Abstract
AIMS:
The epidemiologic Study of Women’s Health Across the Nation (SWAN) includes urinary incontinence (UI) questionnaire items. We introduced an independently self-administered paper towel test (PTT-ISA; invention disclosure #2021–347) to objectively demonstrate UI. Aims were to determine: 1) PTT-ISA compliance and 2) relationship to questionnaire results.
METHODS:
276 community women were invited to complete both SWAN questionnaire and PTT-ISA. For PTT-ISA, a woman holds a trifold brown paper towel against her perineum while coughing hard three times. She checks the towel for wetness and compares with pictorial showing wetted area gradations (dry towel through >6ml/saturated). She then selects best photo-match to her towel. A newly conceptualized variable constructed as PTT-ISA plus questionnaire results was formed.
RESULTS:
Of 276 women, noncompliance with PTT-ISA was 2.2% (6 women). Four others (1.5%) were missing questionnaires. For remainder 266 women, conceptual cohesiveness between questionnaire only and PTT-ISA+questionnaire was demonstrated in 165 (62.0%). Lack of cohesiveness occurred in 101 (38.9%), including 41 women who said “no” to the questionnaire item indicative of stress UI and had leakage on PTT-ISA; leakage degree varied across the full pictorial spectrum from drops to saturated.
CONCLUSION:
PTT-ISA demonstrates high compliance, with rate comparable to survey compliance. It is a novel measure for objective sign of urine loss when independently self-administered by community women outside of a clinic environment. Further research comparing PTT-ISA with clinician observed cough test is warranted. As independently self-administered, PTT-ISA is simple, non-invasive, inexpensive, and an acceptable test that adds value to otherwise survey-dependent research.
INTRODUCTION
Typically, in epidemiologic studies, evaluating for evidence of urinary incontinence (UI) relies on survey method alone; representing a methodologic limitation in understanding the complexity in women’s experiences of UI. 1 However, if additional information can only be gained by adding “a clinician” procedure with resultant extra cost and participant burden, these factors work against incorporation into large repeated-measures studies that can span decades.
We hypothesized benefit of a self-test for objective sign of accidental urine loss under provocation of coughing. The Independently Self-Administered Paper Towel Test (PTT-ISA), conducted without clinician presence, was introduced into the in-person study visit at the Michigan site of the Study of Women Across the Nation (SWAN). 2
Aims were to: 1) determine compliance rate of women with the PTT-ISA, and 2) describe findings in relation to questionnaire responses.
MATERIALS AND METHODS
Design:
All women provided written informed consent. The study was approved by the Institutional Review Board of the University of Michigan. The study design for this paper’s report was cross-sectional, with SWAN study participants from the Michigan site.
SWAN began in 1996 as a longitudinal study originally focused on menopausal transition and now following women into old age. At Michigan, the original cohort was 543 women, with 276 seen at the in-person visit in 2015/2016 when the PTT-ISA was introduced.
Independently Self-Administered Paper Towel Test (PTT-ISA):
In the original 1998 version3, the paper towel test was developed for quantifying variance in degrees of urine loss at quantities too small to be detected by the standard pad test of the time. Each woman self-administered her own paper towel test but under direct observation by a clinician.3 In the PTT-ISA the woman is not under direct observation by a clinician or anyone else during the actual self-testing and the woman records results of the PTT-ISA herself (Figures 1 and 2).
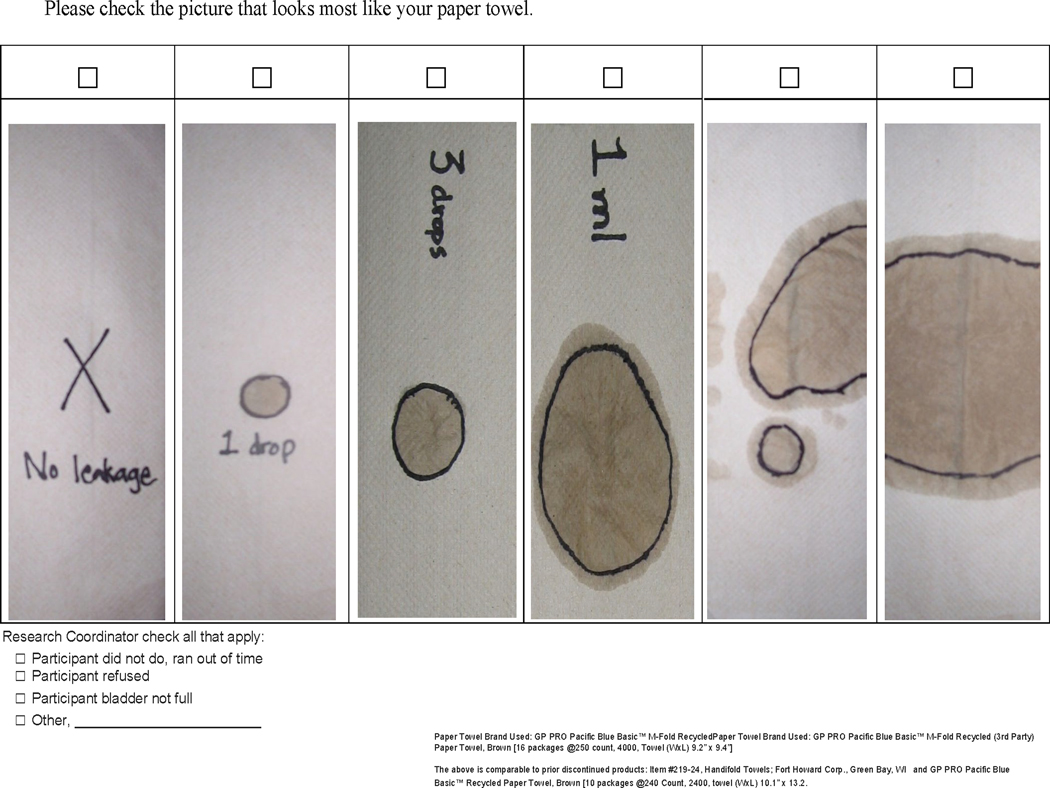
Figure 1.
Results recording form with pictogram (images choices) to document findings from the Independently Self-Administered Paper Towel Test (PTT-ISA) as administered in SWAN for this study. Each woman was asked to select best match with the results of her own PTT-ISA (Invention Disclosure #2019–349 University of Michigan Tech Transfer).
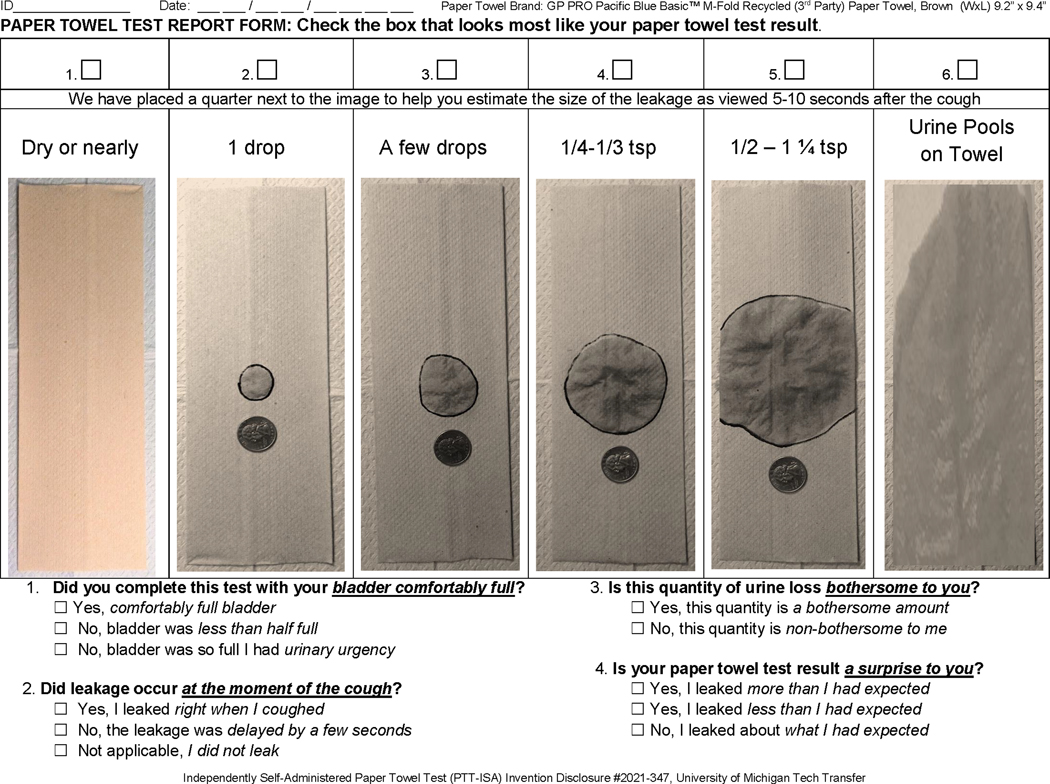
Figure 2.
Newly recommended pictogram with inclusion of questions to provide a woman-centric perspective on her Independently Self-Administered Paper Towel Test (PTT-ISA) results, and expanded range of photos to reflect a representation for fully saturated towel (well beyond 6 ml). (Invention Disclosure # 2021–347 March 16, 2021 University of Michigan Tech Transfer).
PTT-ISA is consistent with the recently published ICS-Uniform Cough Stress Test 5 regarding testing with bladder volume as comfortably/subjectively full. Differences are PTT-ISA: a) is performed in standing posture, not lithotomy, to match with when cough-provoked leakage typically occurs, b) quantifies objectively demonstrated leakage by amount, not just yes/no, c) costs nearly zero, d) is more convenient, and g) preserves modesty/dignity since no need for the woman to bare her bottom to another’s view. See full protocol in supplemental materials.
Repeatability of the paper towel test was studied under clinician-supervised conditions and is within less than 1 ml in that setting. 3,4 Since leakage to outer garment occurs at about 1 ml, leakage of 1/4 to 1/3 teaspoon in US customary unit of volume, greater might be considered a clinically important finding of urine amount lost during a cough event. 3 Full protocol for conducting the PTT-ISA is provided in supplemental materials.
PTT-ISA Procedure per SWAN study:
Each woman chose an opportunity during the 2-hour in-person visit to do the PTT-ISA before emptying her bladder. She was encouraged to choose the testing moment as when her bladder was comfortably full defined as subjectively perceived need to urinate but prior to discomfort and before the point of urgency. For performing the self-test, each woman was offered a private restroom adjacent to the room where the in-person visit was being conducted.
A pictogram was provided (Figure 1) for the woman to record her results. The pictogram recording form showed towels of progressively larger wetted area from urine dispensed onto it. Each woman compared her own PTT-ISA result against the pictogram and selected which picture best matched her towel results.
Incontinence Questions:
Consistent with the SWAN study, women answered questions about urine leakage that were embedded within a much larger survey, which took about two hours to complete. Specific to incontinence, the survey questions were to report leakage as: a) ‘even a small amount, beyond your control’ b) ‘when you were coughing, laughing, sneezing, jogging, jumping, with physical activity, or picking up an object from the floor, or similar activity’, c) ‘when you have the urgency to void and can’t reach the toilet fast enough,’ and c) ‘any leakage in the past month’.
Data Management and Analysis
Data management for UI questionnaire responses within the SWAN survey has been previously defined.2 If participants reported leakage ‘even a small amount, beyond your control’ ‘when you were coughing, laughing, sneezing, jogging, jumping, with physical activity, or picking up an object from the floor, or similar activity’ then the value label applied was STRESS. If participants reported leakage ‘when you have the urgency to void and can’t reach the toilet fast enough’, this was labeled URGENCY. The label MIXED was for participants coded ‘yes’ for both STRESS and URGENCY. ‘OTHER’ was used for participants who reported ‘yes’ to ‘any leakage in the past month’ but ‘no’ for stress question and ‘no’ to urgency question. NONE for reporting ‘no’ to the question of ‘any urine leakage in the past month’.
To explore the relationship of PTT-ISA with the questionnaire data, we built code for a new variable PTT-ISA+Questionnaire, with conceptually constructed values and accompanying labels. When PTT-ISA showed any wetted area from urine, and ‘no’ was reported by questionnaire for ‘when you have the urgency to void and can’t reach the toilet fast enough,’ the value label given was WETPTT/NO Q-URGENCY. When PTT-ISA was dry and ‘yes’ was reported for ‘when you have the urgency to void and can’t reach the toilet fast enough,’ the label was DRYPTT/YES Q-URGENCY. When there was a wet PTT-ISA and ‘yes’ on the urgency question, WETPTT/ YES Q-URGENCY.
Two additional values were conceptually defined. The first coded Dry PTT-ISA but ‘yes’ on stress question was labeled DRYPTT/Q-OTHER1, which considers individuals who show dry PTT-ISA and answered “yes to the single survey question inquiring about trigger for leakage with laughing, jumping, jogging, etc. in addition to listing cough. For when there was a dry PTT-ISA, ‘no’ on stress and urgency questions, but ‘yes’ to ‘any leakage in last month’, we similarly again used the term “other” DRYPTT/Q-OTHER2. This conceptual labeling choice was for clarity that a traditional designation of incontinence (stress, urge, mixed) cannot be presumed in these cases with values labeled OTHER.
Frequencies, cross-tabulations of groups generated by the old and new UI questionnaire-only versus PTT-ISA+questionnaire were calculated, as was percentage agreement per data reduction groups conceptualized as likely similar. Finally, Cohen’s Kappa and 95% CI was calculated after we collapsed DRYPTT/Q-OTHER1 and DRYPTT/Q-OTHER2 into DRYPTT/Q-OTHER to estimate comparison with the questionnaire-only OTHER variable.
RESULTS
Of the 276 women who came to the in-person visit, six (2.2%) were missing information on the PTT-ISA. One woman was unable to follow instructions; two women declined the test (one for fear of wetting her clothes and one because she felt it would be too uncomfortable due to a health condition). For three, there was no reason recorded for missing data. Four (1.5%) additional women were missing information on the questionnaire but not on the PTT-ISA. Thus, 266 women were available for the remainder of the analysis. Table 1 portrays characteristics of the sample according to who did and did not complete the PTT-ISA.
Table 1.
Demographic characteristics by whether or not the independently self-administered paper towel test (PTT-ISA) was completed at the in-person visit.
| Independently Self-Administered Paper Towel Test Completed | ||
|---|---|---|
| Yes n=270 | No n= 6 | |
|
| ||
| Age, years, mean (SD) | 65.0 (2.7) | 64.6 (3.8) |
| Body mass index, kg/m2, mean (SD) | 33.7 (7.7) | 35.0 (5.9) |
| Race, n (%) | ||
| Black | 170 (63.0) | 4 (66.7) |
| White | 100 (37.0) | 2 (33.3) |
| How hard to pay for basics, n (%) | ||
| Very | 15 (5.7) | 0 (0.0) |
| Somewhat | 78 (29.6) | 2 (40.0) |
| Not at all | 171 (64.8) | 3 (60.0) |
Summative data showed 190 (71.4%) of the women reported incontinence per the questionnaire-only data. This compared to 203 (76.3%) with a finding of incontinence by PTT-ISA+questionnaire. The underlying structures of the code to derive this summary data are shown in Table 2, using exploratory conceptually driven value labels in the derived PTT-ISA+questionnaire variable.
Table 2.
Of the 266 women in the sample with both survey data and paper towel test data, results are shown for the 101 women who did not show cohesiveness between questionnaire-only variable and PTT-ISA+Questionnaire variable, as shown in columns 5 and 6. The data for coding questionnaire-only is derived from responses to questionnaire items shown in columns 1–3. The data for coding PTT-ISA+questionnaire is derived from variable items shown in columns 1–4.
| Response Patterns Detail Shown by Discrete Variables in those Women (n=101) Whose Findings Differ Conceptually | ||||||
|---|---|---|---|---|---|---|
| Responses by Individual Variables | Incontinence Typing Derived from Data Reduction Coding | |||||
| Any Leakage in Last Month1 (Questionnaire) | Leakage Due to Stress2 (Questionnaire) | Leakage Due to Urgency3 (Questionnaire) | WET Paper Towel (PTT-ISA) | Questionnaire-Only | PTT-ISA +Questionnaire | Number of Women |
| No | No | No | Yes | NONE | WETPTT/No-Q-URGENCY | 13 |
| Yes | Yes | No | No | STRESS-only | DRYPTT/Q-OTHER | 6 |
| Yes | No | Yes | Yes | URGENCY-only | WETPTT/Yes-Q-URGENCY | 22 |
| Yes | Yes | Yes | No | MIXED | DRYPTT/Yes-Q-URGENCY | 54 |
| Yes | No | No | Yes | OTHER | WETPTT/No-Q-URGENCY | 6 |
Any leakage in past month question: In the last month, about how many days have you lost any urine, even a small amount, beyond your control?
Stress question: In the last month, have you lost any urine, even a small amount, beyond your control when you were coughing, laughing, sneezing, jogging, picking up an object from the floor or similar type of activity?
Urge question: In the last month, have you lost any urine, even a small amount, beyond your control when you have the urge to urinate and can’t get to the toilet fast enough?
Table 2 also provides data from 101 (38.9%) of the study women for whom exploratory conceptual groupings by questionnaire only versus PTT-ISA+questionnaire were not fully cohesive. For instance, 131 women answered ‘yes’ to the question of leakage ‘even a small amount, beyond your control’ ‘when you were coughing, laughing, sneezing, jogging, jumping, with physical activity, or picking up an object from the floor, or similar activity,’ but of these there were 60 (45.8%) who showed a dry PTT-ISA (Table 2).
Table 3 portrays results for the entire sample, adding back in the 165 (62.0%) of women who showed conceptual cohesiveness between questionnaire only and PTT-ISA+questionnaire. Marginal distributions for the full sample are presented as an estimate of the probability distribution. Percentage breakdown within row and within column reveals differences. By questionnaire-only, a total of 76, 22, 50, 109, and 9 women showed results as NONE, STRESS, URGENCY, MIXED, and OTHER. By PTT-ISA+questionnaire, a total of 63, 35, 82, 77, 6 and 3 showed results as NONE, WETPTT/NO-Q-URGENCY, DRYPTT/YES-Q-URGENCY, WETPTT/YES-Q-URGENCY, DRYPTT/Q-OTHER1 or DRYPTT/Q-OTHER2 respectively.
Table 3.
Cross-tabs of results according to conceptualizations by questionnaire-only value and PTT-ISA+questionnaire. The percentages shown within each cell of the table are: marginal percentage representing probability distribution (1st row), row percentage (2nd row) representing questionnaire-only distribution, and column percentage (3rd row) representing PTT-ISA only distribution.
| Paper Towel Test (PTT-ISA) + Questionnaire Items (Q) |
|
||||||
|---|---|---|---|---|---|---|---|
| NONE | WETPTT/No-Q-URGENCY | DRYPTT/Yes-Q-URGENCY | WETPTT/Yes-Q-URGENCY | DRYPTT/Q-OTHER | Total | ||
| Questionnaire-only | NONE | 63 | 13 | 0 | 0 | 0 | 76 |
| (23.7%) | (4.9%) | (0.0%) | (0.0%) | (0.0%) | |||
| (82.9%) | (17.1%) | (0.0%) | (0.0%) | (0.0%) | |||
| (100.0%) | (37.1%) | (0.0%) | (0.0%) | (0.0%) | |||
|
| |||||||
| STRESS | 0 | 16 | 0 | 0 | 6 | 22 | |
| (0.0%) | (6.0%) | (0.0%) | (0.0%) | (2.3%) | |||
| (0.0%) | (72.7%) | (0.0%) | (0.0%) | (27.3%) | |||
| (0.0%) | (45.7%) | (0.0%) | (0.0%) | (66.67%) | |||
|
| |||||||
| URGE | 0 | 0 | 28 | 22 | 0 | 50 | |
| (0.0%) | (0.0%) | (10.5%) | (8.3%) | (0.0%) | |||
| (0.0%) | (0.0%) | (56.0%) | (44.0%) | (0.0%) | |||
| (0.0%) | (0.0%) | (34.1%) | (28.6%) | (0.0%) | |||
|
| |||||||
| MIXED | 0 | 0 | 54 | 55 | 0 | 109 | |
| (0.0%) | (0.0%) | (20.3%) | (20.7%) | (0.0%) | |||
| (0.0%) | (0.0%) | (49.5%) | (50.5%) | (0.0%) | |||
| (0.0%) | (0.0%) | (65.9%) | (71.43%) | (0.0%) | |||
|
| |||||||
| OTHER | 0 | 6 | 0 | 0 | 3 | 9 | |
| (0.0%) | (2.3%) | (0.0%) | (0.0%) | (1.1%) | |||
| (0.0%) | (66.7%) | (0.0%) | (0.0%) | (33.3%) | |||
| (0.0%) | (17.1%) | (0.0%) | (0.0%) | (33.3%) | |||
|
| |||||||
| Total | 63 | 35 | 82 | 77 | 9 | 266 | |
Number agree: 165 (62.03%)
Disagree: 101 (37.97%)
The percentages shown within each cell of the table represent: marginal percentage (1st percentage row), row percentage (2nd percentage row), and column percentage (3rd percentage row)
We further characterized 41 women who said “no” to the questionnaire item indicative of stress UI but showed a wet PTT-ISA (Table 4). For over half of these women, volume was of an amount less than 1 ml, but 14 leaked at least a ml (an amount likely to leak through underwear to outer garment) with eight having urine loss to at least the point of towel saturation (6 ml+).
Table 4.
Participants portrayed are those whose PTT-ISA result was wet paper towel but questionnaire response was “no” to stress type question or any leakage. The rows show PTT-ISA only results ordered by urine loss volume. The columns show questionnaire-only results. Numbers in bold show the women who are of greatest concern regarding lack of cohesiveness with questionnaire from a perspective of potential leakage through to out garment (about 1 ml), which is not picked up by survey only.
| Women responding ‘no to STRESS by Questionnaire and… | ||||
|---|---|---|---|---|
| …no leakage in last month, no urgency UI | yes leakage in last month, yes urgency UI | yes leakage in last month no urgency UI | Total | |
| Paper Towel Test by pictorial leakage category | n (%) | n (%) | n (%) | |
| 1 drop | 3 (23.1) | 7 (31.8) | 1 (16.7) | 11 |
| 3 drops | 2 (15.4) | 5 (22.7) | 1 (16.7) | 8 |
| 1 mL | 5 (38.5) | 5 (22.7) | 2 (33.3) | 12 |
| 3 ml | 1 (7.7) | 0 (0.0) | 1 (16.7) | 2 |
| 6 ml | 2 (15.4 | 5 (22.7) | 1 (16.7) | 8 |
| Total | 13 | 22 | 6 | 41 |
Categories in BOLD indicate Independently Self-Administered Paper Towel Test (PTT-ISA) classification that would likely be deemed clinically important, although perception of bother by volume of urine leaked can vary across woman
Considering the entirety of the sample, Kappa for conceptually similar groups (questionnaire-only versus PTT-ISA+questionnaire ) was calculated as 0.49 (95% CI: 0.41 – 0.57), reflecting moderate agreement by traditional Kappa interpretations.
DISCUSSION
This study showed near total study participant compliance in conducting PTT-ISA at an in-person visit of an epidemiologic study, and that PTT-ISA extends information about individual women in important ways as compared to data acquired by questionnaire only. 2 Our study findings are consistent with prior work. A historical study conducted in 1999 reported on 47 women recruited by answering ‘yes’ to screening question of leakage with coughing.6 Agreement between questionnaire-only and clinician-administered paper towel test was reached in half (53%) of the cases. This was when data for each participant was reduced to none, some, or a lot of leakage. Similarly, a study from 2010 concluded that questionnaire-only had low sensitivity in predicting demonstrable leakage on cough provocation. This was amongst women awaiting an ultrasound procedure requiring very full bladder.7
Our findings differ somewhat in magnitude from Wiskind et al (1994) of “One Hundred Stable Bladders.” 8 This team showed urodynamic confirmation of stress UI (leakage produced on coughing with catheter in the urethra) could only be demonstrated in 34% of 76 women who self-reported stress UI (as compared to our study showing agreement of 45.8% of 131 women). Their team’s lower agreement between the measures may be due to the protocol since a catheter in place partially blocks the urethra, and the supine or lithotomy position is typically protective against leakage.
There are many potential explanations of differences between questionnaire recall data and objective cough-provocation tests’ results. For instance, a category often referred to as occult stress UI in clinical settings was labeled descriptively in our study as DRYPTT/Q-OTHER1 to indicate coding for women who noted “yes” to stress UI on questionnaire but had no demonstrable leakage on PTT-ISA. Many situational differences might account for this type of finding, including provocations that differ from cough, such as high impact exercise or relative low or high bladder volume at time of PTT-ISA. Compound questions in survey or interview, such as ‘do you leak with cough, laugh, sneeze, exercise… logically limits cohesiveness with cough-only objective testing.
To our knowledge, leakage variance at differing bladder volumes and relative to a woman’s usual bladder volume has not been systematically evaluated. For instance, women who avoid bladder volumes that approach a normal physiologic fullness by practicing very frequent voiding may feel a sensation of need to toilet at bladder volumes too low to be responsive to leakage from cough provocation. Alternatively, indicating ‘no’ to stress leakage on questionnaire could occur in women whose activities, including cough effort, are so low that there is absence of rise in bladder pressures to the extent that would induce leakage.
Another explanation of differences found in the literature is altered findings of a cough provocation test is performed in front of someone because the act of performing a cough of enough pressure that might induce leakage would result in an embarrassing event. Therefore, a woman may produce a cough pressure below her customary normal. We believe women may be less prone to hold back on coughing when the awkwardness of clinician observation of the urethra is removed, which is an advantage to using the PTT-ISA.
On the contrary, a woman may cough above her “usual” cough pressure, in an effort to elicit the leakage that she reported by questionnaire, which typically includes examples beyond just coughing, for instance, during physical exercise. We have found in related studies that maximum cough pressures do not vary by more than 15–20% (unpublished data), likely because coughing is such a familiar and well-practiced human activity. So, altered cough pressure is a less plausible explanation for the differences we found.
It is important to recognize that conduction of the PTT-ISA in a restroom might increase likelihood of urgency-induced leakage in women for whom sight of a toilet is an urgency trigger that might compound tendency to leak on cough. Cough-induced detrusor instability leakage would be expected to occur a few seconds after the cough provocation event, rather than precisely at the moment of cough. Less likely is that a drop of sweat or vaginal secretion could be mistaken for urine. In clinical practice, we find that women readily differentiate these experiences in the moment of testing.
Most likely incomplete cohesiveness between questionnaire-only and PTT-ISA+questionnaire is a reflection of the complexity of UI. This complexity is important to capture in our measures. Offering women opportunity to respond to a few simple questions in addition to recording their PTT-ISA results could help resolve some of these contextual issues.
Pragmatically, a question on whether degree of leakage revealed by PTT-ISA is of bother to an individual woman is important. Bother can vary widely across women, with even a drop or two of leakage perceived by some as bothersome, while others express no bother by amount typically requiring a pad. Furthermore, a woman may find the PTT-ISA result to be a surprise. She may express that the result in that moment of volitional hard coughing differs from her lived experience (more or less than PTT-ISA leakage) outside of this controlled test condition, for many reasons.
We now recommend providing opportunity for participants to add clarification regarding these complexities via a few simple questions at the end of the results report form for the PTT-ISA: 1) Did you complete this test with your bladder comfortably full? 2) Did leakage occur at the moment of the cough? 3) Is this quantity of urine loss bothersome to you? 4) Is your paper towel test result a surprise to you?
Fig 2 shows our newly recommended PTT pictogram with these questions and accompanying response options. The updated pictogram now includes a US coin (quarter) placed on the paper towel during photographing so relative size visually can help in selection of wetted area closest to the individual’s towel result. The new pictogram options also better reflect meaningful gradation in leakage, by adding an additional photo on the far right of urine pooling on the paper towel to the extent that the entire towel is wet (well beyond 6 ml volume, which is when urine begins to run off the towel).
The fully explicated PTT-ISA protocol, with newly recommended pictogram, introductory language, and step-by-step instructional for the woman self-testing is provided in Supplemental Materials. Additionally, a script for research/medical staff is provided in the spirit of “manual of procedures”, which may be needed in either research or clinical applications when a staff person invites a woman to do PTT-ISA.
Limitations:
The UI questions used in the SWAN study are limited to those reported here and reflect the necessary balance in the parent study of minimizing burden and retaining original questions over decades of time. That said, these basic questions do reflect similar phrasing to that found in lay literature commonly presented to healthy community women per magazines, websites, and primary care screening forms. Arguably, these phrasings of questions are also consistent with primary care providers’ history taking to form an initial impression of continence status, prior to referral for specialist care.
PTT-ISA, the protocol in our study did not include passive bladder filling as is typically done in clinical studies via catheter, nor did it include collecting post-void bladder volumes immediately after testing to estimate bladder volume on testing. Although these were choices made due to the limitations of the testing environment and desire to avoid disrupting well-established data collection procedures in place, we cannot rule out the possibility that the PTT-ISA was conducted in a moment of exceptionally high or exceptionally low bladder volume, which could alter results of the test.
Although women were asked to wipe the perineum with toilet paper prior to self-testing to remove dampness, e.g. vaginal secretions, sweat, residual urine, it remains possible that substances still transferred to a testing towel and were mistaken for urine. In our experience with paper towel testing, we have observed that women readily recognize sweat and vaginal secretions apart from urine on the towel, and disregard.
The significance of our study results is demonstrating potential to expand data-informed experiences of bladder control as captured within epidemiologic studies. Simple, inexpensive, independently self-administered tools for objective sign of urine loss, conducted without need for interaction with a medical clinician, is pragmatically and scientifically important.
We have shown the PTT-IAP meets epidemiology demands for rigor that assure robust generalizability of findings per compliance with use of the tool in those with and without the disorder, and per compliance rates equivalent to survey instrument enabling subjective experience of urine loss to be relationally explored against cough provocation objective sign otherwise typically missing in survey-based epidemiology.
Further research warrants additional reliability and validity testing. Suggestions for validity testing include a pictorial panel with photo of a paper towel that includes vaginal secretions or sweat to contrast appearance to either dry towel or urine on towel. Validity testing might include a control group of women who hold the PTT test against the perineum but do not cough to account for such factors.
CONCLUSIONS
We conclude the PTT-ISA merits consideration as a simple measure for objective sign of unwanted urine loss in studies that otherwise rely solely on survey methods. PTT-ISA is of minimal to no cost and ensues low additional participant burden. It potentially offers high yield of important new data, which can be used to generate new hypotheses that account for variance in experience of urinary incontinence across community-based populations.
Supplementary Material
Acknowledgements
Clinical Centers:
University of Michigan, Ann Arbor ‒ Siobán Harlow, PI 2011 ‒ present, MaryFran Sowers, PI 1994‒2011; Massachusetts General Hospital, Boston, MA ‒ Joel Finkelstein, PI 1999 ‒ present; Robert Neer, PI 1994 ‒ 1999; Rush University, Rush University Medical Center, Chicago, IL ‒ Imke Janssen, PI 2020 ‒ Present; Howard Kravitz, PI 2009 ‒ 2020; Lynda Powell, PI 1994 ‒ 2009; University of California, Davis/Kaiser ‒ Elaine Waetjen and Monique Hedderson, PIs 2020 ‒ Present; Ellen Gold, PI 1994‒2020; University of California, Los Angeles ‒ Arun Karlamangla ‒ Present; Gail Greendale, PI 1994‒2020; Albert Einstein College of Medicine, Bronx, NY ‒ Carol Derby, PI 2011 ‒ present, Rachel Wildman, PI 2010 ‒ 2011; Nanette Santoro, PI 2004 ‒ 2010; University of Medicine and Dentistry ‒ New Jersey Medical School, Newark ‒ Gerson Weiss, PI 1994 ‒ 2004; and the University of Pittsburgh, Pittsburgh, PA ‒ Rebecca Thurston, PI ‒ present; Karen Matthews, PI ‒2020.
NIH Program Office:
National Institute on Aging, Bethesda, MD ‒ Rosaly Correa-de-Aranjo 2020 ‒ present; Chhanda Dutta 2016 present; Winifred Rossi 2012‒2016; Sherry Sherman 1994 ‒ 2012; Marcia Ory 1994 ‒ 2001; National Institute of Nursing Research, Bethesda, MD ‒ Program Officers.
Central Laboratory:
University of Michigan, Ann Arbor ‒ Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center:
University of Pittsburgh, Pittsburgh, PA ‒ Maria Mori Brooks, PI 2012 - present; Kim Sutton-Tyrrell, PI 2001 ‒ 2012; New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995 ‒ 2001.
Steering Committee:
Susan Johnson, Current Chair
Chris Gallagher, Former Chair
Committee on Vaginal, Urological, Sexual Health (VUSH):
Elaine Waetjen, Current Chair
Coordinating Center Internal Forms Group
Alicia Brook Colvin
We thank the study staff at each site and all the women who participated in SWAN.
Funding information:
This work was supported by The Study of Women’s Health Across the Nation (SWAN), which has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495).
Footnotes
Competing interest: The authors have no competing interests.
Supplemental Materials Recommended detailed instructions: steps for women performing the Independently Self-Administered Paper Towel Test (PTT-ISA), instructional script for research coordinators, and suggested checklist for documenting reasons for missing data.
REFERENCES
- 1.Minassian V, Bzai T, Steward W. Clinical epidemiological insights into urinary incontinence. Int Urogynecol J 2017; 28: 687–696. [DOI] [PubMed] [Google Scholar]
- 2.Waetjen LE, Liao S, Johnson WO, Sampselle CM, Sternfield B, Harlow SD, Gold EB, for the Study of Women’s Health Across the Nation. Factors Associated with Prevalent and Incident Urinary Incontinence in a Cohort of Midlife Women: A Longitudinal Analysis of Data: Study of Women’s Health Across the Nation, American Journal of Epidemiology, Volume 165, Issue 3, 1 February 2007, Pages 309–318, 10.1093/aje/kwk018 [DOI] [PubMed] [Google Scholar]
- 3.Miller JM, Ashton-Miller JA, DeLancey JO. Quantification of cough-related urine loss using the paper towel test. Obstet Gynecol. 1998;91(5): 705–9. [DOI] [PubMed] [Google Scholar]
- 4.Neumann P1, Blizzard L, Grimmer K, Grant R. Expanded paper towel test: an objective test of urine loss for stress incontinence. Neurourol Urodyn, 2004; 23(7): 649–55. [DOI] [PubMed] [Google Scholar]
- 5.Guralnick ML, Fritel X, Tarcan T, Espuna-Pons M, Rosier P FWM. ICS Educational Module: Cough stress test in the evaluation of female urinary incontinence: Introducing the ICS-Uniform Cough Stress Test. [DOI] [PubMed] [Google Scholar]
- 6.Miller JM, Ashton-Miller JA, Carchididi LT, DeLancey JO. On the lack of correlation between self-report and urine loss measured with standing provocation test in older stress-incontinence women. J Womens Health. 1999;8(2): 157–62. [DOI] [PubMed] [Google Scholar]
- 7.Adanu RMK, DeLancey JOL, Miller JM, Asante A. The Physical Finding of Stress Urinary Incontinence among African Women in Ghana.” International Urogynecology Journal. 2006: 17(6) Springer-Verlag, pp. 581–85, doi: 10.1007/s00192-005-0062-x. [DOI] [PubMed] [Google Scholar]
- 8.Wiskind AK, Miller KF, & Wall LL. One Hundred Unstable Bladders. Obstetrics & Gynecology; 1994: 83(1), 108–112. Journal Article, United States: The American College of Obstetricians and Gynecologists. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.