Abstract
Mothers of children with autism report higher levels of depression than mothers of children with other developmental disabilities. We explored the relations between child characteristics of diagnostic severity and problem behaviors, parenting stress, relationship quality, and depressive symptoms in 70 mothers of young children with autism. We hypothesized that relationship quality and parenting stress would relate to maternal depression beyond the contributions of child characteristics. Multiple regression analysis revealed a main effect of parenting stress above and beyond child problem behaviors and autism severity. A significant interaction emerged, with relationship quality buffering the effect of parenting stress on depression. Results suggest that the relation between child problem behaviors and maternal depression should be considered in conjunction with other measures of marriage and family stress. Relational quality and parenting stress may also represent important factors to be explicitly considered within intervention paradigms for young children with autism spectrum disorders.
Introduction
Mothers of children with autism spectrum disorders (ASD) report higher levels of stress and depression than mothers of children with developmental delays (Blacher and McIntyre, 2005; Carter et al., 2009; Taylor and Warren, 2011). Beyond the potential negative impacts for individuals and families, understanding and addressing this increased distress is particularly important since caregivers of very young children with ASD are often placed in the difficult roles of advocates, service coordinators, and interventionists for their children (Warren and Stone, 2011). Caregiver depression may be especially deleterious following diagnosis, negatively impacting the day-to-day life of the entire family as well as potentially limiting intervention access and benefit during a critical window of neurobehavioral plasticity (Osborne et al., 2008). It is therefore essential to understand what factors ameliorate or exacerbate such distress for primary caregivers over time. This pilot project examined the unique and interactive contributions of child behaviors, parenting stress, and relationship satisfaction to maternal depression in mothers of young children diagnosed with ASD an average of 1.4 years earlier.
Although multiple potential contributors to maternal depression have been identified, the relative contributions of child and family-level factors remain unclear. Several studies have described child characteristics that contribute to maternal stress and depression, including behavior problems, sleep problems, emotion regulation deficits, and cognitive impairment (Blacher and McIntyre, 2005; Lecavalier et al., 2006; Lyons et al., 2010). Increasingly, research suggests that behavior problems may contribute to more parent psychological distress than other aspects of core impairment, such as autism symptoms or cognitive abilities (Lecavalier et al., 2006; Lounds et al., 2007).
Family factors, particularly spousal relationships, are also likely important determinants of depression above and beyond child factors. Parents of children with autism tend to report less marital satisfaction (Benson and Kersh, 2011; Lee, 2009) than parents of typically developing children. Low marital satisfaction in mothers of children with ASD is linked to higher maternal negative affect (Siman-Tov and Kaniel, 2011). In addition, work with school-aged children with ASD has demonstrated associations between marital satisfaction and well-being as well as parenting efficacy (Benson and Kersh, 2011). There may be complex interactive relations between depressive symptoms, relationship satisfaction, and parenting stress. With significantly impairing core challenging behaviors inherent to the disorder present within families over time, relationship strength and satisfaction may buffer the effects of parenting stress on psychological distress and wellbeing, as has been found in parents of school-aged children with developmental disabilities (Kersh et al., 2006). Conversely, over time, a deleterious cascade of effects may result from relational and parenting stress increasing parents’ depression and potentially decreasing their abilities to access and implement treatments (Osborne et al., 2008; Osborne and Reed, 2010). In this context, describing the complex relations of family-level variables in addition to child-specific factors, may provide important information about components of effective care planning for families of young children with ASD.
In the current study, we used cross-sectional regression analysis to examine the relations between maternal depressive symptoms and 1) child characteristics (problem behaviors, adaptive and cognitive skills, and diagnostic severity), 2) family-level variables (parenting stress, relationship satisfaction), and 3) the interaction between the family level variables of parenting stress and relationship satisfaction. Given known contributions of socioeconomic factors to depression, we incorporated measures of annual income into our model. We hypothesized that higher levels of stress and less relationship satisfaction would result in higher levels of depression, beyond contributions of child characteristics. We also hypothesized that parenting stress and relationship satisfaction would interact to contribute to depressive symptoms, with relationship satisfaction buffering the negative effects of parenting stress on depressive symptoms.
Methods
Participants and Design
Participants included 70 mothers of recently-diagnosed children with ASD. This sample was drawn from families (n=201) receiving an ASD diagnosis from a university-based autism center for young children over a three-year interval. Parents completed a survey at a single time point (mean = 1.38 years [SD=.75]) after diagnosis assessing parental depression, child behavior, and other areas of child and family functioning (see Taylor and Warren, 2011). Clinical data from the child’s initial diagnostic evaluation were extracted from the medical record for all invited participants
Eighty-two families (41%) completed and returned the survey. We found no significant differences between responders and non-responders regarding income, age at diagnosis, child cognitive abilities, adaptive behavior, or autism severity scores (Gotham et al., 2009) generated from the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000). Respondents were primarily mothers (91%) and all subsequent analyses were restricted to maternal data (n=75). Five mothers did not provide information regarding a current partner relationship and as such were dropped from subsequent analyses, yielding a final sample size of 70.
Measures
Clinical Assessment Data.
Cognitive assessments were matched to a child’s age and developmental level and included two scales with the same standardized scores, the Mullen Scales of Early Learning (MSEL; Mullen, 1995) and the Differential Ability Scales – Second Edition (DAS-II; Elliot, 2007). These scores were combined into one index of cognitive ability. Adaptive behavior was assessed by the Vineland Adaptive Behavior Scales – Second Edition (VABS-II; Sparrow et al., 2005). Autism symptoms were based on scores on the ADOS Diagnostic Observation Schedule and a standardized severity score was generated based on age and language level (Gotham et al., 2009). Clinical diagnosis of children was based on all available data by a licensed clinical psychologist with established research reliability on the ADOS.
Maternal Distress.
To index psychological, parenting, and relationship distress, respectively, mothers completed the Center for Epidemiological Studies – Depression Scale (CES-D; Radloff, 1977), the Parenting Stress Index-Short Form (PSI; Abidin, 1995), and the Dyadic Adjustment Scale (DAS; Spanier, 1989).
Child behavior.
Caregivers reported on their child’s behavior problems by completing the Achenbach Child Behavior Checklist (CBCL; Achenbach, 2001) which yields Internalizing, Externalizing, and Total Problem composite scores. We only used CBCL-Total scores in our analyses due to the high correlation between CBCL-Internalizing and CBCL-Externalizing behaviors (r = .56, p < .01).
Results
Descriptive Statistics
Means, standard deviations, and correlations between key variables are presented in Table 1. Cognitive and adaptive behavior scores did not significantly relate to variables of interest and were excluded from further analyses. Higher depressive symptoms related to more parenting stress (r = .65, p < .01), less partner relationship satisfaction (r = −.40, p < .01), and more child problem behaviors (r = .45, p < .01). Higher levels of parenting stress (r = .50, p <.01) were significantly related to more child problem behavior.
Table 1.
Correlations and Descriptive Statistics for Key Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child Age | -- | |||||||||
| 2. Dx Severity | .13 | -- | ||||||||
| 3. IQ | −.05 | −.33* | -- | |||||||
| 4. Vineland | −.07 | −.17 | .60** | -- | ||||||
| 5. CBCL-Int | −.08 | −.12 | .03 | .17 | -- | |||||
| 6. CBCL-Ext | .20 | −.24* | .21 | .04 | .56** | -- | ||||
| 7. CBCL-Tot | .13 | −.22 | .14 | .19 | .81** | .87** | -- | |||
| 8. CESD | .17 | .15 | .00 | .18 | .39** | .34** | .45** | -- | ||
| 9. PSI | .34** | .05 | .26 | .17 | .40** | .50** | .54** | .65** | ||
| 10. DAS | .01 | −.18 | .20 | .17 | −.04 | −.05 | −.14 | −.40** | −.19 | -- |
| Mean | 4.98 | 7.15 | 65.90 | 74.02 | 62.19 | 60.73 | 64.07 | 90.96 | 29.65 | 109.70 |
| Standard Deviation | 1.77 | 1.77 | 19.83 | 10.13 | 9.19 | 11.54 | 9.68 | 22.76 | 9.64 | 22.14 |
p < .05
p < .01
p < .001
Regression Analyses
We used multiple regression analysis (see Table 2) to test our hypothesis that higher levels of stress and less interpersonal relationship satisfaction would result in higher levels of depression, independent of child behaviors and diagnostic severity. We included annual income in the first step to control for its possible confounding influence of socioeconomic status. We also included child variables (diagnostic severity and CBCL-Total) to examine the influence of child functioning on depressive symptoms. We then added family-level variables (the PSI and DAS). In our final step, we examined the PSI x DAS interaction.
Table 2.
Regression of CESD onto CBCL-Total, PSI, and DAS, controlling for Income and ADOS Severity
| Predictor | B | SE(B) | β | T | P | ΔR2 |
|---|---|---|---|---|---|---|
|
| ||||||
| Step 1 | ||||||
| Intercept | −.07 | 5.40 | −.01 | .99 | ||
| Income | .11 | .34 | .03 | .31 | .76 | |
| ADOS Severity | 1.63 | .66 | .28 | 2.47 | .02 | |
| CBCL-T | 5.46 | 1.20 | .52 | 4.57 | .00 | .28*** |
|
| ||||||
| Step 2 | ||||||
| Intercept | 8.08 | 4.39 | 1.84 | .07 | ||
| Income | −.19 | .29 | −.06 | −.68 | .50 | |
| ADOS Severity | .77 | .53 | .13 | 1.44 | .15 | |
| CBCL-T | 1.28 | 1.15 | .12 | 1.11 | .27 | |
| DAS | −2.46 | .94 | −.24 | −2.62 | .01 | |
| PSI | 6.18 | 1.15 | .58 | 5.37 | .00 | .30*** |
|
| ||||||
| Step 3 | ||||||
| Intercept | 6.65 | 4.17 | 1.59 | .12 | ||
| Income | −.09 | .27 | −.03 | −.34 | .73 | |
| ADOS Severity | .83 | .40 | .14 | 1.64 | .11 | |
| CBCL-T | 1.10 | 1.09 | .11 | 1.01 | .32 | |
| DAS | −1.17 | 1.00 | −.12 | −1.18 | .24 | |
| PSI | 5.83 | 1.09 | .55 | 5.33 | .00 | |
| DAS x PSI | −1.94 | .68 | −.28 | −2.85 | .01 | .05** |
p < .05.
p < .01.
p < .001.
Although child diagnostic severity and problem behaviors significantly predicted depression in Step 1 of the model, these relations became non-significant after the addition of relationship satisfaction and parental distress (both of which were significantly related to depression). The addition of family environment variables to the model in Step 2 accounted for a significant increase in amount of variance explained (ΔR2 = .30, p < .001). In Step 3, a significant PSI x DAS interaction (β = −.28, p = .01) emerged. High levels of marital satisfaction seemed to buffer the impact of parenting stress on maternal depression (see Figure 1).
Figure 1.
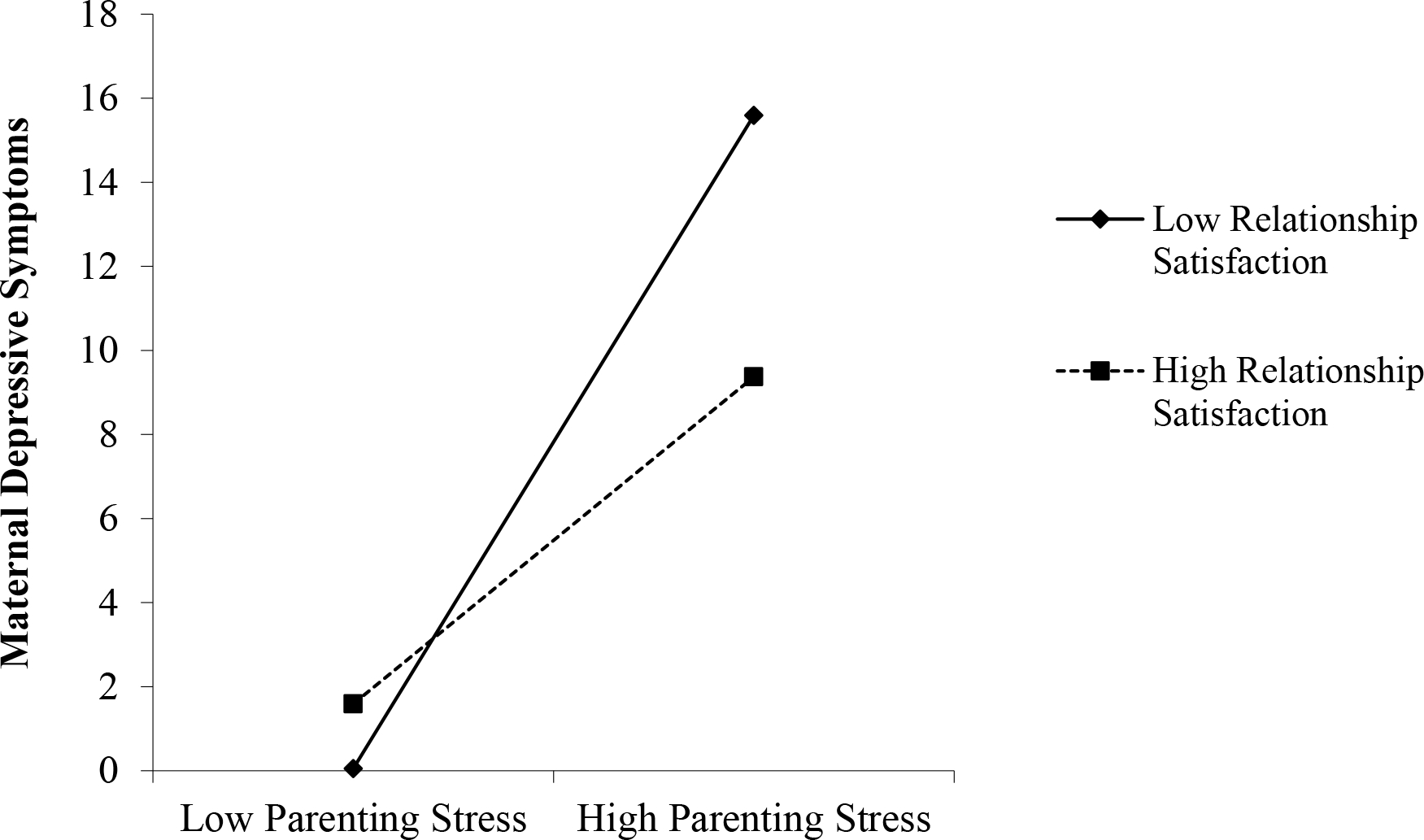
Higher parent stress and lower relationship satisfaction interact and relate to higher levels of depressive symptoms, controlling for child characteristics and problem behaviors. Note that z-scores were used in analyses and thus estimated values could fall below 0.
Discussion
Given the well-documented challenges of raising children with ASD, research identifying factors that worsen or alleviate the clinically significant distress surrounding diagnosis may help families adapt during this critical time by yielding targets for intervention and prevention efforts. Previous work has found elevated distress in parents of children with ASD often relates to child challenging behaviors, with emerging yet less consistent evidence emerging for other core aspects of child functioning such as autism symptoms or cognitive abilities (Lecavalier et al., 2006; Lounds et al., 2007). It is also apparent that child characteristics explain only a part of the patterns of elevated distress in caregivers over time (Carter et al., 2009; Taylor and Warren, 2011).
As expected, we found that parenting and relationship variables were related to maternal depressive symptoms above and beyond characteristics of the child with ASD and other family environment stressors, such as income. Our findings also suggest that relationship satisfaction may buffer, at least to some extent, the impact of parenting stress on maternal depression. This replicates the findings of Kersh et al. (2006) using a preschool-aged sample of children with ASD, suggesting that such protective effects can be found relatively soon after diagnosis.
It is important to note several methodological limitations of the current study. Specifically, we have no data about maternal psychological functioning, parenting stress, or partner relationship quality prior to child diagnosis, our findings are correlational in nature, and we relied on parent report to index many aspects of functioning. Although socioeconomically diverse, our sample was neither ethnically nor culturally diverse. We also explicitly excluded fathers, and single parents were under-represented. Interactive and transactional relations likely exist between partner relationship functioning, parent stress, depressive symptoms, and child characteristics and this study does not provide data that helps us understand the direction of such relations. Given the overlap in existing measurement strategies and significant correlations of these related constructs (e.g., the strong relations between parenting stress and child problem behaviors), we must be cautious in interpreting the magnitude and discrete contributions of effect. Due to these limits and the complex biopsychosocial factors influencing depression, we must be cautious about interpreting current findings in terms of suggesting potential causal relations or timelines of impact.
Despite these limitations, the current findings suggest that complex parenting and partner relationships play important roles in understanding parental adjustment following diagnosis, in addition to child specific factors. Ultimately, the direction of these relationships and the specific discrete contributions of underlying factors is unclear. However, given that over 29% of mothers in the current sample met the CES-D clinical risk cut-offs for depression and 79% retrospectively reported meeting cut-offs in the week following diagnosis (Taylor and Warren, 2011), the clinical relevance and import of understanding these factor relations is much clearer. Elevated caregiver distress after diagnosis of a young child with ASD may have significant harmful effects not only on parents and families, but also on the ability to fulfill the additional complex and challenging roles that caregivers of young children with ASD are frequently asked to play (e.g., advocates, service coordinators, and interventionists).
Parents of young children with ASD face unique caretaking challenges that exist within complex and important relationships. Our findings suggest that relationship quality and parenting stress explain a unique amount of the variance in maternal depressive symptoms, above and beyond the contributions of child-specific factors. In addition, they may exert a specific interactive influence; a more positive marital relationship may buffer the impacts of parenting stress on depressed mood after diagnosis, and a less positive relationship may exacerbate the impact of parenting stress on depressed mood at this time. As such, clinical providers may benefit from evaluating and addressing potentially problematic aspects of parenting and relational stress with caregivers, in addition to coordinating and delivering services targeted at children. Future longitudinal investigations addressing these relations could clarify the genesis, developmental framework, and specific relevance of relational and parenting stress to depression as well as psychological resilience.
Funding
This work was supported by a grant from the Vanderbilt Kennedy Center / Marino Autism Research Institute. This includes core support from a National Center for Research Resources grant to the Vanderbilt Institute for Clinical and Translational Research [UL1 RR024975-01]; and the Eunice Kennedy Shriver National Institute of Child Health and Human Development [P30HD15052].
References
- Abidin R (1995) Parenting Stress Index, 3rd Edition. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Achenbach TM (2001) Achenbach Child Behavior Checklist. Burlington, VT: ASEBA. [Google Scholar]
- Benson PR and Kersh J (2011) Marital quality and psychological adjustment among mothers of children with ASD: Cross-sectional and longitudinal relationships. Journal of Autism and Developmental Disorders 41: 1675–1685. [DOI] [PubMed] [Google Scholar]
- Blacher J and Mcintyre LL (2005) Syndrome specificity and behavioural disorders in young adults with intellectual disability: cultural differences in family impact. Journal of Intellectual Disability Research 50(3): 184–198. [DOI] [PubMed] [Google Scholar]
- Carter AS, de L Martinez-Pedraza F and Gray SA (2009) Stability and individual change in depressive symptoms among mothers raising young children with ASD: Maternal and child correlates. Journal of Clinical Psychology 65(12): 1270–1280. [DOI] [PubMed] [Google Scholar]
- Elliot CD (2007) The Differential Ability Scales (2nd ed.). San Antonio, TX: Pearson. [Google Scholar]
- Gotham K, Pickles A and Lord C (2009) Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders 39(5): 693–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kersh J, Hedvat TT, Hauser-Cram P, & Warfield ME (2006). The contribution of marital quality to the well-being of parents of children with developmental disabilities. Journal of Intellectual Disability Research, 50, 883–893. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Leone S and Wiltz J (2006) The impact of behavior problems on caregiving stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research 50(3): 172–183. [DOI] [PubMed] [Google Scholar]
- Lee (2009) Parents of children with high functioning autism: How well do they cope and adjust? Journal of Developmental and Physical Disabilities 21: 93–114. [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. (2000) The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders 30(3): 205–223. [PubMed] [Google Scholar]
- Lounds JJ, Seltzer MM, Greenberg JS and Shattuck PT (2007) Transition and change in adolescents and young adults with autism: Longitudinal effects on maternal well-being. American Journal on Mental Retardation 112(6): 401–417. [DOI] [PubMed] [Google Scholar]
- Lyons AM, Leon SC, Phelps CER and Dunleavy AM (2010) The impact of child symptom severity on stress among parents of children with ASD: The moderating role of coping styles. Journal of Child and Family Studies 19:516–524. [Google Scholar]
- Mullen EM (1995) Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Osborne LA, McHugh L, Saunders J and Reed P (2008) Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders 38(6): 1092–1103. [DOI] [PubMed] [Google Scholar]
- Osborne LA and Reed P (2010) Stress and self-perceived parenting behaviors of parents of children with autistic spectrum conditions. Research in Autism Spectrum Disorders 4: 405–414. [Google Scholar]
- Radloff LS (1977) The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1: 385–401. [Google Scholar]
- Siman-Tov A and Kaniel S (2011) Stress and personal resource as predictors of the adjustment of parents to autistic children: A multivariate model. Journal of Autism and Developmental Disorders 41: 879–890. [DOI] [PubMed] [Google Scholar]
- Spanier GB (1989) Manual for the Dyadic Adjustment Scale. North Tonowanda, NY: Multi-Health Systems. [Google Scholar]
- Sparrow SD, Cicchetti DV and Balla DA (2005) Vineland-II Adaptive Behavior Scales: Survey Forms Manual. Circle Pines, MN: AGS Publishing. [Google Scholar]
- Taylor JL and Warren ZE (2011) Maternal depressive symptoms following autism spectrum diagnosis. Journal of Autism and Developmental Disorders. DOI: 10.1007/s10803-011-1375. [DOI] [PubMed] [Google Scholar]
- Warren ZE and Stone WL (2011) Clinical best practices: Diagnosis and assessment of young children. In: Amaral D, Dawson G and Gerschwind D (eds) Autism spectrum disorders. New York: Oxford University Press. (pp. 1269–1280). [Google Scholar]


