Abstract
Introduction
The transition from early childhood to teen years (5–12) is a critical time of development, which can be made particularly challenging by a burn injury. Assessing post-burn recovery during these years is important for improving pediatric survivors’ development and health outcomes. Few validated burn-specific measures exist for this age group. The purpose of this study was to generate item pools that will be used to create a future computerized adaptive test (CAT) assessing post-burn recovery in school-aged children.
Methods
Item pool development was guided by the previously developed School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5–12) Conceptual Framework. The item pool development process involved a systematic literature review, extraction of candidate items from existing legacy measures, iterative item review during expert consensus meetings, and parent cognitive interviews.
Results
The iterative item review with experts consisted of six rounds. A total of 10 parent cognitive interviews were conducted. The three broad themes of concern were items that needed 1) clarification, needed context or were vague, 2) age dependence and relevance, and 3) word choice. The cognitive interviews indicated that survey instructions, recall period, item stem, and response choices were interpretable by respondents. Final item pool based on parental feedback consist of 57, 81, and 60 items in Physical, Psychological, and Family and Social Functioning respectively.
Conclusion
Developed item pools (n=198) in three domains are consistent with the existing conceptual framework. The next step involves field-testing the item pool and calibration using item response theory to develop and validate the SA-LIBRE5–12 CAT Profile.
Keywords: Pediatric burn outcomes, burn injury, observer-reported outcomes measure, computerized adaptive test, LIBRE
Introduction
Observer-reported outcome measures provide clinicians and researchers with standard assessment tools for understanding patient experiences of burn injury and treatment. They are an integral part of measuring the long-term physical and psychosocial outcomes of pediatric patients that have experienced burn injuries.1 Observer-reported outcome measures allow health care professionals and researchers to understand, from the survivor’s perspective, the multidimensional and complex adversities that patients encounter during recovery.2–4Additionally, observer-reported outcome measures permit clinicians and researchers to compare a patient’s unique experience against patients with similar demographics who have the same condition.5 This not only highlights areas in which the child is excelling but also uncovers low-performing areas where interventions or tailored care plans might be beneficial. Although several existing legacy measures assess burn outcomes in children, such as the Shriners Hospitals for Children/American Burn Association Burn Outcomes Questionnaire for Children and Youth (BOQ5–18)6, the fixed format of these legacy instruments pose a number of challenges given their length and difficulties of administering in routine clinical practice. These challenges call for a shift from traditional observer-reported outcome measures to computerized adaptive test- (CAT-) based assessments.
Computerized adaptive tests use a computer algorithm and item response theory (IRT) to administer only the most relevant subset of items to respondents from a calibrated item bank, which improves measurement precision, patient engagement, and response burden compared to fixed-form instruments.7 Item banks are large sets of items (e.g., 40–60 items) that aim to assess the continuum of an underlying, unidimensional construct intended for assessment. Items within an item bank aim to capture the full range of patients’ symptom frequency/severity or patients’ functional ability. To develop item banks, item pools, or large sets of candidate items, must be developed based on a conceptual model identifying condition- and treatment-related outcomes of importance from patient/caregiver and clinician perspectives. The development of candidate items follows standard methods for instrument development3, consisting of reviews of existing instruments, patient/caregiver concept elicitation interviews, patient/caregiver cognitive debriefing interviews, and expert clinician review of draft items. Once item pools are developed, they are calibrated using IRT psychometric analyses to form a final set of items that can be used to capture respondents’ symptom severity/function ability level on the underlying construct of interest. Prior to CAT development, researchers begin by creating the item pools in collaboration with clinical experts, burn survivors and their caregivers to ensure relevance to the target population.3,8
The School-Aged LIBRE5–12 item pool was created using the previously developed School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5–12) conceptual framework9. This framework was based on the World Health Organization’s International Classification for Functioning (WHO ICF-CY)10 and American Burn Association/Shriners Hospitals for Children Burn Outcomes Questionnaire (BOQ5–18)6. The primary aim of this paper is to report on the development of parent-reported item pools to assess burn outcomes in children ages 5 to 12 years old, guided by the three domains solidified in the previously established SA-LIBRE5–12 conceptual framework: Physical Functioning, Psychological Functioning, and Family and Social Functioning.9 To achieve this goal, item pools were developed and iteratively revised using clinician and parental feedback. The final item pools will then be administered, calibrated, and ultimately used to develop the SA-LIBRE5–12 CAT (Fig. 1).
Figure 1.
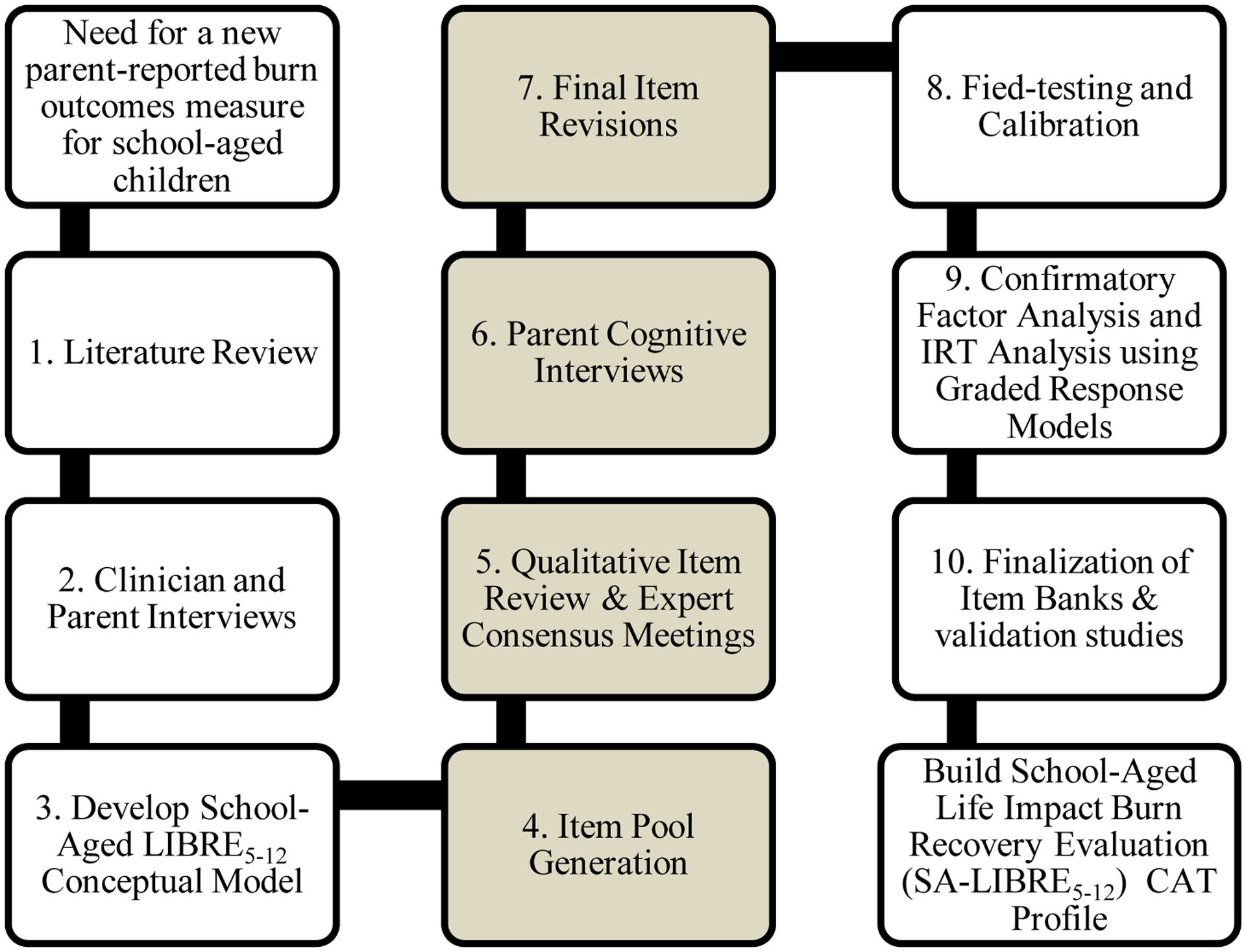
School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5–12) CAT Profile development process. Steps 1–3 are detailed elsewhere (Rencken et al. 2021). Steps 4–7 are described in the methods below.
Methods
The development process of SA-LIBRE5–12 CAT Profile consists of 10 steps (Fig 1). Steps 1 through 3 consisted of developing the conceptual framework and are detailed elsewhere.9 The current study focuses on steps 4 through 7, involving the development and refinement of item pools. This involved generating an initial item pool, qualitative item review, expert consensus meetings, cognitive interviews, and final item revisions.
Generating initial item pools and Qualitative item review
A systematic review previously conducted by our research team to identify literature on the impact of physical and psychosocial functioning on burn injuries guided the initial item pool generation (Appendix 1).11 The different instruments used to assess burn outcomes in the studies identified from the systematic review were further evaluated to capture the intended age group. That is, if the instrument was originally developed to assess outcomes in children 5 to 12 years of age, the research team attempted to obtain the items within the instrument. Instruments that could not be obtained through public access were eliminated. Additionally, initial candidate items were culled using previously developed patient- and observer- reported outcome measures (e.g., Patient-Reported Outcomes Measurement Information System (PROMIS), National Institutes of Health (NIH) Toolbox and Quality of Life in Neurological Disorders (Neuro-QOL)).
Extracted items from each measure were entered into a data collection spreadsheet in Excel. The following information was collected for each measure, as available: instrument name, instrument description, age demographics, the total number of items within the instrument, instructions for completing the instrument, recall period, item stem, item body, response options, and domains assessed.
Two research coordinators (KP and GG) binned and winnowed candidate items to remove duplicative and similar items and facilitate the iterative review process. Items were binned to assess similar content together and any doubts were discussed12. This process of binning was guided by the previously developed SA-LIBRE5–12 conceptual framework.9 Based on the subdomains, the research team ordered items along a continuum ranging from low to high levels of each construct. For example, items assessing “standing” and “walking” were assessed as items requiring low ability whereas “climbing” and “running” were assessed as items requiring high ability. This process ensured that items assessing different levels of ability and difficulty were captured appropriately for the age span included in this measurement for each of the 3 domains. Additionally, some measures included both self-reported and observer-reported items. Only proxy-reported items, appropriate for the parent or guardian of the child, were retained. If an observer-reported item was not available, self-reported items were recrafted for this purpose. Additionally, items were removed if they were irrelevant to this age group or condition-specific to a non-burn condition (i.e. Asthma) and inappropriate.
Expert consensus meetings
Expert consensus meetings were comprised of research coordinators with expertise in psychology, neuroscience, pediatrics, and public health (KP, GG, CR, SR, and EK), a surgeon scientist (CMR), a child and adolescent psychiatrist (FJS) with many years of experience in pediatric burns as well as a health services researcher (LK) who is an expert in psychometric measurement. The primary aim of the expert consensus meetings was to develop the item pool through reviewing and winnowing of items, standardizing language, and solidifying item placement along a continuum of ability. This goal was achieved in a series of six rounds between January 2020 and June 2020.
In the first three rounds, items were revised to clarify language or item content and ensure that items would be easy to understand for respondents. Additionally, they were reviewed to ensure they covered concepts that were important in measuring burn recovery, were age-appropriate, accounted for delayed or advanced development, and could be reliably reported upon. In the fourth round, item placement along the continuum was confirmed within each domain, and items were compared to constructs from the following well-established and valid measures: Burn Specific Health Scale13, Pediatric Symptoms Checklist-1714, Children’s Depression Inventory15, Child and Youth Resilience Measure16, Social-Emotional Assets and Resilience Scales-Parent report17, Child Behavior Checklist.18 Additionally, items were compared to the Preschool1–5 LIBRE19 and LIBRE Profile20 for adults for similarities, continuity, and bridging of the assessments. Items were carefully placed within each domain so that there was a balance of positive and negative items to avoid extreme response bias.21 The fifth round consisted of reviewing item content and language, creating a uniform recall period, item stems, and response options. Finally, in the sixth round, domain placement within the instrument was confirmed and novel items were created to address gaps in content. Other refinement steps used throughout the six rounds included ensuring coverage of the three areas of focus as well as checking verb tense agreement, item appropriateness, and inclusivity for demographic, socioeconomic, clinical, and developmental characteristics. For example, items such as ‘my child’s anxiety interfered with their ability to go to a sports event or ball game’ were revised since they might be socioeconomically or gender biased which might result in differential item functioning when conducting IR-based psychometric analysis. In addition, the refinement process confirmed that item language included common English phrases and not idioms specific to certain regions of the country.
Parent cognitive interviews
Parents/legal guardians who had a child with a history of burn injury and were between the ages of 5 and 12 years at the time of enrollment, received care at Shriners Hospitals for Children – Boston® were identified from electronic health records (EHR) and contacted through indirect methods (e.g., phone calls, emails). Additional inclusion criteria for participants were being 18 years or older, the legal guardian of the child, and able to speak and understand English. Participants were eligible to participate regardless of the child’s burn size, burn location, or time since burn injury, and were ineligible if they had previously participated in the SA-LIBRE5–12 semi-structured interview.9 Of the 15 participants scheduled for individual cognitive interviews, five did not answer at the scheduled time. After three unsuccessful attempts to reach them at follow-up times, these participants were deemed lost to follow-up. Consent information sheets were emailed to participants ahead of the interview time, and verbal informed consent was obtained prior to beginning the interview. Additionally, interviews could only be conducted virtually due to SARS-CoV-2. The following data was collected prior to the interview: participant age, race, and education, participant and child sex, number of children in the family, whether a spouse or adult partner is living with the participant, date of burn injury, burn size, burn location, burns to critical areas (face, hands, feet, genitalia), and burn etiology (contact, scald, flame, friction, or other).
The item pool was divided in half to reduce participant burden, and the contents of each group were reviewed by all investigators to ensure that both groups of parents reviewed items from each of the three domains. The first group of participants reviewed 97 items in the following subdomains and other specific areas: functional impact of physical symptoms (n=20), physical resilience (n=6), emotional functioning (n=21) resilience (n=20), peer relations (n=16) and school (n=14). The second group reviewed 95 items in the following areas: functional independence and activities of daily living (n=29), cognitive functioning (n=10), behavioral functioning (n=15), body image (n=14), community participation (n=7), and family functioning (n=20).
The purpose of cognitive interviews was to obtain feedback on the item content in our preliminary item banks. Participants were asked to assess item quality (i.e., clarity, relevance, comprehensiveness, and appropriateness). Interviews lasted between 45 and 90 minutes with one interviewer and one note-taker. Detailed notes were taken for each item in a word document template created by the research coordinators to later facilitate data analysis. Participants were provided with the appropriate items in a PDF file prior to the interview and the interviewer guided the participant through the slides during the virtual interview. Each item, item stem, and response option were presented individually. Participants read each item (either aloud or to themselves) and were asked about their interpretation of the item and response options (Appendix 2). An example was given to ensure participants understood the purpose of the interviews. Follow-up questions were tailored according to participant input to obtain granular data and ensure that participants were interpreting items as intended by the research team. Participants were provided reimbursement for their time upon interview completion.
Final item pool
Grounded theory methods guided the data analysis process. Cognitive interviews were conducted until thematic saturation was reached, as determined by recurrent themes during data analysis in tandem with data collection.22–24 Data (written notes during the interview) were condensed using an analysis key to identify themes of concerns that emerged. Cognitive interview feedback was presented to the principal investigator and clinical experts to identify item content that needed to be eliminated, added, or revised and make the appropriate adjustments.
Ethical approval
This study was approved by the Western Institutional Review Board (IRB number: 1-1249074-1) for Shriners Hospitals for Children.
Results
Generating initial item pools and qualitative item review
A total of 3,732 initial candidate items were identified from 128 existing measures and checklists during the literature review to generate the initial item pool.
The extracted items were divided into three domains: psychological functioning, physical functioning, and social and family functioning. After items were reviewed and eliminated due to similar items or duplicates, a total of 1,019 items remained.
Expert consensus meetings
During the first five rounds of review, items were winnowed from 1,019 items to 188. After all the qualitative item review rounds, expert consensus meetings, and creating novel items to address gaps in content, a total of 192 items were included in the item pool for cognitive testing. The recall period for all items was standardized to ‘In the past 7 days’. For most items, this recall period was followed by the item stem ‘your child’. The only subdomain without this item stem is parental satisfaction since these items refer to the parent’s emotions and behavior. Additionally, 5-point Likert scale response options were implemented and standardized for each item (Table 1).25,26
Table 1:
5-Point Likert scale options for item pools
| Frequency Assessment | Ability Assessment | General Health Assessment |
|---|---|---|
| Never | Unable to do | Poor |
| Rarely | With much difficulty | Fair |
| Sometimes | With some difficulty | Good |
| Often | With a little difficulty | Very good |
| Always | With no difficulty | Excellent |
Parent cognitive interviews
A total of 10 cognitive interviews were conducted and each item was reviewed by 4 or more parents. The parent sample age in years was 43.6 (range: 30.0 – 64.0), with 70% female and identified as White. The majority (70%) had a Bachelor’s degree or greater. The child age in years was 8.4 (range: 5.8 – 10.4), with 60% female (Table 2). TBSA for 70% of children was greater than 20% and 70% had burns to critical areas (Table 3). The majority of burn etiologies included flame injuries (40%) and scald burns (30%). On average, 1.3 years had elapsed since burn injury.
Table 2:
Cognitive interview parent participants demographics and characteristics of the burn injury (n = 10)
| Age (years), mean (range) | 43.6 (30.0 – 64.0) |
| Sex, n (%) | |
| Male | 3 (30%) |
| Race, n (%) | |
| White | 7 (70%) |
| Education Level, n (%) | |
| Completed some college | 2 (20%) |
| Completed Bachelor’s Degree | 3 (30%) |
| Partner at Home, n (%) | |
| No | 2 (20%) |
| Children under 18 living at home, mean (SD) | 1.9 (0.9) |
Table 3:
Cognitive interview child demographics and characteristics of the burn injury (n = 10)
| Age (years), mean (range) | 8.4 (5.8 – 10.4) |
| Sex, n (%) | |
| Male | 4 (40%) |
| Burn Etiology | |
| Scald | 3 (30%) |
| Other | 1 (10 %) |
| Years elapsed since burn injury, mean (SD) | 1.3 (1.9) |
| Total Body Surface Area Burned | |
| ≥ 20% | 3 (30%) |
| Burn to Critical Area | |
| No | 3 (30%) |
| Burn Location * | |
| Feet | 1 |
| Face | 2 |
Number does not equal sample size as some children had burns to multiple locations.
Parent cognitive interview feedback
Out of the 192 items presented, 37 items were considered clear by all parents. Parents considered the item stem, recall period, and response options to be appropriate with minimal feedback. Three broad themes of concern were notable: 1) needed clarification, needed context or were vague, 2) age dependence and relevance, and 3) word choice. Items were refined based on parental feedback (Table 4).
Table 4:
Examples of candidate items before and after cognitive interview-based refinement.
| Item presented in cognitive interview | Notes from cognitive interview | Broad theme of concern | Final item |
|---|---|---|---|
| Your child was able to use a fork or spoon | Parent 1: Suggestion on rewording? Your child was able to successfully feed themselves using a fork or spoon. Are they able to grip an object and hold it for an extended period of time? Similar to the previous question. Could be some age dependency. Use a fork or spoon mean do they pick it up or do they use it like I use it Parent 2: This is clear I understand exactly what it means. With his non-bandaged hand, yes he can use a fork and a spoon. Parent 4: Can my child eat independently? I think this one makes sense. Parent 5: Yes, very clear |
Word choice; Needs clarification | Your child was able to feed themself with a fork or spoon |
| Your child got tired easily and had little energy | Parent 6: To monitor energy levels; Clear choices Parent 7: Maybe expand the 7-day window; Depending on when, maybe since coming to Shriners or since treatment has started; Could be broken into two questions; Could be potentially two different answers Parent 9: Doesn’t make sense and then it does; Your child was telling you that they got tired. Parent 10: Clear |
Double barreled, needs clarification; time frame | Your child got tired easily |
| Your child had little energy | |||
| Your child was able to complete tasks | Parent 1: Not specific enough ‘complete tasks’. I would want to know if it’s about completing the task physically or mentally, or giving up easily, again putting it into context, were they able to complete tasks for school. Get ready for bed? Parent 2: This is pretty vague, I don’t know how I would be able to answer this. I would ask the specific task, like tie his shoe, or pick up a cup, etc. Parent 3: Pretty straightforward; The only thing that I can see someone getting caught up on between these last two; Reword: your child was able to complete any given task Parent 4:Can he finish something that he starts Parent 5: Yeah always |
Vague; word choice | Your child was able to complete tasks (e.g. simple chores such as pick up toys, clean room, or homework assignments) |
| Your child had eating problems | Parent 1: It’s not clear, is it digestion problems, she eats less than usual or more than usual. Maybe change to in the past 7 days your child’s appetite was typical of their behavior Parent 2: This is easy to answer. Parent 3: Yeah this one would be… I it eating problems like eating disorder or just appetite; How has your child appetite been, reword Parent 4: Specific eating problems like not eating or bulimia Parent 5: No, I want to say. I think about indigestion not appetite |
Need clarification, word choice; time frame | Your child had eating problems |
| Your child had a good appetite | |||
| Your child was anxious around strangers | Parent 6: Yes, this is a pretty relevant question based on the incident. Parent 7: I don’t love the word anxiety or anxious, but people relate to it; Maybe use uncomfortable instead Parent 8: Item is fine; Most children are anxious – normal behavior, but ‘anxious’ more strong than shy and could be related to injury; Anxiety about hospital but not nurses – so more about memory than people Parent 9: No, she just demands attention from strangers. Maybe that is anxious but she is as she has always been she wants attention. Easy to answer. Parent 10: Clear |
Word choice; Needs clarification | Your child was unsure of themselves around strangers |
| Your child was uncomfortable with others because of scars | Parent 1: I don’t know, your child was uncomfortable with other seeing their scars, I guess ‘because of’ feels a little weird. Parent 2: No one can see his scars, I would change it to scars or bandage. Parent 3: Add because of their scars instead ‘of’ Parent 4: I would answer this one, if he seems uncomfortable with the scars Parent 5: Never in the last 7 days |
Word choice | Your child was uncomfortable with others because of the appearance of their injury or scars |
| Your child was physically hurt by others | Parent 6: I mean, it has to be regarding what, I mean, I don’t know, it is too vague and hard to answer Parent 7: Straightforward; If he was purposely hurt byothers. Different form getting tackled while playing football Parent 9: No, Clear Parent 10: Think of one of her cousins hitting her; clear |
Vague | Your child was pushed or shoved around by other children |
| Your child had a before or after school job | Parent 1: doesn’t feel appropriate Parent 2: This does not apply to my 5 year old. Parent 3: Doesn’t apply to 5–12 age group; Probably 14 and up Parent 4: Clear Parent 5: Never, not really related to her age because she is 10. I said never because it’s not applicable |
Not applicable; Age dependent | Eliminated |
| Your child felt very close to our family | Parent 1: I do not know about that one. It says your child and our family so that is not consistent. Maybe reframe as your child was withdrawn. Parent 2: “Closer than usual? I don’t know”; This is hard to answer. Maybe add post-injury. Parent 3: Don’t really understand it; Is it referring to the hospital family?; Say ‘your family’; Your child and our family cancels out Parent 4: I don’t think he would say it, but does he say “I love you” or does he seem happy; If he was not feeling close to our family, I probably would not answer honestly Parent 5: Always, I think it depends on the parent if they would answer this honestly but I feel comfortable answering honestly |
Word choice; need context; hard for parent to know; need clarification; parents will not give an honest response | Your child felt very close to family |
| Others helped me when I had problems taking care of my child | Parent 1: not sure why it had to say ‘when I had problems’ maybe just say ‘when I needed it’s not clear Parent 2: This is easy to answer. Parent 3: Straightforward Parent 4: Who can I turn to help? Clear Parent 5: Mm sometimes. I think about family members when I think of other. The transition in item stem is clear and easy to read |
Need clarification; word-choice | Others helped me take care of my child |
Across parents, 15.4% of the feedback was related to items that needed clarification, context, or were vague. For example, for the item “Your child was able to stand still,” four parents felt the item needed clarification and context in terms of the intention, duration, or setting of the item. Based on parental feedback, this item was changed to “your child was able to stand still for several minutes.” Another item that needed clarification was “Your child felt weak.” Three parents felt that the item was not specific enough on whether it referred to the child’s physical or emotional state or the situation and context during which the child felt weak. Based on these comments, this item was adjusted to be more specific regarding physical ability, “Your child felt physically weak.”
Item age dependence and relevance were the second most common concern, 5.3% of all feedback. Some parents mentioned that certain items did not apply to all ages, did not apply to their child due to their current age, or were not relevant to burn recovery. For instance, the item “Your child volunteered for community activities” was revised on parental input regarding age dependency and relevance. Some parents felt this item did not “feel appropriate” or “would assume this is for older children” and suggested the inclusion of “after school activities” to be clearer. Hence, the research team revised the item to “Your child volunteered for afterschool or community activities”. This accommodated for the lower end of the age group for whom this item may not be applicable.
Lastly, 4.3% of the feedback was related to concerns about the word choice of certain items. For example, parents found the item “I felt that taking care of my child controlled my life” in the parental satisfaction subdomain focus “hard to answer” and felt that “the control part sounds negative”. Due to these concerns regarding word choice, this item was revised to “I felt that taking care of my child takes up all of my life.”
Final item pools
The final item pool consisted of 198 items (Table 5). A total of 52 instruments were used in the item pool along with novel items developed by the study team to address content gaps: 16 in physical functioning, 18 in social and family functioning, and 33 in psychological functioning (Table 6). After cognitive interviews, 14 items were rephrased, one item was removed, four items were added and three items were double-barreled and separated into two items each (Table 4). For instance, the item ‘your child got tired easily and had little energy’ was divided into ‘your child got tired easily’ and ‘your child had little energy’ (Table 4). The item ‘your child had a before or after school job’ was eliminated since it was not considered age-appropriate by parents. While identifying gaps in content and based on parent feedback, experts decided to address appetite (‘your child had a good appetite’) and three items relating to social media use (‘your child used social media as a learning tool,’ ‘your child used social media to connect with others,’ and ‘your child used social media to escape’).
Table 5:
Mapping Finalized Item Pools to the Conceptual Framework of Parent-Reported Child Health Outcomes Post-Burn Injury for Children 5 – to – 12 Years Old
| Domain | Subdomain | Subdomain Focus | Items |
|---|---|---|---|
| Physical Functioning (n= 57) | Functional Independence and Activities of Daily Living | Upper extremity & fine motor (n= 13 items) |
|
| Lower extremity & gross motor (n= 16) |
|
||
| Functional Impact of Symptoms | Sleep & Fatigue (n= 8) |
|
|
| Pain (n= 8) |
|
||
| Skin Symptoms (n= 6) |
|
||
| Physical Resilience (n= 6) |
|
||
| Psychological Functioning (n= 81) | Cognitive (n= 10) |
|
|
| Behavioral (n= 16) |
|
||
| Emotional (n= 21) |
|
||
| Body Image (n= 14) |
|
||
| Resilience (n= 20) |
|
||
| Social & Family Functioning (n= 60) | Social | Peer Relations (n= 16) |
|
| School (n= 14) |
|
||
| Community Participation (n= 10) |
|
||
| Family | Family Relationships (n= 10) |
|
|
| Parental Satisfaction (n= 10) |
|
||
Table 6:
Instruments and checklists included in three item pool along with the number of items included from each (n = 52).
| Instrument | Physical Functioning | Social and Family Functioning | Psychological Functioning |
|---|---|---|---|
| Body Esteem Scale for Adolescents and Adults (BESAA)1 | 2 | ||
| Brief Symptom Inventory2 | 1 | ||
| Burn Outcomes Questionnaire 11 –18(BOQ11–18)3 | 3 | ||
| Burn Outcomes Questionnaire 5 – 18(BOQ5–18)3 | 10 | 9 | 4 |
| Burn Specific Health Scale (BSHC)4 | 1 | ||
| Child and Health Youth Resilience Measure (CYRM)5 | 1 | ||
| Child Behavior Checklist6 | 1 | 5 | |
| Child Stress Disorder Checklist (CSDC)7 | 1 | 3 | |
| CSDC- Short Form (CSDC-SF)8 | 3 | ||
| Children’s Depression Inventory (CDI)9 | 5 | ||
| Children’s Behavior Questionnaire - Very Short Form (CBQ-VSF)10 | 1 | ||
| Cognitive Emotion Regulation Questionnaire (CERQ)11 | 1 | ||
| Emotional and Social Competency Inventory12 | 2 | ||
| Impact of Event Scale – Revised OR13 | 1 | ||
| Interpersonal Support Evaluation List14 | 1 | 1 | |
| Multidimensional Anxiety Scale for Children – Parent15 | 1 | 2 | |
| Neuro QOL Item Bank v1.0 – Pediatric Anxiety16 | 2 | 2 | |
| Neuro QOL Item Bank v1.1 – Pediatric Depression16 | 1 | ||
| Neuro QOL Item Bank v2.1 – Pediatric Fatigue16 | 1 | ||
| Neuro QOL Item v1.0 – Pediatric Stigma16 | 1 | 3 | |
| Neuro-QOL Item Bank v1.0 – Pediatric Social | 1 | ||
| Relationships - Interactions with Peers16 | |||
| NIH Toolbox Fixed Form v2.0 – Fear – Separation Anxiety – Parent Report17 | 1 | ||
| NIH Toolbox Fixed Form v2.0 – Negative Parent Relationship – Parent Report17 | 1 | ||
| NIH Toolbox Fixed Form v2.0 – Sadness – Parent Report17 | 2 | ||
| NIH Toolbox Fixed Form v2.0 – Sibling Rejection – Parent Report18 | 1 | ||
| NIH Toolbox Item Bank/Fixed Form v2.0 – Empathic Behaviors – Parent Report17 | 1 | ||
| NIH Toolbox Item Bank/Fixed Form v2.0 – Self Efficacy – Parent Report17 | 2 | ||
| Parenting Stress Index19 | 6 | ||
| Pediatric Symptoms Checklist20 | 1 | 5 | |
| Peer Relations Questionnaire For Children21 | 1 | ||
| Preschool LIBRE1–522 | 3 | 2 | |
| PROMIS Parent Proxy Bank v1.0 – Family Relationships23 | 4 | ||
| PROMIS Parent Proxy Bank v1.0 – Pain Behavior24 | 7 | ||
| PROMIS Parent Proxy Bank v1.0 - Psychological Stress Experiences25 | 1 | ||
| PROMIS Parent Proxy Bank v1.0 – Strength Impact26 | 4 | ||
| PROMIS Parent Proxy Bank v2.0 – Anxiety26 | 1 | ||
| PROMIS Parent Proxy Bank v2.0 – Fatigue27 | 1 | 1 | |
| PROMIS Parent Proxy Bank v2.0 – Mobility28 | 3 | ||
| PROMIS Parent Proxy Bank v2.0 – Pain Interference29 | 4 | 2 | |
| PROMIS Parent Proxy Bank v2.0 – Peer Relationships30 | 3 | ||
| PROMIS Parent Proxy Bank v2.0 – Upper Extremity31 | 3 | ||
| PROMIS Parent Proxy Item Bank v1.0 – Psychological Stress Experiences25 | 1 | ||
| PROMIS Parent Proxy Item Bank v1.0 – Sleep Disturbance32 | 1 | ||
| PROMIS Parent Proxy Item Bank v1.0 – Sleep Related Impairment32 | 1 | ||
| PROMIS Parent Proxy Item Bank v1.1- Cognitive Function33 | 2 | ||
| PROMIS Parent Proxy Scale v1.0 - Global Health34 | 1 | 2 | |
| PROMIS Pediatric Item Bank v1.0 - Sleep Related Impairment32 | 1 | ||
| Satisfaction with Appearance Scale35 | 1 | ||
| Social Emotional Assets and Resilience Scales - Parent report36 | 1 | ||
| Strength and Difficulties Questionnaire – 4 to 1037 | 3 | ||
| Vineland Adaptive Behavioral Scales38 | 2 | 4 | 6 |
| Youth Quality of Life – Short Form39 | 1 |
Within physical functioning, 57 items are divided among the three subdomains: functional independence and activities of daily living, functional impact of physical symptoms, and physical resilience. Functional independence and activities of daily living covers upper extremity and fine motor function (13 items) as well as gross motor and lower extremity function (16 items). Functional impact of symptoms covers sleep and fatigue (8 items), pain (8 items), and skin symptoms (6 items). The physical resilience subdomain examines adaptation and coping abilities post-burn injury (6 items). The items in the physical functioning domain use an ability, frequency, or perceived health 5-point Likert scale response option.
The psychological functioning item pool is comprised of a total of 80 items with cognitive (10 items), behavioral (16 items), emotional (21 items), body image (14 items), and resilience (20 items) subdomains. Lastly, the family and social functioning domain has 60 items divided among the family functioning and social functioning subdomains. In the family subdomain, items were divided into family relationships (10 items) and parental satisfaction (10 items). The items under social functioning included: peer relations (16 items), school (14 items), and community participation (10 items). Both psychological and family and social functioning domains use 5-point Likert scale response options.
Discussion
The primary aim of this study was to develop parent-reported item pools to assess outcomes that are important for burn recovery in children ages 5 through 12 years old guided by the three domains in the SA-LIBRE5–12 conceptual framework.9 We used previously developed legacy measures such as the Burn Outcomes Questionnaire (BOQ), a rigorous qualitative item review, and co-production including expert consensus meetings and parent cognitive interviews to finalize the item pools. Co-production was a key component of the development process as recent metric development guidelines recommend integrating direct feedback from the target end-users throughout all stages of instrument development.27–29 This ensures that the resulting item bank is age-appropriate, and deemed relevant as determined by all key stakeholders such as parents and clinicians. We created 3 item pools encompassing Physical Functioning (57 items), Psychological Functioning (80 items), and Family and Social Functioning (60 items). These item pools will be the foundation for the SA-LIBRE5–12 CAT which will aid families and physicians to assess children’s recovery and rehabilitation after a burn injury. Previous instruments have been developed to assess post-injury recovery in preschool children (Preschool LIBRE1–5)19,30 and adults (LIBRE journey).20,31 The SA-LIBRE5–12 9 provides an additional stepping stone for the continuity and bridging of the Preschool LIBRE1–5 and the LIBRE journey. Additionally, the item pools developed in the present study will contribute to the expanding literature on outcomes research aimed at improving health care providers’ ability to track and improve recovery efforts for burn survivors using CAT-based observer-reported outcome measures.9,19,20,30,31
The advantages of using CAT-based observer-reported outcome measures have been outlined in prior work19,32. For example, traditional legacy measures require the participant to answer all questions in the item bank, regardless of relevance to the patient. A CAT-based tool will eliminate irrelevant items based on prior endorsed responses in real-time. By limiting the number of questions one has to answer while tailoring the items to the participant, the participant burden can be significantly decreased while still capturing individualized scores to identify the patient’s specific needs. New systems are now being envisioned for future use with platforms that will allow CAT-based tools to be integrated into electronic health records.33 Systems such as REDCap (Research Electronic Data Capture) can use application programming interface (API) links to external servers so they are able to accommodate CAT-based systems. This provides a relatively seamless approach to administering a CAT tool with the scoring of observer-reported outcome measures and their feedback to clinicians not unlike a laboratory test.34–36 While there are many reasons to use observer-reported outcome measures, it is also important to note that in some settings, they may not be feasible. As they rely on technological access, they are likely not the most practical option in low-resource settings where patients and their caregivers do not have access to the necessary technology. In these scenarios, a fixed short-form instrument, adapted from the CAT and administered on paper, might be more appropriate.37
It is vital to assess recovery post-burn injury during middle childhood (5 to 12) since it is a crucial time for development in children. During this time, children gain independence from caregivers, awareness of body image, think about the future, pay attention to friendships and develop a sense of their place in the world.38,39 An estimated 10% of burn injuries occur between the age of 5 and 16.40 A burn injury can disrupt development and physical functioning during this period,41,42 since children’s ability to perform tasks they were previously capable of can be impacted, negatively influencing the level of independence for pediatric burn survivors.43 Erikson’s fourth stage of psychosocial development, industry versus inferiority, defines the importance of social independence gained through peer interactions and family dynamics.44 Previous burn outcomes research has reported bullying, behavioral problems, and emotional dysregulation in burn survivors to be linked to impaired functioning, while the presence of community engagement and peer acceptance have been associated with better outcomes following a burn injury.45–52 During this stage of development, children are also developing a greater sense of reality and body esteem which can be shifted due to changes in appearance resulting from a burn injury (e.g., burn garments, burn contractures, scaring, etc.).45,49,53–55 These changes can influence psychological functioning resulting in symptoms of depression, anxiety, trauma, and behavioral problems.56–58 Furthermore, self-esteem is critical at this time as children begin to separate themselves from their family environment and determine their place in the world.38 It is therefore essential for an instrument such as the SA-LIBRE5–12 to integrate items within physical, psychosocial, and family domains to appropriately track and obtain a holistic understanding of a burn survivor’s recovery.
This study has a number of limitations that need to be considered. First, our patient population had full access to American Burn Association verified pediatric burn centers. Therefore, our study may not be generalizable to other children with burns who did not receive specialized burn treatment. If we had the opportunity to include patients that received less support post-injury, we might observe more extreme results which would emphasize the need for a tool such as the SA-LIBRE5–12. Second, some items were changed from the original items in the legacy measures. For example, the item ‘When I have problems with the care of my son I can resort to some people for help or advice’ from the Pediatric Stress Index59 was changed to ‘Others helped me take care of my child’. The authors attempted to mitigate this limitation by basing items on a well-established conceptual framework that grounds our work in the WHO ICF-CY. Future work will include psychometric analysis and IRT-based analysis to validate the domains of the School-Aged LIBRE5–12 CAT Profile.
Despite these limitations, this item pool development process was comprehensive in covering the age-based development and physical, social, and psychological state of pediatric burn survivors as well as family functioning as reported by their parents. This work is an important contribution to the literature focusing on improving the widespread use of patient-centered and condition-specific outcome measurement tools to measure the long-term outcomes of burn injuries on a pediatric population. The SA-LIBRE5–12 CAT Profile, and observer-reported outcome measures more broadly, have the potential to transform how clinicians administer and measure the recovery process of their patients. CAT-based observer-reported outcome measures reduce participant burden, they are also able to tailor their item administration to respondents in real-time, creating the potential to use these metrics to support highly individualized care.
Conclusions
This study used the SA-LIBRE5–12 Conceptual Framework, qualitative item review, expert consensus meetings, and parent cognitive interviews to develop an item pool of 198 items encompassing the following domains: 1) Physical Functioning, 2) Psychological Functioning, and 3) Family and Social Functioning. The next step in the SA-LIBRE5–12 CAT Profile development will be a large-scale field-test of the item pool. Field-test findings will be used to calibrate the item pools using an IRT-based approach. The SA-LIBRE5–12 CAT Profile will help assess burn outcomes in school-aged children and provide individually tailored care. Additionally, it will allow caregivers, health care professionals, and researchers to track burn recovery outcomes in critical areas for school-aged children. Future research will be focused on developing a Teen-Aged LIBRE CAT to assess burn outcomes in teens 12 to 18 years old. Once each of the age- and condition-specific instruments have been developed and psychometrically tested, researchers will be able to track a patient’s recovery from childhood into adulthood by bridging each assessment. This provides a rich opportunity for improving clinical care and allows researchers to conduct novel longitudinal studies.
Supplementary Material
Acknowledgments
First and foremost, we would like to thank the parents who have participated in this study for their contributions to our research. Additionally, we would like to acknowledge the insight and expertise of the co-investigators and study staff that contributed to the development of the SA-LIBRE5-12 item pools.
Sources of Funding:
This work was supported by Shriners Hospitals for Children (Grant Award ID 79145-BOS-20) and the National Institute on Disability, Independent Living, and Rehabilitation Research (Grant #90DPBU0001) NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. Dr. Brady was affiliated with the Boston University School of Public Health Department of Health Law, Policy & Management at the time of this study and is currently an employee of a pharmaceutical company.
References
- 1.Ryan CM, Lee AF, Kazis LE, et al. Is real-time feedback of burn-specific patient-reported outcome measures in clinical settings practical and useful? a pilot study implementing the young adult burn outcome questionnaire. J Burn Care Res. 2016;37(1). doi: 10.1097/BCR.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 2.Griffiths C, Guest E, Pickles T, et al. The development and validation of the care burn scale-adult form: A patient-reported outcome measure (PROM) to assess quality of life for adults living with a burn injury. J Burn Care Res. 2019;40(3). doi: 10.1093/jbcr/irz021. [DOI] [PubMed] [Google Scholar]
- 3.Rothrock NE, Kaiser KA, Cella D. Developing a valid patient-reported outcome measure. Clin Pharmacol Ther. 2011;90(5). doi: 10.1038/clpt.2011.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Lee AF, Shapiro GD, et al. The development and validity of the adult burn outcome questionnaire short form. J Burn Care Res. 2018;39(5). doi: 10.1093/jbcr/irx043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kazis LE, Lee AF, Rose M, et al. Recovery curves for pediatric burn survivors advances in patient-oriented outcomes. JAMA Pediatr. 2016;170(6). doi: 10.1001/jamapediatrics.2015.4722. [DOI] [PubMed] [Google Scholar]
- 6.Daltroy LH, Liang MH, Phillips CB, et al. American burn association/shriners hospitals for children burn outcomes questionnaire: Construction and psychometric properties. J Burn Care Rehabil. 2000;21(1). doi: 10.1097/00004630-200021010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Reckase MD. Designing item pools to optimize the functioning of a computer adaptive test. Psychol Test Assess Model. 2010;52(2):127–141. https://www.researchgate.net/publication/44298424. [Google Scholar]
- 8.Fayers P, Hays R Assessing quality of life in clinical trials : methods and practice. J Epidemiol Community Heal. 2005;60(9). [Google Scholar]
- 9.Rencken CA, Rodríguez-Mercedes SL, Patel KF, et al. Development of the School-Aged Life Impact Burn Recovery Evaluation (SA-LIBRE5–12) Profile: A Conceptual Framework. J Burn Care Res. 2021. doi: 10.1093/jbcr/irab104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY. World Health Organization; 2007. https://apps.who.int/iris/handle/10665/43737. Accessed July 23, 2021. [Google Scholar]
- 11.Patel KF, Rodriguez-Mercedes SL, Grant GG, et al. Physical and Psychosocial Outcomes in Pediatric Burn Survivors Ages 5–18 Years: A Systematic Review. Manuscr Submitt Publ. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeWalt DA, Rothrock N, Yount S, et al. Evaluation of item candidates: The PROMIS qualitative item review. Med Care. 2007;45(5 SUPPL. 1). doi: 10.1097/01.mlr.0000254567.79743.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kildal M, Andersson G, Fugl-Meyer AR, et al. Development of a brief version of the burn specific health scale (BSHS-B). J Trauma - Inj Infect Crit Care. 2001;51(4). doi: 10.1097/00005373-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Jellinek MS, Murphy JM, Robinson J, et al. Pediatric Symptom Checklist: Screening school-age children for psychosocial dysfunction. J Pediatr. 1988;112(2). doi: 10.1016/S0022-3476(88)80056-8. [DOI] [PubMed] [Google Scholar]
- 15.de la Vega R, Racine M, Sánchez-Rodríguez E, et al. Psychometric properties of the short form of the Children’s Depression Inventory (CDI-S) in young people with physical disabilities. J Psychosom Res. 2016;90. doi: 10.1016/j.jpsychores.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: A brief measure of resilience. Can J Public Heal. 2013;104(2). doi: 10.1007/bf03405676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Endrulat NR, Tom KM, Merrell KW. Strength-based assessment: Applications and development of the Social-Emotional Assets and Resilience Scales, parent version. In: SASP 2009 Mini-Convention.; 2009. [Google Scholar]
- 18.Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment Burlington, VT: University of Vermont. Res Cent Child Youth, Fam. 2001;1617(82). [Google Scholar]
- 19.Grant GG, Brady KJS, Stoddard FJ, et al. Measuring the impact of burn injury on the parent-reported health outcomes of children 1-to-5 years: Item pool development for the Preschool1–5 Life Impact Burn Recovery Evaluation (LIBRE) Profile. Burns. 2021. doi: 10.1016/j.burns.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marino M, Soley-Bori M, Jette AM, et al. Measuring the Social Impact of Burns on Survivors. J Burn Care Res. 2017;38(1). doi: 10.1097/BCR.0000000000000398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinz A, Michalski D, Schwarz R, et al. The acquiescence effect in responding to a questionnaire. Psychosoc Med. 2007;4. [PMC free article] [PubMed] [Google Scholar]
- 22.Corbin JM, Strauss A. Grounded theory research: Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1). doi: 10.1007/BF00988593. [DOI] [Google Scholar]
- 23.Berg BL. Qualitative Research Methods for the Social Sciences. Boston, MA: Allyn and Bacon; 2001. [Google Scholar]
- 24.Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 25.DeWalt DA, Thissen D, Stucky BD, et al. PROMIS pediatric peer relationships scale: Development of a peer relationships item bank as part of social health measurement. Heal Psychol. 2013;32(10). doi: 10.1037/a0032670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kazis LE, Miller DR, Skinner KM, et al. Applications of methodologies of the Veterans Health Study in the VA Healthcare System: Conclusions and summary. J Ambul Care Manage. 2006;29(2). doi: 10.1097/00004479-200604000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7). doi: 10.1136/bmjqs-2015-004315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elwyn G, Nelson E, Hager A, et al. Coproduction: When users define quality. BMJ Qual Saf. 2020;29(9). doi: 10.1136/bmjqs-2019-009830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allen K, Needham C, Hall K, et al. Participatory research meets validated outcome measures: Tensions in the co-production of social care evaluation. In: Social Policy and Administration.Vol 53.; 2019. doi: 10.1111/spol.12468. [DOI] [Google Scholar]
- 30.Brady KJS, Grant GG, Stoddard FJ, et al. Measuring the impact of burn injury on the parent-reported health outcomes of children 1 to 5 years: A conceptual framework for development of the preschool life impact burn recovery evaluation profile cat. J Burn Care Res. 2020;41(1). doi: 10.1093/jbcr/irz110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marino M, Soley-Bori M, Jette AM, et al. Development of a conceptual framework to measure the social impact of burns. J Burn Care Res. 2016;37(6). doi: 10.1097/BCR.0000000000000358. [DOI] [PubMed] [Google Scholar]
- 32.Griggs CL, Schneider JC, Kazis LE, et al. Patient-reported outcome measures: A stethoscope for the patient history. Ann Surg. 2017;265(6). doi: 10.1097/SLA.0000000000002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu AW, Kharrazi H, Boulware LE, et al. Measure once, cut twice - Adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. J Clin Epidemiol. 2013;66(8 SUPPL.8). doi: 10.1016/j.jclinepi.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Riobueno-Naylor A, Romo S, Kazis L, et al. Usefulness of a Novel System for Feedback of Patient-Reported Outcome Measures in Children Recovering from Burns. J Burn Care Res. 2019;40(6). doi: 10.1093/jbcr/irz082. [DOI] [PubMed] [Google Scholar]
- 35.Hart DL, Wang YC, Stratford PW, et al. Computerized adaptive test for patients with knee impairments produced valid and responsive measures of function. J Clin Epidemiol. 2008;61(11). doi: 10.1016/j.jclinepi.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Wang YC, Hart DL, Stratford PW, et al. Clinical Interpretation of Computerized Adaptive Test-Generated Outcome Measures in Patients With Knee Impairments. Arch Phys Med Rehabil. 2009;90(8). doi: 10.1016/j.apmr.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 37.Marino ME, Dore EC, Ni P, et al. Developing Item Response Theory–Based Short Forms to Measure the Social Impact of Burn Injuries. Arch Phys Med Rehabil. 2018;99(3). doi: 10.1016/j.apmr.2017.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Middle childhood (6–8 years old). 2020. https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html. Accessed July 23, 2021.
- 39.Centers for Disease Control and Prevention. Middle Childhood (9–11 years of age). 2021. https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle2.html. Accessed September 17, 2021.
- 40.American Burn Association, Committee NBRA. National Burn Repository 2017 Update. Am Burn Assoc. 2017;60606(312):1–141. http://ameriburn.org/wp-content/uploads/2018/05/2017_aba_nbr_annual_report-1.pdf. [Google Scholar]
- 41.American Burn Association. National burn awareness week fact sheet. 2017.
- 42.World Health Organization. Burns. 2018. https://www.who.int/news-room/fact-sheets/detail/burns. Accessed July 23, 2021.
- 43.Moore P, Moore M, Blakeney P, et al. Competence and physical impairment of pediatric survivors of burns of more than 80% total body surface area. J Burn Care Rehabil. 1996;17(6). doi: 10.1097/00004630-199611000-00012. [DOI] [PubMed] [Google Scholar]
- 44.Erikson EH. Childhood and Society. Norton, New York; 1950. [Google Scholar]
- 45.Van Baar ME, Polinder S, Essink-Bot ML, et al. Quality of life after burns in childhood (5–15 years): Children experience substantial problems. Burns. 2011;37(6). doi: 10.1016/j.burns.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 46.Szabo MM, Ferris KA, Urso L, et al. Social competence in pediatric burn survivors: A systematic review. Rehabil Psychol. 2017;62(1). doi: 10.1037/rep0000116. [DOI] [PubMed] [Google Scholar]
- 47.Liber JM, List D, Van Loey NEE, et al. Internalizing problem behavior and family environment of children with burns: A Dutch pilot study. Burns. 2006;32(2). doi: 10.1016/j.burns.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 48.Pardo GD, García IM, Marrero FDRM, et al. Psychological impact of burns on children treated in a severe burns unit. Burns. 2008;34(7). doi: 10.1016/j.burns.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 49.Sveen J, Sjöberg F, Öster C. Health-related quality of life in Swedish pediatric burn patients and associations with burn and family characteristics. Burns. 2014;40(5). doi: 10.1016/j.burns.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 50.Byrne C, Love B, Browne G, et al. The social competence of children following burn injury: A study of resilience. J Burn Care Rehabil. 1986;7(3). doi: 10.1097/00004630-198605000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Pan R, dos Santos BD, Nascimento LC, et al. School reintegration of pediatric burn survivors: An integrative literature review. Burns. 2018;44(3). doi: 10.1016/j.burns.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 52.Browne G, Byrne C, Brown B, et al. Psychosocial adjustment of burn survivors. Burns. 1985;12(1). doi: 10.1016/0305-4179(85)90180-9. [DOI] [PubMed] [Google Scholar]
- 53.Willebrand M, Sveen J, Ramklint MDM, et al. Psychological problems in children with burns - Parents’ reports on the Strengths and Difficulties Questionnaire. Burns. 2011;37(8). doi: 10.1016/j.burns.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 54.Abdullah A, Blakeney P, Hunt R, et al. Visible scars and self-esteem in pediatric patients with burns. J Burn Care Rehabil. 1994;15(2). doi: 10.1097/00004630-199403000-00011. [DOI] [PubMed] [Google Scholar]
- 55.Jessee PO, Strickland MP, Leeper JD, et al. Perception of body image in children with burns, five years after burn injury. J Burn Care Rehabil. 1992;13(1). doi: 10.1097/00004630-199201000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Landolt MA, Buehlmann C, Maag T, et al. Brief report: Quality of life is impaired in pediatric burn survivors with posttraumatic stress disorder. J Pediatr Psychol. 2009;34(1). doi: 10.1093/jpepsy/jsm088. [DOI] [PubMed] [Google Scholar]
- 57.Beard SA, Herndon DN, Desai M. Adaptation of self-image in burn-disfigured children. J Burn Care Rehabil. 1989;10(6). doi: 10.1097/00004630-198911000-00019. [DOI] [PubMed] [Google Scholar]
- 58.Rimmer RB, Bay RC, Alam NB, et al. Burn-injured youth may be at increased risk for long-term anxiety disorders. J Burn Care Res. 2014;35(2). doi: 10.1097/BCR.0b013e31828c73ac. [DOI] [PubMed] [Google Scholar]
- 59.Richard R Abidin E Parenting Stress Index™. Third.; 1995. [Google Scholar]
References for Assessments
- 1.Mendelson BK, Mendelson MJ, White DR. Body-esteem scale for adolescents and adults. J Pers Assess. 2001;76(1). doi: 10.1207/S15327752JPA7601_6. [DOI] [PubMed] [Google Scholar]
- 2.Derogatis LR. The Brief Symptom Inventory: An Introductory Report. Psychol Med. 1983;13(3). doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- 3.Daltroy LH, Liang MH, Phillips CB, et al. American burn association/shriners hospitals for children burn outcomes questionnaire: Construction and psychometric properties. J Burn Care Rehabil. 2000;21(1). doi: 10.1097/00004630-200021010-00007. [DOI] [PubMed] [Google Scholar]
- 4.Blades B, Mellis N, Munster AM. A burn specific health scale. J Trauma - Inj Infect Crit Care. 1982;22(10). doi: 10.1097/00005373-198210000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: A brief measure of resilience. Can J Public Heal. 2013;104(2). doi: 10.1007/bf03405676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Achenbach T, Rescorla L. Manual for the ASEBA School-Age Forms & Profiles: Child Behavior Checklist for Ages 6–18, Teacher’s Report Form, Youth Self-Report.; 2001.
- 7.Saxe G, Chawla N, Stoddard F, et al. Child stress disorders checklist: A measure of ASD and PTSD in children. J Am Acad Child Adolesc Psychiatry. 2003;42(8). doi: 10.1097/01.CHI.0000046887.27264.F3. [DOI] [PubMed] [Google Scholar]
- 8.Bosquet Enlow M, Kassam-Adams N, Saxe G. The Child Stress Disorders Checklist-Short Form: A four-item scale of traumatic stress symptoms in children. Gen Hosp Psychiatry. 2010;32(3). doi: 10.1016/j.genhosppsych.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de la Vega R, Racine M, Sánchez-Rodríguez E, et al. Psychometric properties of the short form of the Children’s Depression Inventory (CDI-S) in young people with physical disabilities. J Psychosom Res. 2016;90. doi: 10.1016/j.jpsychores.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Putnam SP, Rothbart MK. Development of short and very short forms of the Children’s Behavior Questionnaire. J Pers Assess. 2006;87(1). doi: 10.1207/s15327752jpa8701_09. [DOI] [PubMed] [Google Scholar]
- 11.Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire: Psychometric features and prospective relationships with depression and anxiety in adults. Eur J Psychol Assess. 2007;23(3). doi: 10.1027/1015-5759.23.3.141. [DOI] [Google Scholar]
- 12.Ferry K Emotional and Social Competency Inventory: Research Guide and Technical Manual.; 2017.
- 13.Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41(12). doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Delistamati E, Samakouri MA, Davis EA, et al. Interpersonal support evaluation list (ISEL) - College version: Validation and application in a greek sample. Int J Soc Psychiatry. 2006;52(6). doi: 10.1177/0020764006074184. [DOI] [PubMed] [Google Scholar]
- 15.March JS, Parker JDA, Sullivan K, et al. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4). doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Lai JS, Nowinski C, Victorson D, et al. Quality-of-life measures in children with neurological conditions: Pediatric neuro-QOL. Neurorehabil Neural Repair. 2012;26(1). doi: 10.1177/1545968311412054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salsman JM, Butt Z, Pilkonis PA, et al. Emotion assessment using the NIH Toolbox. Neurology. 2013;80(11 Suppl 3). doi: 10.1212/wnl.0b013e3182872e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cyranowski JM, Zill N, Bode R, et al. Assessing social support, Companionship, And distress: National institute of health (NIH) toolbox adult social relationship scales. Heal Psychol. 2013;32(3). doi: 10.1037/a0028586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abidin. Parenting Stress Index 3rd Edition: Professional Manual.; 1995.
- 20.Jellinek MS, Murphy JM, Robinson J, et al. Pediatric Symptom Checklist: Screening school-age children for psychosocial dysfunction. J Pediatr. 1988;112(2). doi: 10.1016/S0022-3476(88)80056-8. [DOI] [PubMed] [Google Scholar]
- 21.Rigby K Manual for the Peer Relations Questionnaire (PRQ). Point Lonsdale, Victoria, Australia: The Professional Reading Guide; 1998. [Google Scholar]
- 22.Grant GG, Brady KJS, Stoddard FJ, et al. Measuring the impact of burn injury on the parent-reported health outcomes of children 1-to-5 years: Item pool development for the Preschool1–5 Life Impact Burn Recovery Evaluation (LIBRE) Profile. Burns. 2021. doi: 10.1016/j.burns.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bevans KB, Riley AW, Landgraf JM, et al. Children’s family experiences: development of the PROMIS® pediatric family relationships measures. Qual Life Res. 2017;26(11). doi: 10.1007/s11136-017-1629-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Revicki DA, Chen WH, Harnam N, et al. Development and psychometric analysis of the PROMIS pain behavior item bank. Pain. 2009;146(1–2). doi: 10.1016/j.pain.2009.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bevans KB, Gardner W, Pajer KA, et al. Psychometric evaluation of the ProMISVR pediatric psychological and physical stress experiences measures. J Pediatr Psychol. 2018;43(6). doi: 10.1093/jpepsy/jsy010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Irwin DE, Gross HE, Stucky BD, et al. Development of six PROMIS pediatrics proxy-report item banks. Health Qual Life Outcomes. 2012;10. doi: 10.1186/1477-7525-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lai JS, Stucky BD, Thissen D, et al. Development and psychometric properties of the PROMIS® pediatric fatigue item banks. Qual Life Res. 2013;22(9). doi: 10.1007/s11136-013-0357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kratz AL, Slavin MD, Mulcahey MJ, et al. An examination of the PROMIS® pediatric instruments to assess mobility in children with cerebral palsy. Qual Life Res. 2013;22(10). doi: 10.1007/s11136-013-0397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Varni JW, Stucky BD, Thissen D, et al. PROMIS pediatric pain interference scale: An item response theory analysis of the pediatric pain item bank. J Pain. 2010;11(11). doi: 10.1016/j.jpain.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeWalt DA, Thissen D, Stucky BD, et al. PROMIS pediatric peer relationships scale: Development of a peer relationships item bank as part of social health measurement. Heal Psychol. 2013;32(10). doi: 10.1037/a0032670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hung M, Voss MW, Bounsanga J, et al. Examination of the PROMIS upper extremity item bank. J Hand Ther. 2017;30(4). doi: 10.1016/j.jht.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forrest CB, Meltzer LJ, Marcus CL, et al. Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep. 2018;41(6). doi: 10.1093/sleep/zsy054. [DOI] [PubMed] [Google Scholar]
- 33.Irwin DE, Stucky B, Langer MM, et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res. 2010;19(4). doi: 10.1007/s11136-010-9619-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Forrest CB, Bevans KB, Pratiwadi R, et al. Development of the PROMIS® pediatric global health (PGH-7) measure. Qual Life Res. 2014;23(4). doi: 10.1007/s11136-013-0581-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawrence JW, Heinberg LJ, Roca R, et al. Development and validation of the satisfaction with appearance assessing body image among burn-injured patients. Psychol Assess. 1998;10(1). doi: 10.1037/1040-3590.10.1.64. [DOI] [Google Scholar]
- 36.Endrulat NR, Tom KM, Merrell KW. Strength-based assessment: Applications and development of the Social-Emotional Assets and Resilience Scales, parent version. In: SASP 2009 Mini-Convention.; 2009. [Google Scholar]
- 37.Goodman R The strengths and difficulties questionnaire: A research note. J Child Psychol Psychiatry Allied Discip. 1997;38(5). doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 38.Sparrow SS, Cicchetii DV, Saulnier CA. Vineland Adaptive Behavior Scales, Third Edition. Third. Bloomington, MN: Pearson Assessment; 2016. [Google Scholar]
- 39.Patrick DL, Edwards TC, Topolski TD. Adolescent quality of life, part II: Initial validation of a new instrument. J Adolesc. 2002;25(3). doi: 10.1006/jado.2002.0471. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


