DM1) in HER2-positive breast cancer. Br J Cancer. 2020;122:603–12. doi: 10.1038/s41416-019-0635-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nahta R, Yu D, Hung MC, Hortobagyi GN, Esteva FJ. Mechanisms of disease: understanding resistance to HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol. 2006;3:269–80. doi: 10.1038/ncponc0509. [DOI] [PubMed] [Google Scholar]
- 124.D'Amato V, Raimondo L, Formisano L, et al. Mechanisms of lapatinib resistance in HER2-driven breast cancer. Cancer Treat Rev. 2015;41:877–83. doi: 10.1016/j.ctrv.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 125.Canfield K, Li J, Wilkins OM, et al. Receptor tyrosine kinase ERBB4 mediates acquired resistance to ERBB2 inhibitors in breast cancer cells. Cell Cycle. 2015;14:648–55. doi: 10.4161/15384101.2014.994966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Garrett JT, Olivares MG, Rinehart C, et al. Transcriptional and posttranslational up-regulation of HER3 (ErbB3) compensates for inhibition of the HER2 tyrosine kinase. Proc Natl Acad Sci U S A. 2011;108:5021–6. doi: 10.1073/pnas.1016140108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sharial MSN, Crown J, Hennessy BT. Overcoming resistance and restoring sensitivity to HER2-targeted therapies in breast cancer. Ann Oncol. 2012;23:3007–16. doi: 10.1093/annonc/mds200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.